Videofluoroscopy of the Oral Phase of Swallowing in Eight to Twelve Years Old Children with Dental Malocclusion
Abstract
INTRODUCTION
- To observe the oral phase of swallowing in patients with malocclusion;
- To identify the possible tongue adaptations in the oral cavity which make a swallow possible.
METHODS
- 1)
- Group A—Thirteen children with normal dental occlusion (Angle Class I);
- 2)
- Group B—Twenty children with dental malocclusion (Angle Class II);
- 3)
- Group C—Fourteen children with dental malocclusion (Angle Class III).
RESULTS
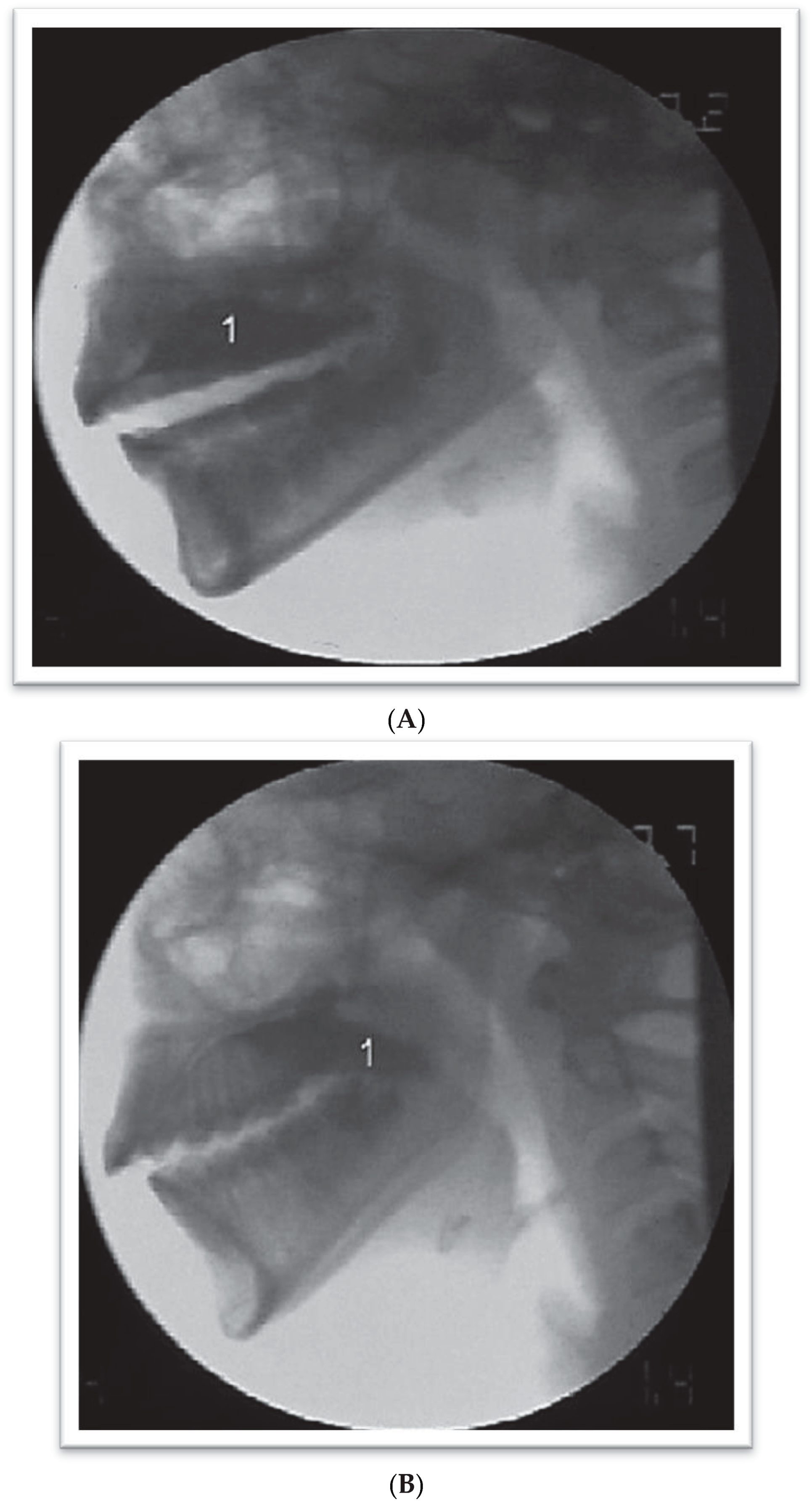
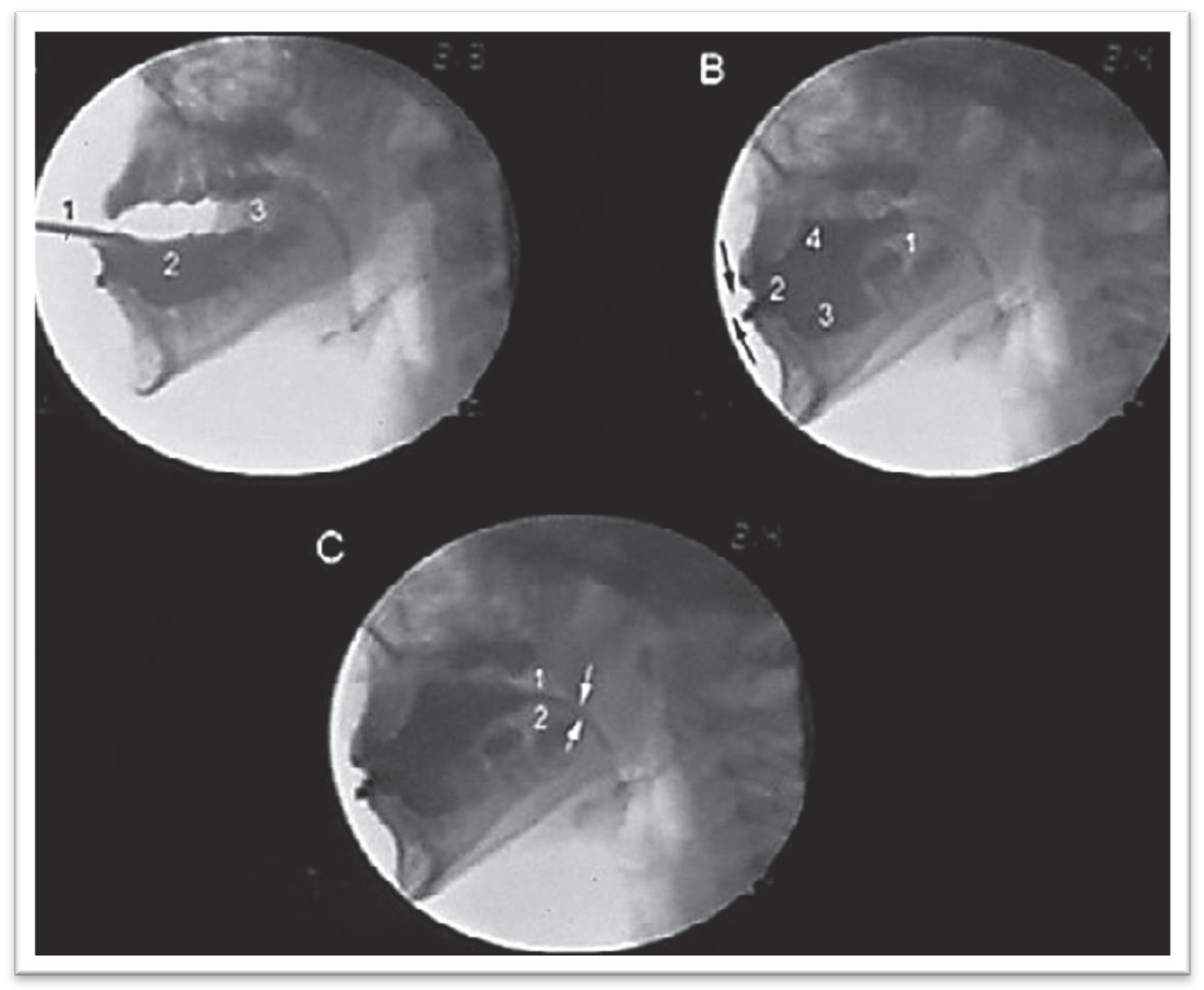
- Type I: Consistent Adaptation—Adapted TipperIndividuals in Group B with Class II malocclusion demonstrated the Adapted Tipper Swallow with the bolus going onto the tongue in 51.66% of the gulps observed. Individuals in Group C with Class III malocclusion demonstrated the Adapted Tipper Swallow in 59.52% of the gulps. The bolus was organized on the tongue and, in some cases this was accomplished with difficulty. It is defined by active mobilization of the tongue in maintaining the content. When ejection takes place, the tip of the tongue is placed between the incisors. Ejection is productive with apparent lower effectiveness and the strong influence of gravity.
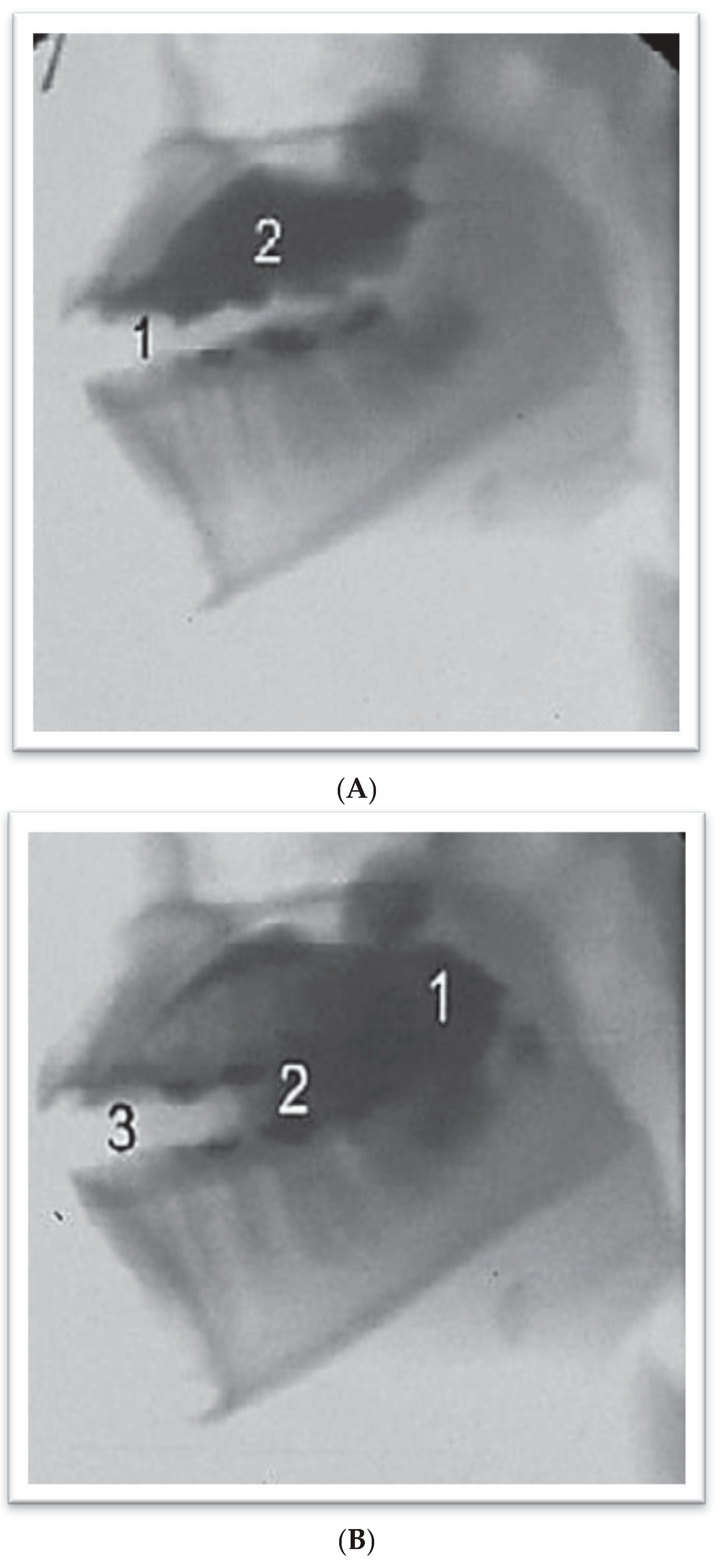
- Type 2 Consistent Adaptation—In two stagesIndividuals in Group B with Class II malocclusion demonstrated the Type 2 Consistent Adaptation—In two stages in 25% of the gulps. Individuals in Group C with Class III malocclusion demonstrated the Type 2 Consistent Adaptation—In two stages in 11.9%. During organization or at the beginning of oral ejection, part of the bolus escapes to the oropharynx and it is only ejected after it reaches the level of the vallecula. The bolus that remains in the oral cavity for this period of time and that is placed on the dorsal surface of the tongue is also propelled to the pharynx by a second ejection. Both ejection processes occur with the tip of the tongue placed between the incisors.
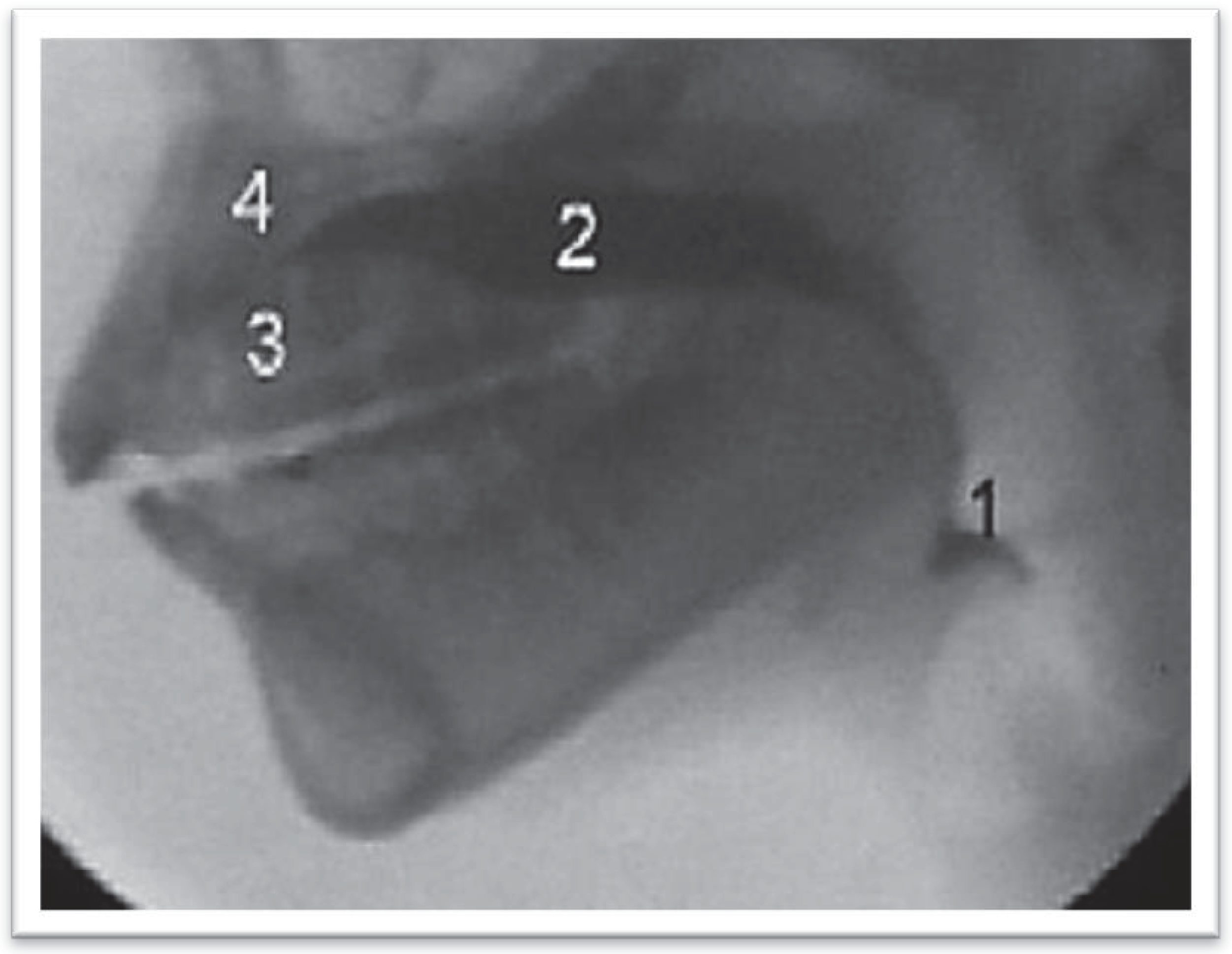
- Type 3 Consistent Adaptations—Extended TimeIndividuals in Group B with Class II malocclusion demonstrated the Type 3 Consistent Adaptation—Extended Time in 11.66% of the gulps. Individuals in Group C with Class III malocclusion demonstrated the Type 3 Consistent Adaptation-Extended Time in 7.14% of the gulps. In this Type 3, the bolus was placed on the dorsal surface of the tongue; however the bolus spread over the entire tongue and did not concentrate in the center of the tongue. The extended time for ejection occurred with the bolus being continuously propelled from the oral cavity to the pharynx, with strong help of gravity. During ejection, the tip of the tongue was placed between the incisors.
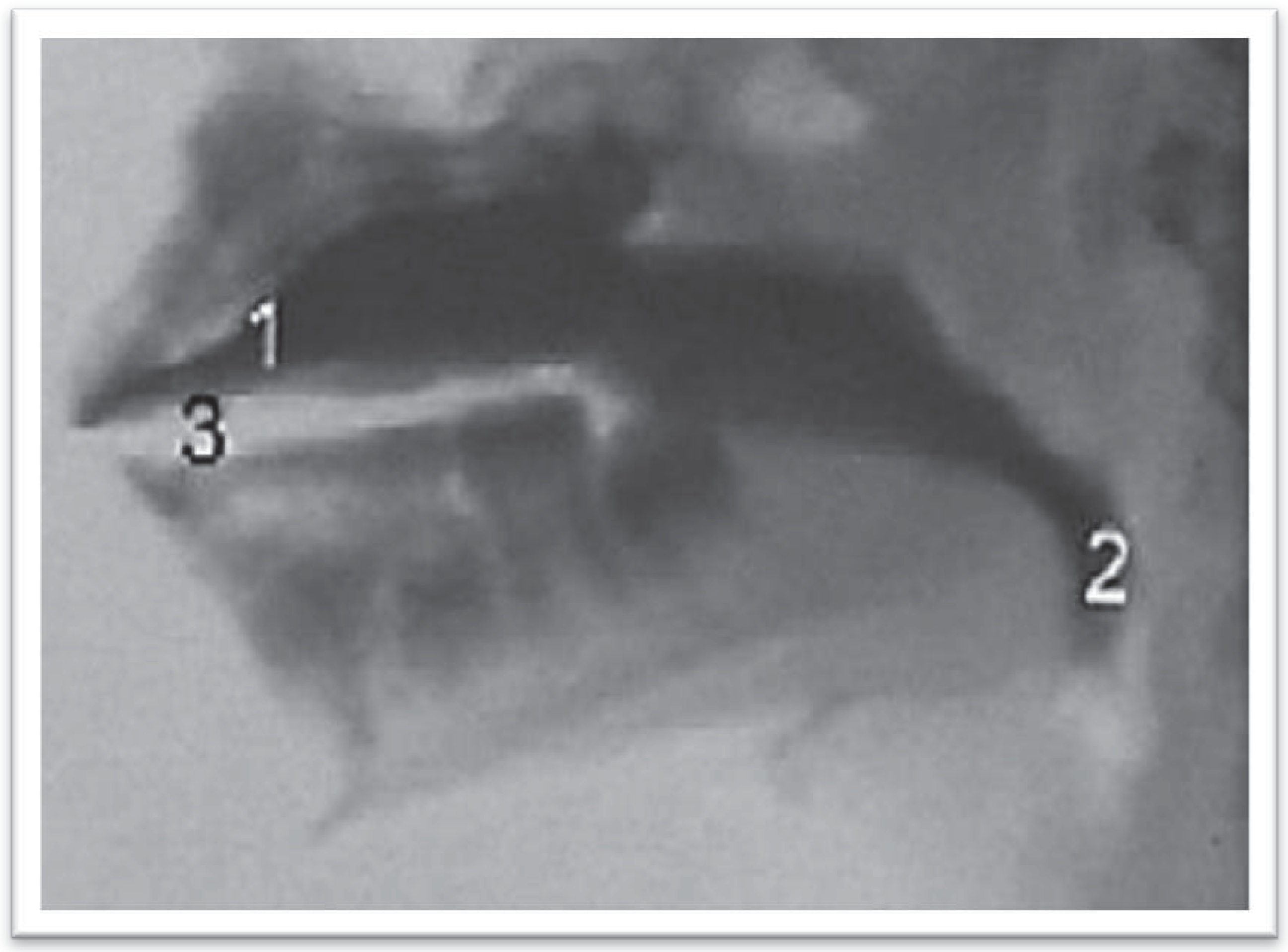
- Type 4 Consistent Adaptations—Adapted DipperIndividuals in Group B with Class II malocclusion demonstrated the Type 4 Consistent Adaptation—Adapted Dipper in 1.66% of the gulps. Individuals in Group C with Class III malocclusion demonstrated the Type 4 Consistent Adaptation-Adapted Dipper in 14.28% of the gulps. It was observed in Type 4 that most of the bolus, was placed under the anterior part of the tongue to start swallowing. Consequently, the tip of the tongue makes an anterior dip to place the bolus on the tongue before transporting it to the oropharynx. When most of the bolus is placed on the tongue, the tip moves from anterior to posterior to eject the bolus into the pharynx. The bolus that is on the tongue and the bolus under the tongue are simultaneously ejected. First, the bolus on the tongue was propelled to the posterior oral cavity, while the bolus under the tongue moved onto it and they both were finally ejected to the pharynx. During ejection, the tip of the tongue was placed between the incisors.
Irregular Inconsistent Adaptation
| Occlusion | Normal | II | III | Total | |||
|---|---|---|---|---|---|---|---|
| Swallowing | N | % | N | % | N | % | N |
| Tipper | 37 | 94.87 | 0 | 0.00 | 0 | 0.00 | 37 |
| Adapted Tipper | 0 | 0.00 | 31 | 51.67 | 25 | 59.52 | 56 |
| In Two Stages | 0 | 0.00 | 15 | 25.00 | 5 | 11.90 | 20 |
| Extended Time | 0 | 0.00 | 7 | 11.67 | 3 | 7.14 | 10 |
| Adapted Dipper | 0 | 0.00 | 1 | 1.67 | 6 | 14.29 | 7 |
| Inconsistent Adaptation | 0 | 0.00 | 6 | 10.00 | 3 | 7.14 | 9 |
| Dipper | 1 | 2.56 | 0 | 0.00 | 0 | 0.00 | 1 |
| Premature Loss of Bolus | 1 | 2.56 | 0 | 0.00 | 0 | 0.00 | 1 |
| Total | 39 | 100.00 | 60 | 100.00 | 42 | 100.00 | 141 |
| ❖ | |||||
| Swallowing | Normal | Adapted | Total | ||
| Occlusion | N | % | N | % | N |
| Normal | 37 | 94.87 | 2 | 5.13 | 39 |
| II | 0 | 0.00 | 60 | 100.00 | 60 |
| III | 0 | 0.00 | 42 | 100.00 | 42 |
| Total | 37 | 26.24 | 104 | 73.76 | 141 |
| ❖ | |||||
| ❖ X calc = 131.197 * | X | crit = 5.99 | |||
| ❖ II and III × Normal | X | calc = 131.197 * | |||
| ❖ II × III | X | calc = 0.000 | |||
DISCUSSION
CONCLUSIONS
- 1)
- The swallowing mode (oral phase) is different between individuals who present with normal occlusion and individuals who present with malocclusion.
- 2)
- There is no consistent pattern of swallowing based on the volume of liquids ingested for individuals with an Angle Class II or Class III malocclusion.
- 3)
- Anterior tongue protrusion occurred in every adapted swallowing mode, no matter the type of malocclusion with an Angle Class II or Class III.
References
- Altmann, E. B. C. 1994. Deglutição atípica. In Fisioterapia, fonoaudiologia e terapia ocupacional em pediatria, Edited by A. M. Kudo, E. Marcondes and L. Lins. , 2nd ed. São Paulo: Sarvier: pp. 125–133. [Google Scholar]
- American Speech-Language-Hearing Association [ASHA]. 2004. Guidelines for speech-language pathologists performing videofluoroscopic swallowing studies [guidelines]. Available online: www.asha.org/policy.
- Ballard, C. F. 1967. The morphological basis of prognosis determination and treatment planning. Dental Practitioner and Dental Record 18, 63: 107–115. [Google Scholar]
- Beck, J. T., and B. W. Gayler. 1990. Image quality abd radiation levels in videofluoroscopy for swallowing studies: A review. Dysphagia 5: 118–128. [Google Scholar] [PubMed]
- Bianchini, E. M. G. 2001. Avaliação fonoaudiológica da motricidade oral: distúrbios miofuncionais ou situações adaptativas. Revista Dental Press de Ortodontia e Ortopedia Facial 6: 73–83. [Google Scholar]
- Bianchini, E. M. G. 2005. Mastigação e ATM: Avaliação e terapia. In Fundamentos em Fonoaudiologia: aspectos clínicos da Motricidade Oral, I. Q. Marchesan (Org.), 2nd ed. Rio de Janeiro: Guanabara Koogan, pp. 45–58. [Google Scholar]
- Braga, G. C., and C. P. Machado. 1992. Deglutição atípica. In Ortodontia para Fonoaudiologia. Edited by E. Petrelli. São Paulo: Lovise, pp. 145–162. [Google Scholar]
- Cayley, A. S., A. P. Tindall, W. J. Sampson, and A. R. Butcher. 2000. Electropalatographic and cephalometric assessment of tongue function in open bite and non-open bite subjects. European Journal of Orthodontics 22: 463–474. [Google Scholar]
- Cleall, J. F. 1965. Deglutition: A study of form and function. American Journal of Orthodontics 51, 8: 566–594. [Google Scholar]
- Cochran, W. G. 1954. Some methods for strengthening the common X2: Test. Biometric 10: 417–451. [Google Scholar]
- Costa, M. M. B. 1998. Edited by M. M. B. Costa, L. Emo and K. Há. Dinâmica da deglutição: fases oral e faríngea. In Colóquio multidisciplinar deglutição e disfagia 1. Rio de Janeiro: PAEDD. [Google Scholar]
- Costa, M. M. B. 1999. Videofluoroscopia da deglutição. In Arquivos de motilidade digestiva e neurogastroenterologia. Edited by V. R. G. Michelsohn. São Paulo: Cop L. Print. [Google Scholar]
- Costa, M. M. B. 2010. Videofluoroscopy: The gold standard exam for studying swallowing and its dysfunction. Arquivos de Gastroenterologia 47, 4. [Google Scholar]
- Costa, M. M. B., J. L. L. Nova, M. T. Carlos, A. A. Pereira, and H. A. Koch. 1992. Videofluoroscopia: um novo método. Radiologia Brasileira 25: 11–18. [Google Scholar]
- Dantas, O. R. 1996. A videofluoroscopia no estudo das fases oral e faringeana da deglutição. Arquivos de Gastroenterologia 33, 3: 122–123. [Google Scholar]
- Dodds, W. J., J. A. Taylor, T. E. Stewart, M. K. Kern, A. J. Logemann, and I. J. Cook. 1989. Tipper and dipper types of oral swallows. American Journal of Roentgenology 153: 1197–1199. [Google Scholar]
- Felício, C. M. 1999. Fonoaudiologia aplicada a casos odontológicos. São Paulo: Pancast. [Google Scholar]
- Fink, F. S. 1986. The tongue, the lingometer and the role of accommodation in oclusion. The Angle Orthodontist 56, 3: 225–243. [Google Scholar]
- Fränkel, R. 1980. Lip seal training in the treatment of the skeletal open bite. European Journal of Orthodontics 2: 219–228. [Google Scholar] [CrossRef]
- Fraser, C. 2006. Tongue thrust and its influence in orthodontics. International Journal of Orthodontics (Milwaukee, Wis.) 17, 1: 9–18. [Google Scholar]
- Fuhrmann, R. A., and P. R. Diedrich. 1994. B-moode ultrasound scanning of the tongue during swallowing. Dentomaxillofacial Radiology 23, 4: 211–215. [Google Scholar] [PubMed]
- Gay, T., K. J. Rendell, and J. Spiro. 1994. Oral and laryngeal muscle coordination during swallowing. Laryngoscope 104: 341–349. [Google Scholar] [CrossRef] [PubMed]
- Hanson, M. L., and M. S. Cohen. 1973. Effects of form and function on swallowing and the developing dentition. American Journal of Orthodontics and Dentofacial Orthopedics 64, 1: 63–82. [Google Scholar] [CrossRef] [PubMed]
- Ichida, T., R. Takakiguchi, and K. Yamada. 1999. Relationship between the lingual-palatal contact duration associated with swallowing and maxillofacial morphology with the use of electropalatography. American Journal of Orthodontics and Dentofacial Orthopedics 116, 2: 146–151. [Google Scholar]
- Jann, H. W. 1960. Tongue thrusting as a frequente unrecognized cause of maloclusion and speech defects. The New York State Dental Journal 26: 72. [Google Scholar]
- Junqueira, P. 1997. A postura em repouso dos órgãos fonoarticulatórios frente aos limites anatômicos do paciente na terapia miofuncional. Pró-Fono: Revista de Atualização Científica 9, 1. [Google Scholar]
- Junqueira, P. 2003. A importância da fase oral na dinâmica da deglutição. In Tópicos em deglutição e disfagia. M. Costa, & L. P. Castro (Orgs.). Rio de Janeiro: Medsi, pp. 20–35. [Google Scholar]
- Junqueira, P., and M. M. B. Costa. 2001. Protocolo para avaliação videofluoroscópica da dinâmica da fase oral da deglutição de volume líquido. Pró-Fono: Revista de Atualização Científica 13: 165–168. [Google Scholar]
- Junqueira, P., and I. Q. Marchesan. 2008. Atípica ou adaptada: como considerar os problemas da deglutição? In Prática e aspectos atuais. Cap. 1. Rio de Janeiro: Revinter. [Google Scholar]
- Kortsch, W. E. 1965. The tongue implicated in classe II maloclusion. Journal of the Wisconsin Dental Association 41: 261–262. [Google Scholar]
- Langmore, S. E., K. Schatz, and N. Olson. 1988. Fiberoptic endoscopic evaluation of swallowing safety: A new procedure. Dysphagia 2: 216–219. [Google Scholar] [CrossRef]
- Logemann, J. A. 1993. Manual for the videofluorographic study of swallowing. Texas: Austin. [Google Scholar]
- Logemann, J. A. 2007. Swallowing disorders. Best Practice & Research Clinical Gastroenterology 21, 4: 563–573. [Google Scholar]
- Logemann, J. A., B. R. Pauloski, A. W. Rademaker, and P. J. Kahrilas. 2002. Oropharyngeal swallow in Young and older women: videofluorospic analysis. Journal of Speech, Language, and Hearing Research 45, 3: 434–445. [Google Scholar] [CrossRef] [PubMed]
- Maciel, C. T. V., and I. C. G. Leite. 2005. Aspectos etiológicos da mordida aberta anterior e suas implicações nas funções orofaciais. Pró-Fono: Revista de Atualização Científica 17, 3: 293–302. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Marchesan, I. Q. 1996. Deglutição atípica ou adaptada? [Vídeo]. São Paulo: Pró Fono. [Google Scholar]
- Marchesan, I. Q. 1998. Deglutição: como e quando tratar. In Temas: em deglutição e disfagia abordagem multidisciplinar. Edited by M. M. B. Costa, E. M. O. Lemme and H. A. Koch. Rio de Janeiro: Supra, pp. 59–63. [Google Scholar]
- Marchesan, I. Q. 1999. Adapted or atypical thrusting? The International Journal of Orofacial Myology 25: 15–17. [Google Scholar] [CrossRef]
- Marchesan, I. Q. 2000. The speech pathology treatment with alterations of the stomatognathic system. The International Journal of Orofacial Myology 26: 5–12. [Google Scholar] [CrossRef]
- Marchesan, I. Q. 2005a. Edited by Q. Marchesan I. Deglutição: diagnóstico e possibilidades terapêuticas. In Fundamentos em fonoaudiologia: aspectos clínicos da motricidade oral, 2nd ed. Rio de Janeiro: Guanabara Koogan: pp. 59–68. [Google Scholar]
- Marchesan, I. Q. 2005b. Tratamento da deglutição: a atuação do fonoaudiólogo em diferentes países. São Jose dos Campos: Pulso. [Google Scholar]
- Marchesan, I. Q. 2005c. Comparando as diferentes formas de atuar na deglutição. In Tratamento da deglutição: a atuação do fonoaudiólogo em diferentes países. I. Q. Marchesan (Org.). São Jose dos Campos: Pulso, pp. 341–360. [Google Scholar]
- Marchesan, I. Q., and A. M. Furkim. 2003. Manobras utilizadas na reabilitação da deglutição. In Tópicos em deglutição e disfagia. Edited by M. Costa and L. P. Castro. Rio de Janeiro: Medsi, pp. 375–384. [Google Scholar]
- Marchesan, I. Q., and N. T. Sanseverino. 2004. Fonoaudiologia e ortodontia/ortopedia facial: esclarecendo dúvidas sobre o trabalho conjunto. São Jose dos Campos: Pulso. [Google Scholar]
- Mason, R. M. 2005. A retrospective and prospective view of orofacial mycology. The International Journal of Orofacial Myology 31: 5–14. [Google Scholar] [CrossRef]
- Mason, R. M. 2008. A retrospective and prospective view of orofacial myology. Reprint of The International Journal of Orofacial Myology 31: 5–14. [Google Scholar] [CrossRef]
- Mason, M. R., and W. R. Proffit. 1974. The tongue thrust controversy: Background and recommendations. Journal of Speech and Hearing Disorders 39, 2: 115–132. [Google Scholar] [CrossRef]
- Medeiros, A. M. C., and M. Medeiros. 2006. Motricidade orofacial: inter-relação entre fonoaudiologia e odontologia. São Paulo: Lovise. [Google Scholar]
- Milne, J. M., and J. F. Cleall. 1970. Cinefluorographic study of functional adaptation of the oropharyngeal structures. The Angle Orthodontist 40: 267–283. [Google Scholar]
- Moyers, R. E. 1988. Ortodontia. Rio de Janeiro: Guanabara Koogan. [Google Scholar]
- Overstatake, C. P. 1970. An investigation of tongue thrust swallowing and the functional relationship of deyiant swallowing, orthodontic problems, and speech defects. American Speech and Hearing Association Convention. [Google Scholar]
- Segovia, M. L. 1977. Interrelaciones entre la Odontoestomatologia y la Fonoaudiologia: la deglución atípica. Buenos Aires: Panamericana. [Google Scholar]
- Steps for Radiation Safety in Pediatric Interventional Radiology. n.d.The alliance for radioation safety in pediatric imaging. Available online: www.imagegently.org.
- Sonies, C. B., G. Chi-Fishman, and L. J. Miller. 2003. Ultrasound Imaging and swallowing. In Normal and abnormal swallowing. Edited by B. M. D. Jones. New York: Springer Science Business Media. [Google Scholar]
- Subtelny, J. D. 1970a. Orofacial muscle activity: To train or not to train? Malocclusions, orthodontic corrections and orofacial muscle adaptation. The Angle Orthodontist 40, 3: 182–185. [Google Scholar]
- Subtelny, J. D. 1970b. Malocclusions, orthodontic corrections and orofacial muscle adaptation. The Angle Orthodontist 40, 3: 171–201. [Google Scholar]
- Subtelny, J. D., and A. Sakuda. 1964. Open-bite: Diagnosis and treatment. American Journal of Orthodontics 50: 337–358. [Google Scholar] [CrossRef]
- Tosello, D. O. O., M. Vitti, and F. Berzin. 1998. EMG activity of the orbicularis oris and mentalis muscles in children with malocclusion, incompetent lips and atypical swallowing—Part I. Journal of Oral Rehabilitation 25: 838–846. [Google Scholar] [CrossRef] [PubMed]
- Valentin, J., ed. 2007. Annals of ICRP/International Commission on Radiological Protection Publication. p. 103. The 2007. Recommendations of the International Commission on Radiological Protection 37, 2–4: 1–332. [Google Scholar]
- Van der Linden, F. P. G. M. 1990. Crescimento e ortopedia funcional dos maxilares. Rio de Janeiro: Quintessence. [Google Scholar]
- Yamada, E. K., K. O. Siqueira, D. Xerez, H. A. Koch, and M. M. B. Costa. 2004. A influência das fases oral e faríngea na dinâmica da deglutição. Arquivos de Gastroenterologia 41, 1: 18–23. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, H., and M. Sebata. 1995. Changes in oral functions and posture at rest following surgical orthodontic treatment and myofunctional therapy. The International Journal of Orofacial Myology 21: 29–32. [Google Scholar] [CrossRef]
- Yamaguchi, H., and K. Sueishi. 2003. Malocclusion associated with abnormal posture. Bulletin of Tokyo Dental College 44: 43–54. [Google Scholar] [CrossRef]
© 2013 by the author. 2013 Patricia Junqueira, Milton Melciades Costa
Share and Cite
Junqueira, P.; Costa, M.M. Videofluoroscopy of the Oral Phase of Swallowing in Eight to Twelve Years Old Children with Dental Malocclusion. Int. J. Orofac. Myol. Myofunct. Ther. 2013, 39, 54-68. https://doi.org/10.52010/ijom.2013.39.1.6
Junqueira P, Costa MM. Videofluoroscopy of the Oral Phase of Swallowing in Eight to Twelve Years Old Children with Dental Malocclusion. International Journal of Orofacial Myology and Myofunctional Therapy. 2013; 39(1):54-68. https://doi.org/10.52010/ijom.2013.39.1.6
Chicago/Turabian StyleJunqueira, Patricia, and Milton Melciades Costa. 2013. "Videofluoroscopy of the Oral Phase of Swallowing in Eight to Twelve Years Old Children with Dental Malocclusion" International Journal of Orofacial Myology and Myofunctional Therapy 39, no. 1: 54-68. https://doi.org/10.52010/ijom.2013.39.1.6
APA StyleJunqueira, P., & Costa, M. M. (2013). Videofluoroscopy of the Oral Phase of Swallowing in Eight to Twelve Years Old Children with Dental Malocclusion. International Journal of Orofacial Myology and Myofunctional Therapy, 39(1), 54-68. https://doi.org/10.52010/ijom.2013.39.1.6




