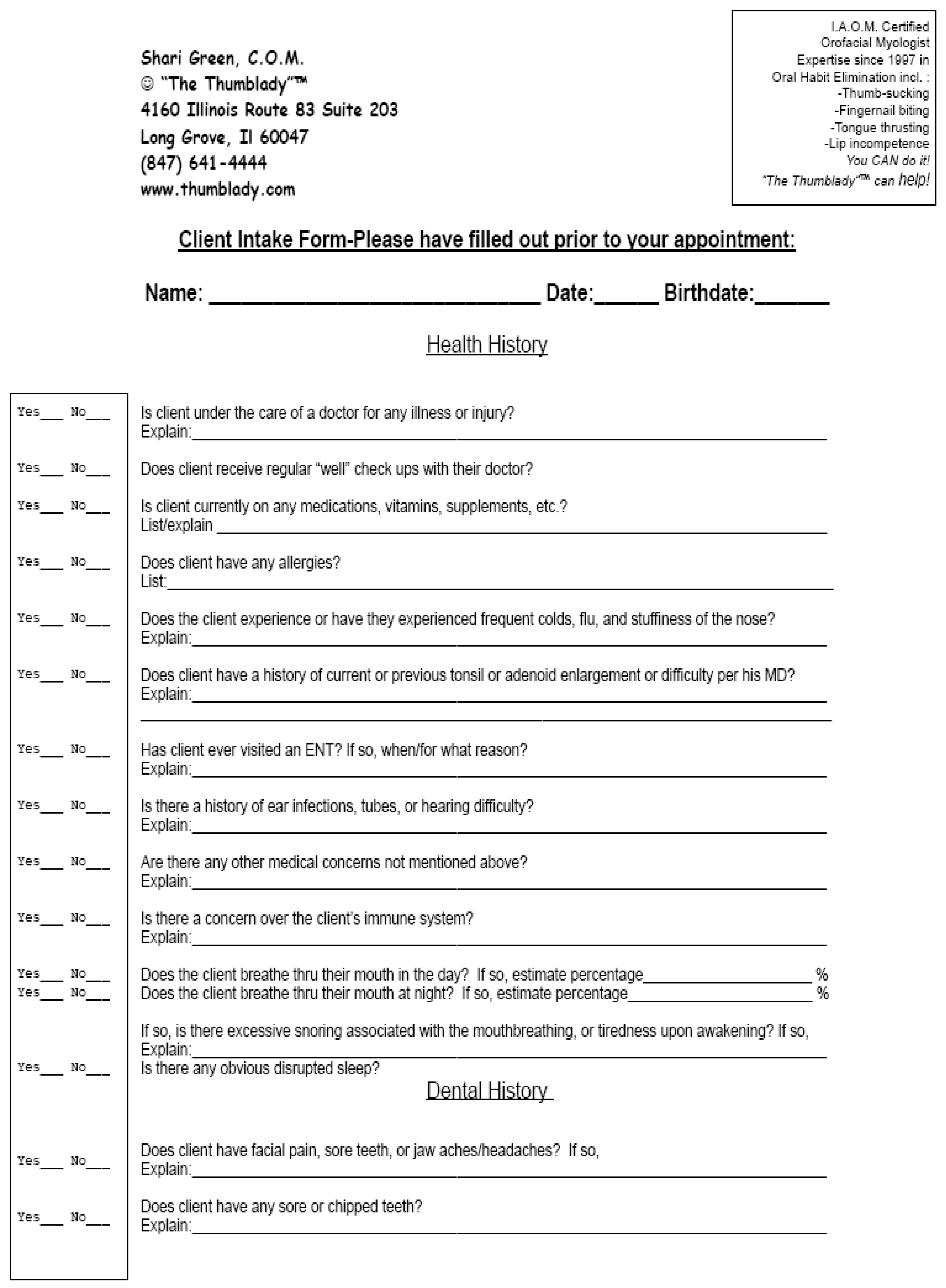
HEALTH HISTORY
The following questions are presented on the Client Intake Form which is provided in
Appendix A. The rationale for each question is dicussed.
Is the client under the care of a doctor for any illness or injury?
One of the initial pieces of information that is important to know about a client is if there are any health issues present that may effect the evaluation or the therapy process. For example, if the child is experiencing a problem with health issues such as tonsillitis, or airway difficulties, the evaluation and the therapy process may be compromised. A child who has physical issues that require other therapies or treatments may impinge on the successful achievement of the goals for orofacial myofunctional therapy and may limit progress.
While the parent is given every opportunity to share this information in written form, a further in-person interview is required. The vast majority of individuals filling out a medical history omit, either by choice or by accident, items that are usually obtained later through the in-person interview. Asking this question in person reiterates the importance of a complete history, and allows the therapist to cover him or herself legally should any future concerns arise that a parent has consciously chosen to omit. Attempting to habituate rest posture and establish appropriate freeway space in the presence of a variety of unidentified challenges would be both inappropriate and unethical.
Does the client receive regular “well” check-ups with their doctor?
Has the child recently been seen by a physician, especially if they present with concerns such as airway, or, learning difficulties? Often, parents only take their child for a check-up when absolutely necessary, and not routinely, due to the recent economy. If they are not currently receiving routine check-ups, this should be noted in their record?
Is the client currently on any medications?
This question will provide a clue to any major health concerns. This question also addresses chronic conditions and their adaptations, such as sensory or attention issues, and timing of any Attention Deficit Hyperactivity Disorder (ADHD) medications in the appointment cycle, seasonal allergy medications that the child is prescribed, and so forth. This question will provide information which may indicate if a child is at risk for emotional concerns. For example, if antidepressant medications are being prescribed by the client’s physician, the therapy sessions may need to be modified. In addition, it is important to recognize that a variety of medications will have the potential to alter the course of therapy, the prognosis, and how the treatment of a particular client is structured.
Does the client have a history of current or previous tonsil or adenoid enlargement or difficulty per his MD?
Perhaps there was a concern that initiated referral by the child's pediatrician, which was determined to be irrelevant by an ENT. For example, a child who presented with significant open lips rest posture and excessive vertical freeway space, and was evaluated by an otolaryngologist. The otolaryngologist may have confirmed that there is no physical reason why this child cannot participate in orofacial myofunctional therapy and expect a good measure of success with their current airway status. In that case, the client may be free to be treated with confidence, given all other aspects of the health history are acceptable.
Does client have a history of allergies?
Allergies are one of the main precursors to OMD. Unmanaged seasonal allergies are a recipe for frustration in attempting to habituate rest posture and establish appropriate freeway space. In addition, any item that a child comes in contact with in your office, has the potential to put the child at risk and the therapist in harm’s way. Is the child allergic to food coloring? Peanuts? Latex? A variety of common substances can trigger an allergy concern in your office, and have the potential to make a child extremely sick.
Has client ever visited an ENT? If so, when, and for what reason?
The fact that a child has visited an ENT for some issue is a red flag. Is this issue being aggressively attended to? Are they “under control”, or is there surgery looming either immediately or in the long term. For example, if the child has seen an ENT for a deviated septum, if they are young, no immediate surgery may be imminent until age 18. How are you going to approach habituation with this challenge? If they have been diagnosed with enlarged tonsils, but have chosen not to obtain surgery, what are the possible ramifications, and what is the outlook for long term tongue thrust or tongue rest posture remediation? How can the patient be educated about the potential impact of these concerns, and provide the therapy in the most timely and appropriate manner so that the best standard of care can be expedited? Perhaps the decision will be to postpone therapy due to a poor prognosis. However, the health history information must be utilized to help the family make an informed decision regarding the realistic expectations of treatment for orofacial myofunctional disorders (OMD).
Is there a history of ear infections, tubes, or hearing difficulty?
Eustachian tube issues, and in particular, otitis media, have a long-standing relationship with OMD. In fact, the vast majority of our clients answer “yes” to this question. Client’s have often experienced recurrent difficulty with ear infections.
Does the client experience or have they experienced frequent colds, flu, and stuffiness of the nose?
A history of airway difficulties is often highly associated with orofacial myofunctional issues. This question allows us to open a dialogue to assess if the child is currently a good candidate for OMT, such as when an intermittent and manageable condition is present, vs. a more significant issue that may require immediate attention by their physician.
If a child is currently ill with a virus, it will potentially alter the initial paperwork and findings assessment. If a child is prone to illness, habituation will be difficult, but let us not dismiss the consideration that perhaps a mouth breathing habit has made them more prone to illness. Both occurrences remain debatable concerns.
Are there any other medical or learning/processing concerns not mentioned above?
This is the most common misanswered question in my practice. Parents are often afraid their child will be "labeled", are not aware of an actual "name" for their child's challenge, or just feel it is not significant. I disagree. If a child is a visual learner, I want to know. If they will listen better with a reward system, have difficulty with eye contact, require written rather than visual cues or assignments, have difficulty with verbal processing, it is critical that the therapist know so that adaptation can be initiated. And, it is critical in treatment planning and expectations.
Does the client breathe thru their mouth during the day? If so, estimate percentage __________________%. Does the client breathe thru their mouth at night?
Habitual mouth breathing is often a sign of either an airway issue, a tonus issue, a neurologic concern, or an issue of misinformation on how to correctly rest one’s oral cavity. Knowing this percentage helps to set a baseline for later exploration or possible referral should the correction of the habit be limited by the structure or health status of the child.
If so, is there excessive snoring associated with mouth breathing, or tiredness upon awakening?
Snoring is often an indication of a history of concerns such as enlarged tonsils, poor tongue posterior tonus, or narrowed arch form. Recent research confirms that the use of rapid palatal expansion (RPE) to correct a narrow arch in sleep disordered children often leads to self-correction of disordered breathing cycles in select patients with obstructive sleep apnea (OSA) (Cistulli, Palmisano, Poole, 1998; Villa, Rizzoli, Miano, Malagola, 2011). An indication of a positive response to this question may warrant further exploration should the child experience the symptoms of sleep disordered breathing. Often, orofacial myologists are the first to ask this question. We are not diagnosing an issue, but reporting responses. It would be impractical to expect a child to habituate night postures under these circumstances, and unethical not to open a dialogue since orofacial myologists teach proper night rest postures of the oral cavity.
Is there a concern over the client’s immune system?
An individual with a challenged immune system may be more prone to infection, and thus have a history of increased mouth breathing and upper respiratory concerns. An individual with immune deficiencies, such as Auto Immune Deficiency Syndrome (AIDS) may present with multiple airway concerns. In addition, although orofacial myologists are expected to promote a high level of asepsis, and adopt universal precautions, it is even more significant that every effort be made to protect both the clinician and others with appropriate aseptic procedures so as to avoid cross contamination of hard surfaces and all aspects in relation to the treatment area.
DENTAL HISTORY
Does Client have facial pain, sore teeth, or jaw aches/headaches? Sore/chipped teeth?
If there is any report of pain, it may require significant adaptation of exercises, the therapeutic process, treatment planning, or necessity for referral. For example, in a client who experiences a temporal mandibular joint disorder (TMD), adapting exercises to either a lower number of repetitions, divided sessions, or omission of exercises that may aggravate symptoms may be crucial. It may take more appointments to complete therapy, which may need to be done at a slower pace and more conservative pace and approach. Resting between exercises and correct pacing of activities will prove useful for many clients to gain a slow and steady remediation result.
For example, any sore or chipped teeth may require modifications, such as the straw exercise adaptation, sticks for isolation on the opposing side. Chipped teeth may be a potential issue as the tongue may wish to stubbornly remain within the open space created by partial tooth loss, which may require referral for reconstruction prior to therapy.
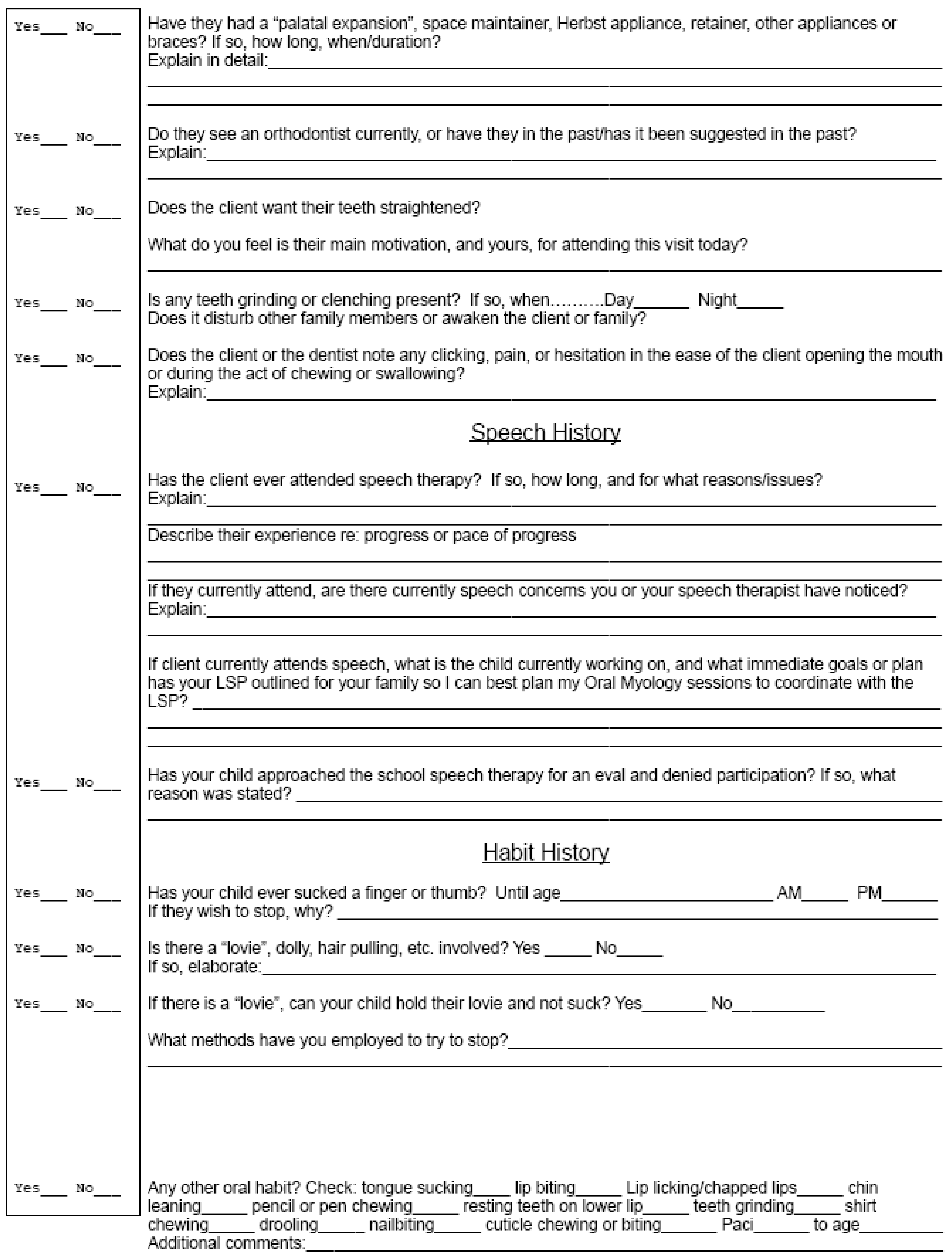
Have they had a palatal expansion, space maintainer, Herbst Appliance, retainer, or other appliances or braces? Do they see an orthodontist currently, or have they in the past/has it been suggested in the past?
The client’s orthodontic history is explored in detail. This information helps to determine what the growth and development path may have been from early childhood (palatal expansion), i.e., was the client previously vaulted and was vertical growth an issue due to a variety of concerns, and/or does the client favor one side for mastication, or have increased lingual lateralization, muscular jaw lateralization patterns, due to a previous posterior crossbite.
It is important to know if there has been early tooth loss (space maintainer) and why, i.e. neglect, missing teeth, early extraction patterns with failure of new dentition to erupt into a space. Was there a reduced mandibular arch width or a retruded mandible which may have lead to compensatory behaviors? Is a retainer currently in place that is lacking sufficient anatomical detail which may cause the client to misjudge rest posture? Can a simple adaptation by the dentist be placed, such as a spot dot, to improve the recognition of anatomical landmarks on the appliance? Is there a history of a “tongue thrust” appliance that did not remediate the tongue concerns, or serve to create accessory tongue behaviors and compensation that must now be dealt with in OMT or in conjunction with speech therapy? Is there a retainer being worn, that despite consistent usage is not assisting the dentition in retaining the client’s optimum completed bite? If they are currently in treatment, the length of treatment without expedient bite closure, for example, may be a concern.
Does the client want their teeth straightened?
If they DON’T want their bite improved, how apt are they to participate willingly in the therapy process? What is their dental I.Q.? How can we educate this individual about the benefits of long term orofacial myofunctional disorders remediation and a properly aligned bite, so as to best motivate them to want to work hard in the therapeutic process?
What do you feel is the main motivation for attendance?
Use the child’s motivation to gain compliance. Are they motivated by a beautiful smile? Are they motivated by clear speech that is so often naturally attained when tongue postures and patterns improve? Would the client be proud to be less noisy while eating and dispense with embarrassing drooling or tongue protrusion? Use this to help motivate the client to succeed!
Any teeth grinding or clenching? Does it disturb others?
Orofacial myologists are the keepers of the freeway space. Clenching and grinding, in addition to causing trauma, and wear on tear on the orofacial complex and dentition, does not allow proper rest posture. Perhaps a referral is needed. Perhaps multiple behavior modification techniques can be instituted early in the treatment program. And, if the grinding or clenching of teeth is so loud that it disturbs family members, the referral source needs to know.
Does the client or dentist note any clicking, pain, or hesitation in the ease of the client opening the mouth or during the act of chewing and swallowing? Once again, is orofacial mobility affected? What exercises or adaptations to our therapy would be appropriate and when is it appropriate to refer?
SPEECH HISTORY
Has the client ever attended speech therapy...if so, how long...what sounds or issues?
Pierce (
1996) reported findings on 100 tongue thrust clients, noting 50% demonstrated articulation issues. A history of lengthy speech therapy is a tip off to many concerns. Are there developmental delays or language concerns that require adaptation to our treatment plan? Are the common sounds that are affected in tongue thrust/retained digit sucking habits coincidentally the sounds that this individual struggles with? (S, Z, N, T, D, L, SH, J, CH, B, and R) (
Green, 2010). A child who fails to advance in speech at an expected rate often cannot meet their IEP goals due to the tongue thrust and rest posture patterns that encourage inappropriate speech sound production. This is a huge motivation for many children and families to attend OMT.
Has your child approached the school speech therapist for an eval and was denied participation? If so, what reason was stated?
This is mainly a demographic question. Many school districts are emphasizing learning skills over articulation therapy, and local school speech therapy departments are depending on the private sector to provide more specific treatment in articulation skills. As this number grows, more awareness of orofacial myofunctional disorders may follow.
Many parents may be frustrated with the challenge of this change in the system and come to the orofacial myologist’s office with this history of concerns. Parents seek not only expedient and targeted treatment to build the oral muscular base necessary for speech so their child may attend future speech therapy, but often come to the orofacial myologist for confirmation of the existence of an actual and true orofacial myofunctional issue.
HABIT HISTORY
Has child sucked a finger or thumb? Until age ____. A.M.? P.M.?
One of the main contributors to sustained tongue thrust swallow pattern and low rest posture of the tongue, beyond the developmentally appropriate ages of 4 to 6 years old, is a retained digit sucking habit. If the client is attending an initial visit to address a digit sucking habit, it is imperative to know WHEN the habit is occurring, so that treatment and reminders can be utilized appropriately. If the client is attending for a tongue thrust behavior pattern, it is crucial to eradicate the digit habit prior to addressing the tongue thrust. Attempting to aggressively treat a tongue thrust or inappropriate rest posture in the presence of a digit habit is unethical and frustrating.
If they wish to stop, why?
Finding out your client’s main motivation for wanting to stop is empowering. For example, if the client has been sick with multiple bouts of colds, flu, and the pediatrician has suggested the thumb may be related to the frequent illnesses, this concern may be a powerful tool that may used to motivate the client to stop the thumb habit.
If the client is being teased, it could indicate a self-esteem issue or bullying that may be affecting the child in school, socially, or internally that may need to be addressed by the parents, school, or other professionals should the problem exist past remediation of the habit. This information will also encourage the clinician to praise the child and recognize or affirm their accomplishments frequently throughout their treatment. This truly can change a child’s life. If a parent states the child has no desire to stop, it is imperative the parent be educated that a child cannot be “forced to quit”, as some motivating factor must be the impetus to stop, along with the enthusiasm of the orofacial myologist with a well-prepared plan of action.
Is there a lovie? Doll? If so, please elaborate. Can your child hold their lovie and not suck?
A lovie (i.e., item of chained attachment such as a blanket, doll, etc.) may be a trigger for more sucking, or it may be neutral. It is the job of the orofacial myologist to determine the status of the lovie and address if it is chained or not. This “chained” lovie then becomes a crucial link in therapy. Addressing the lovie may entail full elimination, minimizing exposure, or teaching alternate behaviors that “unchain” the lovie from the sucking process.
What methods have you employed to try to stop?
Most parents have employed a combination of positive and negative strategies prior to visiting the orofacial myologist’s office. If there were positive strategies offered, most likely there will be some that they have already utilized that the orofacial myologist plans to employ as well. This helps open a dialogue to inform parents that sometimes it is not so much the scattered technique used, but rather the consistency and the third party that makes the difference between success and frustration.
Are there any other oral habits? (drooling, paci, bruxing, baby bottle, etc.)
Again, there are a variety of early childhood habits that contribute to sustaining orofacial myofunctional disorders. Addressing these habits is crucial to success. If the child had a baby bottle, for example, for 36 months, this could impact their orofacial myofunctional status. If they have a nail biting habit, this may impact rest posture significantly. If there is a bruxing issue, addressing and educating the client about proper freeway space and oral rest postures is crucial to long term correction of OMD. Drooling often indicates difficulty a client has sucking back saliva, and the fine coordination needed to accomplish this action by utilizing proper vertically based tongue behaviors, and which may also involve the buccinator and/or the obicularis oris, and/or mentalis compensatory activities.
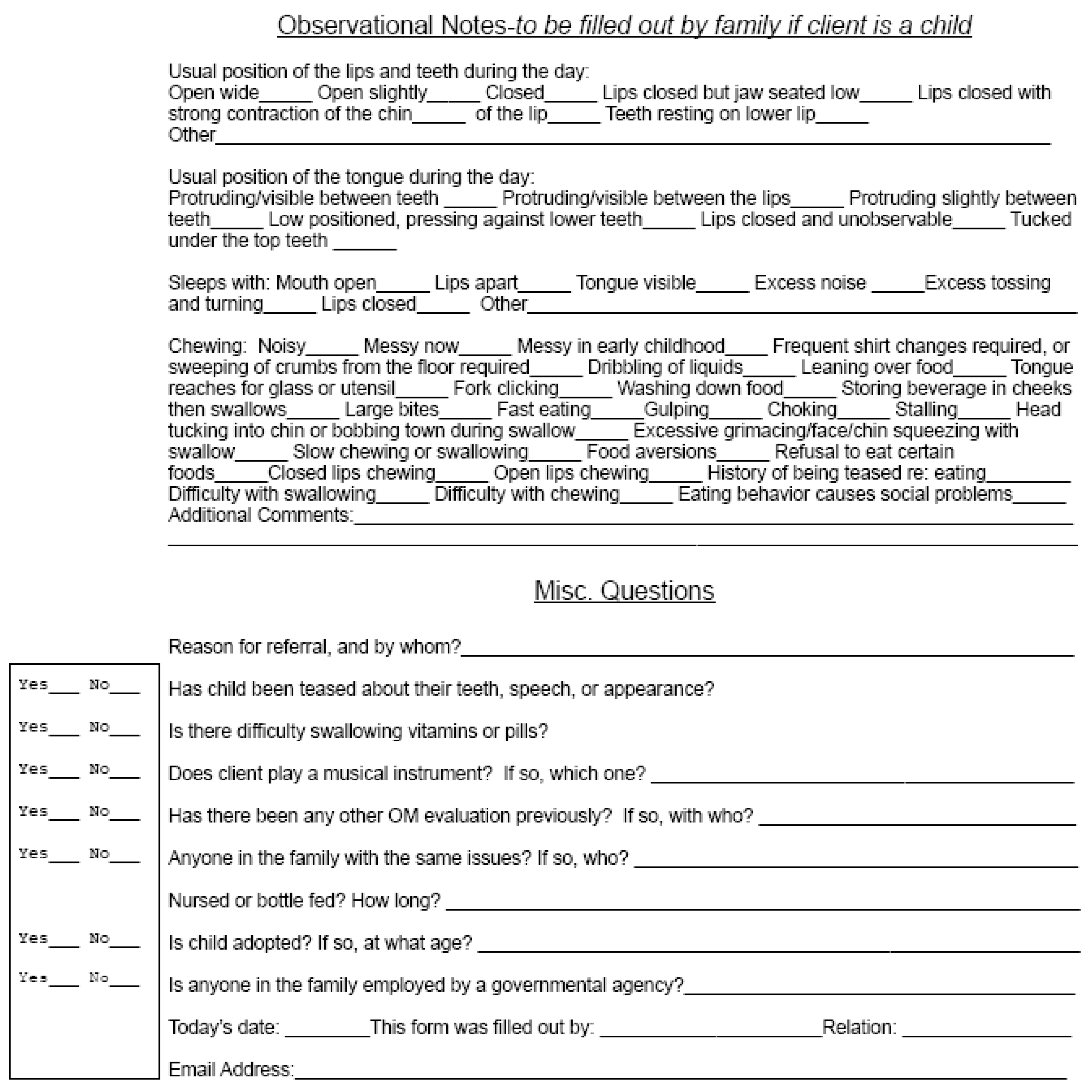
OBSERVATIONAL NOTES
Usual position of the lips and teeth during the day/Usual position of the tongue during the day.
The client is often aware that their tongue is “pushing on their teeth”, or that it is resting outside of their mouth. Often a family has never thought about this issue. This opens a dialogue in which key information is provided regarding what is most appropriate when compared with the actual activities being demonstrated. It also “plants the seed” so the parent may begin to observe their child’s behaviors so they can monitor improvement as therapy begins.
Sleeps with ....
Sleep posture is a subject of much controversy. However, it is never normal for a child to awaken frequently or suddenly night after night. New research (Villa, Rizzoli, Miano, Malagola, 2011) points to the relationship between disrupted sleep and narrow palatal arches, and their role in growth and development. In addition, a child who sleeps on one side habitually may develop altered tongue lateralization issues, symmetry concerns, and have difficulty maintaining proper night rest postures. Sleep posture in which an individual prefers to sleep face down directly into the pillow may be associated with an increased propensity for TMD, cervical concerns, or breathing concerns. Proper ergonomic night postures will perpetuate proper tongue, lip, and jaw rest postures as we near habituation.
Chewing (Food Behavior):
Masticatory and swallow habits are often a huge concern for parents, and often the most highly motivating factor encouraging parents to seek OMT for their children. A child who limits textures, gags, chokes, is noisy, shovels, or washes down food or uses other multiple compensatory behaviors is common in an orofacial myofunctional practice.
In addition, although many parents are aware there are “some” problems, most are not aware of all the issues, and under report observations in this section. This is an opportunity to “nicely” point out the intricacies of food behavior often seen in OMD, and how these activities may encourage the perpetuation of low rest posture, poor vertical utilization patterns, and on occasion, the incidence of choking.
Has child been teased about their teeth/speech/appearance?
The appearance can play a key role in motivating a client to want to pursue successful remediation of an OMD. The open lips rest posture, along with the bite concerns and speech irregularities that often follow can create social and self esteem issues that most teens, for example, would be willing to work hard to improve. This can be a strong motivator, as many of these issues may resolve either directly, or indirectly, as a result of therapy.
Is there difficulty swallowing pills?
Poor pill swallowing skills often indicate a poor posterior lift, difficulty with gathering, and vertically based initiatives. It suggests coordination issues between gather and swallow. This issue often resolves as therapy progresses.
Does client play a musical instrument? If so, which one?
In many cases, improper musical instrument choice or techniques can contribute to OMD. Poor playing ability may signal the presence of an OMD. They may also be beneficial, if chosen wisely. A client who displays difficulty with lip closure, for example, could benefit from playing certain instruments (trumpet, French horn).
Has there been any other OMT evaluation previously? If so, with who?
Has the client attended sessions previously and been unsuccessful? Why? Was there a failure to aggressively address allergy or tonsil concerns, timing, poor attitude, or other possible intervening variables?
Is there anyone in the family with the same issues? If so, who?
This is often more common than we may realize. A parent with severe allergies (respiratory), for example, may be a clue to the etiology behind a child’s OMD.
Who referred you to my office?
Of course, this is critical to allow free flow of information and communication. Release of information is obtained at this time as per HIPPA regulations.
Is child adopted? If so, at what age?
A child who had a poor start in life, for example a child who may have spent several years in an orphanage with limited resources, may have encountered challenges in that environment that would lead to nutritional issues, developmental concerns, unattended health concerns, when compared with a child who has been provided a more positive adoption experience. The child may have sucked a digit out of boredom or hunger for the majority of their day, instead of being provided with a more positive experience of attention, adequate and optimum nutrition, and access to medical care of an expedient nature.
Signature/Date
All forms must be dated and signed.