Abstract
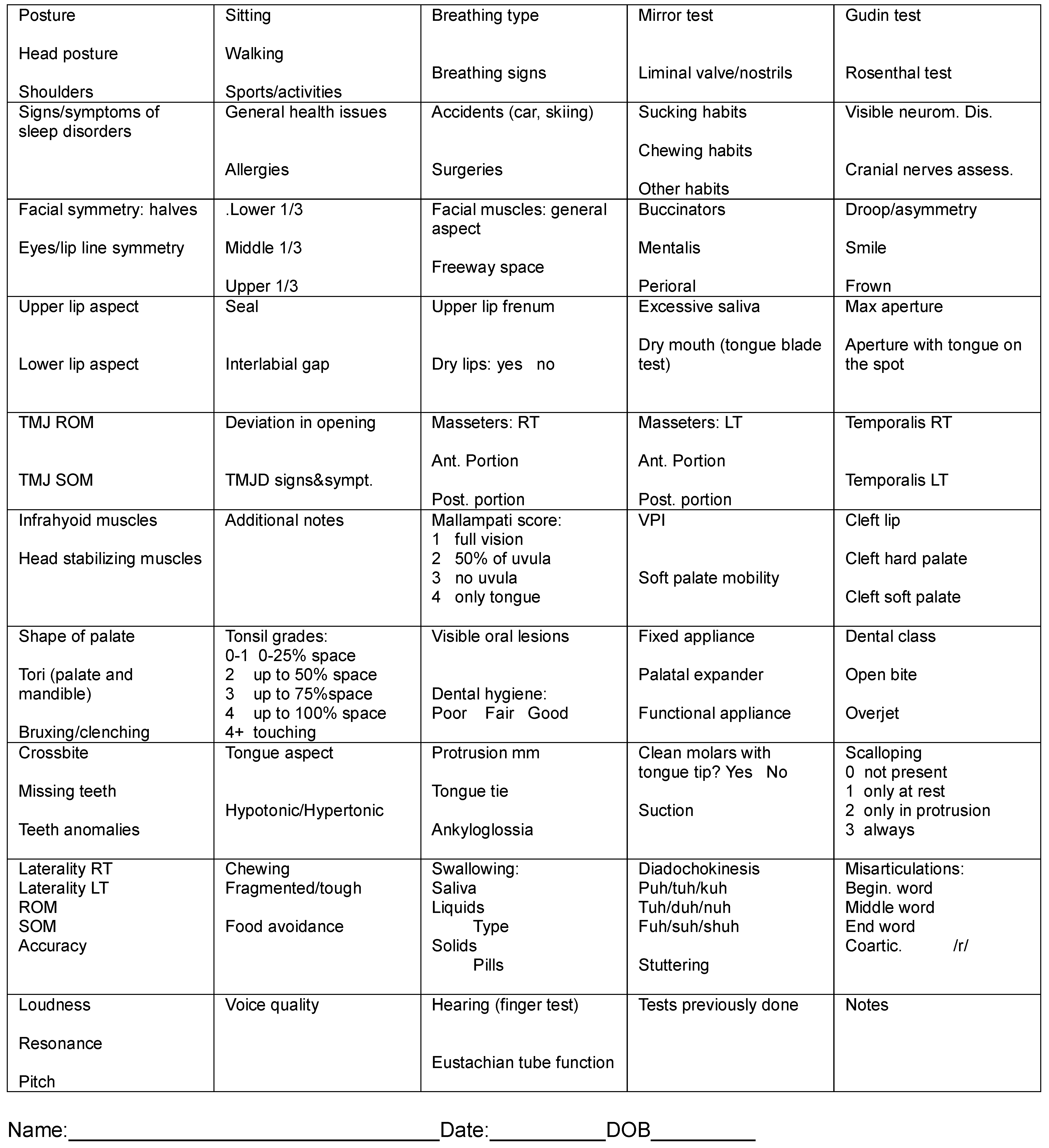
The author presents her own proposal of a one-page orofacial myofunctional assessment and for each item on the list a brief rationale is provided. The protocol is an easy but comprehensive form that can be faxed or emailed to referral sources as needed. As science provides more objective assessment and evaluation tools, this one-page form can be easily modified.
INTROUCTION
Although our professional world is increasingly computer driven, there are certain advantages to paper and pen assessments. The proposed form tries to capture the most common aspects of a patient assessment without excessive details that can be left to the overall intake conversation, and it’s also simple enough to allow constant revision and incorporations of new items. This one-page assessment form is meant to hold quick and short notes, such as: within normal limits (WNL), within functional limits (WFL), dysfunctional or disordered (D), range of motion (ROM), strength of motion (SOM), accuracy of motion (AOM), increased (INC), decreased (DEC) and whatever else is needed. When the assessment requires further explanation an asterisk is placed in the corresponding box and a separate note is made.
Although this assessment protocol (Appendix A) is meant for orofacial myologists with a speech-language pathology background, it can be easily modified to assist dental professionals, cranio-osteopathic physicians, occupational therapists and others. However, every state (or nation) and every professional and licensing board has different requirements and restrictions with regards to the various sections of the evaluation. This specific assessment form was prepared in compliance with the laws of the State of California and in compliance with the American Association of Speech-Language and Hearing (ASHA) (ASHA, 1991 & 1993) and the standards of the International Association of Orofacial Myology (IAOM).
The assessment protocol, in its present form, was inspired by the Interdisciplinary Orofacial Examination Protocol for Children and Adolescents (Donato, Lapitz & Grandi, 2009; Echarri et al, 2009) form used by Diana Grandi and her team at the College for Speech-Language Therapists of Catalonia, Barcelona, Spain and by the MGBR Protocol (Genaro et al, 2009) used at CEFAC in São Paulo, Brazil, by Irene Q. Marchesan, PhD and by her team of multidisciplinary professionals.
ASSESSMENT PROTOCOL DISCUSSION
The assessment protocol begins with the general observation of the patient walking, sitting in a chair and standing. In a normal head posture position the ears should be lined up with the middle of the shoulders. This is important because the life-long complications of a forward head posture at rest and while walking are well documented (Korbmacher, Koch & Kahl-Nieke, 2005; Okuro, Morcillo, Oliveira Ribeiro, Sakano, Margosian Conti, Ribeiro, 2011). Slouching in the chair and a lack of any regular physical activity should also be noted on the chart, because correcting the orofacial myofunctional disorders (OMD) in a patient might not be successful without placing those disorders in a much larger context of proper posture (Miles, 2007; Mathur, Mortimore, Jan, Duglas 1995).
However, diagnosing and treating postural problems is not in the scope of practice of US-based orofacial myologists. Fortunately, in many countries the posturologist is an intrinsic member of the orofacial management team, along with the orthodontist, the otolaryngologist (ENT) and the orofacial myologist. In the US, if the forward head posture is significant, a consultation with and/or a referral to a physical therapist may be helpful.
Next, the type of breathing is assessed by direct observation, to determine if the breathing is primarily either “clavicular” or “abdominal” (often referred to as “diaphragmatic”). Upon inquiry, some patients may report breathing signs like sighing or shortness of breath during or after eating or during speech. The nostrils aperture is noted (liminal valve) as per the Multidisciplinary Protocol (Donato, Lapitz & Grandi, 2009; Echarri, Carrasco, Vila, Bottini, 2009) and three tests are performed if needed: the Rosenthal breathing test for minimum breathing endurance, the Gudin test (or the “sniff” test) for flaring of the nostrils and the nasal mirror test for patency of the nasal cavities (Garretto, 2003 and 2005).
When the nasal passages seem to be somewhat restricted or compromised, an inquiry into sleep disorders is warranted, as sleep disorders are potential life threatening conditions (Barsh 1998, Bonuck, Freeman, Chervin, Xu, 2012). Apart from known signs and symptoms of sleep disorders such as: Mallampati score 1 or 2, hypertrophic tonsils and/or adenoids, scalloped tongue, increased body-mass index (BMI), neck circumference, or retrognathic mandible, (Guimarães, Drager, Genta, Marcondes, Lorenzi-Filho, 2009; Coceani, 2003; Li, Wong, Kew, Hui, Fok 2002; Weiss, Atanasov & Calhoun, 2005), the positive findings in the Epworth Sleepiness scale (available through www.stanford.edu) and individual reports are added to the overall assessment in order to decide if the patient needs to be referred back to his treating physician or dentist, to determine whether or not a sleep study is warranted.
In the box reserved for general health, notes are made about chronic conditions (not allergies, which have their own box) such as diabetes, Crohn’s disease, or autism. In addition, conditions such as cancer (current and past chemo and radiation therapy) are also noted, since each disorder may require modifications to the therapy style, tools and procedures.
Special attention is given to known allergies but also to tale-tell signs such as: “allergic shiners” or dark areas under the eyes, “allergic salute” or wiping the nose with the hand, stuffy nose, runny nose, red eyes. Identifying allergies is relevant to the evaluation process as flare-ups may impact therapy and orofacial posture habituation. If medications are already being taken by the patient, but strong symptoms still persist, then questions about compliance, diet modification or environmental modifications should be asked. However, because consulting on a hypo-allergenic diet is not within the scope of practice of US-based SLPs, patients are usually referred for all their additional needs back to the referring physician and for additional information to science-based educational websites such as mayoclinic.com, webmd.com, health.gov, health.harvard.edu and others.
This specific assessment form notes any past accidents, mostly those related to injuries of the head and face but also to the legs and back to identify possible starting points of compensatory postures or behaviors. Significant surgeries are mostly those to the head and face or oral cavity (like avulsion of wisdom teeth or tonsillectomies) but also surgeries that could impact orofacial or breathing functions, like abdominal surgeries resulting in scars affecting the breathing pattern or significant back surgery as they affect posture and trigger compensatory positions and functions.
Next, a specific box allows for a quick inquiry into any orofacial habits, such as thumb and finger sucking, chewing habits, leaning on one’s hand (Miyake, Ohkubo, Takehara, Morita, 2004), lip licking, tongue sucking or cheek biting. The current frequency, duration and possibly intensity of the habits are also noted, along with an approximate starting date in years or months for that habit.
In cases of suspected or medically diagnosed disorders such as Parkinson’s or Multiple Sclerosis or Cerebral Palsy, a note is made if the disorder is affecting jaw stability, chewing, swallowing, breath control or speech. In selected patients (those who have or might have a neuromuscular disorder or are stroke survivors) a quick assessment of the cranial nerves and their symmetry is done: asking about the sense of smell (CN I), ability to react to light (CN II), track a finger or a light point in all directions (CNs III, IV, VI), face sensitivity and biting (CN V), facial expressions (CN VII), finger rubbing test (CN VIII), soft palate movement (CN IX), voice (CN X), shoulder shrug (CN XI) and tongue waggle (CN XII). This protocol can be easily found in neurology books or websites.
In patients who present perceptual asymmetry of the face, especially in those with habitual mouth open/mouth breathing (Bresolin, Shapiro, Shapiro, Dassel, Furukawa, Pierson, Chapko, Bierman, 1984), it is useful to quantify such a finding, by taking a full frontal picture or a freeze frame from a video to analyze the two halves of the face (such as in the case of habitual unilateral chewing) and to measure the line linking the corners of the eyes versus the line linking the corners of the mouth. Such lines should be parallel and often in OMDs, these lines are not. However, therapy can positively influence these measures. A quick measurement of the 3 thirds of the face can also be useful, as therapy might influence the dimension of the lower one third. The measurements are taken between menton and nasion, nasion and glabella and glabella and trichion. For further details, please refer to Paskay, 2006; Scarborough, Ghali & Smith, 1997; Quintal, Tessitore, Rizzoato Paschoal, Nizam Pfeilsticker, 2004; Proffit & Fields, 1986; Ferrario, Sforza, Poggio, Tartaglia, 1994.
The assessment should include a general overview of the facial muscles, including the eyes (semi-closed or wide open) and the forehead (furrowed at the glabella, wrinkled) as possible signs of stress, pain or compensatory use of facial muscles to support and stabilize the mandible. If the freeway space is clearly excessive or reduced, the space can be measured (Mason, 2005) and listed in this box. The ability of “blowing one’s cheeks” should be an indication of the functionality of the buccinators and the perioral muscles in general, while the mentalis should be relaxed and not “bunched up”. Droops and asymmetry in facial movements can be evaluated by having the patient smile or frown.
The lips are assessed next and the shape of each lip is noted to see if either one deviates from the “norm”; which is racially determined. The rationale for this note is that lips can be modified by growth and development (Vig & Cohen, 1979), therapy (Meyer, 2000) and also by atypical breathing conditions (mouth breathing) or surgeries (cleft lip or lip injury). The loss of integrity of the orbicularis oris should be noted as it may affect the therapy results (Carvajal, Miralles, Cauvi, Berger, Carvajal, Bull, 1992). The range of motion (ROM), strength of motion (SOM) and accuracy of motion (AOM) can be listed here. Within Functional Limits (WFL) indicates lip movements that, although not “normal” or optimal, still accomplish the task nonetheless. For instance, although the patient might not be able to properly pucker or frown his or her lips on command or in imitation, they do not lose liquids or food as they eat, so their lips are still functioning although not at an optimal level.
The presence or absence of labial seal is noted and when a gap between lips is present, its dimension is also noted. This measure is very important to orofacial myologists because lip seal can be achieved through therapy (Satomi, 2001). Lifting the upper lip reveals the length and thickness of the labial frenum and if it’s too thick it may not only contribute to the presence of a diastema but also prevent a proper lip seal. Dry lips are documented because they can suggest a generalized dehydration, which itself can cause drowsiness and confusion in children and elderly patients, but dry lips also stimulate bad oral habits like lip licking, thumb sucking, lip sucking or lip wedging (lower lip between upper and lower teeth in a severe overjet).
A note is made as to the quantity and quality of saliva. If the saliva pools white and foamy at the sides of the mouth then there is an obvious change in both the quality and quantity of saliva. Mavash Navazesh, PhD wrote in several articles for the Journal of American Dental Association (JADA) that the term “xerostomia” indicates qualitative and quantitative changes to the saliva. In this assessment chart, presence of excessive salivation (scialorrhea or drooling) is noted, as well as “dry mouth” by the patient’s own admission and by pressing a wooden tongue depressor against the internal surface of the cheek. If the tongue depressor sticks then the salivary output is already 50% or less of what it should be (Navazesh, 2003). A positive tongue depressor test, especially in adults, should be followed by an inquiry into medications that might cause a reduction in salivation. The rationale to investigate, in greater detail, the production of saliva is because saliva affects speech (and/or oral health), chewing, and swallowing which are within the myofunctional purview. Also, noting changes in saliva triggers inquiries into sleep habits and sleep disorders. According to a 2012 article by Joseph Shames, DMD (in press), oral saliva is part of a liquid film that extends from the oronasal cavities to our stomach and beyond and a dry mouth seems to be linked to sleep disorders by increasing the surfactant tension of the oral soft structures that collapse and stick together during sleep.
The maximal aperture of the mouth should be measured with a caliper or a ruler and noted on the chart, always using the same teeth as references. When the opening is between 35 mm and 50 mm it’s defined as WNL, if it is less but the patient is still able to eat fairly well, it is WFL. An aperture greater than 50 mm may indicate an articular laxity, which does not affect the work of an orofacial myologist but should nevertheless be noted on the chart. A second measurement is taken with the tip of the tongue on the retro-incisal papilla to measure the functional measurement of the lingual frenum. According to the Marchesan protocols (Marchesan, 2004, 2005 and 2010) for lingual frena (tongue-tie), if the second measurement is less than 50% of the first measurement, then surgical “release” of the frenum should be considered. If the second measurement is between 51% and 59% of the full mouth opening, then the case is “borderline” and some stretching exercises could be considered to repattern the tongue. Anything above 60% is considered WNL. A lingual frenum attached to the tip of the tongue is considered a true ankyloglossia for which a surgical consultation is warranted.
Because of all the connections between tempomandibular joints (TMJ) and breathing, chewing, swallowing, and speech, a gentle assessment of the ROM and SOM of the jaw offers an insight into the integrity of the TMJs (Goncalves Bianchini, 2000; Rodrigues Correa & Berzin, 2004; De Felicio, Melchior & Da Silva, 2010). The ROM is tested by asking the patient to move the jaw in antero-posterior, right-left and vertical (mouth opening) directions. Questions about biting apples, hamburgers or simply eating soup with a spoon may gain some insight into the adequacy of the mouth opening during feeding. It is important to note if the patient can move the mandible without a teeth assist, with a teeth assist or with a tongue depressor assist. The strength of motion is considered at least WFL if the patient is able to chew most foods. If the patient reports significant impairment in the chewing ability then a referral to the treating orthodontist or TMJ specialist is warranted. However, some patients might be sent to orofacial myologists by surgeons after maxillofacial surgery, or by TMJ pain management specialists, in cases where the TMJs have already been assessed, to be treated in a multidisciplinary fashion and the plan of care has been discussed and approved by the TMJ specialist. In this case a gentle passive opposition to the opening of the mandible, the lateral movement and antero-posterior movement along a tongue depressor may indicate the SOM of the mandible. The ability to chew increasingly “tough” foods is also an indication of the SOM of the TMJ.
Since not every patient is referred to the orofacial myologist by an orthodontist or a dentist, asking a patient to gently open the mouth as wide as possible (but without pain or discomfort) allows the clinician to note the presence of a lateral, ‘S’ shaped shift of the mandible, suggesting problems with the TMJ meniscus that might warrant a consultation with a dentist, orthodontist or a TMJ specialist. Signs and symptoms of TMJ disorders should be noted and a consultation or a referral needs to follow. Signs and symptoms (according to mayoclinic.com and webmd.com) are: popping or grinding noises, impaired functions (mouth open or closed), pain, discomfort, headache, neck ache, shoulder ache. A stethoscope could be used to listen to noises coming from the TMJ and, by gently pressing a finger against the patient’s external ear, it’s possible to feel the asymmetric movement of the TMJs.
Unlike the facial muscles, the masseters have an important role in the stability of the mandible because they have a stretch reflex (Scutter & Turker 2001; Miles, Flavel & Nordstrom, 2004; Goulet, Clark & Flack, 1993). Therefore assessing their tone and activation timing (they should activate almost simultaneously), gives an indirect indication of the condition of posterior occlusion, therefore chewing capabilities. The activation of the anterior vs. the posterior portion indicates the specific extent or absence of an adequate occlusion. The infrahyioid muscles (below the hyoid bone, antagonistic of the chewing muscles) are tested by opening the mouth wide. The temporalis are also palpated while the pterygoids are not directly assessed because of their location, but indirectly assessed by the lateral excursion of the mandible. Tension to the head stabilizing muscles (the posterior neck muscles, especially when coupled with a forward head posture) is an indicator of possible compensatory positions, strain and muscle pain which may complicate therapy. The tongue at rest is in different positions when the head is not properly aligned and the neck muscles are tense. For additional information on muscle testing please refer to Camargo Tanigute, 2005; Hanson & Mason 2003; Queiroz Marchesan 2005.
The Mallampati score is useful in identifying patients more likely to have a tongue thrust and sleep disorders (Guimaraes et al. 2009). Although the traditional Mallampati is assessed with the mouth fully open and the tongue sticking out, several “modifiers” have been added in the last few years, such as the tongue sticking out with/without maximum extension, with/without phonation (aahh) (Mallampati, Gatt, Gugino, Desai, Waraksa, Freiberger, Liu, 1985; Samsoon & Young, 1987).
Speech-language pathologists should note any type of cleft, repaired or not, including fistulas, their position and their extent. The type and severity of velopharyngeal incompetence, insufficiency or inadequacy (VPI) should be noted (Peterson-Falzone, Harding-Jones & Karnell, 2009). If possible, this information should be coupled with objective data and reports from referring doctors or care team members. A VPI can be the temporary result of adenotonsillectomy, a more common occurrence in speech and dental practice. Additional genetic anomalies should be noted, like skin tags or auricular fissures, as they are part of a larger issue that might impact therapy. The mobility of the soft palate should be noted as well by pretending to gag with the mouth wide open or by saying “ah”.
The shape and appearance of the palate should be noted, either subjectively or by measuring the space between the lingual cusps of the first upper premolars. It could be inadequate for orthodontic needs but WFL for tongue suction and tongue placement. Any exostosis, torus palatinus and mandibular tori should be noted. They are bony growths that can impact tongue rest posture, chewing and swallowing. Because tori are often linked to bruxing and clenching (and genetic predisposition), an inquiry can be made about these habits, if they are not already mentioned in the patient’s dental report.
Although tonsils and their evaluation should be left to the ENT, in order to properly document a referral or justify a delay in myofunctional therapy a rough tonsil grading is appropriate (for grading of tonsils please refer to Harley, 2002). Again, it’s a mere description of the visible tonsils on assessment day. Also, any type of oral lesion whatsoever is referred, since serious medical issues may arise and a diagnosis must be made by the appropriate medical or dental professional, as this assessment form is mostly designed for SLPs. The general oral hygiene of the patient is merely an indication of the compliance of the patient and is not meant to replace the evaluation of a dental professional, but also suggests issues with chewing and oral clearance due to muscles working at a less than optimal level.
A note may be made regarding past, present and scheduled orthodontic conditions, both in terms of fixed appliances and removable appliances, including palatal expanders (rapid and slow) sleep-dental appliances, night guards, oral hygiene appliances, habit trainers or functional appliances. Oral appliances impact not only teeth and bone but also muscles and oral functions (Jonas, Mann, Munker, Junker, Schumann, 1978; Kucukkeles & Ceylanoglu, 2003; Halazonetis, Katsavrias & Spyropulos, 1994).
Although ONLY a dentist can diagnose any dental issue, including Angles Class, if and when it is appropriate a note should be made of the various spatial relationships between dental arches, as they indicate where there is a functional disorder or less than optimal function. An anterior open bite is often accompanied by an anterior tongue thrust, an excessive overjet may stimulate “lip-wedging” against the upper teeth, also a crossbite may be an indication of a unilateral tongue thrust or a significant asymmetry of the tongue.
The tongue is assessed in its overall aspect, which most of the time is WNL but in certain cases it may look either flaccid or “stiff”. For additional information about assessment strategies please refer to Solomon, 2004; Solomon & Munson, 2004; Lazarus, 2005; Clark, 2012; Clark & Solomon, 2012. Often measuring the actual protrusion of the tongue can be useful to document the need for a referral for a lingual frenum release. The measurement can be done easily with the tongue extending on top of the tongue depressor and by measuring the length on the tongue depressor itself, anchored against the lower incisors (Marchesan, 2005). A functional way to assess the tongue movement is to determine if the patient can clean the buccal surfaces of the lower and upper molars. As mentioned before, when talking about signs and symptoms of sleep disorders, the scalloping of the tongue is noted, with the various degrees of severity (Weiss, Atanasov & Calhoun, 2005). It may denote an obligatory or a compensatory tongue thrust. A full ROM, SOM and AOM assessment of the tongue is also performed.
Skills regarding chewing and the quality of the food chewed are noted, including food avoidance or texture avoidance and the reasons why. Chewing with the mouth open or not is also noted. Swallowing is assessed in all its types such as: saliva, liquid (holding, gulping, sipping, chugging), foods and pills. Anything of note is recorded, like gagging or burping.
The diadochokinetic assessment (fast repetition of trains of syllables like “buttercup” or puh-tuh-kuh) is useful primarily to speech pathologists, as speed is needed mostly in speech performance (Fletcher, 1972 and 1985). Also, although orofacial myologists in general should be able to document speech misarticulations by having the patient repeat easy sentences, often the misarticulations are multiple and complex, warranting a referral to a speech language pathologist, if the treating orofacial myologist is not already an SLP. Misarticulations affecting the /s/ and /z/ are more common in OMDs followed by the misarticulation of the /r/ as the tongue is not able to properly elevate its sides.
Because this assessment tool includes functions of interest to a speech language pathologist, information about the general aspect of voice and hearing is also listed. While some speech pathologists might have access to digital tools and software to identify voice disorders, this tool only lists perceptual characteristics of the voice, like its volume (intensity) pitch (frequency) and nasality (resonance). Also the quality of the voice is noted: hoarseness, dyplophonia, wetness. A note about prosody can be added when appropriate. If everything is normal the note written is WNL (within normal limit).
In addition to information collected from the patient or the parents, the finger rub test for hearing acuity is used. This is a very simple screening test well documented in medical literature. Clearly it requires a quiet office environment. An inquiry is also made to the integrity of the tubaric function, to address possible disturbances due to allergies and hypertrophic tubal tonsils. Poor functionality of the Eustachian tubes is conducive of decreased hearing, increased internal noise during chewing, and trouble swallowing. (Mew & Meredith, 1992).
The dental professionals might want to skip these two sections above or modify them for their own needs. They may also be used to document referrals when the voice or the speech of the patient is perceptually not “right”.
Additional tests done or scheduled can be added and a narrative about birth, development and life style related to OMDs can be added separately, including any musical instruments played, reading and writing skills, or dexterity.
CONCLUSIONS
By no means is this assessment chart complete, but it’s quite comprehensive, evidence-based and easy to scan and share with referrals and parents, if needed. Moreover, there is always room for improvement and new items for the form may be added if necessary.
Disclaimers
The author has no institutional affiliations and no sources of funding. The author has no financial interest or other benefits, either direct or indirect, that may represent a conflict of interest.
Appendix A. Assessment Chart for Speech and Swallow
References
- American Speech-Language-Hearing Association, and Ad Hoc Joint Committee with the International Association of Orofacial Myology. 1993. Orofacial myofunctional disorders: Knowledge and skills. American Speech-Language-Hearing Association. ASHA Suppl. 35 Suppl. 10: 21–23. [Google Scholar]
- American Speech-Language-Hearing Association. 1991. The role of the speech-language pathologist in assessment and management of oral myofunctional disorders. American Speech-Language-Hearing Association. ASHA 33 Suppl. 5: 7. [Google Scholar]
- Barsh, L. I. 1998. Dentistry’s Role in the Recognition and Treatment of Sleep-Breathing Disorders: The Need for Cooperation with the Medical Community. Journal of California Dental Association 26, 8: 591–598. [Google Scholar] [CrossRef]
- Bonuck, K., K. Freeman, R. D. Chervin, and L. Xu. 2012. Sleep-Disordered Breathing in a Population-Based Cohort: Behavioral Outcomes at 4 and 7 Years. Pediatrics. [Google Scholar] [CrossRef]
- Bresolin, D., G. G. Shapiro, P. A. Shapiro, S. W. Dassel, C. T. Furukawa, W. E. Pierson, M. Chapko, and C. W. Bierman. 1984. Facial characteristics of children who breathe through the mouth. Pediatrics 73, 5: 622–625. [Google Scholar] [CrossRef]
- Camargo Tanigute, C. 2005. Edited by I. Queiroz Marchesan. A documentacao como ferramenta para o diagnostico e controle da degluticao. In Tratamento da degliticao: A atuacao do fonoaudiologo em diferentes paises. Sao Jose dos Campos SP, Brazil: Pulso, pp. 107–115, [Brazilian]. [Google Scholar]
- Carvajal, R., R. Miralles, D. Cauvi, B. Berger, A. Carvajal, and R. Bull. 1992. Superior orbicularis oris muscle activity in children with and without cleft lip and palate. Cleft Palate Craniofacial Journal 29, 1: 32–36; discussion 36–37. [Google Scholar] [CrossRef]
- Clark, H. M. 2012. Specificity of Training in the Lingual Musculature. Journal of Speech-Language and Hearing Research 55: 657–667. [Google Scholar] [CrossRef] [PubMed]
- Clark, H. M., and N. P. Solomon. 2012. Muscle Tone and the Speech-Language Pathologist: Definition, Neurophysiology, Assessment, and Interventions. Perspectives on Swallowing and Swallowing Disorders. [Google Scholar] [CrossRef]
- Coceani, L. 2003. Oral structures and sleep disorders: A literature review. International Journal of Orofacial Myology 29: 15–28. [Google Scholar] [CrossRef]
- De Felicio, C. M., M. O. Melchior, and M. A. Da Silva. 2010. Effects of Orofacial Myofunctional Therapy on Temporomandibular Disorders. The Journal of Craniomandibular Practice 28, 4: 249–259. [Google Scholar] [CrossRef]
- Donato, G., L. Lapitz, and D. Grandi. 2009. Protocolo de exploración interdisciplinar orofacial para niños y adolescentes. Revista Logopèdia Collegi de Logopedes de Catalunya, 12–15, [Spanish]. [Google Scholar]
- Echarri, P., A. Carrasco, E. Vila, and E. Bottini. 2009. Protocolo de exploración Interdisciplinar orofacial para niños y adolescentes. Revista Ortodoncia Española 49, 2: 107–115, [Spanish]. [Google Scholar]
- Enlow, D. H., and M. G. Hans. 1996. Essentials of facial growth. Philadelphia: Saunders WB. [Google Scholar]
- Ferrario, V. F., C. Sforza, C. E. Poggio, and G. Tartaglia. 1994. Distance from symmetry: A three-dimensional evaluation of facial asymmetry. Journal of Oral Maxillofacial Surgery 52, 11: 1126–1132. [Google Scholar] [CrossRef]
- Fletcher, S. G. 1972. Time-by-count measurement of diadochokinetic syllable rate. Journal of Speech and Hearing Research 15: 763–770. [Google Scholar] [CrossRef]
- Fletcher, S. G. 1985. Speech production and oral motor skill in an adult with an unrepaired palatal cleft. Journal of Speech and Hearing Disorders 50, 3: 254–261. [Google Scholar] [CrossRef] [PubMed]
- Garretto, A. L. 2003. Edited by M. L. Hanson and R. M. Mason. Orofacial Myology in Argentina. In Orofacial myology: International perspectives. Springfield, IL: CC Thomas, pp. 313–328. [Google Scholar]
- Garretto, A. L. 2005. Edited by I. Queiroz Marchesan. Experiencia fonoaudiologica no aprendimento odontopediatrico e ortodontico. In Tratamento da degluticao: A atuacao do fonoaudiologo em diferentes paises. Sao Jose do Campo, Brazil: Pulso, pp. 35–59, [Brazilian]. [Google Scholar]
- Genaro, K. F., G. Berretin-Felix, M. I. Rehder, and I. Q. Marchesan. 2009. Orofacial myofunctional evaluation: MBGR protocol. Rev CEFAC 11, 2: 237–255. [Google Scholar] [CrossRef]
- Gonçalves Bianchini, E. M. 2000. Articulação temporomandibular: Implicações, limitações e possibilidades fonaudiológicas. SP Brazil: Pro Fono, [Brazilian]. [Google Scholar]
- Goulet, J. P., G. T. Clark, and V. F. Flack. 1993. Reproducibility of examiner performance for muscle and joint palpation in the temporomandibular system following training and calibration. Community Dental and Oral Epidemiolgy 21, 2: 72–77. [Google Scholar] [CrossRef]
- Guimarães, K. C., L. F. Drager, P. R. Genta, B. F. Marcondes, and G. Lorenzi-Filho. 2009. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. American Journal of Respiratory and Critical Care Medicine 179, 10: 962–966. [Google Scholar]
- Halazonetis, D. J., E. Katsavrias, and M. N. Spyropoulos. 1994. Changes in cheek pressure following rapid maxillary expansion. European Journal of Orthodontics 16, 4: 295–300. [Google Scholar]
- Harley, E. H. 2002. Asymmetric tonsil size in children. Archives of Otolaryngology and Head and Neck Surgery 128, 7: 767–769. [Google Scholar] [CrossRef]
- Hanson, M. L., and R. M. Mason. 2003. Orofacial myology: International perspective, 2nd ed. Springfield, IL: Charles C. Thomas Publishing Company. [Google Scholar]
- Jonas, I., W. Mann, G. Munker, W. Junker, and K. Schumann. 1978. Relationship between tubal function, craniofacial morphology and disorder of deglutition. Archives of Otorhinolaryngology 218, 3–4: 151–162. [Google Scholar] [CrossRef]
- Korbmacher, H., L. E. Koch, and B. Kahn-Nieke. 2005. Orofacial myofunctional disorders in children with asymmetry of the posture and locomotion apparatus. International Journal of Orofacial Myology 31: 26–38. [Google Scholar]
- Küçükkeles, N., and C. Ceylanoglu. 2003. Changes in lip, cheek, and tongue pressures after rapid maxillary expansion using a diaphragm pressure transducer. Angle Orthodontics 73, 6: 662–668. [Google Scholar]
- Lazarus, C. L. 2005. Lingual strengthening and swallowing. Perspectives on Swallowing and Swallowing Disorders (Dysphagia) 14, 2: 2–6. [Google Scholar]
- Li, A. M., E. Wong, J. Kew, S. Hui, and T. F. Fok. 2002. Use of tonsil size in the evaluation of obstructive sleep apnoea. Archives of the Disordered Child 87, 2: 156–159. [Google Scholar] [CrossRef] [PubMed]
- Mallampati, S. R., S. P. Gatt, L. D. Gugino, S. P. Desai, B. Waraksa, D. Freiberger, and P. L. Liu. 1985. A clinical sign to predict difficult tracheal intubation: A prospective study. Canadian Anaesthesiology Society Journal 32, 4: 429–434. [Google Scholar]
- Marchesan, I. Q. 2004. Lingual frenum: Classification and speech interference. International Journal of Orofacial Myology (30): 31–38. [Google Scholar]
- Marchesan, I. Q. 2005. Lingual frenulum: Quantitative evaluation proposal. International Journal of Orofacial Myology (31): 39–48. [Google Scholar]
- Marchesan, I. Q., A. D. Teixeira, and D. M. Cattoni. 2010. Correlations between different lingual frenulums and speech disorders. Revista do Disturbios da Comunicação 22, 3: 195–200, [Brazilian]. [Google Scholar]
- Mason, R. M. 2005. A retrospective and a prospective view of orofacial myology. International Journal of Orofacial Myology 31: 5–14. [Google Scholar]
- Mathur, R., I. L. Mortimore, M. A. Jan, and N. J. Douglas. 1995. Effect of breathing, pressure and posture on palatoglossal and genioglossal tone. Clinical Science 89: 441–445. [Google Scholar] [PubMed]
- Mew, J. R., and G. W. Meredith. 1992. Middle ear effusion: An orthodontic perspective. Journal of Laryngology and Otology 106, 1: 7–13. [Google Scholar] [PubMed]
- Meyer, P. G. 2000. Tongue lip and jaw differentiation and its relationship to orofacial myofunctional treatment. International Journal of Orofacial Myology 26: 44–52. [Google Scholar]
- Miles, T. S. 2007. Postural control of the human mandible. Archive of Oral Biology 52, 4: 347–352. [Google Scholar] [CrossRef]
- Miles, T. S., S. C. Flavel, and M. A. Nordstrom. 2004. Stretch reflexes in the human masticatory muscles: A brief review and a new functional role. Human Movement and Science 23, 3–40: 337–349. [Google Scholar] [CrossRef]
- Miyake, R., R. Ohkubo, J. Takehara, and M. Morita. 2004. Oral parafunctions and association with symptoms of temporomandibular disorders in Japanese university students. Journal of Oral Rehabilitation 31, 6: 518–523. [Google Scholar] [PubMed]
- Navazesh, M. 2003. How can oral health providers determine if patients have dry mouth? Journal of American Dental Association 134: 613–620. [Google Scholar] [CrossRef]
- Okuro, R. T., A. M. Morcillo, A. M. G. Oliveira Ribeiro, E. Sakano, P. B. Margosian Conti, and J. D. Ribeiro. 2011. Mouth breathing and forward head posture: Effects on respiratory biomechanics and exercise capacity in children. Journal of Brasilian Pneumology 37, 4: 471–479. [Google Scholar]
- Paskay, L. C. 2006. Instrumentation and measurement procedures in orofacial myology. International Journal of Orofacial Myology 32: 37–57. [Google Scholar]
- Peterson-Falzone, S. J., M. A. Hardin-Jones, and M. P. Karnell. 2009. Cleft palate speech, 4th ed. Saint Lewis, MO: Mosby. [Google Scholar]
- Proffit, W. R., and H. W. Fields. 1986. Contemporary orthodontics. St. Louis, MO: CV Mosby Company. [Google Scholar]
- Queiroz Marchesan, I. 2005. Tratamento da degliticao: A atuacao do fonoaudiologo em diferentes paises. Sao Jose dos Campos SP, Brazil: Pulso, [Brazilian]. [Google Scholar]
- Quintal, M., A. Tessitore, J. Rizzoato Paschoal, and L. Nizam Pfeilsticker. 2004. Facial paralysis quantification by digital paquimeter. Revista CEFAC 6, 2: 170–176, [Brazilian]. [Google Scholar]
- Rodrigues Correa, E. C., and F. Berzin. 2004. Temporomandibular disorder and dysfunctional breathing. Brazilian Journal of Oral Sciences 3, 10: 498–502. [Google Scholar]
- Samsoon, G. L., and J. R. Young. 1987. Difficult tracheal intubation: A retrospective study. Anaesthesia 42, 5: 487–490. [Google Scholar] [CrossRef] [PubMed]
- Satomi, M. 2001. The relationship of lip strength and lip sealing in MFT. International Journal of Orofacial Myology 27, 1: 18–23. [Google Scholar] [CrossRef]
- Scarbrough, F. E., G. E. Ghali, and B. R. Smith. 1997. Anatomic guidelines for the placement of external references for maxillary repositioning. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics 84, 5: 465–468. [Google Scholar] [CrossRef]
- Scutter, S. D., and K. S. Turker. 2001. The role of the muscle spindles in human masseters. Human Movement Science 20, 4–5: 489–497. [Google Scholar] [CrossRef]
- Shames, J. 2012. Xerostomia / Qualitative Changes in Saliva, With Reasonable Medical Probability, Contributes to Sleep Disordered Breathing (article in press, personal communication). [Google Scholar]
- Solomon, N. P. 2004. Assessment of tongue weakness and fatigue. International Journal of Orofacial Myology 30: 8–19. [Google Scholar] [CrossRef]
- Solomon, N. P., and B. Munson. 2004. The effects of jaw position on measures of tongue strength and endurance. Journal of Speech Language and Hearing Research 43, 3: 584–594. [Google Scholar] [CrossRef] [PubMed]
- Vig, P. S., and M. Cohen. 1979. Vertical growth of the lips: A serial cephalometric study. American Journal of Orthodontics 75, 4: 405–415. [Google Scholar] [CrossRef]
- Weiss, T. M., S. Atanasov, and K. H. Calhoun. 2005. The Association of Tongue Scalloping with Obstructive Sleep Apnea and Related Sleep Pathology. Otolaryngology-Head and Neck Surgery 133: 966–971. [Google Scholar] [CrossRef]
© 2012 by the author. 2012 Licia Coceani Paskay.