INTRODUCTION
Principals of using a positive behavior modification approach in the elimination of digit habits and non-nutritive sucking behaviors rather than habit appliances are employed by orofacial myologists. Van Norman’s life work was dedicated to establishing a positive approach in the treatment of these behaviors. Moore (2008) supports this need for a positive approach to treatment in his extensive review of research.
Rewarding a desired behavior to eliminate an undesired behavior is not new to the literature. The premise of behavior modification can be utilized effectively when applied to digit sucking. “Behavior is often shaped by the consequences it produces; actions are repeated if they yield positive outcomes” (
Baron, 1998, p. 595.) Ferster and Skinner (1957) found this type of continuous schedule of reinforcement effective in establishing and strengthening new behaviors. In addition, rewarding a subject for the desired behavior in an expedient manner usually results in the performance of that particular desired behavior better than a delayed-reward approach (
Capaldi, 1978). In essence, Rose Van Norman utilized these proven and respected techniques to design an effective program for digit sucking elimination. Through this approach a child who desires to extinguish the behavior of digit sucking is rewarded for their efforts expediently, aggressively and consistently.
The frustration of a child’s own inability to stop their subconscious habit, and the constant feeling of disapproval by family and peers, often leads to a negative spiral. There is a tendency to demonstrate speech disorders (Umberger and Van Reenen, 1995), poor eating habits, open lips rest posture, and tongue protrusion when not sucking, lessened socialization, and an altered dental, facial, or soft tissue appearance (
Van Norman, 1997).
Self esteem is a topic that has been previously addressed (Anthony, Holmes, Wood, 2007). Self esteem is attuned to appearance, and in most roles, appearance determines acceptance. Peer disapproval decreases self esteem, and peer approval increases self-esteem (Thomaes, Reijntjes, Orobio de Castro, Bushman, Poorthuis, and Telch, 2010). A child’s view of themselves and how the world view’s them are deeply intertwined. Positive social adjustment is correlated with low peer victimization (Rudolph, Caldwell, Conley, 2005). Teasing and victimization leads to social withdrawal, something with which digit sucking children must often contend. Social approval enhances self worth and self esteem. Poor self esteem, and social disapproval are issues many digit sucking children also struggle with (
Van Norman, 1997). It is critical to provide support to the child with a digit habit in their efforts to cease this behavior.
METHODS
This study was a confirmational analysis in which information was collected on 441 subjects who were enrolled in an orofacial myofunctional program emphasizing a positive behavior modification approach over a 10 year period of time from 1999 to 2010. Subjects ranged in age from 3.5 to 16 years of age. Subjects were seen in a private office setting with the same orofacial myologist. At approximately 30 days after the initial visit, parents were asked to complete a survey at this follow-up visit. The survey was completed in the therapist’s office. The survey was developed by Van Norman (1997), and was used with her permission. That same survey was used in an attempt to confirm Van Norman’s findings. Once completed, the surveys were bound and the data was compiled for this study. Simple percentages were calculated to determine results. Inclusion criteria included individuals who had either a digit habit, a pacifier habit, or a habit that included both.
In addition, any children included in the study who were 3 years of age were a direct referral from a pediatrician who asked that the child be admitted to the program due to a health concern. These children were allowed to participate at a younger age than is typically preferred. It is this author’s opinion that although younger subjects are able to participate in such a program, the preferred age for a habit elimination program is closer to 4, which is the typical age at which signs of readiness are present. Criteria used for exclusion of individuals from this study included that a parent needed to complete the survey. It should be noted that 2 college age individuals, one female - age 21, and one male - age 19, were excluded from the study results. These students did participate in the program and were successful in habit elimination, but a parent was not in attendance for the 30 day visit to complete the parental survey. In addition, individuals were not included in the study if the parents were unable or unwilling to attend each treatment session and implement the recommended parent program. These individuals were also not enrolled for treatment as parent participation is integral to the success of the treatment program.
This survey attempts to detail the duration of habit and cessation on specific individuals, specify the former techniques utilized to attempt cessation of digit sucking behavior, and quantification of the number of days needed to achieve success with cessation behavior. The study attempts to confirm results provided in 1997 by Van Norman.
The techniques used in the habit elimination program provided for the purposes of this study were based on the following premise: oral habit elimination using positive reinforcement, reward, and strategies to assist the client in distracting themselves from the habit will be successful. This, in essence, is the basis of oral habit elimination programs as specified by the International Association of Orofacial Myology (IAOM.) For example, children would be encouraged to engage in alternate activities, utilize indoor manipulatives for distraction, or other strategies designated to keep their digits and minds otherwise occupied. They quickly identified their trigger situations, such as “when I sit and watch TV, now I play with my doll, instead of when I sit and watch TV, now I play with my doll instead of when I sit and watch TV, I suck my fingers.” The premise is that the child will ultimately eliminate the sucking habit and learn a newer and more appropriate set of positive behaviors in specific environments, and thus develop a chain of events encouraging cessation of sucking behavior. Parents were instructed about when and how to positively reinforce the desired behavior using praise, tokens, or rewards, and encouraging the child’s feeling of accomplishment and positive self-control expediently and consistently. This approach utilizing behavior modification and positive reinforcement techniques (
Van Norman, 1997) was utilized extensively in the protocol for the current study.
Rewarding desired behaviors in turn creates a positive spiral of success, rather than the negative spiral of sucking resulting in negative self-thoughts focused on sucking, which triggers increased sucking, which triggers increased negative feelings and self-thoughts. Most avid thumb and finger sucking children experience this negative spiral that encourages them to sustain the habit. Night time and daytime reminders were placed on the fingers or thumb to remind the client that the finger was approaching, encouraging them to redirect the digit to another activity. Parents were provided with the same basic strategic information on implementing a behavioral approach using positive reinforcement, while adapting some individual strategies to suit the particular habit profile to each particular child’s unique habit experience and environment. Again, parents were encouraged to provide rewards of praise, or tokens, expediently and consistently when this more positive behavior was demonstrated. The ultimate goal was that eventually the automatic subconscious behavior of digit to oral cavity is extinguished over time, in a positive manner.
While survey information was completed around the one month milestone, contact was maintained between the child, family, and therapist throughout the first 60 days. Daily communication was encouraged. After the initial visit, clients attended three additional sessions during the first month, and once during the second month.
RESULTS
Overall
This study included 441 subjects with a sucking habit, of which 73.02% were female (322) and 26.98% were male (119.) Of the total number of subjects 441 had a digit habit with 322 females and 119 males. Of 441 total subjects, 17.46% (77) reportedly had previously sucked a pacifier. No participants included this study reported a current use of pacifier sucking. Of the 322 females included in this study 59 (17.77%) were reported to have a former pacifier habit more frequently than males, 18 of 119 males (15.13%). The population reported to have a former pacifier habit who also had history of a concurrent digit habit was 5.66% (25), which included 4 males and 21 females. Of 441 total subjects in this study, parents of 179 subjects (40.59%) reported a speech concern which included 30.17% (54) males and 69.83% (125) females.
Based on direct observation of the orofacial myologist as reflected in the records, 99% of children had low rest posture of the tongue and/or tongue thrusting. When asked if the program participation led to increased self-worth and self-confidence, 429 (97.27%) of parents reported ‘Yes’ that it did. 100% of the parents responding to the survey indicated that they would recommend the program to other parents of a child with a thumb/finger-sucking habit.
Pacifier
Of all subjects (77) reporting a previous pacifier sucking history, 22.66% of males and 76.31% of females used only a pacifier, and not a thumb or finger and pacifier concurrently. Of those 77 subjects, parents of 68 were able to quantify the duration of the pacifier habit. Upon analysis of the data, the average duration of all subject’s pacifier habit, both male and female, was an average of 18.85 months. Females sucked their pacifiers longer than males, with females using a pacifier an average of 20.23 months, and males, an average of 14.37 months total.
Speech problems
It should be noted that the author is not a speech pathologist; therefore any speech concerns included within the framework of this study are based on the parental reporting of speech concerns, and are not a direct result of any diagnostic tests to assess neither appropriate speech nor inappropriate speech. It should also be noted that most parents did not report a tongue thrust problem, because most individuals were not aware of its existence prior to treatment.
Of 441 total subjects in this study, parents of 40.59% (179) of the subjects reported a speech concern. Of those 179 parents reporting speech concerns for their children, 30.17% (54) were male subjects, and 69.83% (125) were female. When comparing the proportion of males (30.17%) and females (69.83%) who experienced speech difficulties with the proportion of males (26.98%) and females (73.02%) in the total study population, males appeared to have a slightly lower percentage of parents reporting speech issues than females.
Of the 179 reports of speech concerns, parents of 56.98% (102) of the subjects reported more than one speech issue which included general non-specific concerns items such as: many concerns (1); multiple concerns (1); general concerns (20); lisp (21); parentally reported tongue thrust (7); sloshy (2); or, delay/processing issues (6). Parents reporting more than one speech concern represent 23.13% of the total population of 441. Only 35.20% (63) of parent reports addressed concerns of only one specific articulation variable. The most common four sounds that parents reported were of concern included: S or Sh (72), R (46), Th (34), and L (16). In addition, parents reported concerns about the following sounds: CH (10), Z (7), F (8), T (6), W (5), V (4), J (4), G (3), D (3), N (3), B (2), A (1).
Parents of 67 subjects with speech concerns reported a history of speech therapy. The average time a child spent in speech therapy was 24.73 months. This means that of the 179 subjects with reported speech issues, more than half, 62.57% (112 subjects), did not receive speech therapy. Perhaps in the future it might be interesting to collect information on why this percentage was so high.
Cessation of habits
The most common methods parents reported to extinguish digit sucking behavior prior to enrollment in the orofacial myofunctional treatment program were: rewards (82), Band AidsTM (55), sock (45), chart (24), tape (30), bad tasting polish or crème (65), bribe (54), remind (52), and positive reinforcement (25). Please see chart 7 for further detail. Parents specified 62 various methods in total. This indicates that parents offered multiple trials and multiple methods in an attempt to bring about cessation. There were also reports of dental appliances reported by five parents. The longest duration of time a dental appliance was worn was 18 months, and the shortest was approximately 2 hours. There were 28 trials reported by parents which were physically and emotionally based, and which may be considered negative in nature.
Parents of the total number of subjects (44) reported that after receiving orofacial myofunctional treatment their child began to discontinue the sucking habit : immediately (84.35%); immediately to within 24 hours (88.20%); during the first 24 to 48 hours (92.29%); within 72 hours (94.55%); by day 7 (97.95%); by day 14 (99.773%); and all subjects had stopped by day 21. A slightly higher percentage of males 103 (86.56%) than females 269 (83.54%) stopped immediately.
Interestingly, in the youngest age groups of 3 and 4 year olds, all parents of 3 year olds (3 subjects) reported having ceased their habit within the first 24 hours. There were 34 subjects in the group of 4 year olds, 79.41% of whom stopped digit sucking within the first 24 hours. The longest duration of time taken for habit cessation was 21 days for a 4 year old female. Otherwise, 33 (97.05%) of the 3 to 4 four year olds stopped within the first week, and 29 out of 34 subjects who were 4 years old (85.29%) stopped by day 3. Parents reported that cessation occurred immediately within the first 24 hours in all subjects in a number of age categories including 7, 9, 14, and 15 year old males, and 10, 12, 14, and 16 year old females. In addition, 90% or more of both 5 and 7 year old males and females ceased their digit habit within the first 24 hours.
Emotional concerns
When asked if discontinuing the sucking process lead to any emotional issues, 82.53% of parents of all subjects reported a definite ‘no.‘ However, parents of 100% of the group of 15 year olds reported yes and parents of 66% all 3 year olds indicated concerns. No pattern could be identified by age for the occurrence of emotional issues as reported by parents across the remaining age groups.
Parents of 83 subjects (18.82%) reported their children had a specific short term emotional issue as a result of participation in the program. There were 8 (1.81%) responses of ‘maybe’ or “possibly” noted for the presence of short term difficulties. The parent of one 8 yr. old female had two complaints. No parents reported any long term emotional concerns in the survey findings. Four parents reported slightly longer times to fall asleep at day 60, but no distress was reported in these instances, only the existence of longer sleep latency until slumber.
The highest percentage of emotional issues was reported in 15 year old males (50%), 12 year old females (100%) and 3 yr. old females (67%). However, these age groups represented an extremely small part of the overall population two 15 year olds, six 12 year olds, and three 3 year old subjects out of a total of 441 subjects. When examining the majority of the subject population and comparing the instance of emotional issues reported, no particular age range stood out as experiencing more difficult than another. In general, the percentage reported remained in approximately the 20-25% range.
When analyzing emotional issues by sex, the greatest discrepancies were as follows: 3 year old males - 0/3 (0%) compared to 3 year old females - 2/3 (67%), 6 year old males 1/87- (1.149%) compared to 6 year old females 22/87- (25.28%), 10 year old males 0/23 (0%) compared to 10 year old females 1/23- (4.347%), 11 year old males 1/16- (6.25%) compared to 11 year old females 0/16- (0%), and 12 year old males 0/6- (0%) compared to 12 year old females 1/6- (33%). Again, subject population was lower in the 11 and 12 year old subject ranges (16 and 6 years, respectively).
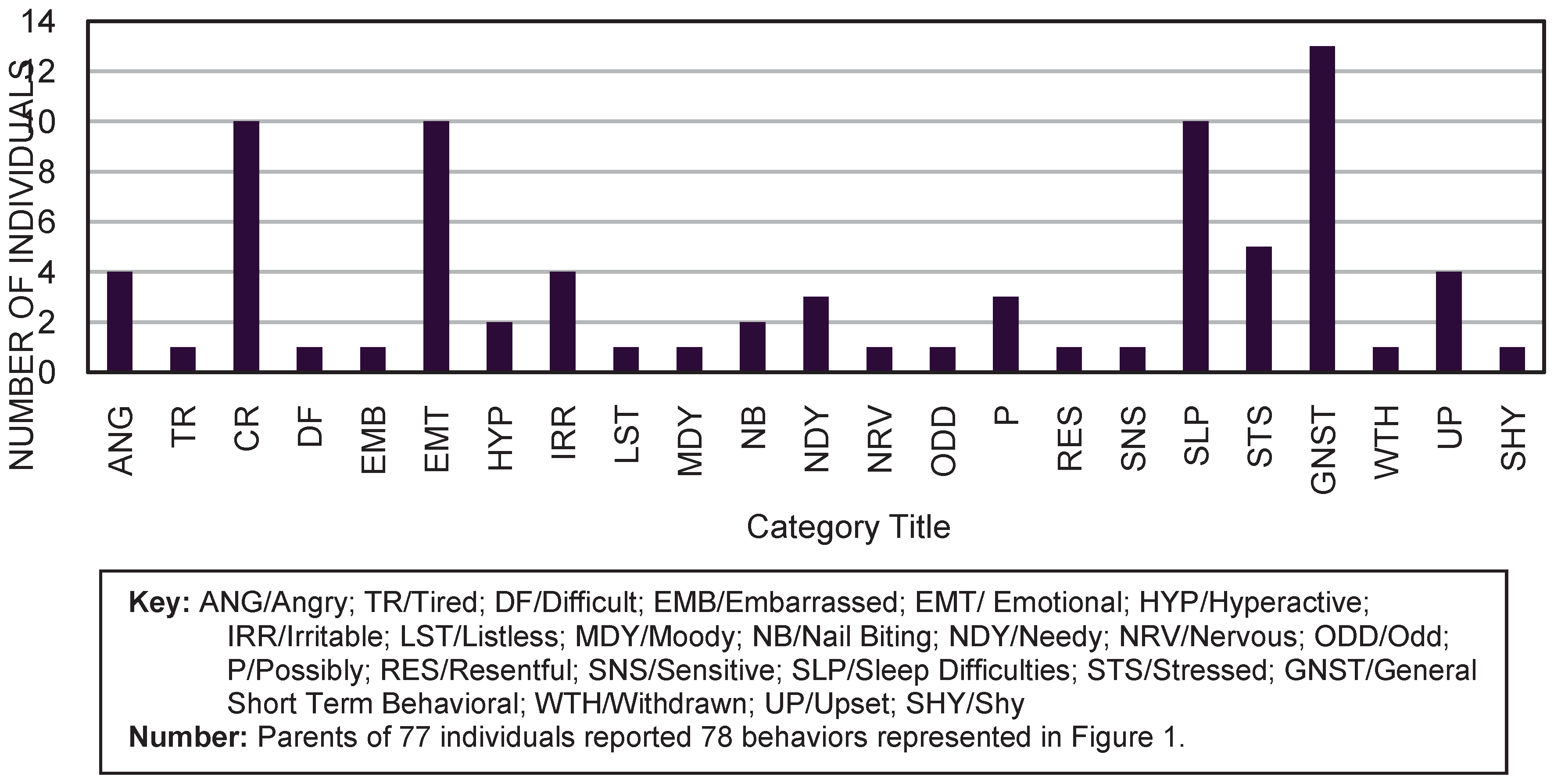
The most common emotional issues reported by parents of 83 subjects voicing 84 complaints (16 males and 67 females) were: sleep (9 out of 83), crying (11 out of 83), emotional (11 out of 83), and general short term issues (15 out of 83). Out of the 11 subjects who reported “crying”, 10 out of 11 were female, and only 1 subject was male. That male subject was eleven years old. Of females reporting crying, 2 were age four, 2 were age five, 3 were age six, two were age seven, and 1 was age eight. Of the total 441 subjects, 10 out of 332 (3.01%) females, compared to 1 out of 119 (.08%) males reported crying as their emotional behavior. A slightly higher percentage of parents of females reported the presence of emotional issues compared to parents of males: 16 out of 119 (13.45%) children with emotional concerns were male, and 67 out of 332 (20.18%) were female. The average age of all children whose parents reported crying was 6.25 years.
Regarding total population with reported sleep difficulties, 2 out of 119 (1.68%) males and 7 out of 332 (2.11%) females reported “yes” to this issue. Parents of female children reporting sleep difficulties: 1 was age three, 1 was age four, 3 were age five, 2 were age six, and 2 were age seven. Parents of males reporting sleep difficulties: 1 was age five, and 1 was age eight. Of all 441 subjects, 2.04% reported difficulties with sleep. (
Figure 1.)
Unexpected outcomes
The parent of one subject reported the existence of pathological skin picking (PSP), which may be considered a chained behavior to digit sucking. Parents of 5 subjects reported the existence of trichotillomania (hair pulling). It should be noted that only the digit habit in this program was addressed in the treatment program (
Green, 2009). However, it is interesting to note that as a direct result of the elimination of the sucking habit, four of the five subjects with reported trichotillomania achieved full cessation of their chained habit at thirty days. One of the children experienced mild pulling intermittently at 60 days, with no continued sucking behavior. All of the children whose parents reported these chained behaviors achieved full and expedient sucking habit cessation.
In addition, the subject whose parent reported pathologic skin picking was also treated exclusively for the thumb habit. It is noted that the PSP stopped immediately and coincidentally. This child continued to be free of both habits at 60 days.
DISCUSSION
Overall
This study correlates overall with research by Van Norman (1997), and Umberger et al, (1995). It confirms the greater propensity for females to have a digit habit than males. Please see the table in appendix A for further information on specific similarities.
Pacifiers
A somewhat proportionate number of males and females previously sucked a pacifier when compared to the entire study population (22.66% vs. 76.31%, respectively). This was similar to, but not identical to the overall percentage of male subjects compared to female subjects in the study (26.98% vs. 73.01%, respectively). The average duration of pacifier sucking in this study was 20.23 mo. for females and 14.37 months for males.
Pacifier sucking habits are on the rise internationally, and research is fruitful on this topic. For example, Santos, Holanda, Sena, Gondim, Ferreira (2009), report that 40% of their subject population had a retained sucking habit, with 27.70% comprised of the pacifier, and 12.5% of a digit. Current pacifier research has recently highlighted an increased potential for multifaceted negative effects on the dentition and propensity for a vertical growth pattern of the palatal structure than previously recognized (Melnick, Vagner, Hocevar-Boltezar, and Ovsenik, 2010).
As a result of new research, more information on the deleterious effects of extended sucking habits, that has not been available previously, is now able to be more easily ascertained (
Larsson, 2001; Onyeaso and Isiekwe, 2008;
Santos et al., 2009; Mistry, Moles, O’Neil, and Norar, 2010; and Yemitan, daCosta, Sanu, and Isiekwe, 2010).
However, on a more positive note, research suggests that pacifier use may reduce the risk of Sudden Infant Death Syndrome (SIDS) (
Cinar, 2004; Hauck, Omoiokun, and Siadaty, 2005; and Sexton and Natale, 2009). The American Academy of Pediatrics (AAP) recommends that parents consider offering pacifiers to infants one month and older at the onset of sleep to reduce the risk of sudden infant death syndrome. The AAP provides guidelines and specific suggestions, including delaying the introduction of the pacifier one month in the breastfeeding infant to better assist in the establishment of breastfeeding. The AAP states “Although the mechanism is not known, the reduced risk of SIDS associated with pacifier use during sleep is compelling…unless new evidence dictates otherwise, the task force recommends use of a pacifier throughout the first year of life.” (
American Academy of Pediatrics, 2005, p.1252).
In addition, Sexton (2009) relates that a pacifier may be used as an adjunct to stave off the pain of minor procedures and discomforts in the infant. Cinar (2004) reports that it is useful to minimize discomfort following minor childhood accidents. However, when exploring the possible negative effects of pacifier usage, Sexton (2009) relates that using a pacifier for a long period of time has a negative consequence on breastfeeding, malocclusion, and may increase the propensity for experiencing otitis media. Jackson and Mourino (1999) studied 200 infants age 12 months and younger, and also found that the risk of otitis media in an infant is twice as great if a pacifier has been utilized than if it had not. Hauck, et al (2005), in their meta-analysis also note that encouraging pacifier weaning should occur between 6-12 months of age due to risk of otitis media. The AAP Task Force on SIDS states “There is an approximate 1.2- to 2-fold increased risk of otitis media associated with pacifier use, but the incidence of otitis media is generally lower in the first year of life, especially the first 6 months, when the risk of SIDS is the highest. However, pacifier use, once established, may persist beyond 6 months, thus increasing the risk of otitis media.” (AAP, 2005, p.1248).
In discussing potential dental concerns, the American Academy of Pediatric Dentistry indicates that oral habits may have a long term impact on dentition, and recommend that if cessation of oral habits does not occur spontaneously between 3 to 4 years of age, oral habits should be discouraged after the age of 4 (AAPD, 2007, p.1). When appropriate, the AAPD encourages treatment of oral habits to “prevent or intercept possible malocclusion or skeletal dysplasia from occurring”. (AAPD, Policy Statements, 2000, p. 31). The American Dental Association (ADA) (2007) also recommends actively discouraging pacifier use after four years of age.
Speech problems
Overall the number of parents reporting concerns regarding speech problems was 40.59%. Of this group for whom speech concerns were indicated, 62.57% did not receive speech therapy. Many parents reported anecdotally that an assessment had occurred at school but therapy did not materialize, or that they had been told by a professional that the thumb or finger sucking should be eradicated before speech therapy was provided. It appeared that many parents had attempted to secure speech therapy through the educational system, but were unsuccessful.
Parents of more than half of the children who indicated that speech was a concern reported more than one speech concern. It is this author’s observation that tongue posture, use, and patterns of rest may be suspected of being a contributing factor. Although most parents did not report a tongue thrust problem, there are similarities between sounds that parents reported to be of concern in this study population for children with retained sucking habits (S, Z, N, T, D, L, SH, J, CH, B, and R), and those sounds indicated by Hansen (1976) which are distorted in children exhibiting a tongue thrust swallow pattern (S, Z, N, T, D, L).
This author notes a casual observation of suspected possible difficulty with the bilabial sounds as well. Again, this is a casual observation, as the author is not a speech pathologist. It is the opinion of this author that the tendency of many of the children in this study to display possible or suspected excessive overjet and maxillary incisor protrusion/labioverted upper anterior incisors, was most likely the direct result of the digit sucking habit, and may have played a role in the suspected distortion of these particular sounds which were heard in casual conversation between examiner and subject. Speech distortions, including the bilabial sounds, were also observed by children with retained sucking habits and reported by Khinda and Grewal (1999).
With 23% of all study participants reporting multiple speech concerns, it appears that some form of intervention aimed at the formidable assault that thumb sucking has on the speech and oral motor complex, habit cessation might be an important consideration. Given this information, one must consider whether the placement of an appliance in the mouth to remediate thumb sucking in a child is the best solution when placement of these devices tends to impact the speech negatively. This may be an area for speech pathologists to explore further in expanding the information on the relationship between sucking habits and articulation errors.
Cessation of habits
Given the high percentage of 4 year olds with cessation by day 3, and the high percentage of 3 year olds by day 1, using the positive behavioral approach employed in this study, one might reconsider the participation of younger clients when medical need necessitates their participation in a habit cessation protocol. Again, one must recall that patient selection for participation is key. Merely taking any child of a 3 or 4 year old into treatment would be unethical unless a medical, social, or dental necessity existed in which the risk of distress or negative impact would outweigh the reward of participation. That is the case in this study’s 3 year old population, but with the 4 year old population, some selection process for participation is prudent.
This researcher feels the high percentage of 5 to 7 year olds who demonstrated 100% cessation within the first 24 hours is significant for two reasons. The reality of a 5 year old attending kindergarten is highly motivating for parents and child. First, the child may feel they want to stave off their own embarrassment by peers or teachers in the school setting.
Parents are also concerned about their child’s socialization or speech being impacted by a sucking habit. The second reason is that parents may be concerned with viral or bacterial transmission and subsequent lost school attendance due to these issues. In the 7 year old, there is a strong motivation because the permanent teeth have begun to erupt signaling more recognizable and obvious bite changes in the mixed dentition. The child at this age is able to visually observe and quantify the results of the habit. They are better able to understand the concerns expressed by the dentist or physician regarding growth and development opening a dialogue for educating the child that considering cessation.
In addition, it appeared that 3 to 6 year old children yielded similar cessation duration results when compared with children in the mixed dentition stage of 7 to 12 years of age. All were within the range of 83% to 94% cessation occurring from within the first 24 hours. In this author’s opinion, it behooves us to consider that a younger child is just as apt to cease their habit as readily as a mid-age range child.
Because the study population only included 7 children ages 13 years to 16 years of age, few conclusions can be drawn as to whether a teen aged child struggles longer to achieve habit cessation. The obvious reason for the low number of subjects in this age range may be that most children have stopped their digit habit by this point, and so fewer parents of children in this age range would seek out a cessation program. Another is that many health care providers do not refer older children who maintain a digit habit because they are not aware the habit still exists. The health care provider may make the assumption the habit was eradicated previously.
One may question how the results reflect such a high percentage of both immediate and favorable cessation. It is the author’s belief that no child should be taken into such a habit elimination program unless they are able to demonstrate ‘a spark of willingness’ to stop. This may be one reason the results of this study are favorable. The clinician’s determination of readiness is key to success. This begins with the initial phone contact. The clinician must be prepared to ask the parent if their child is ‘ready to stop’, and if so what brings them to this conclusion. Responses such as “I am not sure” warrant further investigation. It is suggested that the parent ask the child directly, wait for a response, and the report back over the phone what transpired in that conversation. It is critical the parent be asked, “Have you asked your child if they want to stop”? If a parent states that their child says “I want to stop, but it is so hard”, or “mommy, I’m trying, but I just can’t”, they are often a good candidate, given no emotional issues or major life changes are currently an issue.
When a child undergoes a life change such as a move, new sibling, illness in the family, new school, death of a pet, or similar situations, a red flag should go up. The best way to success is for the child to be in the best possible emotional place so that they can move forward, devoid of concerns, able to dedicate themselves to the program fully. Likewise, if a parent is traveling, has had a recent job change, or is overwhelmed with a heavy workload, the child’s success may be challenged. Again, if all pieces of the puzzle are in place emotionally and for the necessary parental support for the child, the chances of success will be greater. Under such circumstances, utilizing an appropriate program such as the one utilized by Ms. Van Norman and colleagues, an extremely high rate of success should be obtained.
The majority of techniques parents reported they used to encourage habit cessation were positive in nature. However, 45% were considered negative by this author. One must consider the number of children who are receiving negative input and feedback and their frustration with these negative attempts of others to control their subconscious behavior of digit sucking. This alone warrants the consideration of a positive based program of digit sucking elimination.
Five parents reported the use of a habit appliance. The longest duration of habit appliance use reported was 18 months, and was unsuccessful. This author questions why the unsuccessful utilization of a habit appliance would be considered when there are positive techniques, such as those that are outlined in this study, and have been extremely successful in a shorter duration of time.
The results of this study indicate that parents of their own volition sought out a program that was positively based. Parents indicated that they chose a positively based program and wanted to avoid appliance therapy and negative based treatment at all costs. The concerns expressed by parents for the avoidance of appliances anecdotally were possible injury during sports or normal childhood outdoor activity where there was a propensity for an accident or injury, taking a habit which was not in the conscious control of their child and punishing the child for displaying it, concerns over the impact of an appliance on speech or drooling/eating, and the cost of an appliance when compared with the cost of a behavioral program such as that outlined in this study.
This author believes that there are occasionally children who may require such a form of treatment as a habit appliance. The ultimate decision and responsibility to assess the comprehensive health and well-being of a child lies with the child’s parents, dentist, and/or physician. However, considering this use of habit appliances from the perspective of this study’s results, it appears that many parents overwhelming prefer a positive protocol, and anecdotally would not be prone to consider an appliance. Many dental resources view recommending the digit cessation appliance form of treatment as a last resort. Many parents verbally reported having chosen to leave their dental providers when an appliance was suggested and sought help for their child’s habit elsewhere. Some parents reported seeking out a new dental practitioner, and others utilized the popular media to seek answers for their child’s oral habit. It is this author’s hope that this article will provide additional insight on this topic to the professionals addressing the complex issue of habit cessation.
Emotional concerns
In the past, it has been questioned whether or not a very young child should be considered as a participant (
Van Norman, 1997). For parents concerned about the initiation of a formal cessation program prior to age 5, it is evident that the majority of three and four year olds included in this study were able to cease their sucking behavior expediently. However, for the three year olds, this came at a cost. There were 3 three year olds and 34 four year olds included in this study.
Two of the most significant concerns parents often had were the experience of crying and disrupted sleep. Both of these issues were short term in nature. Emotional concerns were reported for 2 out of 3 three year olds and 7 out of 34 four year olds. In the study population, half of the parents of 4 year old females had reported crying issues, while parents of one 3 year old and one 4 year old reported sleep issues. Parents of 13, 14, and 16 year old subjects reported the least emotional concerns. The greatest concern was in the 3 year old and 15 year old group. However, the groups were limited in size in these age ranges.
Anecdotally, a significant number of parents ultimately reported that they felt their children were more well-rested, and required less sleep. It is interesting to note that crying was reported by both males and females. Of the entire subject population, fewer males (1 male) (.008%) than females (10 females) (.031%) demonstrated crying behavior.
Reports of emotional concerns were of short term duration. It is felt that these emotional responses impacted the risk reward factor quite favorably. This was most evident by parent survey responses that indicated that even though some emotional consequences were experienced by their children, the consequences were of a short-term duration. All of the parents stated they would recommend the program and all parents stated they thought the program was worthwhile. In particular, when asked if the program participation let to increased self-confidence and self-esteem, 97.27% of parents responded ‘Yes’. This favorable response is well worth the administration of this program, in this author’s opinion.
Unexpected outcomes
Miscellaneous notations in the findings section regarding chained habits indicated 80% cessation of chained trichotillomania, and 100% for chained pathological skin picking behavior. All of the children in this study with a concomitant chained trichotillomania or skin picking habit remediated their digit sucking habit immediately. A sucking habit program does not take the place of psychological services and medical follow up for children who demonstrate a chained behavior, but can add a dimension to the potential success in a team approach.
COMPARING CURRENT STUDY RESULTS TO VAN NORMAN’S 1997 RESULTS
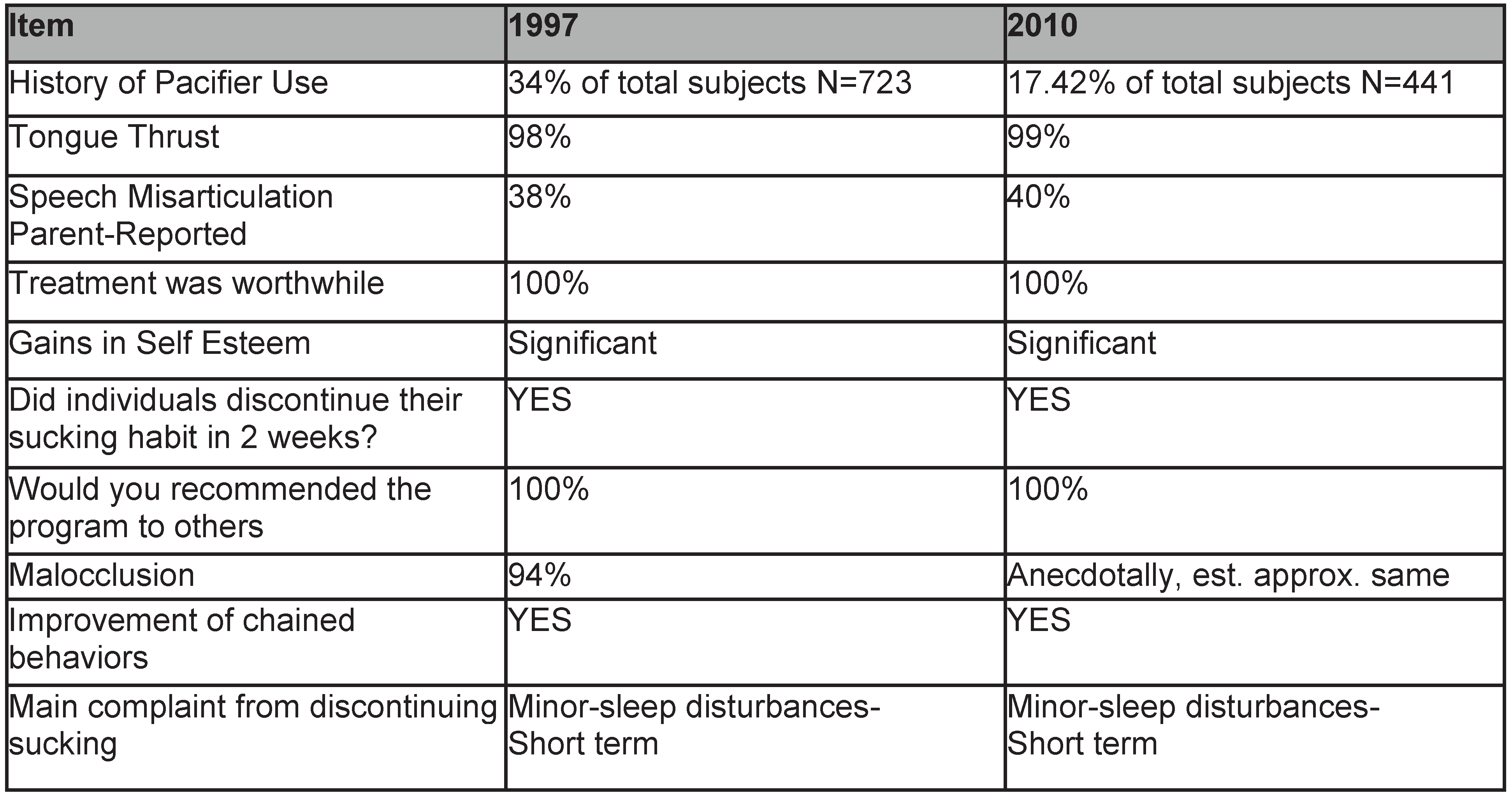
The results of the 1997 study by VanNorman were replicated almost exactly when compared with the current study, with the exception of reported pacifier use (
Table 1.). This may be attributed to increased parental awareness of the negative effects of using a pacifier since the 1997 study was completed. There may also be differences in cultural use of the pacifier in Van Norman’s region of the country which was Nebraska when compared with the current study population location in Chicago. This author also postulates that there may have been increased incidence of breastfeeding since Van Norman’s study, which may have contributed a reduction in the use of a pacifier. However, this author does question why there was not an increased report of pacifier use due to the recent AAP recommendations on pacifier use since the Van Norman study. Otherwise, the current study does confirm Van Norman’s results.
Tongue thrust or low rest posture of the tongue is enjoying increased recognition in the research community as a related factor in malocclusion in children with sucking habits. Ovsenik (2009) recommends children with a history of sucking habits be assessed for swallow pattern and orofacial myofunctional issues. This current study and that of Van Norman (1997) provide confirmation of the importance of Ovsenik’s recommendations. Documentation of the presence of tongue thrust and myofunctional concerns through clinical assessment is provided for over 723 clients by Van Norman, and 441 in this study, and confirm, in this author’s opinion, the necessity for myofunctional assessment in the digit sucking child.
Both Van Norman’s 1997 study and the current study on sucking habits reported an extremely high percentage of tongue thrust/low or forward rest posture of the tongue (98% and 99% respectively). It is this author’s belief, based on these two studies, that tongue thrust is an expected observation for the majority of children with retained sucking habits who are older than 3.5 years of age.
However, one must consider that it is normal to exhibit a tongue thrust behavior up to approximately 6 years of age, when a natural transition to a more adult swallow usually occurs. It is when this natural developmental transition fails to occur after age 6 that this author becomes concerned. Van Norman concluded that malocclusion was present in 94% of her participants, and anecdotally, although not a dentist, this author supports a similar suspected observation.
Ovsenik (2009) found that swallow pattern played a role in the development of posterior crossbite, and in particular in those with a history of sucking habits. He suggests that children should be assessed for swallow patterns as a result of these findings. Melink, Vagner, Hocevar, and Ovsenik (2010) suggest low rest posture of the tongue due to the duration of sucking habits, and short lingual frenum are associated with the presence of unilateral posterior crossbite in the 4 to 5 year old child. They conclude that more research would be beneficial to determine the relationship between swallow pattern, tongue posture, and lingual frenum issues in the child with a posterior crossbite. This author postulates that as further research continues in this area, the importance of addressing not only the retained sucking behavior but the swallow or rest posture of the tongue will emerge.
The true implications of comparing the Van Norman study with the current study are the core similarity of the two studies: presence of speech errors, increased self-esteem, improvement of chained behaviors, similar complaints of emotional issues when present. Looking at the overall impact, professionals now have over twenty five years of extremely detailed documentation from two independent studies from which to draw. The similarity in outcomes are too similar to be coincidental, and to important to ignore.