Lip-Closing Function of Elderly People During Ingestion: Comparison with Young Adults
Abstract
:INTRODUCTION
METHODS
Subjects
Measurement method of labial pressure during ingestion
Data Analysis
RESULTS
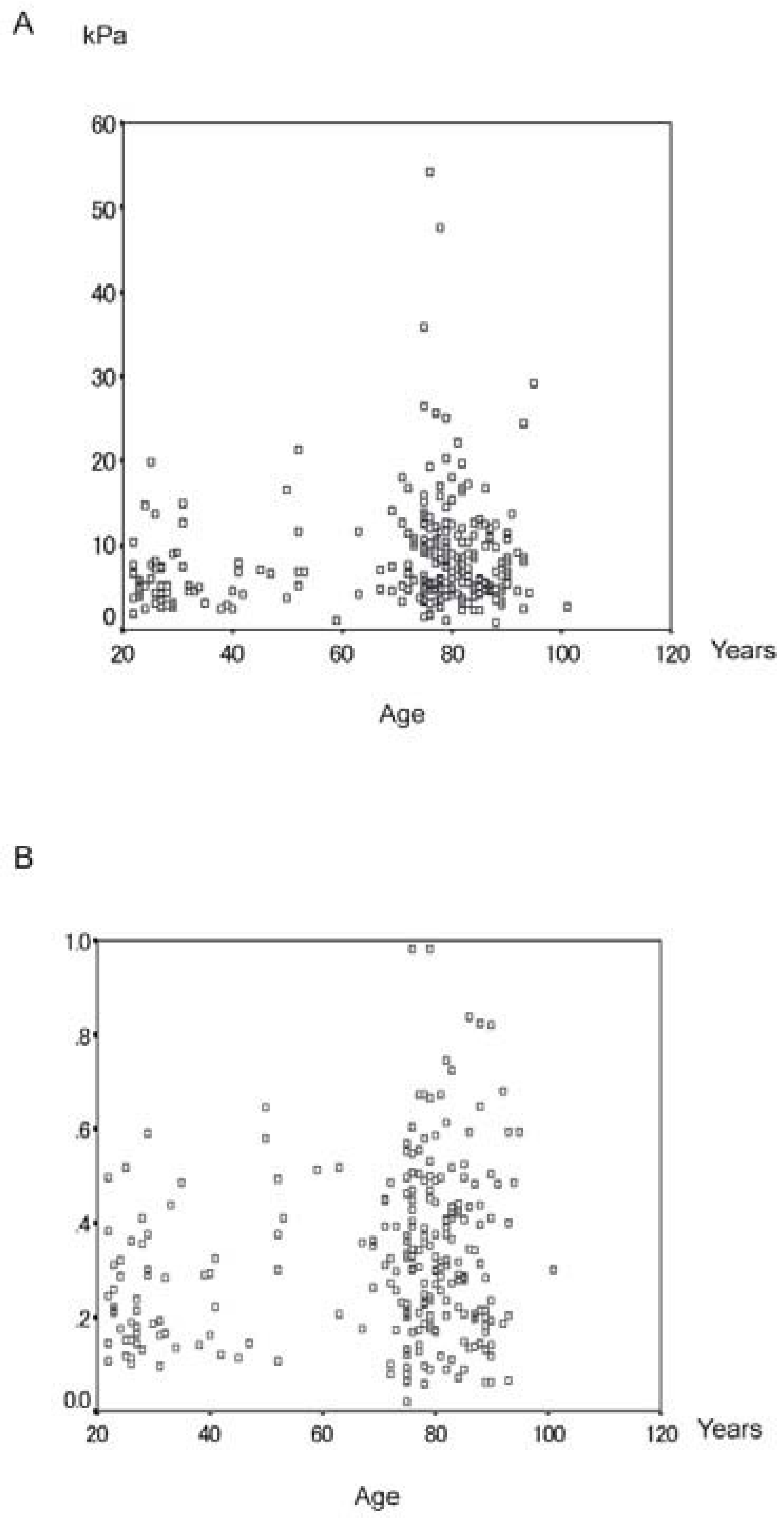
Relationship between measurement results and age
- 1)
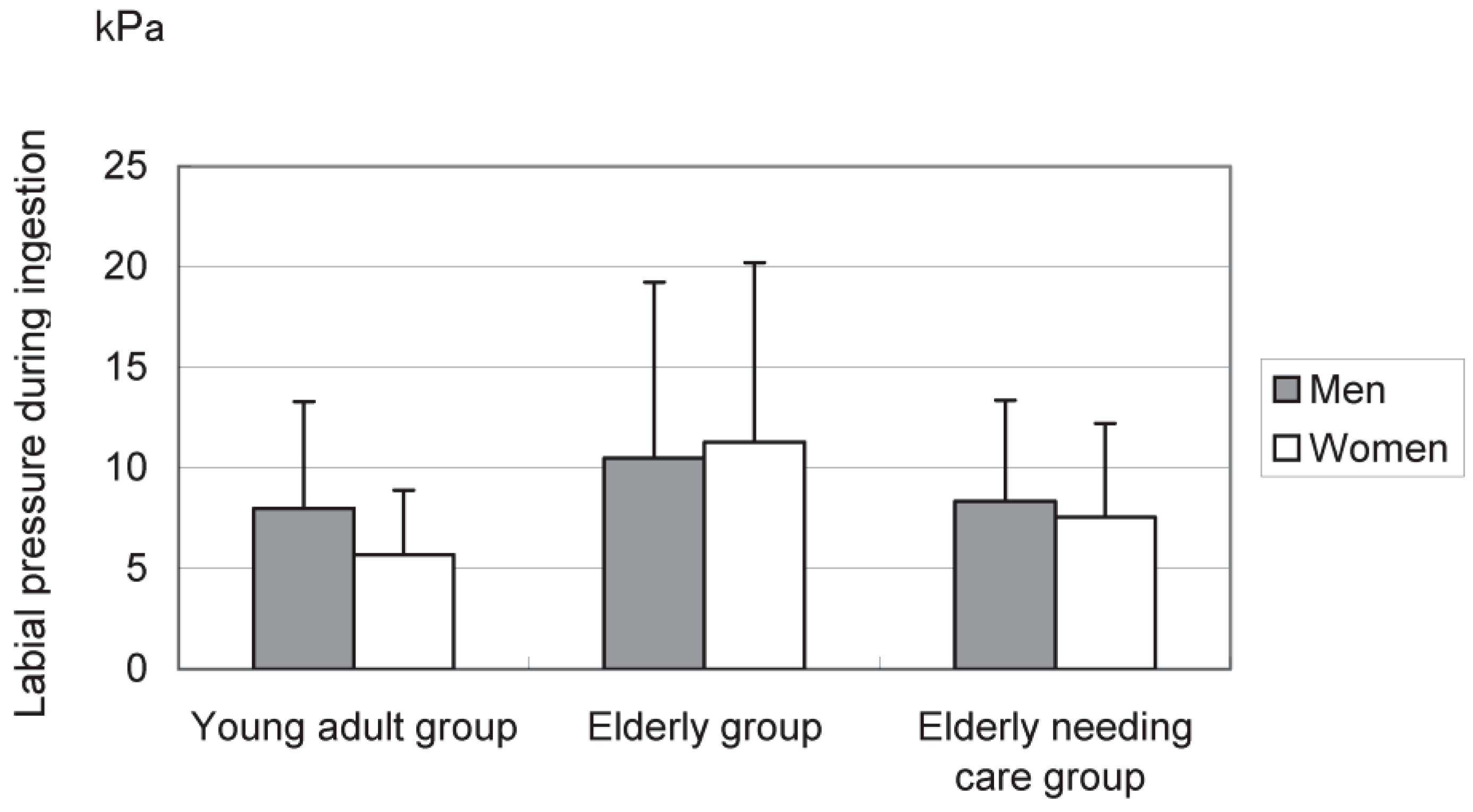
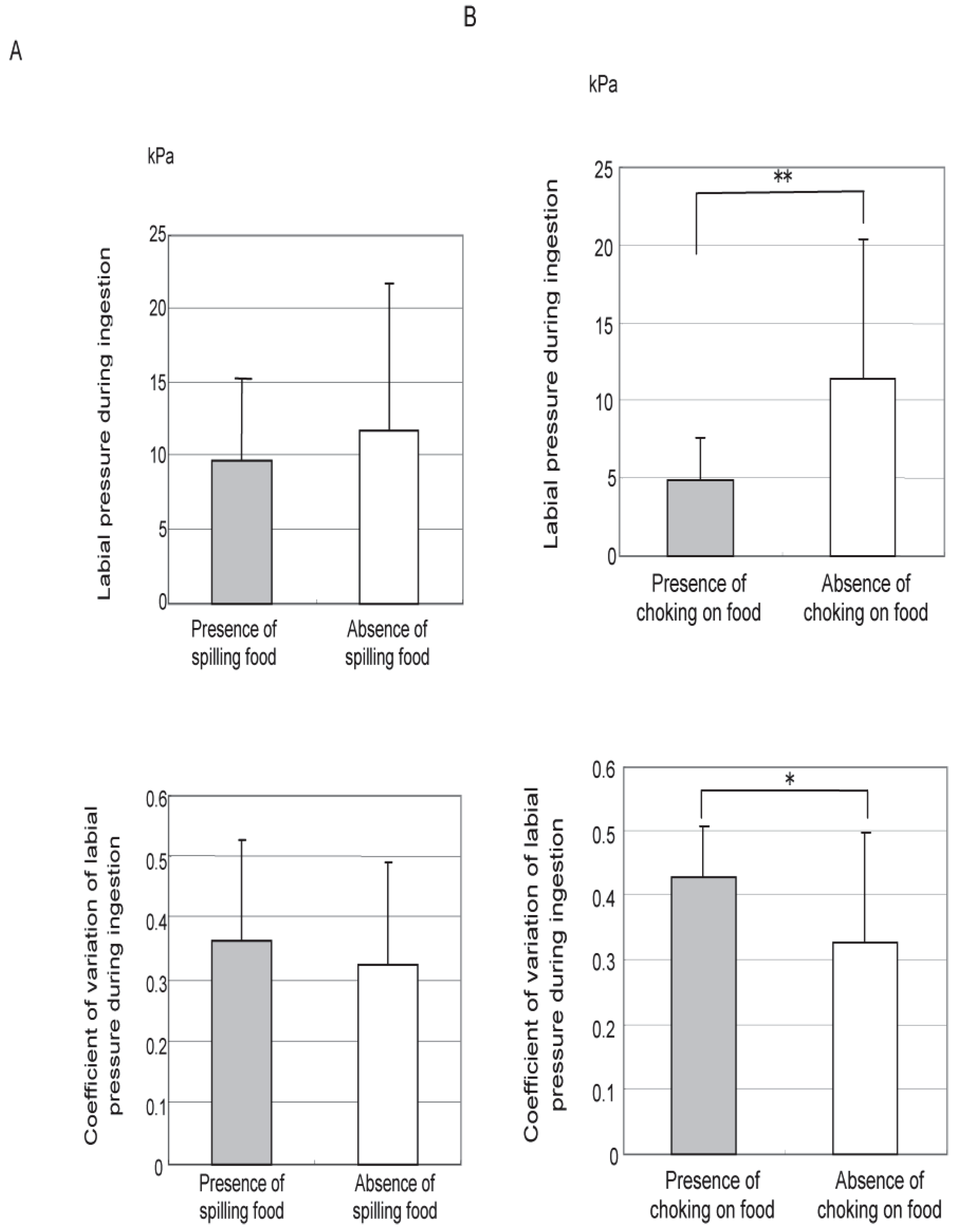
- Labial pressure during ingestion The mean value of labial pressure during ingestion was 6.6 ± 4.2 kPa in the control group (men: 8.0 ± 5.3, women: 5.7 ± 3.2), 11.2 ± 8.9 in the elderly group (men: 10.5 ± 8.7, women: 11.3 ± 8.9), and 7.9 ± 4.8 in the elderly needing care group (men: 8.5 ± 5.0, women: 7.6 ± 4.7). There was no significant difference in sex among all groups (Fig. 4).
- 2)
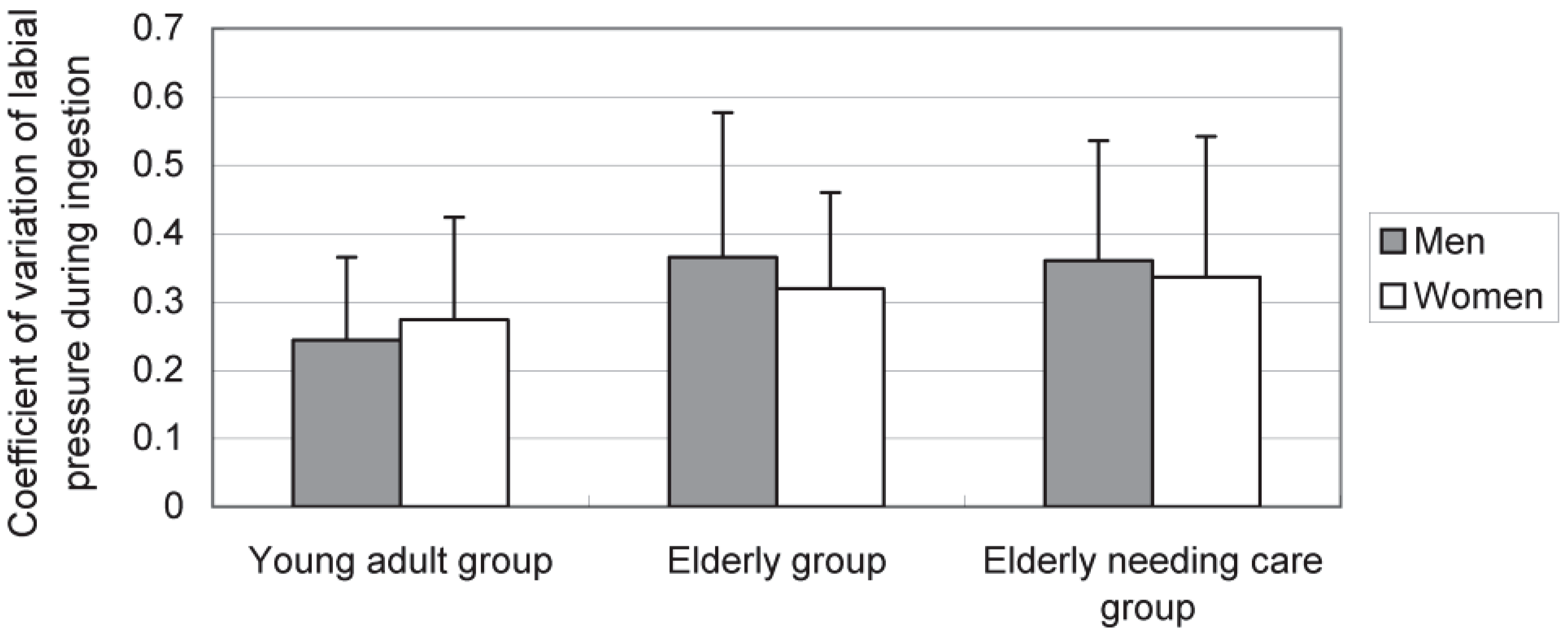
- Coefficient of variation The mean value of the coefficient of variation of labial pressure during ingestion was 0.26 ± 0.14 in the control group (men: 0.25 ± 0.12, women: 0.27 ± 0.21), 0.34 ± 0.17 in the elderly group (men: 0.37 ± 0.21, women: 0.32 ± 0.14), and 0.34 ± 0.19 in the elderly needing care group (men: 0.36 ± 0.18, women: 0.34 ± 0.21). There was no significant difference in sex among all groups (Fig. 5).
DISCUSSION
CONCLUSION
Funding
Acknowledgments
REFERENCES
- Baum, B.J., and L. Bodner. 1983. Aging and oral motor function: evidence for altered performance among older persons. Journal of Dental Research 62: 2–6. [Google Scholar] [CrossRef] [PubMed]
- Chigira, A., K. Omoto, Y. Mukai, and Y. Kaneko. 1994. Lip closing pressure in disabled children: a comparison with normal children. Dysphagia 9: 193–198. [Google Scholar] [CrossRef] [PubMed]
- Eichner, K. 1955. Über eine Gruppeneinteilung der Lunckengebisse für die Prothetic. Deutsche Zahnarztliche Zeitschrift 10: 1831–1834. [Google Scholar]
- Floystrand, F. 1986. Vestibular and lingual muscular pressure on complete maxillary dentures. Acta Odontologia Scandinavica 44: 71–75. [Google Scholar] [CrossRef] [PubMed]
- Fucile, S., P.M. Wright, I. Chan, S. Yee, M.E. Langlais, and E.G. Gisel. 1998. Functional oral-motor skills: Do they change with age? Dysphagia 13: 195–201. [Google Scholar] [CrossRef] [PubMed]
- Inagaki, A. 1993. Development of an estimation method of body fat percentage using body mass index, physical strength diagnosis/test for ability to exercise: for junior high school students. The Japanese Journal of Behaviormetrics 20: 8l–91, [in Japanese]. [Google Scholar]
- Kaneko, Y., Y. Mukai, and K. Omoto. 1987. Impairment of eating function. Tokyo: Ishiyaku Publishers, [in Japanese]. [Google Scholar]
- Kawamura, Y. 1979. Oral Physiology for Dental University Students. Tokyo: Nagasue Syoten, [in Japanese]. [Google Scholar]
- Kikutani, T., R. Enomoto, F. Tamura, K. Oyaizu, and A. Suzuki I. 2006. Effects of oral functional training for nutritional improvement in Japanese older people requiring long-term care. Gerodontology 23: 93–98. [Google Scholar] [CrossRef] [PubMed]
- Leopold, N.A., and M.C. Kagel. 1983. Swallowing, ingestion and dysphagia: a reappraisal. Archives of Physical Medicine and Rehabilitation 64: 371–373. [Google Scholar] [PubMed]
- McHenry, M.A., J.T. Minton, L.L. Hartley, K. Calhoun, and S.S. Barlow. 1999. Age-related changes in orofacial force generation in women. Laryngoscope 109: 827–830. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.G., A. Barnes, and J. Newman. 1983. A study of bilabial lip pressure in a normal population. Australian Orthodontic Journal 8: 51–55. [Google Scholar] [CrossRef] [PubMed]
- Ono, T., K. Hori, and T. Nokubi. 2004. Pattern of tongue pressure on hard palate during swallowing. Dysphagia 19: 259–264. [Google Scholar] [CrossRef] [PubMed]
- Sheth, N., and W.C. Diner. 1988. Swallowing problems in the elderly. Dysphagia 2: 209–215. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M., and Y. Mukai. 2002. Relationship between labial pressure/buccal pressure and lip movement in pointing movement. Pediatric Dental Journal 40: 64–76, [in Japanese]. [Google Scholar]
- Tamura, F., and S. Suzuki. 2004. Effects of edentulisum on lingual functions during swallowing. Journal of International Association for Disability and Oral Health 5: 83–87. [Google Scholar]
- Tamura, F., K. Tomita, T. Okano, M. Mizukami, T. Kikutani, and Y. Mukai. 2004. Effect of the presence or absence of full dentures on labial pressure of edentulous patients at the time of swallowing. Japanese Journal of Gerodontology 19: 169–173, [in Japanese]. [Google Scholar]
- Tomita, K., T. Okano, F. Tamura, and Y. Mukai. 2002. Relationship between labial pressure and maximum labial pressure at the time of swallowing - Comparison between the elderly and adults. Japanese Journal of Dysphagia Rehabilitation 6: 19–26, [in Japanese]. [Google Scholar]


| Care level | Criteria for care level |
|---|---|
| Needing support 1 | Slight decline in physical function in some activities of daily living due to impairment, but will improve with preventive support. |
| Needing support 2 | Partial decline in physical function in some activities of daily living due to impairment, but will improve with preventive support. |
| Needing care 1 | Observation and/or assistance needed for all activities of daily living. Support needed for standing up and walking. |
| Needing care 2 | Observation and/or assistance needed for all activities of daily living. Support needed for standing up and walking. Observation and/or assistance needed for eating and toileting. |
| Needing care 3 | Cannot take care of oneself or stand up by oneself. General care needed for toileting, etc. |
| Needing care 4 | Considerable decrease in activities of daily living. General care often needed. Problematic behavior or decreased comprehension. |
| Needing care 5 | Significant decrease in activities of daily living. General care needed. Much problematic behavior or significantly decreased comprehension. |
© 2009 by the author. 2009 Fumiyo Tamura, Tomoko Fukui, Takeshi Kikutani, Reiko Machida, Mitsuyoshi Yoshida, Takeyoshi Yoneyama, Akira Hamura
Share and Cite
Tamura, F.; Fukui, T.; Kikutani, T.; Machida, R.; Yoshida, M.; Yoneyama, T.; Hamura, A. Lip-Closing Function of Elderly People During Ingestion: Comparison with Young Adults. Int. J. Orofac. Myol. Myofunct. Ther. 2009, 35, 33-43. https://doi.org/10.52010/ijom.2009.35.1.3
Tamura F, Fukui T, Kikutani T, Machida R, Yoshida M, Yoneyama T, Hamura A. Lip-Closing Function of Elderly People During Ingestion: Comparison with Young Adults. International Journal of Orofacial Myology and Myofunctional Therapy. 2009; 35(1):33-43. https://doi.org/10.52010/ijom.2009.35.1.3
Chicago/Turabian StyleTamura, Fumiyo, Tomoko Fukui, Takeshi Kikutani, Reiko Machida, Mitsuyoshi Yoshida, Takeyoshi Yoneyama, and Akira Hamura. 2009. "Lip-Closing Function of Elderly People During Ingestion: Comparison with Young Adults" International Journal of Orofacial Myology and Myofunctional Therapy 35, no. 1: 33-43. https://doi.org/10.52010/ijom.2009.35.1.3
APA StyleTamura, F., Fukui, T., Kikutani, T., Machida, R., Yoshida, M., Yoneyama, T., & Hamura, A. (2009). Lip-Closing Function of Elderly People During Ingestion: Comparison with Young Adults. International Journal of Orofacial Myology and Myofunctional Therapy, 35(1), 33-43. https://doi.org/10.52010/ijom.2009.35.1.3




