Abstract
This prospective study was designed to evaluate a new concept of myofunctional therapy in comparison with conventional myofunctional therapy. 45 children aged three to sixteen years in need of myofunctional therapy were randomly divided into two groups: 19 children were referred to myofunctional therapy in private practices in Hamburg and served as controls. The remaining 26 children were treated with face former therapy at the Department of Orthodontics by a medical assistant specializing in myofunctional therapy. The overall observation time was six months. Every three months an overall clinical assessment was performed at the Department of Orthodontics by a speech pathologist and an orthodontist, who documented the clinical situation. The clinical examination included measurement of lip strength, palatography to document the swallowing pattern, logopedic diagnosis, and an orthodontic examination with reference to a standardized diagnostic sheet. In all children’s orofacial function could be improved. Children treated with the Face Former showed a statistically significantly improvement in palatal tongue position during swallowing. They achieved stronger lip pressure within a shorter time than children who did not use the Face Former. However, at the end of the observation time there was no statistically significant difference in lip strength between the two groups. Habitual mouth closure was also achieved within a shorter time for children treated with the FaceFormer than children with myofunctional therapy. Face Former therapy seems to offer a good alternative to conventional myofunctional therapy. Longitudinal studies will follow to judge whether the established orofacial balance could be stabilized, i.e. the established physiological orofacial function becomes automatic.
INTRODUCTION
Orofacial dysfunctions such as a visceral swallowing pattern or habitual mouth breathing inhibit the physiological development of the jaw and dentition (Bertolini and Paschoal, 2001; Garetto, 2001; Josell SD, 1995) and may have a negative impact on speech development (Biegenzahn, Fischman and Mayrhofer-Krammel, 1992). Persistent orofacial dysfunctions lead to instability within the orofacial system (Benkert, 1997) and are discussed in this context both as a cofactor in the pathogenesis of malocclusion and, in persistent cases, as a possible cause of relapse after orthodontic therapy (Khinda and Grewal, 1999).
Myofunctional therapy (MFT) was developed with the aim of harmonizing orofacial functions. Today, a large number of different therapy concepts are reported in the literature (Bacha and Rispoli, 1999; Umberger and Johnston, 1997; Krüger and Tränkmann, 1997); these distinguish between individual or group therapy and the type of exercises, depending on the patient’s age at the start of therapy (from three years to adulthood). The primary therapeutic objectives of all known approaches are strengthening of the orofacial muscles to pave the way for mouth closure, establishment of nasal breathing, and learning a physiological swallowing pattern. According to a study carried out among speech/language pathologists in the Hamburg region of Germany, up to 18 months have to be scheduled for harmonization of orofacial functions after the initial diagnosis (Klocke, Korbmacher and Kahl-Nieke, 2000). This period comprises an average waiting time of six months for new referrals before the start of therapy and a mean treatment duration of less than one year.
As an active exercise concept, MFT is crucially dependent on compliance on the part of the patient and on the part of the parents (Marchesan, 2000). While good compliance is more likely, if the patient has a fundamental psychological understanding of the reasoning and objectives underlying the daily exercises, such an understanding is not always present.
Although first results of MFT were published in the early 20th century, the rationale and benefit are a matter of controversial discussion. Critics point out that, even today, there is inadequate scientific evidence of a permanent change in function (Sergl, 1988). It is for this reason too that the statement published by the German Orthodontic Society in 1988 (Schopf, 1988) on MFT has yet to be revised.
The aim of the present prospective clinical study was to evaluate any changes in the orofacial system during MFT. In particular, a newly developed appliance-based therapy concept, Face Former Therapy (FFT) was to be compared with conventional MFT as performed by speech/language pathologists with a supplementary qualification.
PATIENTS AND METHODS
All 45 patients enrolled in this study had been referred to the Department of Orthodontics, University of Hamburg. Inclusion criteria were multiple untreated orofacial dysfunctions and further ongoing treatments (orthodontic therapy, ergotherapy, physiotherapy). The patients were randomized to an MFT group (19 patients: 4 female, 15 male) and an FFT group (26 patients: 9 female, 17 male). The MFT group served as the control group and the FFT group as the study group. The two groups were statistically comparable with respect to age and gender distribution and to the extent of findings reported by orofacial specialists, orthodontists and speech/language pathologists. The mean age at baseline (T0) was 8.4 years in the MFT group and 8.3 years in the FFT group (Table 1). The researchers did not know to which group (MFT, FFT) the children belonged.
Within the framework of this study, all patients were clinically examined by an orthodontist and a speech/language pathologist at three-month intervals: T0 = baseline, i.e. before the start of MFT or FFT, T1 = three months after the start of therapy, and T2 = six months after the start of therapy. At all three time points the examination covered extraoral and intraoral findings, the diagnosis by the speech pathologist, a parent and patient interview, lip strength measurement, and palatography. At none of the examinations could conclusions be drawn on the group membership of the respective children (MFT or FFT group). The clinical examination was performed with reference to a standardized diagnostic sheet for patients with orofacial dysfunctions (Korbmacher and Kahl Nieke, 2001). Standardized extraoral and intraoral clinical photos at rest and in function (swallowing) were taken for documentation purposes.
A dental assistant conducted the FFT under the supervision of a dentist. The dental assistant and the dentist attended training courses in myofunctional therapy and special courses on the Face-Former therapy. Both had been working on myofunctional disorders for more than two years.
Criteria
The present publication deals with therapeutically induced changes concerning the following four criteria:
- Breathing: Organically induced mouth breathing, allergies and/or asthma were ruled out at baseline in all children with the finding “mouth breathing“. Before each clinical examination the mode of breathing was assessed. The children were unaware of being observed. Signs of habitual mouth breathing such as a continuously open mouth and cracks at the corners of the mouth were also recorded on the diagnostic sheet. The findings were supplemented by questioning both the parents and the children on the mode of breathing during the day and at night.
- Lip strength: Lip strength was measured with a Myo-Bar-Meter® (Akkuphon, Unna, Germany), a digital precision pressure gauge with a piezoresistive relative-pressure sensor. The measuring principle is based on overpressure measurement. The measured values provide information on the development of lip strength and thus on lip competence. Three measurements per patient were made at each examination time point, with lip competence being clinically rated.
- Swallowing pattern: Within the scope of the initial diagnosis, morphological factors impairing proper tongue position, e.g. a shortened frenulum or enlarged tonsils, were ruled out in all children. The existing swallowing pattern was assessed by clinical examination during mastication and speech and by means of palatography (Engelke, Engelke and Schwestka, 1990). After application of a paste to the tip and lateral edges of the tongue, the patient was asked to swallow. The color impressions were rated visually and documented by means of photos taken immediately thereafter.
- Sigmatism: This examination unit was performed exclusively by the speech/language pathologist. Within the scope of a conventional diagnosis by the speech/language pathologist (visual rating of the movement pattern during /s/ sound formation and acoustic rating), irregular /s/ sound formation was rated, followed by the movement pattern during articulation of the phonemes l, n, t, and d.
- Dropout rate28 patients attended all three scheduled examinations, 10 attended only the baseline diagnostic examination, and 17 failed to attend at least one examination. The loss of data within the individual groups is shown in Table 2. The most frequent reason given for absence was illness, holidays or lack of time on the part of the parents.

Table 1.
Age structure within the individual groups.
Table 1.
Age structure within the individual groups.
| Mean age (months) | Minimum age (months) | Maximum age (months) | Standard deviation (± months) | |
| Control group | 101 | 55 | 203 | 35 |
| Study group | 100 | 47 | 190 | 38 |
Therapy Concepts
Control group: At T0 the children in the control group started conventional myofunctional therapy at practices run by speech/language pathologists in the Hamburg region. The therapy concept applied could be stipulated individually by the respective therapist. The therapy concepts selected by speech/language pathologists were based on the approaches of Kittel, Grums and Garliner. None of the control children was treated with the Face Former or another orthodontic appliance.
Study group: Face Former therapy consists of tongue and lip exercises using a training device. The flexible silicone appliance (Face Former, Akkuphon®, Unna, Germany) is inserted in the oral vestibulum, behind the lips in front of the teeth. This makes the lips protrude slightly and directs the lip wedge outwards. During the exercises, the neck is extended, i.e. the angle between chin and neck is 90 degrees, and the tongue should assume a palatal position [Figure 1]. When necessary, supplementary tongue exercises such as “Assuming the Rest Position“ and “Pressing the Tongue against the Palate” should be performed prior to the exercises with the appliance in situ. The basic exercise with the Face Former comprises active compression of the lip wedge with the lips for six seconds; this is followed by a six-second relaxation phase. A training cycle comprises 20 repetitions and is performed three times a day. The other exercises are modifications of the basic exercise, with the lip wedge of the Face Former being drawn upwards, forwards or downwards during lip compression. After a three-week training period the appliance is worn overnight.

Table 2.
Dropout rate within the individual groups.
Table 2.
Dropout rate within the individual groups.
| Group | N = | Missing | |
|---|---|---|---|
| T0 | control | 19 | 0 |
| study | 26 | 0 | |
| total | 45 | 0 | |
| T1 | control | 14 | 5 |
| study | 19 | 7 | |
| total | 33 | 12 | |
| T2 | control | 13 | 6 |
| study | 17 | 9 | |
| total | 30 | 15 |
At six-week intervals the patients were recalled to the Department of Orthodontics for an exercise control and remotivation. The controls were performed by a dental assistant under the supervision of a dentist.
Statistical Analysis
Evaluation of the data material was based on two different approaches. The first approach was a comparison of patient characteristics between the MFT and FFT groups at one of the three respective time points. This related to those patients who had taken part in the measurements at the time point concerned.
The second approach was based on a statistical analysis of the characteristics of only one group across the measuring time points in a repeat-measurement design. This took account of only those patients who had been present at all three measuring time points (T0, T1, T2) (n=28) The 28 children who had been present at all three measuring time points included: 13 children from the MFT group; and 15 patients from the FFT group.
In some cases the interval scale level of the data permitted a two-way analysis of variance (ANOVA) with repeat measurement to be performed. Both samples could thus be examined simultaneously across the measuring time points.
Patients who had attended only the baseline examination (T0) were considered. However, information is provided on these patients in purely descriptive terms.
In accordance with the hypotheses, an advantage of FFT over MFT had been assumed for the individual statistical analyses set out below. For this reason the hypotheses were tested unilaterally. A further assumption was that both therapeutic approaches would result in an improvement, so that unilateral significance tests were performed here too as far as possible.
In compliance with the statistical convention, the result was considered statistically significant from a value of p ≤ 0.05 (*), and as statistically highly significant from p ≤ 0.01 (**).
The statistical tests used were:
- 2-way ANOVA with repeat
- measurement Friedman test
- Wilcoxon test
- Mann-Whitney U test
- Chi-square test
RESULTS
Breathing
In the total collective a highly significant success in overcoming the habit of mouth breathing was recorded during the six-month treatment period (Table 3). However, the crucial factor in the treatment success was the type of therapy performed. Only the therapeutic approach within the study group was statistically highly significantly efficient in changing the breathing mode, whereas changes within the control group failed to reach statistical significance (p=0.097). The course of the change in breathing mode is detailed below:
- At time point T0, 91.1% (41/45) of all examined children were habitual mouth breathers. This habit was observed in 94.7% (18/19) of the children in the control group [Figure 2a] and in 88.5% (23/26) of those in the study group [Figure 2b]. The significance value of p= 0.627 confirms that the two treatment groups were statistically comparable with each other at time point T0 [Table 3].
- At time point T1, 33.3% (11/33) of all children were already breathing through their nose, meaning that mouth breathing was still observed in 66.7% (22/33). The habitual mouth breathing had not been changed in 85.7% (n=12) of children in the control group and in 52.6% (n=10) of those in the study group. In the comparison of the two patient collectives at time point T1, the chi-square test revealed a statistical trend with a significance value of p=0.051.
- At time point T2, 43.3% (13/30) of the patients were still observed to be habitual mouth breathers. At this time point the intergroup difference was statistically significant (p=0.016): Continued habitual mouth breathing was recorded in 69.2% (9/13) of those in the control group and in 23.5% (4/17) of those in the study group.
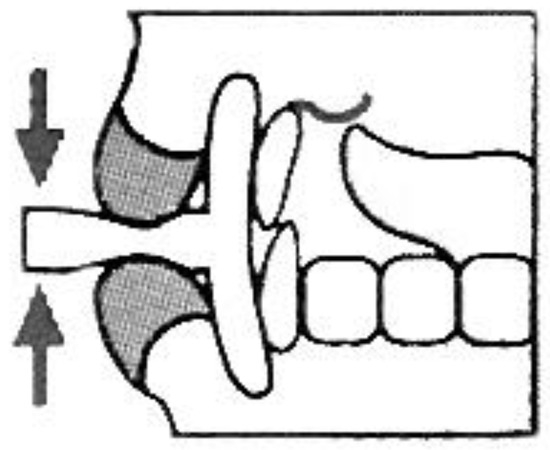
Figure 1.
Basic Exercise in Face Former Therapy. The Face Former is inserted in the vestibulum in front of the teeth, the tongue assumes the rest position, and the lips actively compress the lip wedge.
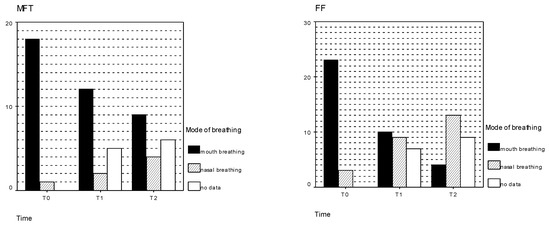
Figure 2.
a and b Mode of Breathing. Mode of breathing at all three measuring time points, differentiated for the MFT and FFT Groups.

Table 3.
Percentage of children with habitual mouth breathing at all three measuring time points in each group and in the total collective, plus statistically determined significances.
Table 3.
Percentage of children with habitual mouth breathing at all three measuring time points in each group and in the total collective, plus statistically determined significances.
| Control group | Study group | Total | ||
|---|---|---|---|---|
| T0 | 94.7% | 88.5% | 0.627 | 91.1% |
| T1 | 85.7% | 52.6% | 0.051 | 66.7% |
| T2 | 69.2% | 23.5% | 0.016* | 43.3% |
| p=0.097 | p=0.001** | p=0.000** |
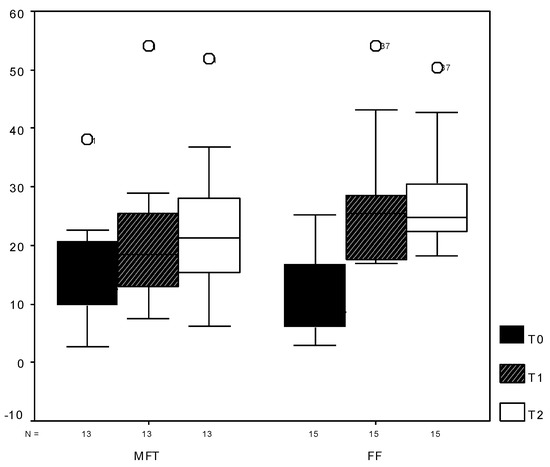
Figure 3.
Data Analysis. Box plots showing the statistical analysis of the data from the Myo-Bar-Meter® measurements at all three measuring time points.
Development of Lip Strength
The assessment of the therapy with respect to increased lip strength took account of only those patients present at all measuring time points (13 in the control group, 15 in the study group) [Figure 3].
An analysis of the values at time point T0 using the nonparametric Mann-Whitney U test to check for any differences between the samples prior to treatment confirmed at a level of p=0.441 that there was no significant intergroup difference.
A statistically highly significant increase in lip strength over the three time points was established for both therapeutic approaches by means of one-way ANOVAs with repeat measurement [Table 4a].
Differences between the therapeutic approaches were observed over time in the course of lip strength development [Figure 4]. At p=0.009, a 2-way ANOVA with repeat measurement showed a highly significant change in group/time interaction in both groups during therapy. However, no significant intergroup difference was ascertained in the group factor over the duration of treatment [Table 4b]. In other words, at T2 there was no statistically significant difference in lip strength. However, the FFT reached the improvement level within a statistically significant shorter time frame.
Swallowing Pattern
Despite differentiated division of tongue positions during swallowing, the diagnosis was reduced to a division between “physiological“ and “pathologic“ swallowing pattern for purposes of statistical analysis. A tongue thrust swallow pattern was thus recorded for all patients at time point T0.
The Friedman test revealed a highly significant improvement in the swallowing pattern of all patients in the total collective, irrespective of the type of therapy. Separated according to type of therapy, the individual tests revealed a statistically highly significant improvement (p=.000) in the study group, whereas no statistically significant improvement was recorded in the control group (p=0.097). (Please see Table 5).
Initial statistically significant differences between the therapeutic approaches (p=0.028) were determined with the chi-square test at time point T2. A tongue thrust swallow pattern was registered palatographically in 76.9% (10/13) of those in the control group versus 35.3% (6/17) in the study group. Figure 5a and b gives a more differentiated representation of the change in swallowing pattern in the two groups.
Sigmatism
No statistically significant improvement could be registered for patients, in regard to the type of therapy they received – FFT or MFT, within the six-month observation period [Table 6]. At none of the measuring time points did the chi-square test reveal any differences between the two therapeutic approaches.
DISCUSSION
The results of the present study indicate that orofacial dysfunctions can be harmonized by means of myofunctional therapy concepts. Within the six-month observation period, statistically highly significant results were registered in the population as a whole in the following areas: establishment of nasal breathing in cases of previous habitual mouth breathing, increased lip strength paving the way for competent lip closure, and establishment of a physiological swallowing pattern. Only in the correction of existing sigmatism were no statistically significant changes recorded.
Consideration of the therapy concepts in detail reveals clear-cut differences between the individual approaches. Face Former Therapy appears to be more successful in establishing nasal breathing and a physiological swallowing pattern within a six-month period. A statistically highly significant improvement in both criteria was recorded in the FFT group, whereas the change in these two criteria in the MFT group fell short of significance level (p=0.097 in each case).
The observed improvement both in mouth breathing and in swallowing pattern underlines the interaction reported in the literature between persistent mouth breathing and tongue thrust swallow pattern, and thus the influence of respiratory mode on the establishment of a physiological swallowing pattern (Marchesan and Hubermann-Krakauer, 1996; Pierce, 1983). According to Marchesan and Hubermann-Krakauer (1996) the relapse of a corrected swallowing pattern is often due to failure to correct mouth breathing.

Table 4a.
Highly significant changes in lip strength confirmed in both the control group and the study group by one-way ANOVAs.
Table 4a.
Highly significant changes in lip strength confirmed in both the control group and the study group by one-way ANOVAs.
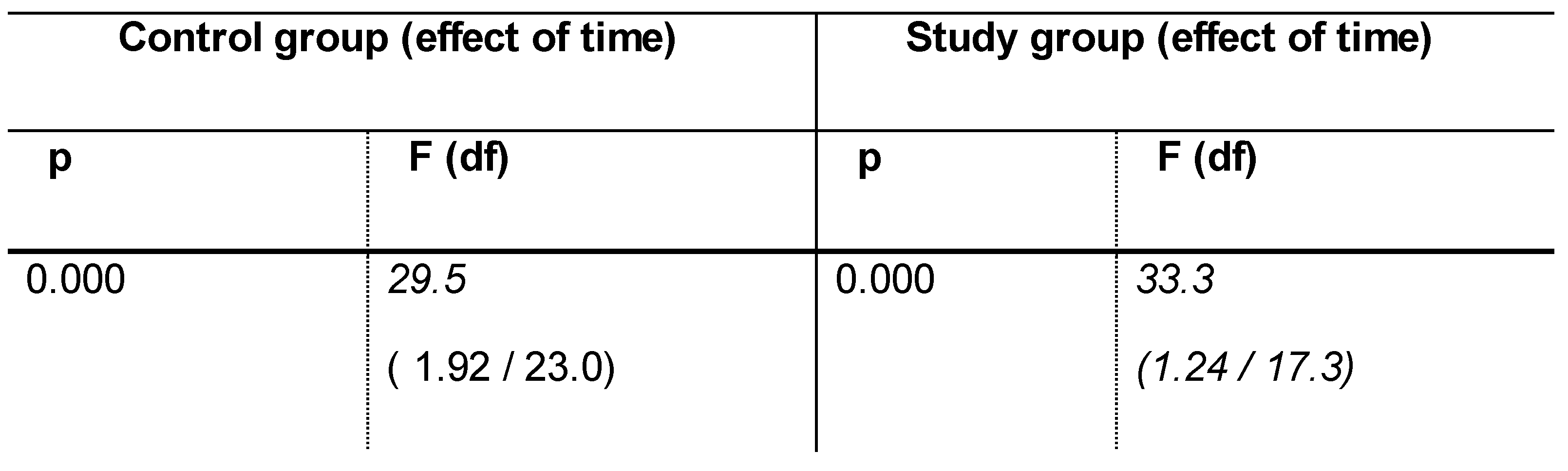

Table 4b.
As no sphericity could be assumed, significance testing was performed using degrees of freedom determined by means of Greenhouse-Geisser correction: highly significant change (p=0.000) in both groups during treatment in the time effect, no significant intergroup differences (p=0.51) in the group factor during treatment, significant intergroup difference (p=0.009) in the development over time.
Table 4b.
As no sphericity could be assumed, significance testing was performed using degrees of freedom determined by means of Greenhouse-Geisser correction: highly significant change (p=0.000) in both groups during treatment in the time effect, no significant intergroup differences (p=0.51) in the group factor during treatment, significant intergroup difference (p=0.009) in the development over time.
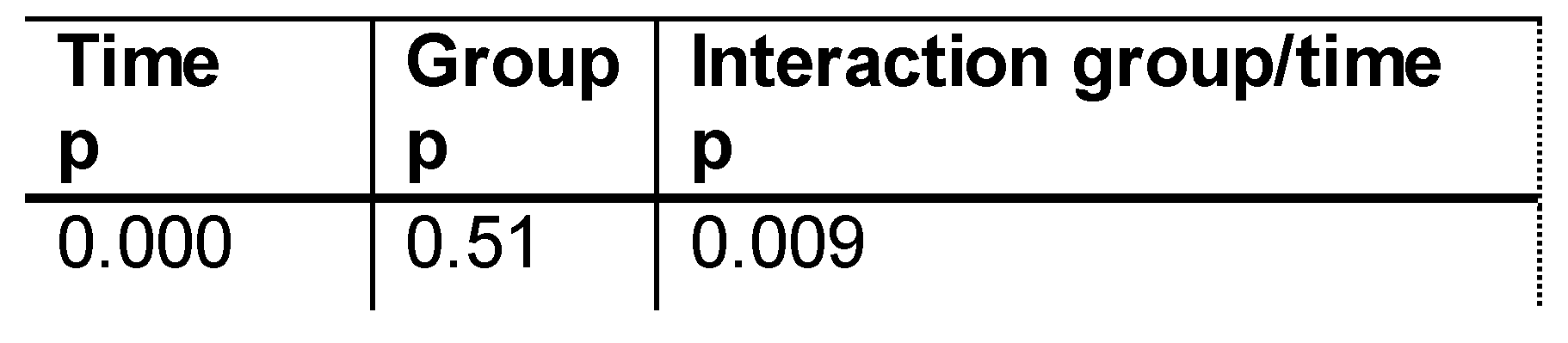
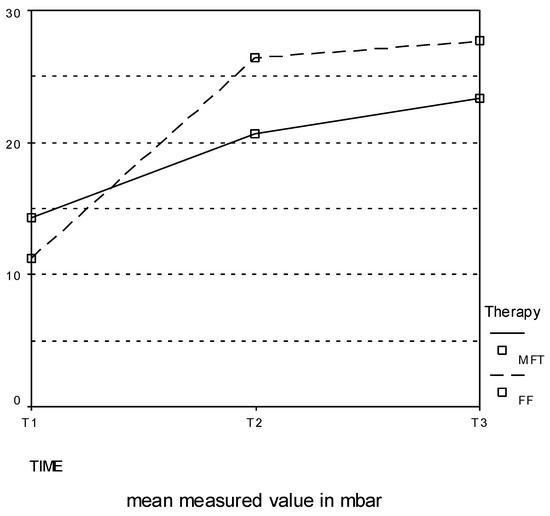
Figure 4.
Time-dependent increase in lip strength. Despite the initially low mean lip strengthwithin the study group, a marked increase in mean lip strength was recorded at T2 in comparison with the control group.

Table 5.
Percentage of patients with a pathologic swallowing pattern at all three measuring time points in each group and in the total collective, plus statistically determined significances.
Table 5.
Percentage of patients with a pathologic swallowing pattern at all three measuring time points in each group and in the total collective, plus statistically determined significances.
| Control group | Study group | Total | ||
|---|---|---|---|---|
| T0 | 100% | 100% | 100% | |
| T1 | 92.9% | 73.7% | 0.171 | 81.8% |
| T2 | 76.9% | 35.3% | 0.028* | 53.3% |
| 0.097 | 0.000** | 0.000** |

Table 6.
Percentage distribution of diagnosed cases of sigmatism. No statistically significant intragroup changes from T0 to T2 and no significant intergroup differences were registered with respect to the diagnosis of sigmatism.
Table 6.
Percentage distribution of diagnosed cases of sigmatism. No statistically significant intragroup changes from T0 to T2 and no significant intergroup differences were registered with respect to the diagnosis of sigmatism.
| Control group | Study group | Total | ||
|---|---|---|---|---|
| T0 | 100% | 96.2% | 0.578 | 97.8% |
| T1 | 100% | 94.7% | 0.576 | 97% |
| T2 | 92.3% | 88.2% | 0.603 | 90% |
| 0.368 | 0.368 | 0.135 |
The pronounced success of FFT can be attributed to the application mode and the type of exercises. Although both approaches induced a statistically highly significant increase in lip strength and thus an improvement in lip competence, competent mouth closure and nasal breathing could be achieved in the present study only by means of exercises with an appliance. Overnight insertion of the Face Former to encourage the patient to practice competent mouth closure and nasal breathing while sleeping is of special significance to long-term adaptation of the breathing mode and is thus superior in this respect to speech therapy exercises performed during the day only. As a positive secondary effect of the improvement in nasal breathing, Marchesan and Hubermann-Krakauer (1996) observed a normalization of the swallowing pattern without additional tongue training.
A physiological posture is moreover essential for stabilization of a nasal breathing pattern (Hubermann-Krakauer and Guilherme, 2000). The fact that an upright head-neck posture is practiced during FFT may be another factor contributing to the pronounced therapeutic success.
Lip strength can be improved by means of simple exercises that are essential to the stabilization of successful myofunctional therapy (Meyer, 2000; Satomi, 2001). Both FFT and MFT induced a statistically highly significant increase in lip strength, but this improvement was achieved within a shorter time, which was statistically significant in the FFT group. The time factor is not to be underestimated with respect to motivation and compliance. As many MFT failures are due to lack of motivation on the part of the patient, a therapy concept aimed at harmonizing orofacial dysfunctions should be effective in terms of time and execution simplicity.
It is controversially discussed in the literature whether a direct improvement in articulation is achieved through conventional MFT (Landis, 1994; Pierce and Taylor, 2001; Wadsworth, Maul and Stevens, 1998). Although some authors (Biegenzahn, Fischman and Mayrhofer-Krammel, 1992; Pierce and Taylor, 2001) have reported the correction of sigmatism during ongoing MFT, no statistically significant change in articulation was recorded in the present study within the six-month observation period. For this reason, an improvement in primary functions (breathing, swallowing pattern) should be followed by individualized articulation sequences aimed at correcting secondary functions (articulation), irrespective of the concept being applied. Our results are supported by the observation reported by Freiesleben and Hahn (1995) that secondary functions cannot be regulated until primary functions have been improved.
One point open to criticism in the methodology of the present study is the potentially wide range of conventional MFT concepts applied in the speech therapy practices concerned. However, the concept applied within the control group can be assumed to reflect routine therapeutic procedure at those practices.
The level of data loss within the two groups was comparable with that reported in clinical studies and displayed no intergroup differences. The probands in both groups can thus be assumed to have been comparably motivated.
The extent to which the attained improvements in the orofacial region can be sustained in the long term needs to be investigated in further studies with a longer follow-up period.
Within the six-month observation period, Face Former Therapy appears to have been more successful than conventional MFT. Especially from the aspect of economic efficiency, one factor not to be overlooked is that the improved treatment outcome is achieved with reduced personnel costs on account of the fewer therapeutic units required.
In view of the waiting times that are currently routine for patients wishing to start conventional MFT, FFT offers a good alternative for patients in urgent need of therapy. In view of its efficiency in establishing nasal breathing, Face Former therapy might furthermore be used as adjunctive treatment aimed at optimizing conventional MFT for relapse prevention.
CONCLUSIONS AND RECOMMENDATIONS
Myofunctional therapy concepts enable orofacial dysfunctions to be successfully harmonized within six months.
FFT proved to be more efficient than MFT in speech therapy practices within the six-month observation period. However, further studies are needed to determine the extent to which the newly established orofacial balance is stabilized. In addition, future research should be conducted to determine if similar results may be obtained on a larger population.
A long term follow up will be carried out in order to see if the achieved results can be stabilized or if any spontaneous improvement in articulation occurs. Unfortunately, the authors are unable to give any information regarding articulation therapy, which was provided after the completion of this study, because therapy approaches of the speech/language pathologists were too heterogeneous to be compared with on scientific basis. Therefore, future studies should be conducted in order to determine if, and in what ways an improvement in articulation can be affected by a successfully completed MFT/ FFT treatment.
References
- Bacha, S. M., and C. F. Rispoli. 1999. Myofunctional therapy: brief intervention. International Journal of Orofacial Myology 25: 37–47. [Google Scholar] [CrossRef]
- Benkert, K. K. 1997. The effectiveness of orofacial myofunctional therapy in improving dental occlusion. International Journal of Orofacial Myology 23: 35–46. [Google Scholar] [CrossRef]
- Bertolini, M. M., and J. Z. Paschoal. 2001. Prevalence of adapted swallowing in a population of school children. International Journal of Orofacial Myology 27: 33–43. [Google Scholar] [CrossRef]
- Biegenzahn, W., L. Fischman, and U. Mayrhofer-Krammel. 1992. Myofunctional therapy in patients with orofacial dysfunctions affecting speech. Folia Phoniatrica et Logopaedica 44, 5: 238–44. [Google Scholar] [CrossRef]
- Engelke, W., D. Engelke, and R. Schwestka. 1990. Zur klinischen und instrumentellen Untersuchung motorischer Zungenfunktionen. Deutsche Zahnärztliche Zeitschrift 45, 7: 11–6. [Google Scholar]
- Freiesleben, D., and V. Hahn. 1995. Grundlagen und Praxis der myofunktionellen Therapie unter besonderer Berücksichtigung des Einsatzes in der pädagogischen Sprachtherapie. Sprache Stimme Gehör 19: 118–25. [Google Scholar]
- Garretto, L. 2001. Orofacial myofunctional disorders related to malocclusion. International Journal of Orofacial Myology 27: 44–54. [Google Scholar] [CrossRef]
- Hubermann-Krakauer, L., and A. Guilherme. 2000. Relationship between mouth breathing and postural alterations of children: a descriptive analysis. International Journal of Orofacial Myology 26: 13–23. [Google Scholar] [CrossRef]
- Josell, S. D. 1995. Habits affecting dental and maxillofacial growth and development. Dental Clinics of North America 39, 4: 851–60. [Google Scholar] [CrossRef]
- Khinda, V., and N. Grewal. 1999. Relationship of tongue-thrust swallowing and anterior open bite with articulation disorders: a clinical study. Journal of the Indian Society of Pedodontics and Preventive Dentistry 17, 2: 33–9. [Google Scholar]
- Klocke, A., H. Korbmacher, and B. Kahl-Nieke. 2000. Der Status der myofunktionellen Therapie im Rahmen der interdisziplinären Zusammenarbeit aus der Sicht des Muskelfunktionstherapeuten. Sprache Stimme Gehör 24, 1: 38–43. [Google Scholar] [CrossRef]
- Korbmacher, H., and B. Kahl-Nieke. 2001. Optimizing interdisciplinary cooperation for patients with orofacial dysfunctions. Journal of Orofacial Orthopedics 62, 3: 246–50. [Google Scholar] [CrossRef]
- Krüger, M., and J. Tränkmann. 1997. Myofunktionelle Therapie. Sprache Stimme Gehör, 173–84. [Google Scholar]
- Landis, C. F. 1994. Applications of orofacial myofunctional techniques to speech therapy. International Journal of Orofacial Myology, 40–51. [Google Scholar] [CrossRef]
- Marchesan, I. Q., and L. R. Hubermann-Krakauer. 1996. The importance of respiratory activity in myofunctional therapy. International Journal of Orofacial Myology, 23–7. [Google Scholar] [CrossRef]
- Marchesan, I. Q. 2000. The speech pathology treatment with alterations of the stomatognathic system. International Journal of Orofacial Myology, 5–12. [Google Scholar] [CrossRef]
- Meyer, P. G. 2000. Tongue, lip and jaw differentiation and its relationship to orofacial myofunctional treatment. International Journal of Orofacial Myology, 44–52. [Google Scholar] [CrossRef]
- Pierce, R. B. 1983. The relationship between mouth breathing and tongue thrusting. International Journal of Orofacial Myology 9, 2: 4–5. [Google Scholar] [CrossRef]
- Pierce, R. B., and P Taylor. 2001. Rationale for including orofacial myofunctional therapy in university training programs. International Journal of Orofacial Myology, 24–32. [Google Scholar] [CrossRef]
- Satomi, M. 2001. The relationship of lip strength and lip sealing in MFT. International Journal of Orofacial Myology, 18–23. [Google Scholar] [CrossRef]
- Schopf, P. 1988. Myofunktionelle Übungen/ Myofunktionelle Therapie Wissenschaftliche Stellungnahme der Deutschen Gesellschaft für Zahn-, Mund-und Kieferheilkunde. Deutsche Zahnärztliche Zeitschrift. [Google Scholar]
- Sergl, H. G. 1988. 15 Thesen zur aktuellen Situation der myofunktionellen Therapie. Fortschritte der Kieferorthopädie 49: 312–314. [Google Scholar] [CrossRef] [PubMed]
- Umberger, F. G., and R. G. Johnston. 1997. The efficacy of oral myofunctional and coarticulation therapy. International Journal of Orofacial Myology, 3–9. [Google Scholar] [CrossRef]
- Wadsworth, S. D., C. A. Maul, and E. J. Stevens. 1998. The prevalence of orofacial myofunctional disorders among children identified with speech and language disorders in grades kindergarten through six. International Journal of Orofacial Myology 24: 1–19. [Google Scholar] [CrossRef]
© 2004 by the author. 2004 Korbmacher, H.M., Schwan, M., Berndsen, S., Bull, J., Kahl-Nieke, B.