INTRODUCTION
Individuals with adapted and maxilla functional orthopedics swallowing (AS) are frequently seen in speech therapy, otorhino- laryngology, and orthodontic offices.
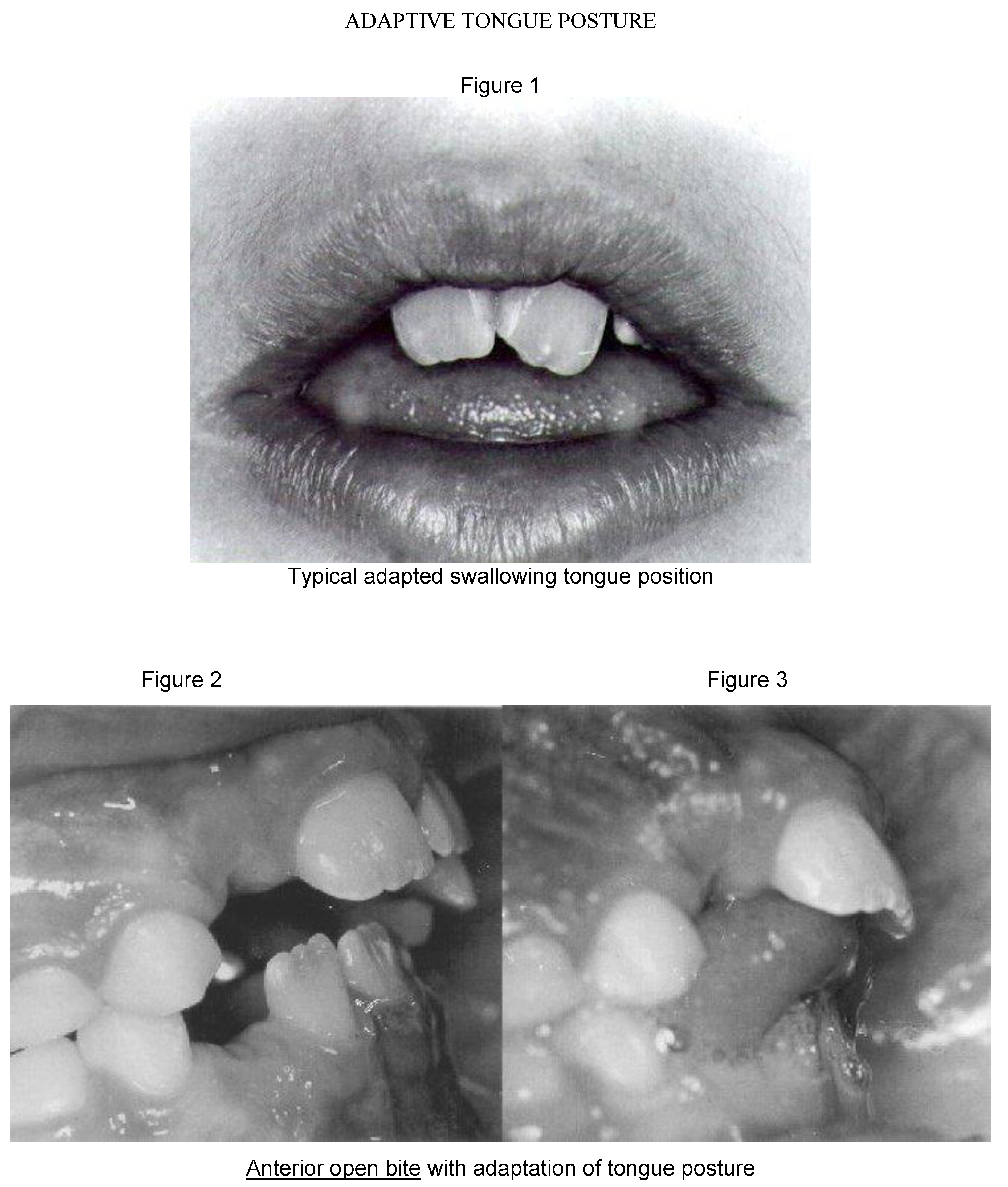
However, the diagnosis is underestimated in most cases. Changes in swallowing pattern in its oral phase are the result of primarily anatomic alterations of the oral cavity. The effects of these alterations on the dentofacial balance are often observed along with orofacial myofunctional changes in areas such as breathing, chewing and speech articulation. Adaptations of tongue and lips rest postures, and the cephalic- physical posture with orofacial muscular hypotonicity result in a major clinical picture: orofacial myofunctional disturbances. AS is merely a clinical sign. Figures 1, 2, 3, 4, 5, and 6 depict relevant clinical aspects of typical cases of AS with dentofacial impairment.
Structural changes, such as dental malocclusions, impair orofacial functions (breathing, swallowing, chewing, and speech articulation) which result in functional adaptations. Adapted functions, in turn, impair originally normal structures. A vicious circle is created resulting in an “unattractive physical appearance which evokes an unfavorable social answer and negative stereotypes” (Kenealy, 1989).
Re-establishing balance requires a multidisciplinary approach and represents a therapeutic challenge due to aetiopathogenic complexity. Several factors (age, oral habits, orofacial anatomic characteristics, genetic, and environmental factors) have to be considered during facial esthetic-functional rehabilitation. During orofacial myofunctional assessment, all morphofunctional aspects of the face must be observed.
![Ijom 27 00004 g001]()
![Ijom 27 00004 g002]()
OBJECTIVES
The purpose of this research is to identify the frequency of adaptive swallowing in its oral phase, aiming at the different clinical categories diagnosis among a population of school children.
METHODOLOGY
One hundred school children attending the Children and Adolescents’ Supporting Program (PRODECAD) of the State University of Campinas (UNICAMP) Brazil who were between seven and nine years of age were selected at random. Selected children received an orofacial myofunctional evaluation. Standard protocol was used to assess dentofacial structures and related aspects such as tonus, mobility, and rest posture (physical, cephalic, tongue, lips, and mandibular). Further, orofacial functions were assessed (breathing, chewing, and swallowing). Parents were asked to complete a questionnaire on nutrition, oral habits, mouth breathing and/or its originating signs.
A speech therapy assessment was carried out at school. The child was seated face-to- face to the test person, who observed head and neck posture, facial typology, hard and soft palates, teeth, and dental occlusion.
During dental examination, the general state of the teeth was observed regarding preservation (early tooth loss, cavities) and positioning (crossed teeth, superior incisor inclination, shrouding, diastema). The presence of periodental changes was also observed.
The aspect, tonicity, mobility and resting posture of lips, tongue, and mandibles regarding anatomic-functional assessment of dentofacial structures was also noted.
Further observation was completed of alterations of facial symmetry comparing the facial muscles and/or bones of both facial sides regarding tonicity of buccinatory muscles.
The tonicity of masseter and temporal muscles was examined by palpation at maximum occlusion of dental arcades. During palpation, we checked for a possible muscular contraction asynchronicity or impairment. The Temporomandibular Joint (T.M.J.) was assessed by palpation during quick opening and closing mouth to detect possible mandibular lateral deviation and its direction.
Occlusal alterations were classified according to ANGLE (
Angle, 1899) based on the “molar key”: the first superior molar encases its
mesiovestibular cusp into the sulcus of the first inferior molar. Alterations were studied on the vertical plane (open bite) as well as on the transversal plane (crossed bite, deviations of the mid-line).
Orofacial functions assessed included:
Breathing: expiratory nasal permeability, tested with Glatzel metal plate. Permeability was described as “on the right” and/or “on the left” and breathing as oral, nasal, or mixed.
Chewing: bite observation, more precisely triturating and chewing. Bite was classified as anterior or lateral, on the right, or on the left. During food trituration, mandibular movement types (vertical or rotating) were verified, as well as the presence/absence of lip sealing. Also examined were lateralization of alimentary bolus, its squashing, and possible breathing-chewing non- coordination. Chewing was classified as bi-lateral or predominantly unilateral through palpation of masseter, temporal, and buccinator muscles.
Oral phase of swallowing: swallowing of water and solid food was observed focusing on tongue protrusion or projection. Concomitant palpation was conducted of the of digastric anterior belly and of the hyoide bone. Swallowing pattern in this phase was identified as:
- a)
without protrusion and without tongue thrust;
- b)
with anterior tongue protrusion;
- c)
with tongue lateral and/or anterior thrust;
- d)
with lip and tongue thrust;
- e)
with inferior lip interposition.
Swallowing patterns were considered adapted to dentofacial form, except for the pattern without protrusion and without tongue thrust (item a). Also at this stage of the evaluation process, associated head movements were observed, as well as anterior mandibular gliding, perioral muscles contraction, and non-coordination of breathing-swallowing, or breathing-chewing- swallowing.
The following categories were considered, according to the results:
Normal swallowing pattern: rest posture and functional dynamics of dentofacial structures were adequate, harmonious, and featured nasal breathing.
Adapted swallowing associated to dentofacial disharmony: adaptation of resting postures of tongue, lips, and mandibula worsened by mouth breathing,
Adapted swallowing without compromised dentofacial morphology: postural and functional adaptations of dentofacial structures.
RESULTS
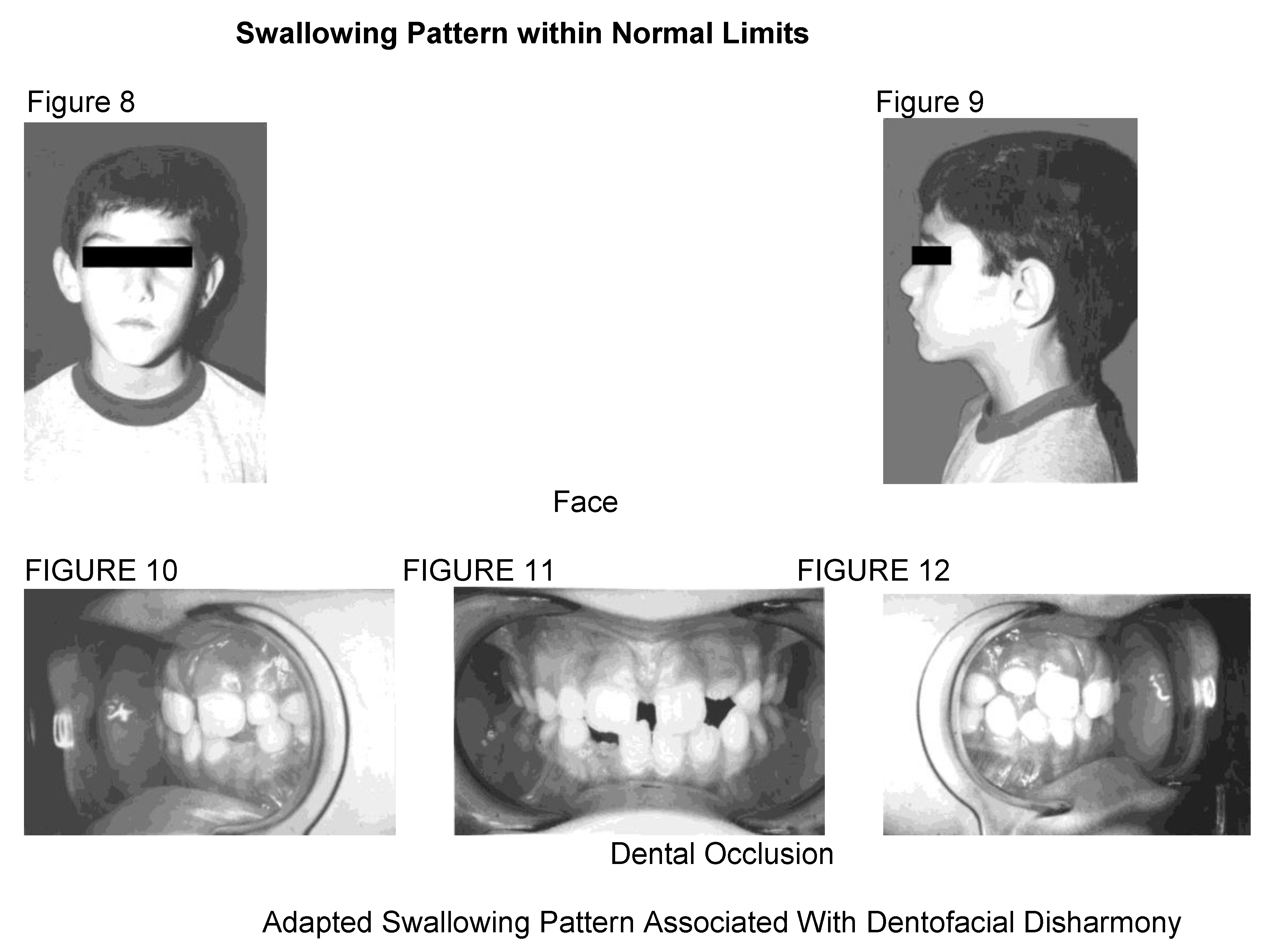
Distribution of studied population according to diagnosis is represented in Figure 7:
24% of the children had a swallowing pattern within normal limits;
57% had an adapted swallowing pattern associated with dentofacial disharmony;
19% had adapted swallowing without dentofacial disharmony.
![Ijom 27 00004 g003]()
Adapted swallowing associated with dentofacial disharmony group
In this study, adapted swallowing with or without dentofacial alterations was observed. In the group with adapted swallowing associated with dentofacial disharmony, it was noted that mouth breathing compromises orofacial muscular tonicity and the stomatognathic functions (swallowing and chewing). In the majority of the cases alterations of dental occlusion, maxilomandibular disproportions, and alterations in tooth positioning was observed.
Additional observations included:
Posterior crossed bite was present in 10% of cases and/or anterior open bite in 15% of cases.
Class II malocclusion according to Angle with or without associated crossed and/or open bite was found in 31% of cases.
An increase in vertical diameter of the inferior third of face and of palate depth was present with consequent postural and functional adaptations.
Predominantly unilateral chewing prevailed (39%).
Morphological alterations of major complexity featuring bone and/or muscular facial asymmetry was diagnosed in 14% of cases.
Changes in physical and cephalic posture were diagnosed in 43% of examined subjects. Postural deviations showed asymmetry in shoulder position, its anteriorization, spine curve with anteriorization or posteriorization of head and mandibular drop.
Deleterious oral habits (digit sucking, use of pacifier, use of nursing bottle) associated to mouth breathing was identified in 38% of the population.
Adapted swallowing without compromised dentofacial morphology group
In the group of adapted swallowing without dentofacial morphology impairment, it is felt that the observed occlusion was part of the initial phase of mixed dentition. Characteristics of this group may also be the result of hereditary characteristics (i.e. lack of space, detrimental positioning of the teeth).
Diagnostic categories
To clarify the subjectivity of assigning subjects to the three diagnostic categories used in this study a sample of the primary visual pattern representing each category is illustrated in the Figures 8 through 22.
![Ijom 27 00004 g004]()
![Ijom 27 00004 g005]()
DISCUSSION
The face represents a complex morphofunctional unit related to vital functions, to communication and consequently to socialization. It should be examined as a whole and treated in a way as to respect its structural and functional integrity (Endlow, 1993). Its study entails interdisciplinary observations that relate form-posture-function to craniofacial growth and development. Only interdisciplinary teamwork can result in a precise diagnosis, efficient treatment and intercepting measures when alterations are detected early.
Swallowing patterns in children between the ages of seven and nine years show characteristics of early mixed dentition, which were observed in the majority of subjects. This period, also called the “ugly duckling” phase (
Broadbent, 1975), is marked by a transitional swallowing process that differs from the normal adult pattern.
Maturation of swallowing pattern is not a simple phenomenon nor does it happen in a consistent way. A combination of childhood and maturational swallowing patterns is frequently observed during the deciduous phase. In some cases, this combination of swallowing patterns is observed at the outset of mixed dentition. Ongoing craniofacial growth and development associated to sensorial-motor-oral maturation and to involution of pharyngeal tonsils result in an increase of oral cavity space. This results in a greater space for the tongue to position itself and carry out its functions (Garattini, 1991; Proffit, 1975; Subtelny, 1973).
Swallowing pattern, rather than the entire facial complex, has more often been the focus of speech therapists, otorhinolaryngologists, and orthodontics or maxilla functional orthopedics. During the period of dentofacial growth and development, when a deviation is diagnosed, the goal should be to harmonize facial expression for all aspects. Preventive and rehabilitation measures are imperative to achieve the goal.
The face is an individual’s relationship portal to the outer world. It translates emotional and social responses and influences behavioral patterns or styles. In AS, the natural process of functional behavior is reversed, due primarily to anatomic local alterations of the oral cavity. Even small changes can trigger other morphofunctional facial alterations. Through functional adaptation phenomena, these alterations can develop into a wide range of clinical symptoms that impact on diagnosis and treatment of functional deviation cases.
Alterations range from minimal symptoms, such as in stigmatism, when only the lingual function during speech articulation reveals some alteration, to more global symptoms which may include the face, breathing, audition, language, speech, learning, and physical posture are highly altered. These characteristics may project a psychological pattern, which very often is inconsistent with the individual’s intellectual level. The way in which an individual relates to others socially may even be compromised.
The tongue adapts itself to the intra-oral space and to the dentofacial structures in its resting position and functional dynamics during the oral phase of swallowing. Tongue posture, in its resting and swallowing position, depends on the vertical diameter of the lower third of the face, on the width of dental arcs, on the palatine plane, on dental occlusion, and on breathing. Adaptation of lingual positioning may intensify dental and/or skeletal malocclusion and functional adaptations, or promote relapse of orthopedic-orthodontic treatment.
If the buccal phase of swallowing is not accompanied by thrust or protrusion of tongue in resting position it does not impact on dental malocclusion. Deleterious oral habits, especially digit sucking, force the tongue and its projection into an inferior position during swallowing. Hypertrophy of palatine tonsils, when severe enough to cause mouth breathing, leads to tongue lowering and anteriorization which triggers tongue thrust during swallowing. During the period of deciduous or mixed dentition these symptoms are considered physiological if they are not associated to dental malocclusion.
Structural alterations which occur during the period of craniofacial growth and development predisposethe individual to transitory functional adaptations not considered abnormal. Based on these concepts, this group was characterized as adapted swallowing without dentofacial impairment. On the other hand, it was verified that atypical structural alterations for the craniofacial growth and development period were inter-related to postural adaptations and muscular hypotonicity of dentofacial structures, to oral or mixed breathing, to adaptations of orofacial functions (oral phase of swallowing, chewing), and to deleterious environmental factors. These characteristics were considered predisposing factors for the category of adapted swallowing with dentofacial impairment. Results show that this group represents the most frequent swallowing pattern found in assessed children.
Swallowing patterns change naturally with aging, with intra-oral space available, mixed dentition, oral habits, obstructed breathing, type of dental occlusion, skeletal type, tonus of orofacial muscles, and proprioception.
Food consistency also modifies it, which is an adaptation phenomenon.
Orofacial myofunctional assessment, which is fundamental for the swallowing pattern diagnosis, should not be limited to simple observation of tongue protrusion or thrust in function. Tongue resting, lip and mandibular postures, breathing mode, facial configuration, dental occlusion, chewing, and lingual dynamics during swallowing should also be assessed. Besides, environmental interferences, especially digit sucking habits, must also to be considered.
Mouth breathing, which almost always had an impact on the children examined, was the suspected starting point for the anti- physiological adaptation of tongue posture and functionality, altering the normal course of physiological adaptation. Several authors point out that mouth breathing resulting from naso-respiratory obstruction is the main cause of alterations in dentofacial growth and development in childhood, and consequently in the age group similar to that of our study (Harvold, 1981; Linder-Anderson, 1979;
McNamara, 1981;
Todd, 1936).
In the group of children classified as adapted swallowing without dentofacial morphology disharmony, adaptations might be clinically less severe and part of the normal developmental process. They are therefore transitory. The potentiality to perpetuate themselves as dentofacial morphophysiological alteration in natural development depends on the associated environmental interferences.
Results reinforce the painstaking attention necessary for correctly interpreting morphofuncional alterations of the face in children during the transitional phase of dentition. Attention must be paid to the perspective of spontaneous correction of morphofunctional alterations if interferences are eliminated.
However, the need to correctly diagnose cases which have already been characterized as proper dentofacial morphofunctional alterations should not be underestimated, especially in the phase of transition. Both the situations require professional discernment, since the procedure obviously differs according to the case.
Furthermore, treatment success always implies interdisciplinarity involving otorhinolaryngology, speech therapy, and maxilla functional orthopedics/orthodontics. Isolated therapies will never be successful.
CONCLUSION
Adapted swallowing in studied population occurred in 76% of the population evaluated. The majority of cases, 57%, demonstrated an association with dentofacial deformations which needed immediate therapy. The remaining 19% of cases showed absolute need for orientation and prophylactic measures to interrupt a possible deviation from normal evolution