Rationale for Including Orofacial Myofunctional Therapy in University Training Programs
Abstract
:INTRODUCTION
- Oral-facial-pharyngeal structure, development and functions;
- Interrelationships among oral- vegetative functions and adaptations, speech, and dental occlusion, using interdisciplinary approaches;
- Nature of atypical oral-facial patterns and their relationship to speech dentition, airway competency, and facial appearance;
- Relevant theories such as those involving oral-motor control and dental malocclusion;
- Rationale and procedures for assessment of oral myofunctional patterns, and observation and participation in the evaluation and treatment of patients with oral myofunctional disorders;
- Application of current instrumental technologies to document clinical processes and phenomena associated with oral myofunctions and disorders; and
- Treatment options.
- Abnormal non-nutritive sucking habits (thumb, finger, pacifier, etc. sucking habits)
- Other detrimental orofacial habits
- Abnormal orofacial rest posture problems
- Abnormal neuromuscular muscle patterns associated with inappropriate mastication, bolus formation and deglutition
- Abnormal functional breathing patterns
- Abnormal swallowing patterns
- Abnormal speech problems (only if the COM has the speech-language pathology credential required by his/her State, Province or Country)
METHODS
| San Francisco 1999 | 55 |
| South Carolina 2000 | 50 |
| Las Vegas 2000 | 20 |
| April 2000 | 3 |
| Total | 128 |
RESULTS
Speech-Language Pathologists
| WORK SETTING | # REC’D | % RESPONSE |
|---|---|---|
| Public School | 67 | 52.3 |
| Rehab. Center | 20 | 15.6 |
| Hospital | 8 | 6.3 |
| University | 5 | 3.9 |
| Private Practice | 34 | 26.6 |
| Student | 10 | 7.8 |
| Other | 15 | 11.7 |
| (Several reported dual work settings.) | ||
| SLP EXPERIENCE | # REC’D | % RESPONSE |
|---|---|---|
| None | 12 | 9.3 |
| 1 - 5 yrs | 39 | 30.2 |
| 6 - 10 yrs | 13 | 10.1 |
| 11 - 15 yrs | 14 | 10.9 |
| 16 - 20 yrs | 21 | 16.3 |
| 21 - 25 yrs | 13 | 10.1 |
| Greater than 25 yrs | 14 | 10.9 |
| Unknown | 2 | 1.6 |
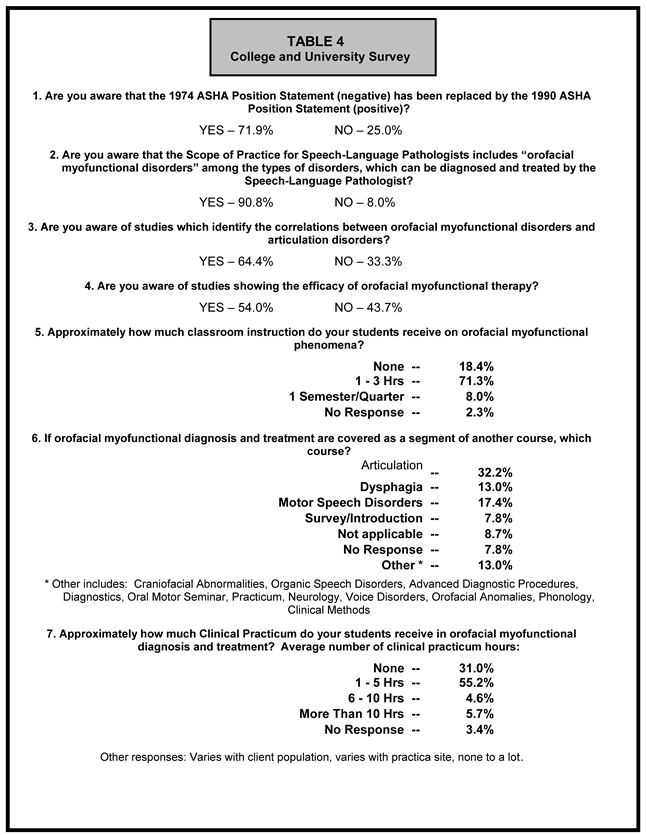
Colleges and Universities
DISCUSSION AND RECOMMENDATIONS
- 34% reported having no classroom instruction.
- 63% reported having no practicum experience.
- Of the 65 who had received some classroom instruction, 57 (87%) rated it as inadequate.
- Of the 35 who had received some practicum experience, 29 (87%) rated it as inadequate.
- 92% of the total sample believed that academic and clinical training in oral myofunctional phenomena is necessary.
- 15% - 18% of the participants felt they had received adequate training to evaluate and treat students with myofacial disorders. However, approximately 88% reported treating students with articulation impairments that appeared to be directly related to an oral myofunctional disorder. 85% reported serving students with apparent oral myofunctional disorders.
- 59% said their coursework did not adequately prepare them to evaluate and 63% did not feel adequately prepared to treat students with oral myofacial disorders.
- 97% believed that more coursework on oral myofunctional disorders is needed in training programs.

SUMMARY
References
- Advance for Speech-Language Pathologists, and Audiologists. 2001 October 1.
- Advance for Speech-Language Pathologists, and Audiologists. 2001 October 8.
- American Speech-Language-Hearing Association. 1975. Position statement on tongue thrust. ASHA 17: 331–337. [Google Scholar]
- American Speech-Language-Hearing Association. 1989. Report: Ad Hoc Committee on Labial-Lingual Posturing Function. ASHA 31, 11: 92–94. [Google Scholar]
- American Speech-Language-Hearing Association. 1991. The role of the speech-language pathologist in assessment and management of oral Myofunctional disorders. ASHA 33, Supplement 5, 73. [Google Scholar]
- American Speech-Language-Hearing Association. 1997. Preferred practice patterns for the profession of speech-language pathology. ASHA pp 54-55 92: 69–70. [Google Scholar]
- Bell, D., and A. Hale. 1963. Observations of tongue thrust swallow in preschool children. Journal of Speech and Hearing Disorders 28: 195–197. [Google Scholar]
- Blyth, P. 1959. The relationship between speech, tongue behavior, and occlusal abnormalities. The Dental Practitioner 10, 1: 11–22. [Google Scholar]
- Christensen, M., and M. Hanson. 1981. An investigation of the efficacy of oral myofunctional therapy as a precursor to articulation therapy for pre-first grade children. Journal of Speech and Hearing Disorders 46: 160–167. [Google Scholar] [PubMed]
- D’Asaro, M., S. Shapiro, A. Baum, and M. Jacoby. 1961. Incidence and relationship of abnormal swallow, open bite, absence of gag reflex, lisping and lip posture in children from 8 to 10 years. Asha 3: 369. [Google Scholar]
- Fletcher, S., R. Casteel, and D. Bradley. 1961. Tongue thrust swallow, speech articulation, and age. Journal of Speech and Hearing Disorders 26, 3: 201–208. [Google Scholar]
- Gommerman, S., and M. Hodge. 1995. Effects of oral myofunctional therapy on swallowing and sibilant production. International Journal of Orofacial Myology 21: 9–22. [Google Scholar]
- Goda, S. 1968. The role of the speech pathologist in the correction of tongue thrust. American Journal of Orthodontics 54, 11: 852–859. [Google Scholar] [PubMed]
- Hahn, V., and H. Hahn. 1992. Efficacy of oral myofunctional therapy. International Journal of Orofacial Myology, 18. 18–23. [Google Scholar] [CrossRef]
- International Association of Orofacial Myology. 2000. Business Handbook. IAOM p 2. [Google Scholar]
- Jann, G., M. Ward, and H. Jann. 1964. A longitudinal study of articulation, deglutition, and malocclusion. Journal of Speech and Hearing Disorders 29: 424–435. [Google Scholar] [PubMed]
- Landis, C. 1994. Application of orofacial myofunctional techniques to speech therapy (Clinical Exchange). International Journal of Orofacial Myology 20: 40–51. [Google Scholar]
- Moran, E., M. Harmon, L. Montgomery, and D. Morse. 1999. Training and competence in oral myofacial disorders. In Poster Session at the ASHA Convention. San Francisco, CA. [Google Scholar]
- Overstake, C. 1975. Investigation of the efficacy of a treatment program for deviant swallowing and allied problems. International Journal of Oral Myology 1, 3: 29–60. [Google Scholar]
- Pierce, R. 1980. The role of myofunctional therapy in speech pathology. International Journal of Orofacial Myology 6, 4: 11–12. [Google Scholar] [CrossRef]
- Pierce, R. 1996. Age and articulation characteristics: A survey of patient records on 100 patients referred for tongue thrust therapy. International Journal of Orofacial Myology, 32–33. [Google Scholar] [CrossRef]
- Ronson, I. 1965. Incidence of visceral swallowing among lispers. Journal of Speech and Hearing Disorders 30: 318–324. [Google Scholar] [PubMed]
- Straub, W. 1960. Malfunction of the tongue. Part I. The abnormal swallowing habit: Its cause, effects, and results in relation to orthodontic treatment and speech therapy. American Journal of Orthodontics 46, 6: 404–424. [Google Scholar]
- Subtelney, J., and Joanne Subtelney. 1962. Malocclusion, speech, and deglutition. American Journal of Orthodontics 48: 685–697. [Google Scholar]
- Toronto, A. 1975. Long-term effectiveness of oral myology. International Journal of Orofacial Myology 1, 4: 132–136. [Google Scholar] [CrossRef]
- Umberger, F., and R. Johnston. 1997. The efficacy of oral myofunctional and coarticulation therapy. International Journal of Orofacial Myology 23: 3–9. [Google Scholar] [CrossRef]
- Umberger, F., and J. Van Reenen. 1993. Speech-language pathologist’s knowledge of, exposure to, and attitudes toward oral myofunctional phenomena. International Journal of Orofacial Myology 19: 4–10. [Google Scholar] [CrossRef]
- Wadsworth, S., C. Maul, and E. Stevens. 1998. The prevalence of Orofacial myofunctional disorders among children identified with speech and language disorders in grades kindergarten through six. International Journal of Orofacial Myology 24: 1–19. [Google Scholar] [CrossRef]
- Ward, M., H. Malone, G. Jann, and H. Jann. 1961. Articulation variations associated with visceral swallowing and malocclusion. Journal of Speech and Hearing Disorders 26: 334–341. [Google Scholar] [CrossRef]
© 2001 by the author. 2001 Roberta Pierce, Patricia Taylor.
Share and Cite
Pierce, R.; Taylor, P. Rationale for Including Orofacial Myofunctional Therapy in University Training Programs. Int. J. Orofac. Myol. Myofunct. Ther. 2001, 27, 24-32. https://doi.org/10.52010/ijom.2001.27.1.3
Pierce R, Taylor P. Rationale for Including Orofacial Myofunctional Therapy in University Training Programs. International Journal of Orofacial Myology and Myofunctional Therapy. 2001; 27(1):24-32. https://doi.org/10.52010/ijom.2001.27.1.3
Chicago/Turabian StylePierce, Roberta, and Patricia Taylor. 2001. "Rationale for Including Orofacial Myofunctional Therapy in University Training Programs" International Journal of Orofacial Myology and Myofunctional Therapy 27, no. 1: 24-32. https://doi.org/10.52010/ijom.2001.27.1.3
APA StylePierce, R., & Taylor, P. (2001). Rationale for Including Orofacial Myofunctional Therapy in University Training Programs. International Journal of Orofacial Myology and Myofunctional Therapy, 27(1), 24-32. https://doi.org/10.52010/ijom.2001.27.1.3




