Mastication in the Oral Myofunctional Disorders
Abstract
INTRODUCTION
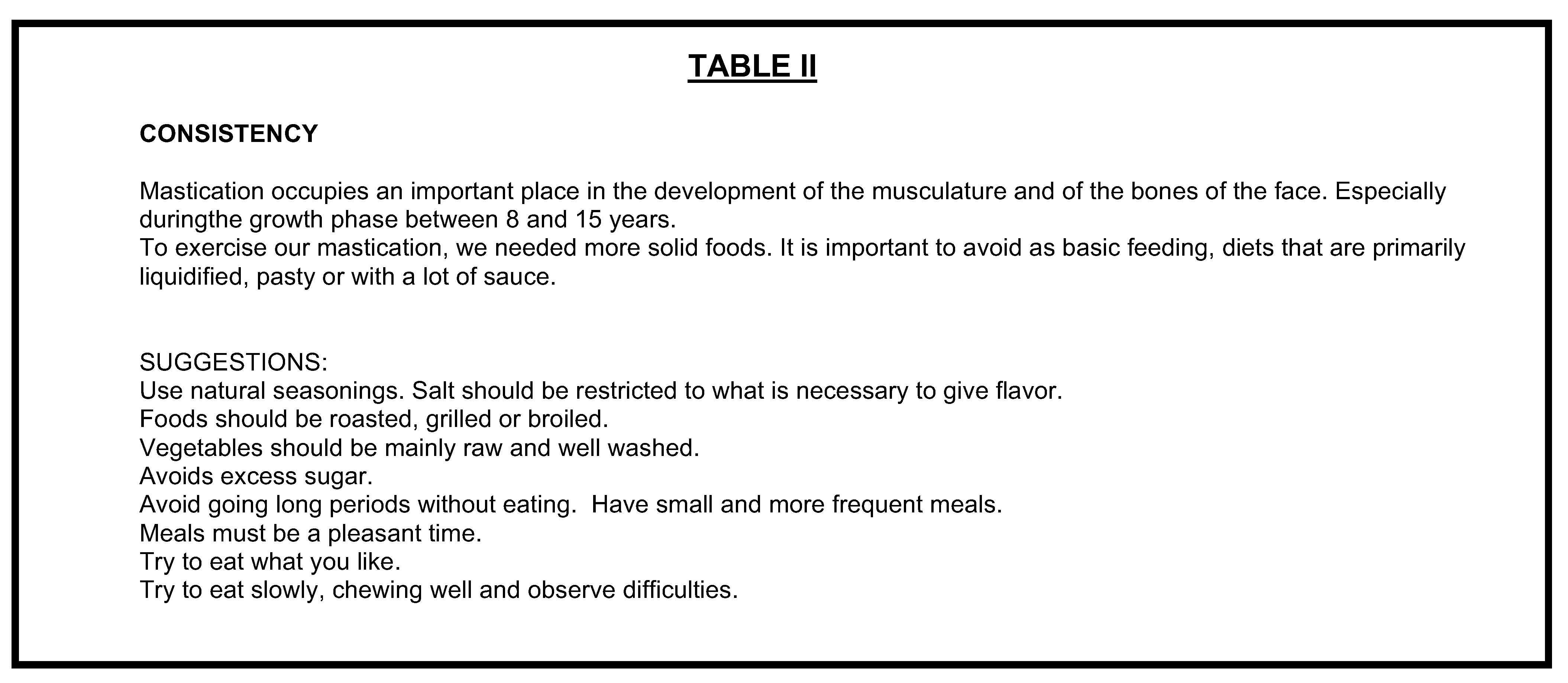
PROPOSALS OF WORK WITH THE MASTICATION
- ▪
- signs and/or symptoms of alterations in the temporo-mandibular joint - improper postural positions in the rest; deviations or cracks when opening the mouth; atypical movements of the jaw in the functions; pain when speaking, when chewing or during palpation;
- ▪
- occlusion conditions that limited mastication movements - class I with agglomeration and/or accentuated overjet, deep overbite, cross bite, open bite; class II and class III;
- ▪
- type of orthodontic appliance
- ▪
- loosing teeth.
I) Procedures for cases Without Limitations
II) Procedures for the cases With Limitations (TMJ, occlusion, appliance, loosing teeth)


CONCLUSION
References
- Altmann, E. (1990). Deglutio At’pica. In Kudo, A. M. Et Al, Coords. - Physiotherapies, Fonoaudiologia e Terapia Occupational em Pediatric. São Paulo: Sarvier. P.116-131.
- Altmann, E., & Vaz, A C. (1992). Avaliação e treatment fonoaudiológico nas cirurgias ortognáticas. In Altmann, E. B. Fissuras Labiopalatinas. Carapicuíba/SP: Pró-Fono, p. 410-417.
- Altmann, E. (1997). Avaliação myofunctional nas deformidades maxilomandibulares. In Psillakis, J. Cirurgia craniomaxilofacial - osteotomias estéticas da face. São Paulo: Medsi, p. 325-331.
- Altmann, E. (1996). Fazendo exercícios miofuncionais com Elisa B.C. Altmann. VT. Carapicuíba/SP: PróFono.
- Bacha, S, R’ispoli, C. (1999). Myofunctional therapy: Brief Intervention. The International Journal of Orofacial Myology. USA: International Association of Orofacial Myology, vol. XXV p. 37-47.
- Bacha, S., Camargo, A F., Ennes, J., Ribeiro, J., & Volpe, M.R. (1998). ExercÌcios de motricidade orofacial. Fita de vÌdeo e guia. CarapicuÌba/SP: Pró-Fono.
- Baptista, J.M. (1996). Ortodontia - fundamentos da colusão e da ATM. Curitiba: Editek, p. 12-118.
- Bianchini, E. (1993). Cefalometria nas alterações miofuncionais orais – diagnóstico e tratamento fonoaudiológico. Carapicuíba/SP, Pró-Fono. P.05-28.
- Bianchini, E. (1998a). Mastigação e ATM Avaliação e terapia. In Fundamentos em fonoaudiologia. Marchesan, I. Rio de Janeiro: Guanabara Koogan. P.37-49.
- Bianchini, E.M.G. (1998). Disfunções da Articulação Temporomandibular: Relações com a articulação da Fala. Tese de mestrado em Fonoaudiologia. PUC-SP.
- Bradley, R. (1981). Fisiologia oral básica. São Paulo: Panamericana. p. 13-46, 70-84, 114-122, 151-163.
- Camargo, M.A., & Hernandes, M.H. (1987). Enfoque tátil proprioceptivo em relação à aquisição do sistema fonêmico. In Lacerda, E., Cunha, M. Sistema Sensório Motor Oral. Série Distúrbios da comunicação. São Paulo: EDUC. p.76-85.
- Cravioto, J., & Milan, R. (1989). Má nutrição e sistema nervoso central. In: Diament.A, Cypel, S. Neurologia Infantil – Lefèvre. 2 ed. Rio de Janeiro: Atheneu. p. 1207-1231p. 1207-1231.
- Douglas, C.R. (1994). Tratado de Fisiologia. 1a ed. São Paulo: Robe, p. 163-167, 763-774, 827-844, and 857-885.
- Felõcio, C. M. (1999). Sistema Estomatognático e Funções – Mastigação. In Fonoaudiologia Aplicada a casos odontológicos – Motricidade oral e audiologia. São Paulo: Pancast, 1999, p. 23-35.
- Franco, M.L.Z. (1998). Mastigação bilateral: mito ou realidade? In, Revista da Sociedade Brasileira de Fonoaudiologia, ano 2 No.3 junho. p. 35-42.
- Gomes, R.C. (1999). Relações entre postura corporal e sistema estomatognático. In Jornal Brasileiro de Fonoaudiologia. Curitiba: Maio ano 1 No 1 p. 36-43.
- Gomes, I.C., Proen a, M.G., & Limongi, S.C. (1984). Avaliação e terapia da motricidade oral. In Ferreira, L.P. et al.l. Temas de Fonoaudiologia. São Paulo: Loyola, 1984, p. 59-119.
- Jabur, L. (1994). Inter-relação entre forma e função na cavidade oral. In Marchesan, I., Bolaffi, C., Gomes, I., Zorzi, J. (orgs). Tópicos em Fonoaudiologia, 1994. São Paulo: Lovise. p. 223-225.
- Junqueira, P. (1994). A atuação fonoaudiológica nos casos de mordida aberta anterior na dentição decídua. In Marchesan, I., Bolaffi, C., Gomes, I., Zorzi, J. (orgs). Tópicos em Fonoaudiologia, 1994. São Paulo: Lovise, 1994, p. 227-230.
- Krakauer, L. (1995). Alterações de funções orais nos diversos tipos faciais. In Marchesan, I., Bolaffi, C., Gomes, I., Zorzi, J. (orgs). Tópicos em Fonoaudiologia, V. II, 1995. São Paulo: Lovise, 1995, p. 147-154.
- Limongi, S. (1987). Considerações sobre a importância dos aspectos morfo-fisiológicos e emocionais no desenvolvimento e profilaxia dos órgãos fono-articulatórios. In LACERDA, E., CUNHA, M. Sistema Sensório Motor Oral. Série Distúrbios da comunicação. São Paulo: EDUC. p.58-75.
- Madeira, M. C. (1997). Anatomia da Face – bases anátomo-funcionais para a prática odontológica. 2 ed. São Paulo: Sarvier. p. 68-77.
- Marchesan, I.Q. (1989). Motricidade oral - visão clínica do trabalho fonoaudiológico integrado com outras especialidades. Dissertação de Mestrado em distúrbios da comunicação na Pontifícia Universidade Católica de São Paulo.
- Marchesan, I. (1993). Motricidade Oral. São Paulo: Pancast, p.19-40.
- Marchesan, I. Q. (1994). O Trabalho fonoaudiológico nas alterações do sistema estomatognático. In Marchesan, I., Bolaffi, C., Gomes, I., Zorzi, J. (orgs). Tópicos em Fonoaudiologia, 1994. São Paulo: Lovise. p. 83-96.
- Marchesan, I.Q. (1997). Avaliando e tratando o sistema estomatognático. In LOPES FILHO, O (editor) e cols. Tratado de Fonoaudiologia. São Paulo. p. 763-780.
- Marchesan, I. (1998). Uma visão compreensiva das práticas fonoaudiológicas. São Paulo: Pancast. p.221-230.
- Meurer,E., Veiga, L., & Capp, E. (1998). Hábitos mastigatórios e de deglutição em crianças de 3 a 5 anos. In Revista da Sociedade Brasileira de Fonoaudiologia, ano 2 – No.3 – junho p. 29-34.
- Morales, R. C. (1991). Terapia de Regulação Orofacial. São Paulo: Memnon. p.54- 56, 109-120.
- Moyers, R. (1988). Ortodontia. Rio de Janeiro: Guanabara Koogan. p107-116, 265-282.
- Padovan, B.A.E. (1976). Reeducação Mioterápica nas pressões Atípicas de Língua. In Revista Ortodontia, vol. 9, ns. 1 e 2, janeiro/abril e maio/agosto.
- Planas, P. (1988). Reabilitação Neuro-oclusal. Traduzido por Wilma Alexandre Simões. São Paulo: MEDSI. p. 17 – 44.
- Petrelli, E. (1992). Classificação da Má-oclusão. In, Petrelli, E. (coord). Ortodontia para fonoaudiólogos. Curitiba/PR: Lovise. p. 81 – 96.
- Rõspoli, C., & Bacha, S. (1998). Terapia miofuncional: Intervenção fonoaudiológica breve. In Marchesan, I., Zorzi, J., Gomes (orgs), I. Tópicos em Fonoaudiologia 1997/1998 vol IV. São Paulo: Lovise. p.545-585.
- Tanigute, C. (1998). Desenvolvimento das funções estomatognáticas. In Fundamentos em Fonoaudiologia. Marchesan, I. Rio de Janeiro: Guanabara Koogan. pp. 1-6.
© 2000 by the author. 2000 Stella M. Cortez Bacha, Cybele de F. Mandetta Ríspoli.
Share and Cite
Bacha, S.M.C.; Ríspoli, C.d.F.M. Mastication in the Oral Myofunctional Disorders. Int. J. Orofac. Myol. Myofunct. Ther. 2000, 26, 51-58. https://doi.org/10.52010/ijom.2000.26.1.7
Bacha SMC, Ríspoli CdFM. Mastication in the Oral Myofunctional Disorders. International Journal of Orofacial Myology and Myofunctional Therapy. 2000; 26(1):51-58. https://doi.org/10.52010/ijom.2000.26.1.7
Chicago/Turabian StyleBacha, Stella M. Cortez, and Cybele de F. Mandetta Ríspoli. 2000. "Mastication in the Oral Myofunctional Disorders" International Journal of Orofacial Myology and Myofunctional Therapy 26, no. 1: 51-58. https://doi.org/10.52010/ijom.2000.26.1.7
APA StyleBacha, S. M. C., & Ríspoli, C. d. F. M. (2000). Mastication in the Oral Myofunctional Disorders. International Journal of Orofacial Myology and Myofunctional Therapy, 26(1), 51-58. https://doi.org/10.52010/ijom.2000.26.1.7


