Abstract
Reducing the stigma and discrimination faced by men who have sex with men (MSM) and transgender women (TGW) in healthcare settings is key to improving health outcomes. Using a one-group pre- and post-test design, we tested the efficacy of a theory-informed, multi-level pilot intervention (“Harmony”) among 98 healthcare workers (HCWs) to reduce sexual orientation and gender identity (SOGI)-related stigma and discrimination faced by MSM and TGW in two public hospitals. The intervention contained group-level (a half-day workshop) and individual-level (four videos) components. Using multi-level modelling, we compared knowledge, attitudes, and comfort level among HCWs across three timepoints: pre-intervention, post-intervention, and follow-up (2 months after the intervention). Client surveys were conducted among 400 MSM/TGW (two independent samples of 200 MSM/TGW) attending the intervention hospitals, before the intervention among HCWs and three months after the intervention. Generalised estimating equations assessed service users’ satisfaction with hospital services, discrimination experiences, and positive interactions with HCWs. Significant changes were observed in primary outcomes: 30% increase in positive attitude scores (incidence rate ratio (IRR) = 1.30, 95% CI 1.13–1.49) and 23% increase in the proportion of HCWs reporting being comfortable in providing care to MSM/TGW (IRR = 1.23, 95% CI 0.03–1.68). Similarly, there was a significant improvement in secondary outcomes (scores): support for non-discriminatory hospital policies (IRR = 1.08, 95% CI 1.004–1.15), the importance of asking SOGI questions in clinical history (IRR = 1.17, 95% CI 1.06–1.29), and perceived self-efficacy in providing clinical care (IRR = 1.13, 95% CI 1.01–1.27). Service users’ data provided corroborative evidence for intervention efficacy: e.g., 14% increase in the proportion of MSM reporting overall satisfaction with hospital services and 6% and 15% increase in the scores of positive interactions with HCWs in the combined sample of MSM/TGW and TGW, respectively. The Harmony intervention showed preliminary evidence for improving positive attitudes, comfort level, and understanding of the healthcare issues of MSM/TGW among HCWs, warranting large-scale implementation research.
1. Introduction
Stigma denotes the social process of devaluing people or groups [1,2] based on real or perceived differences, such as age, sexual orientation, gender identity, behaviour, HIV status, or ethnicity. It results in the unfair and unjust treatment (discrimination) of an individual based on their socially identified status [3]. Men who have sex with men (MSM) and transgender women (TGW) are particularly stigmatised because of erroneous perceptions among the general public and healthcare workers (HCWs). Studies have shown that prejudice towards MSM and TGW among HCWs could be a result of inadequate or incorrect knowledge about MSM and TGW, moral values and religious notions related to sexuality, and lack of positive interactions with MSM and TGW [4]. Also, MSM and TGW themselves may be reluctant to access healthcare services due to fear of discrimination by HCWs, lack of trust, and previous bad experiences in healthcare settings, including sexual healthcare services [5,6]. Stigma and discrimination in health settings remains a neglected issue, and the lack of sensitive and trained HCWs can limit access to care, contributing to health inequalities. Insufficient training and lack of exposure to MSM and TGW impact the ability of HCWs to provide medically competent and sensitive care [7,8].
India’s National AIDS Control Organisation (NACO) is committed to achieving the international target of “zero stigma and discrimination” in healthcare settings [9,10]. Stigma reduction efforts have been part of NACO’s efforts to improve access to and use of HIV prevention, treatment, and care services for key populations [11]. The midterm evaluation report of the fourth National AIDS Control Programme (NACP-IV) specifically recommended the need to focus on reducing the stigma and discrimination faced by key populations in healthcare settings. NACO has released the guidelines for implementing the “HIV/AIDS (Prevention & Control) Act 2017” to reduce stigma and discrimination against people living with HIV and key populations. Stigma reduction efforts and community-led monitoring of stigma and discrimination are part of NACO’s vision to strengthen community systems and improve access to high-quality services for key populations. Considering that it is crucial to improve coverage and access to healthcare for key populations, including MSM and TGW, it becomes critical to develop and test the efficacy of theory-based interventions to reduce the stigma and discrimination faced by them in healthcare settings. The availability of such evidence-informed stigma reduction interventions will fill a long-term gap in the armoury of tools to eliminate the discrimination faced by MSM and TGW [12].
Several studies have been conducted in developed countries like the USA that assessed the effect of training HCWs or medical students on reductions in sexual and transgender prejudice and improvements in clinical and cultural competency in providing healthcare services to sexual and gender minorities (SGMs) [13,14,15,16,17]. One multi-country study conducted among 2825 participants (of which 32 participants were from India), who were mostly staff from the HIV-program-implementing agencies, reported sustainable decreases in negative attitudes toward SGMs [18]. From South Asia, a limited number of studies have focused on reducing stigma and discrimination faced by SGMs in healthcare settings; most studies focused on reducing HIV-related stigma [19]. While most training interventions in healthcare settings aimed to reduce discrimination faced by SGMs as a whole [15], some interventions have focused exclusively on reducing stigma faced by transgender people in healthcare settings [20,21]. From India, one pilot intervention among HCWs [22] focused on reducing HIV-/STI-related stigma faced by TGW through a one-day workshop and reported a significant improvement in positive attitudes among HCWs.
Given that discrimination occurs at interpersonal, institutional, and structural levels, interventions to reduce stigma and discrimination might work better if they address factors at multiple levels [23]. However, in India, there is a paucity of comprehensive interventions at multiple levels to reduce stigma and discrimination in healthcare settings towards key populations [12]. Accordingly, this study aimed to develop and evaluate a multi-level intervention for HCWs to reduce the sexual orientation and gender identity (SOGI)-related stigma and discrimination faced by MSM and TGW in public healthcare settings. This intervention aimed to improve HCWs’ positive attitudes and comfort level in providing care to MSM and TGW. The intervention was expected to ultimately improve the quality of care provided to MSM and TGW in public hospitals.
2. Materials and Methods
2.1. Study Setting and Design
Between September 2021 and June 2022, using a one-group pre- and post-test quasi-experimental design [24,25], we conducted a pilot intervention among HCWs in two public hospitals in two Indian cities (Chennai and Thane). These hospitals were selected based on the commitment of the hospital administrators, support from the local government and community stakeholders, and the feasibility of recruiting diverse MSM and TGW who use the services of these public hospitals, especially given the challenges during the COVID-19-related lockdown periods.
In parallel to assessments among HCWs, a repeated cross-sectional study, with pre- and post-intervention assessments among independent samples of MSM and TGW (who accessed healthcare services in the intervention hospitals), was conducted to assess changes in their stigma and discrimination experiences.
2.2. Intervention Development
Qualitative Formative Research
We conducted a qualitative formative research study by examining 12 focus groups with 37 MSM and 30 TGW, as well as 4 key informant interviews with community leaders [26]. The main objectives of this formative research were to confirm and expand on the conceptual framework by exploring: (1) barriers to and facilitators of the use of healthcare services by MSM and TGW; (2) experiences of stigma and discrimination; (3) perceived quality of services and interactions between HCWs and MSM/TGW; (4) presence of hospital policies that are supportive of or restrictive to the engagement of MSM and TGW (e.g., hospital’s policy on which ward trans women will be admitted to); and (5) recommendations and suggestions for reducing stigma and discrimination in healthcare settings. In addition, we also sought feedback from the focus group participants and key informants on the draft intervention content and delivery and their suggestions for potential popular opinion leaders among HCWs in the intervention hospitals to contribute as intervention champions. Inputs from the formative research helped in finalising the intervention components (workshop and videos) and their delivery mode (in-person workshop and videos through WhatsApp) and duration (half to one day for the workshop and 5 min for one video).
2.3. Conceptual Framework
We used the findings from the qualitative research as well as theory-informed logic model of change (Figure 1) to design a culturally tailored multi-level intervention (Harmony) for HCWs by including components to address sexual and trans prejudice—improving knowledge, changing negative attitudes, and enhancing understanding of healthcare challenges faced by sexual and gender minorities in healthcare settings.
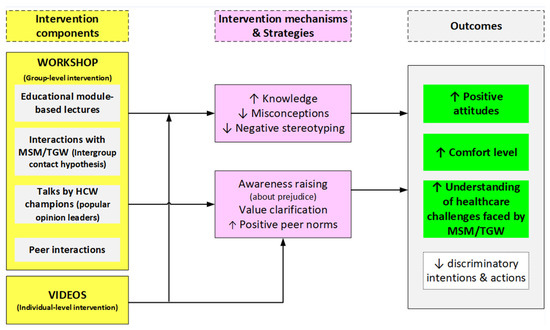
Figure 1.
Logic model of change for the Harmony intervention.
The Harmony intervention used two models of social change [27]: (1) stigma/prejudice reduction—how to reduce negative attitudes and bias among HCWs toward MSM/TGW; (2) collective action—involving MSM/TGW communities to actively participate in stigma reduction efforts. The intervention contained group-level (training workshop) and individual-level (sharing of videos) components. The content creation and delivery of the interventions used several theory-based approaches (Table 1). The Diffusion of Innovation theory states that new behavioural trends are likely to be adapted by the target populations when popular opinion leaders (e.g., senior doctors in healthcare settings as intervention champions) adopt and endorse the new trend [28]. As per the intergroup contact hypothesis, under appropriate conditions, interactions between a majority (or powerful) and a minority (oppressed or vulnerable) group can reduce prejudice [29]. Accordingly, in the group-level intervention (workshop), in addition to the educational lectures, HCW champions shared their perspectives (popular opinion leader approach) to promote positive peer norms [28,30,31], and a panel of MSM/TGW community champions interacted with HCWs (intergroup contact hypothesis) [29,32]. These interactive sessions focused on increasing the awareness of prejudice (awareness raising) [33], along with peer interactions in a non-judgemental setting [34]. In relation to the individual-level intervention, the contents in the videos (an infotainment-based e-intervention to promote understanding of MSM/TGW) were developed in collaboration with MSM/TGW community members, increasing their ownership of the intervention in line with the “collective action” model [27] and enhancing the legitimacy of the content in the videos.
2.4. Intervention Description
Group-level intervention—Workshop: A single half-day (3 h) workshop was conducted separately for the clinical (doctors/nurses) and non-clinical/paramedical staff (e.g., counsellors, lab technicians, and ward attendants) in each of the two public hospitals. The workshop aimed at enhancing the clinical care provided to SGM, especially transgender people and same-sex-attracted people. The main topics covered in these workshops were: the essentials of same-sex sexuality and gender identity, inclusive language, MSM/TGW-friendly practices, and legal aspects. The eight modules used in the workshop (Table 1) were adapted from the modules that were extensively used to train HCWs (doctors and counsellors) on the health issues of MSM and TGW in several parts of India [35] as well as from reputed international resources [36,37,38,39]. Experienced facilitators (doctors, researchers, and community experts) delivered the workshop sessions using various theory-based approaches (Table 1).


Table 1.
Description of “Harmony” multi-level intervention among HCWs to reduce stigma and discrimination faced by MSM and TGW in public health facilities.
Table 1.
Description of “Harmony” multi-level intervention among HCWs to reduce stigma and discrimination faced by MSM and TGW in public health facilities.
| Intervention Components | Evidence-Based Approaches | Activities |
|---|---|---|
| Workshop (Group-level intervention) | Provision of education through lectures and interactive sessions | Conducted half-day training for facility HCWs (8 modules): Information on same-sex and bisexuality and gender identity; Talks by MSM and TGW (telling their stories); stigma and discrimination in healthcare settings; healthcare needs (including mental health and gender transition care); relevance of sexual orientation and gender identity questions in clinical history taking; inclusive language, communication and practice; discussion on sexual/gender minority-friendly and non-discriminatory hospital policies; developing action steps to improve quality of services for MSM and TGW. |
| Involvement of popular opinion leaders (HCW Champions) [28,30] | Identified local hospital champions among HCWs (based on community agencies’ inputs) who shared their perspectives and experiences on how to provide non-discriminatory care to MSM and TGW. | |
| Involvement of MSM/TGW community champions—Intergroup contact (Contact hypothesis) [29,32] | Community champions as co-trainers. Interactions of the HCWs with MSM/TGW community leaders and representatives, and hearing their testimonials regarding the issues faced by them in healthcare settings. | |
| Awareness of prejudice (Consciousness raising) [40] | Participants were made self-aware of their prejudice by a description of scenarios during the lectures, good practices and the testimonials of MSM/TGW community representatives. | |
| Peer interactions | HCWs discussed their beliefs and feelings with peers in a safe, non-judgmental environment. | |
| Entertainment | A break in between the workshop sessions during which MSM/TGW community representatives provided a dance performance. This also showcased the artistic and creative talent among MSM/TGW communities. | |
| Short videos (Individual level intervention) | Collective action [27] (Creation of short videos) | Short videos were created based on the inputs from the MSM/TGW communities in the qualitative formative research. MSM/TGW community representatives acted in the short videos that highlighted the issues faced by MSM/TGW in healthcare settings. Inputs on the scripts of the videos were obtained from community and policy stakeholders. |
| Entertainment/Infotainment (Sharing of short videos) | Four short videos (in local languages) were shared with HCWs (one video per week for 4 weeks) over WhatsApp over a period of two months after the workshop. These videos were intended to raise awareness about the issues faced by MSM and TGW in healthcare settings. |
Individual level intervention—Videos: The half-day workshop was followed by an individual-level intervention, in which four short videos, each of about 5 min duration (two videos each on MSM and TGW) in local languages (Hindi and Tamil), were shared with HCWs individually over WhatsApp (Table 1). The direction of messages was one-way, i.e., from the research team to the participants. The storyline/scripts of the videos were prepared in consultation with MSM and TGW, who themselves were the lead actors in these videos. The videos focused on the challenges faced by MSM/TGW in healthcare settings and what can be undertaken by HCWs to provide optimal care.
Three assessments (using self-administered questionnaires) were conducted: one immediately prior to the workshop, one immediately after the workshop (a paper-and-pencil survey), and a follow-up assessment (an online survey with the link sent via WhatsApp) 2 months after the workshop (Figure 2).
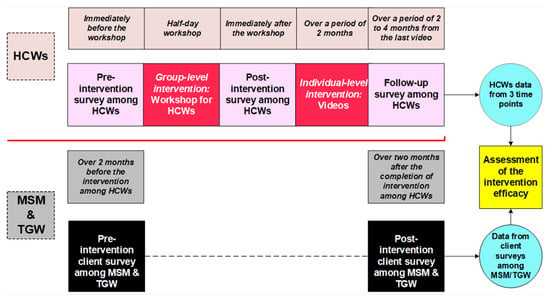
Figure 2.
The sequence of the intervention-related activities and data collection points among HCWs and hospital clients (MSM and transgender women).
2.5. Participants and Recruitment
Surveys among HCWs: For the intervention among HCWs in the two public hospitals, an average of two staff representatives from each department (e.g., medicine, surgery, skin and STD, gynaecology, and psychiatry) were invited. HCWs included clinicians, nurses, counsellors, and other staff (e.g., lab technicians and data entry operators). Thus, disproportionate stratified sampling, a non-probabilistic sampling technique, was used given the exploratory and pilot nature of the intervention as the primary goal was to assess the study’s feasibility and obtain preliminary evidence for efficacy. For pilot intervention projects, a sample size of 50 per subgroup and 100 each for pre- and post-intervention is considered sufficient [41]. Based on these guidelines, a total of 98 HCWs were recruited.
Client surveys among MSM and TGW: For the pre- and post-intervention surveys among MSM and TGW to cross-validate the outcomes of the intervention among HCWs, a total of 100 MSM (50 in each city) and 100 TGW (50 in each city) were recruited through convenience sampling with the help of partner community-based organisations (CBOs) that provide HIV prevention services to MSM and TGW through physical outreach and/or engaging in advocacy activities to promote acceptance of SGMs. The inclusion criteria were: at least 18 years of age, self-identification as MSM or TGW (using any equivalent indigenous terms that denote gay and bisexual men, transgender women, or non-binary identities), and use of hospital services in the past 3 months. Eligible participants were recruited consecutively until the required sample sizes of MSM and TGW were reached. The interviews were conducted by trained peer research interviewers in private rooms in CBOs or in a private place of the participant’s choosing. The post-intervention survey among service users was conducted three months after the intervention among HCWs.
3. Measures
Surveys among HCWs: In addition to sociodemographic data, the self-administered questionnaire measured three primary and three secondary outcomes (Table 2). The primary outcomes included: (1) positive attitudes toward MSM/TGW score (5-item scale); (2) comfort level in providing care to MSM/TGW (2 items); and (3) understanding the challenges faced by MSM/TGW in healthcare settings (2 items). Three secondary outcomes were: (1) support for non-discriminatory policies score (3-item scale); (2) perceived self-efficacy in providing clinical care score (3-item scale); and (3) understanding of the importance of sexual orientation and gender identity (SOGI) question score (3-item scale). Given the lack of standardised scales in the Indian context, the items of these scales were compiled from diverse sources [35,42,43,44,45,46] and in consultation with community members. All negatively worded items were reverse scored. The “Comfort level” and “Understanding the challenges faced by MSM/TGW” concepts were measured using two items each; hence, a total score was not used, and only individual items were used. For ease of interpretation, the Likert scale responses of each of these items were dichotomised. The scales with three or more items were subjected to Horn’s parallel analysis (PA), Velicer’s minimum average partial correlation analysis (MAP), and principal components analyses (PCAs) to determine the number of components to be extracted (Table 2), and a total score was used. The analyses were conducted on the baseline data after confirming that the correlation matrix was factorable (significant Bartlett’s test of sphericity with Kaiser–Meyer–Olkin measure of sampling adequacy > 0.50) using Stata-16. The findings of these three approaches were convergent. Hence, we report PCA findings.

Table 2.
Survey among HCWs: summary of the key outcome measures.
The intervention feasibility was assessed via the post-intervention survey completion rate: i.e., the percentage of enrolled HCWs who completed the post-intervention survey, which was administered just after the completion of the workshop. The intervention acceptability was assessed qualitatively immediately after the completion of the workshop (oral feedback) and after the follow-up assessment (WhatsApp messages from participants) by asking the participants to describe the usefulness of the intervention and suggest points for improving the intervention further.
MSM and TGW client surveys: Essential sociodemographic characteristics were collected. The main outcome measures included (Table 3): overall satisfaction with the hospital services (1 item: yes/no), discrimination experiences score (6-item scale) [47,48], and positive interactions with HCWs score (4-item scale) [49]. The scales were subjected to PA, MAP, and PCA to determine the number of components to be extracted.

Table 3.
Client surveys among MSM and TGW: summary of the key outcome measures.
3.1. Data Analysis
The longitudinal dataset consisted of outcome measurements of 98 HCWs at 3 time points. As the study aimed to test the efficacy of the intervention, we were interested in the between-HCW variability rather than within-HCW variability. Intervention efficacy among HCWs was, therefore, evaluated using multi-level modelling that takes into account the clustered nature of the observations (unlike linear regression, which assumes the observations to be independent). Further, multi-level modelling uses all the available data from incomplete observations in a longitudinal dataset, preserving the sample size in analysis. Based on the type of data distribution indicated by normality tests (all outcome scores were non-normal) and summary statistics (mean and variance), positive attitudes score, support for hospital non-discriminatory policies score, perceived self-efficacy in providing clinical care score, and importance of asking SOGI questions score were treated as count outcomes. Poisson or negative binomial mixed (multi-level) models are some of the options available to analyse and interpret count and binomial data from prospective cohort studies [50,51], especially by using robust error variance [52,53]. Multi-level Poisson regression models with robust standard errors were used for both count (e.g., positive attitudes score, support for non-discriminatory hospital policies score, perceived self-efficacy in providing clinical care score, and importance of asking SOGI questions score) and categorical (e.g., comfort level in providing care to MSM/TGW and understanding the healthcare challenges faced by MSM/TGW) outcomes. Incidence rate ratios (IRRs)—exponentiated Poisson regression coefficients—were reported to compare the change in the outcomes at different time points.
For evaluation of the intervention efficacy among the intervention hospital service users (MSM and TGW), pre-/post-intervention data from two independent samples of MSM and TGW clients were compared using generalised estimating equations (GEEs) with robust standard errors to estimate the post-intervention changes in the outcomes [54]. As stated above, based on the summary statistics, discrimination experiences score and positive interactions with HCWs score were treated as count outcomes. Therefore, different models were estimated based on the distribution of the outcome variables: Poisson model for a binary outcome (overall satisfaction with the hospital services), negative binomial model for an over-dispersed count outcome (discrimination experiences score), and zero-inflated Poisson model for an outcome with excess zeros (positive interactions with HCWs score) [53]. Given that this is a quasi-experimental trial and not a randomised controlled trial, and considering that certain factors might influence the effect of the intervention on the outcomes between HCWs, the models were adjusted for relevant covariates, such as age, gender, prior training on health issues of MSM and TGW, city (Chennai vs. Thane), number of years of practice, and number of SGM patients seen in the past 3 months (for the clinical staff). Similarly, we adjusted the models for service users with covariates, such as age, monthly income, engagement in sex work, health insurance, and antiretroviral treatment status (a proxy for HIV-positive status). All analyses were conducted using Stata/SE 16.1 (Stata Corporation, College Station, TX, USA). We used robust standard errors for all the models by including “vce(robust)” option in Stata commands.
3.2. Ethical Considerations
The institutional review boards of the Centre for Sexuality and Health Research and Policy (Ref. 221/2021), Tata Institute of Social Sciences (Ref. 2020-2021/31), and the Humsafar Trust (Ref. 52-06/2021 & 52/1-12/2021) approved this study. Written informed consent was obtained from all participants. No identifying information was collected. HCWs were not paid. For the surveys among MSM and TGW, participants received INR 300 (~USD 5) each in pre- and post-intervention assessment surveys.
4. Results
4.1. Characteristics of HCWs
A total of 98 healthcare workers (clinical (n = 56) and non-clinical staff (n = 42)) participated in the intervention (Table 4). Participants’ mean age was 40.5 years (SD = 9.1). Nearly three-fifths (59%) were women. The clinical staff reported having seen an average of eight sexual- or gender-minority clients in their departments in the past 3 months. None of the clinical staff and five of the non-clinical staff reported having received any focused training on the care of lesbian, gay, bisexual, and transgender (LGBT) people. About one-tenth of clinical (10.7%) and non-clinical staff (11.9%) reported having had a friend or acquaintance who self-identifies as a gay, bisexual, or transgender person.

Table 4.
Sociodemographic and other characteristics of HCWs participating in the Harmony intervention (N = 98).
4.1.1. Characteristics of MSM/TGW Participants of the Client Surveys
Independent samples of 200 hospital clients completed the pre-intervention (MSM = 100, TGW = 100) and post-intervention (MSM = 100, TGW = 100) client surveys (Table 5). Pre- and post-intervention participants were similar in age (mean age 29 years (SD 6.14); range: 19–48 years), monthly income (mean monthly income INR 10,939 (SD 7091)), and health insurance and antiretroviral treatment (ART) status. In the post-intervention period, a lower proportion of participants were engaged in sex work (p < 0.01). More than four-fifths (86%) of participants (pre-intervention: MSM: 76%, TGW: 97%; post-intervention: MSM: 78%, TGW: 96%) reported that their doctors knew about their sexual or gender identity.

Table 5.
Comparison of characteristics among pre- and post-intervention independent samples of MSM and TGW client surveys.
4.1.2. Outcomes among HCWs to Assess the Intervention Efficacy
Primary outcomes (Table 6).

Table 6.
Findings from multivariable analyses: Outcomes evaluation of ‘Harmony’ intervention among healthcare workers.
Positive attitudes towards MSM and TGW among HCWs: Positive attitude scores increased by 20% from baseline to follow-up (IRR = 1.20, 95% CI 1.07–1.32, p < 0.01) and by 30% from post-intervention to follow-up (IRR = 1.30, 95% CI 1.13–1.49, p < 0.001). Age (IRR = 0.99, 95% CI 0.98–0.99, p = 0.001) was negatively associated with positive attitudes scores, and women had higher positive attitudes scores when compared to men (IRR = 1.15, 95% CI 1.02–1.29, p = 0.01). Compared to HCWs in Chennai, those in Thane had lower positive attitudes scores (IRR = 0.81, 95% CI 0.72–0.91, p < 0.01).
Comfort level in providing care to MSM and TGW: A significant increase of 23% was observed from baseline to post-intervention (IRR = 1.23, 95% CI 1.08–1.41, p = 0.002) in the proportion of HCWs who endorsed the statement that they are comfortable providing care, support, and treatment services to MSM/TGW. Compared to HCWs in Chennai, those in Thane were more likely to endorse this statement (IRR = 1.23, 95% CI 1.04–1.44, p = 0.01). No significant difference was observed in the proportion of HCWs who endorsed the statement that MSM and TGW populations are often more difficult to care for, support, and treat.
Understanding healthcare challenges faced by MSM and TGW: A significant increase of 34% was observed in the proportion of HCWs from baseline to post-intervention (IRR = 1.34, 95% CI 1.004–1.79, p < 0.05) who endorsed the statement that most healthcare providers automatically make the assumption that all their patients are heterosexuals. No significant differences were observed in the proportion of HCWs who endorsed the statement that access to healthcare services is the same for MSM/TGW as for other members of the population.
Secondary outcomes (Table 6).
Support for hospital policies for MSM and TGW: The support for non-discriminatory hospital policy score significantly increased from baseline to post-intervention (IRR = 1.08, 95% CI 1.004–1.15, p < 0.05). Higher scores on understanding healthcare challenges faced by MSM/TGW (IRR = 1.05, 95% CI 1.03–1.06, p < 0.001) were positively associated with support for non-discriminatory hospital policies for MSM/TGW. Compared to HCWs in Chennai, those in Thane had lower scores on the support for hospital policies (IRR = 0.87, 95% CI 0.78–0.97, p < 0.05).
Importance of asking SOGI questions: The importance of asking SOGI questions score significantly increased by 17% from baseline to post-intervention (IRR = 1.17, 95% CI 1.06–1.29, p < 0.01). Understanding healthcare challenges faced by MSM/TGW (IRR = 1.04, 95% CI 1.01–1.07, p < 0.01) and endorsing the statement “If trans people request, gender-affirming procedures should be offered to them in government hospitals” (IRR = 1.23, 95% CI 1.07–1.39, p < 0.01) were positively associated with the importance of asking SOGI questions. Compared to HCWs in Chennai, those in Thane had lower scores on the importance of asking SOGI questions (IRR = 0.87, 95% CI 0.78–0.97, p < 0.05).
Perceived self-efficacy in providing clinical care to MSM and TGW: The perceived self-efficacy score among clinical staff significantly increased by 13% from baseline to post-intervention (IRR = 1.13, 95% CI 1.01–1.27, p < 0.05). However, a significant decrease was observed from baseline to follow-up and from post-intervention to follow-up. Endorsing the statement “If trans people request, gender-affirming procedures should be offered to them in government hospitals” was positively associated with perceived self-efficacy scores (IRR = 1.12, 95% CI 1.02–1.24, p < 0.05). Compared to HCWs in Chennai, those in Thane had lower scores on perceived self-efficacy (IRR = 0.88, 95% CI 0.78–0.99, p < 0.05).
Outcomes among MSM/TGW clients (Table 7).

Table 7.
Predictors of the outcomes among MSM and TGW who used healthcare services in the intervention hospitals.
Overall satisfaction with the hospital services: Among MSM in the post-intervention period, there was a 14% increase (IRR = 1.14, 95% CI 1.00–1.30, p < 0.05) in the percentage of those reporting overall satisfaction compared to the pre-intervention period. No significant change was observed for the combined sample of MSM/TGW or TGW. In the combined sample, each unit increase in discrimination experiences score was associated with a 7% reduction (IRR = 0.93, 95% CI 0.91–0.95, p < 0.001) in the percentage of those who reported having overall satisfaction with the hospital services. In both the combined sample and TGW sample, those on ART (a proxy for HIV-positive status) were more likely to report overall satisfaction compared to those not on ART.
Discrimination experiences related to sexual orientation and gender identity: The intervention among HCWs had no significant effect on the discrimination experiences score among MSM/TGW over time. However, among the combined sample, higher scores of positive experiences with HCWs and having insurance were significantly associated with a 12% (IRR = 0.88, 95% CI 0.85–0.92, p < 0.001) and 26% (IRR = 0.74, 95% CI 0.59–0.94, p < 0.05) reduction in discrimination experiences score, respectively. Additionally, higher income was associated with lower scores of discrimination experiences among the combined sample and MSM. Counterintuitively, TGW who engage in sex work were found to have lower scores of discrimination experiences compared to those not in sex work, although we did not ask whether participants disclosed their engagement in sex work to HCWs.
Positive experiences with HCWs: Positive experiences with HCWs among the combined sample of MSM/TGW significantly increased by 6% (IRR = 1.06, 95% CI 1.00–1.13, p < 0.05) after the intervention among HCWs and by 15% among TGW (IRR = 1.15, 95% CI 1.03–1.28, p < 0.05). Discrimination experiences score (IRR = 0.97, 95% CI 0.96–0.98, p < 0.001) and engagement in sex work (IRR = 0.94, 95% CI 0.88–0.99, p < 0.05) were negatively associated with positive experiences with HCWs score among the combined sample. Among the combined sample and TGW, having insurance was associated with lower positive experiences scores. Higher income was associated with higher scores of positive experiences among TGW.
4.2. Intervention Feasibility and Acceptability
The intervention was feasible—77 HCWs (78.5%) completed the post-intervention survey, and 51 HCWs (52.0%) completed the follow-up assessment, which was conducted two months after the workshop. Participants took 10 to 15 min to complete the survey questionnaire. Qualitative feedback from the participants indicated that they found the intervention to be useful and relevant, and a few participants wanted more resources and training (Table 8).

Table 8.
End-of-study comments from the healthcare workers (intervention participants).
5. Discussion
This study provides evidence for the feasibility, acceptability, and preliminary efficacy of a theory-informed multi-level pilot intervention among healthcare workers (HCWs) to reduce the stigma and discrimination faced by MSM and transgender women, contributing to the scant literature on this topic from India. This intervention significantly improved positive attitudes toward MSM/TGW as well as increasing the comfort level of HCWs in providing healthcare. Further, there was an increase in the support for non-discriminatory policies, endorsing the need to ask about sexual orientation and gender identity in clinical history taking, and understanding healthcare challenges faced by MSM/TGW. These findings were also corroborated by the client surveys conducted among MSM and TGW who accessed services in the two public hospitals (intervention sites) before and after the intervention among HCWs. The findings from the comparison of these users’ experiences demonstrated a significant increase in overall satisfaction with hospital services and improved positive interactions with HCWs over time.
Extensive literature is available from Western countries on the effect of training medical students and healthcare providers on clinical and cultural competency in providing care to LGBT people [13,14]. However, only very few studies from South Asia have focused on reducing stigma and discrimination faced by MSM and transgender people in healthcare settings; a majority focused on reducing HIV-related stigma [19]. From India, we are aware of only one earlier study, called the Shakti project [22], that developed an intervention among HCWs to reduce HIV-/STI-related stigma faced by transgender women in Mumbai through a one-day workshop, which resulted in significant improvements in positive attitudes among HCWs. Our Harmony intervention, which focused on reducing SOGI-related stigma and discrimination, employed a range of recommended strategies in the development and assessment of a pilot intervention [55]. These strategies included engagement of MSM and transgender communities (especially by sharing their real-life stories) and healthcare facility leadership and conducting a qualitative formative research study to understand the experiences of MSM and transgender people in accessing healthcare services, as well as to gain their inputs in refining the intervention and study tools. Further, we adapted the data collection tools and training curricula to the local context, involved key opinion leaders among HCWs who endorsed the intervention, and involved sexual- and gender-minority community leaders as co-trainers, a common component in effective training interventions [15]. We used participatory training techniques and videos to extend HCWs’ understanding of MSM and transgender communities and the issues they face in healthcare settings and gain support for actions against discrimination within public hospitals. Through these steps, we ensured that the intervention was culturally appropriate and obtained buy-in from the hospital administrators.
The difficulty in changing the attitudes of healthcare providers towards SGMs has been documented empirically in studies from the United States and Canada [15]. In the Harmony intervention, post-intervention, there was no significant increase in positive attitudes. However, compared to pre-intervention, the effect of the intervention on positive attitudes was found to be positive and significant in the follow-up assessment and increased from post-intervention to follow-up. This could be partly because of the four videos shared with the HCWs after the workshop over one month, which might have acted as boosters. This suggests that in order to reinforce new information or values, it may be useful to offer follow-up booster training or other ways of sharing information or building skills that are tailored to the specific needs of various categories of HCWs. The original plan was to have a one-day workshop for HCWs. Because of COVID-19-pandemic-related duties, the time available for HCWs was very limited; thus, we had to shorten the duration of the workshop to a half day. Still, we made it participatory and arranged interactive sessions with MSM and trans community representatives (in line with the intergroup contact hypothesis) and obtained significant improvements in key outcomes despite the short duration of the workshop.
We found that compared to HCWs in Chennai (a large metropolitan city in South India), those in Thane (a city in Western India) were more likely to have lower positive attitudes, lower comfort level, and lower perceived self-efficacy in providing clinical care. This means that a more intensive approach to understanding and addressing the prejudices and biases behind regional differences that might contribute to these findings is needed, and future interventions need to consider the possibility of higher levels of pre-existing negative attitudes towards SGMs in certain regions.
One of the secondary outcomes, perceived self-efficacy in providing clinical care (score), significantly decreased from post-intervention to the follow-up assessment period. This is understandable as the workshop and videos focused on improving the attitudes toward and understanding of SGM (cultural competency) [56] and not on improving clinical skills (e.g., in sexual history taking or providing gender-affirmative hormone therapy). This finding, however, points out the importance of focusing on improving relevant clinical and counselling skills among HCWs, tailored to their role in the provision of care to SGMs. In fact, training workshops to improve cultural competency among HCWs need to be followed by or complemented by training workshops to improve clinical competency [57]. Similarly, an increase in discrimination experiences score was associated with a reduction in overall satisfaction with the hospital services and reduction in positive experiences with HCWs, highlighting the connection between perceived quality of care and discrimination experiences and the possibility of training HCWs on SGM health as training for improving the quality of services, as suggested by a government official.
Studies from India have reported several barriers to healthcare access for MSM and TGW, especially discrimination and negative experiences with HCWs [5,6]. Those studies have reported verbal or physical abuse, lack of correct knowledge about SGM misgendering transgender people, and lack of confidentiality. The findings from this pilot intervention suggest that HCWs are willing to learn about SGMs, and the intervention is acceptable and feasible.
6. Limitations and Strengths
This study has several limitations. First, by the very nature of the pre- and post-test study design of the intervention among HCWs, there was no control group, and the participants served as their own control. A vast majority of the participants self-reported that they had never received any specific training on SGM, and our discussions with hospital administrators did not reveal any LGBT-specific training provided in those hospitals. It is possible that after attending the Harmony intervention workshops, some HCWs might have been motivated to self-learn about SGM and their health issues, which could have contributed to improvements in outcomes as well. Nevertheless, the lack of any focused interventions at the hospital level and lack of structured training programs on the health of SGM mean that the observed outcomes were most likely due to the Harmony intervention’s effects.
Second, some of the scales were used for the first time or were created with items adapted from diverse sources, with partial validation by the findings from the qualitative formative research conducted among MSM and transgender communities. The focus of the study was not to validate the scales but to have reasonable parsimonious measures to assess changes in the key outcomes, especially in the context of a pilot intervention. To ensure the validity of the scales, we checked with community experts for face validity, conducted pilot testing, and checked for factorability. The reliability of the scales, except the scale on support for hospital non-discriminatory policy, was adequate. However, the convergent and divergent validity of these scales is yet to be established in the Indian context. Future studies can explicitly check for these aspects of the scales used. Third, there was a relatively longer duration (3 to 4 months) between the second and third data collection points in one of the two study sites due to the COVID-19 pandemic, which means that it is possible that the effect of the intervention might have waned during that period and might have reduced the power to detect statistically significant changes. Retention of change is rarely assessed in provider education interventions [15]; the Harmony intervention, however, included a follow-up assessment period as well, which was a strength of this study.
Fourth, social desirability bias might have led some HCWs to underreport any negative attitudes towards their MSM and TGW clients. As we did not collect any identifying information from HCWs that could be linked to their responses, they are less likely to have underreported negative attitudes or actions. Even if there had been social desirability bias, it would then be present in both pre- and post-intervention assessments and, thus, unlikely to bias the magnitude and direction of the effect of the intervention. However, social desirability bias would not explain the increase in overall satisfaction with hospital services and the increase in positive interactions reported by MSM and transgender people who used public hospitals after the intervention period (when compared to those who used those services prior to the intervention). Fifth, given the re-emergence of the COVID-19 pandemic during the follow-up assessment period, we could not obtain responses from about half of the HCWs. Additionally, for follow-up, the online survey might have further decreased the response rate as some HCWs might not be familiar with completing a survey online. As we used multi-level modelling that automatically adjusts for missing outcome variables, with the assumption of missing at random, fitting the models to the observed data will give valid results. Further, we conducted a sensitivity analysis using multiple imputations for the key outcomes and found that the results were similar. Hence, the inferences are most likely to be valid despite the missing data.
7. Lessons Learnt and Implications
The involvement of MSM and TGW communities and buy-in from the local key stakeholders (State AIDS Control Societies and hospital administration) were key to the successful implementation of the intervention and may be helpful for the sustainability of educational and awareness creation activities in public hospitals. Initiating training interventions on SGM health and stigma reduction, thus, requires support from the participating hospital administration, which is more likely to be obtained if government agencies like NACO organise or support the training and make such training part of the orientation programme for HCWs who provide services under the National AIDS Control Programme. The COVID-19 pandemic posed challenges in bringing together HCWs for the workshop; however, commitment from the hospital administration helped in conducting these workshops, even though the duration of the workshop was reduced from one day to a half day, retaining the essential content. This means flexibility in the duration and content of the workshop may be needed considering local contexts. Interactions with MSM and TGW community representatives were greatly appreciated by HCWs, a majority of whom had not interacted with MSM and TGW prior to the workshop. The involvement of MSM and TGW communities is key and needs to be an essential component of any training interventions among HCWs.
The patient redressal committees in public hospitals, including those redressal committees in antiretroviral treatment centres, should be open to register complaints from SGMs and resolve those issues. The Harmony intervention modules focused on increasing positive attitudes towards sexual and gender minorities; however, some MSM and TGW engage in sex work, and some are living with HIV. This could be a reason why the Harmony intervention did not significantly reduce the discrimination reported by service users as it primarily focused on reducing sexual and trans prejudice and not the attitudes and prejudices related to HIV and sex work. Thus, future interventions among HCWs need to explicitly address this intersectionality and have modules to address the intersectional stigma faced by SGM in relation to not only sexual orientation and gender identity but also in relation to sex work status, HIV status, and physical ability, among other intersecting marginalised statuses. Such interventions can also include information on the anti-discrimination clauses in the Transgender Persons (Protection of Rights) Act, 2019 [58] and the HIV and AIDS (Prevention and Control) Act, 2017 [59] so that HCWs understand the consequences of discriminating against patients in healthcare settings. The Harmony intervention research was conducted among clinical and non-clinical staff in public hospitals. While such supplemental targeted training interventions are important for HCWs currently working in hospitals, a comprehensive curriculum for health and allied professional students in undergraduate and postgraduate medical/nursing colleges on the health needs of SGMs can be developed by the National Medical Commission of India, in consultation with the Ministry of Health and Family Welfare and National AIDS Control Organisation to ensure discrimination-free healthcare settings in the future. Online training modules on SGM health issues with post-completion certificates or CME (continuous medical education) credits will encourage the voluntary participation of HCWs. NACO can conduct periodic national surveys to monitor stigma and discrimination against SGMs in healthcare and other settings. The findings from those studies can help in taking evidence-informed actions to achieve the global and national target of reducing stigma and discrimination faced by key populations to <10% by 2025.
8. Conclusions
Reducing stigma and discrimination faced by SGMs in healthcare settings is key to improving access to health services, especially sexual- and HIV-related health services, contributing to India’s effort to end the AIDS epidemic by 2030. With the active involvement of SGM communities, we developed, implemented, and evaluated a brief multi-level pilot intervention among HCWs for improving positive attitudes toward MSM and transgender people as well as helping them to better understand the issues faced by these populations in healthcare settings. This pilot intervention, which combined an in-person workshop and videos, improved HCWs’ attitudes, and comfort levels in providing care for MSM and transgender people, increased support for non-discriminatory hospital policies. Our interactions with HCWs and the results from community surveys indicate that the intervention also needs to address stigma related to sex work and HIV status and not just sexual orientation and gender identity. Overall, the findings support scaling up this intervention by incorporating the lessons learnt in measuring and addressing intersecting stigma and support the training needs of diverse HCWs, enabling them to provide non-discriminatory and culturally competent health services to sexual and gender minorities in India.
Author Contributions
Conceptualization and methodology, V.C., K.R., S.N., S.S., V.V., C.D. and S.R. (Shobini Rajan); data curation, M.S., R.N., B.M. and S.T.S.; software and formal analysis, V.C., J.K. and S.T.S.; writing—original draft preparation, V.C. and M.S.; writing—review and editing, V.C., J.K., V.V., N.K., K.R., S.N., S.S., S.R. (Shruta Rawat), C.D., S.R. (Shobini Rajan), U.D., A.K.P., B.R., B.S.K. and T.E.; supervision, C.D., S.R. (Shobini Rajan), A.K.P., B.R., T.E. and B.S.K.; project administration, V.V., N.K., B.R., M.S., U.D., T.E. and S.R. (Shruta Rawat); funding acquisition, C.D., S.R. (Shobini Rajan), A.K.P. and B.S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a grant (Ref. number: T-11020/79/2019-NACO[R&D]) from the Global Fund to fight against AIDS, Tuberculosis and Malaria to National AIDS Control Organization (NACO), Ministry of Health and Family Welfare, Government of India. The funders had no role in the study design, data analysis, decision to publish, or preparation of the manuscript.
Institutional Review Board Statement
The study protocol was approved by the Institutional Review Boards (IRBs) of the Centre for Sexuality and Health Research and Policy (Ref. 221/2021), Tata Institute of Social Sciences (Ref. 2020-2021/31), and the Humsafar Trust (Ref. 52-06/2021 & 52/1-12/2021).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
The data underlying the results presented in the study are available from the Head of Department—Strategic Information (hod.simu@gmail.com), National AIDS Control Organisation, Ministry of Health & Family Welfare, Government of India. Access will be granted to de-identified datasets on a case-by-case basis.
Acknowledgments
We sincerely thank our community partners—Sahodaran and Thozhi in Chennai, Ekta Foundation in Airoli and Triveni Samaj Vikas Kendra in Kalwa, Thane—for their support in the recruitment of and data collection among service users. We gratefully acknowledge the support of the Maharashtra State AIDS Control Society (MSACS) and Tamil Nadu State AIDS Control Society (TANSACS). We thank Ramakant Gaikwad, AiM Institute, Mumbai; and Amenla Nuken, ICRW, New Delhi, for their inputs on the study design and tools. We would also like to thank the support from the leadership of Madras Medical College and Thane Civil Hospital. V.C. received support from the DBT/Wellcome Trust India Alliance Senior fellowship (IA/CPHS/16/1/502667).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Parker, R.; Aggleton, P. HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Soc. Sci. Med. 2003, 57, 13–24. [Google Scholar] [CrossRef]
- Goffman, E. Stigma: Notes on the Management of Spoiled Identity; Prentice-Hall: Englewood Cliffs, NJ, USA, 1963. [Google Scholar]
- Herek, G.M.; McLemore, K.A. Sexual prejudice. Annu. Rev. Psychol. 2013, 64, 309–333. [Google Scholar] [CrossRef]
- Herek, G.M. Stigma and Sexual Orientation: Understanding Prejudice against Lesbians, Gay Men, and Bisexuals; Sage Publications: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Chakrapani, V.; Newman, P.A.; Shunmugam, M.; Dubrow, R. Barriers to free antiretroviral treatment access among kothi-identified men who have sex with men and aravanis (transgender women) in Chennai, India. AIDS Care 2011, 23, 1687–1694. [Google Scholar] [CrossRef] [PubMed]
- Woodford, M.R.; Chakrapani, V.; Newman, P.A.; Shunmugam, M. Barriers and facilitators to voluntary HIV testing uptake among communities at high risk of HIV exposure in Chennai, India. Global Public Health 2016, 11, 363–379. [Google Scholar] [CrossRef] [PubMed]
- Lurie, S. Identifying Training Needs of Health-Care Providers Related to Treatment and Care of Transgendered Patients: A Qualitative Needs Assessment Conducted in New England. Int. J. Transgenderism 2005, 8, 93–112. [Google Scholar] [CrossRef]
- Ayhan, C.H.B.; Bilgin, H.; Uluman, O.T.; Sukut, O.; Yilmaz, S.; Buzlu, S. A Systematic Review of the Discrimination Against Sexual and Gender Minority in Healthcare Settings. Int. J. Health Serv. 2020, 50, 44–61. [Google Scholar] [CrossRef]
- UNAIDS. Miles to Go: Closing Gaps, Breaking Barriers, Righting Injustices; Global AIDS Update 2018; UNAIDS: Geneva, Switzerland, 2018. [Google Scholar]
- NACO. National Strategic Plan for HIV/AIDS and STI 2017—24: Paving the Way for an AIDS-Free India; NACO, Ministry of Health & Family Welfare, Government of India: New Delhi, India, 2017.
- Palchaudhuri, R.; Niggl, M.; Palmer, C.S. Eliminating HIV & AIDS in India: A roadmap to zero new HIV infections, zero discrimination & zero AIDS-related deaths. Indian J. Med. Res. 2016, 144, 789–792. [Google Scholar] [CrossRef]
- Bharat, S.; Chakrapani, V.; Shunmugam, M.; Eshwarlal, A. HIV-Related Stigma Research in India: Current Knowledge, Gaps, and Recommendations; United Nations Development Programme: New Delhi, India, 2014. [Google Scholar]
- Sekoni, A.O.; Gale, N.K.; Manga-Atangana, B.; Bhadhuri, A.; Jolly, K. The effects of educational curricula and training on LGBT-specific health issues for healthcare students and professionals: A mixed-method systematic review. J. Int. AIDS Soc. 2017, 20, 21624. [Google Scholar] [CrossRef]
- Hunt, R.; Bates, C.; Walker, S.; Grierson, J.; Redsell, S.; Meads, C. A Systematic Review of UK Educational and Training Materials Aimed at Health and Social Care Staff about Providing Appropriate Services for LGBT plus People. Int. J. Environ. Res. Public Health 2019, 16, 4976. [Google Scholar] [CrossRef]
- Morris, M.; Cooper, R.L.; Ramesh, A.; Tabatabai, M.; Arcury, T.A.; Shinn, M.; Im, W.; Juarez, P.; Matthews-Juarez, P. Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: A systematic review. BMC Med. Educ. 2019, 19, 325. [Google Scholar] [CrossRef]
- Radix, A.; Maingi, S. LGBT Cultural Competence and Interventions to Help Oncology Nurses and Other Healthcare Providers. Semin. Oncol. Nurs. 2018, 34, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Minturn, M.S.; Martinez, E.I.; Le, T.; Nokoff, N.; Fitch, L.; Little, C.E.; Lee, R.S. Early Intervention for LGBTQ Health: A 10-Hour Curriculum for Preclinical Health Professions Students. MedEdPORTAL 2021, 17, 11072. [Google Scholar] [CrossRef] [PubMed]
- Poteat, T.; Park, C.; Solares, D.; Williams, J.K.; Wolf, R.C.; Metheny, N.; Vazzano, A.; Dent, J.; Gibbs, A.; Nonyane, B.A.S.; et al. Changing hearts and minds: Results from a multi-country gender and sexual diversity training. PLoS ONE 2017, 12, e0184484. [Google Scholar] [CrossRef]
- Pollack, T.M.; Duong, H.T.; Vinh, D.T.N.; Phuong, D.T.; Thuy, D.H.; Nhung, V.T.T.; Uyen, N.K.; Linh, V.T.; Van Truong, N.; Le Ai, K.A.; et al. A pretest-posttest design to assess the effectiveness of an intervention to reduce HIV-related stigma and discrimination in healthcare settings in Vietnam. J. Int. AIDS Soc. 2022, 25, e25932. [Google Scholar] [CrossRef]
- Lelutiu-Weinberger, C.; Pollard-Thomas, P.; Pagano, W.; Levitt, N.; Lopez, E.I.; Golub, S.A.; Radix, A. Implementation and Evaluation of a Pilot Training to Improve Transgender Competency Among Medical Staff in an Urban Clinic. Transgender Health 2016, 1, 45–53. [Google Scholar] [CrossRef]
- Lacombe-Duncan, A.; Logie, C.H.; Persad, Y.; Leblanc, G.; Nation, K.; Kia, H.; Scheim, A.I.; Lyons, T.; Horemans, C.; Olawale, R.; et al. Implementation and evaluation of the ‘Transgender Education for Affirmative and Competent HIV and Healthcare (TEACHH)’ provider education pilot. BMC Med. Educ. 2021, 21, 561. [Google Scholar] [CrossRef]
- Banik, S.; Srivastava, A.; Setia, M.S.; Jerajani, H.; Anand, A.; Bockting, W.; Fisher, L. Exploring HIV stigma and transphobia among healthcare providers in Mumbai, India: Preliminary findings from project Shakti. In Proceedings of the 141st APHA Annual Meeting and Exposition, Boston, MA, USA, 2–6 November 2013. [Google Scholar]
- Altman, D.; Aggleton, P.; Williams, M.; Kong, T.; Reddy, V.; Harrad, D.; Reis, T.; Parker, R. Men who have sex with men: Stigma and discrimination. Lancet 2012, 380, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Shadish, W.R.; Cook, T.D.; Campbell, D.T. Experimental and Quasi-Experimental Designs for Generalized Causal Inference; Wadsworth, Cengage Learning: Belmont, CA, USA, 2002. [Google Scholar]
- Reichardt, C.S.; Little, T.D. Quasi-Experimentation: A Guide to Design and Analysis; The Guilford Press: New York, NY, USA, 2019. [Google Scholar]
- Mohan, B.; Ranade, K.; Nair, S.; Das, U.; Nuken, A.; Gaikwad, R. Experiences of MSM and transgender women in accessing healthcare services from public hospitals: A qualitative study from India. In Proceedings of the the 24th International AIDS Conference, Montreal, QC, Canada, 29 July–2 August 2022; International AIDS Society: Geneva, Switzerland, 2022. [Google Scholar]
- Dixon, J.; Durrheim, K.; Stevenson, C.; Cakal, H. From Prejudice Reduction to Collective Action: Two Psychological Models of Social Change (and How to Reconcile Them). In The Cambridge Handbook of the Psychology of Prejudice. Cambridge Handbooks in Psychology; Sibley, C.G., Barlow, F.K., Eds.; Cambridge University Press: Cambridge, UK, 2016; pp. 481–499. [Google Scholar]
- Kelly, J.A. Popular opinion leaders and HIV prevention peer education: Resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care 2004, 16, 139–150. [Google Scholar] [CrossRef]
- Christ, O.; Kauff, M. Intergroup Contact Theory. In Social Psychology in Action: Evidence-Based Interventions from Theory to Practice; Sassenberg, K., Vliek, M.L.W., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 145–161. [Google Scholar]
- Li, L.; Guan, J.; Liang, L.J.; Lin, C.; Wu, Z. Popular Opinion Leader intervention for HIV stigma reduction in healthcare settings. AIDS Educ. Prev. 2013, 25, 327–335. [Google Scholar] [CrossRef]
- Feyissa, G.T.; Lockwood, C.; Woldie, M.; Munn, Z. Reducing HIV-related stigma and discrimination in healthcare settings: A systematic review of quantitative evidence. PLoS ONE 2019, 14, e0211298. [Google Scholar] [CrossRef]
- Walch, S.E.; Sinkkanen, K.A.; Swain, E.M.; Francisco, J.; Breaux, C.A.; Sjoberg, M.D. Using Intergroup Contact Theory to Reduce Stigma Against Transgender Individuals: Impact of a Transgender Speaker Panel Presentation. J. Appl. Soc. Psychol. 2012, 42, 2583–2605. [Google Scholar] [CrossRef]
- Bartos, S.E.; Berger, I.; Hegarty, P. Interventions to reduce sexual prejudice: A study-space analysis and meta-analytic review. J. Sex Res. 2014, 51, 363–382. [Google Scholar] [CrossRef] [PubMed]
- Paluck, E.L.; Green, D.P. Prejudice reduction: What works? A review and assessment of research and practice. Annu. Rev. Psychol. 2009, 60, 339–367. [Google Scholar] [CrossRef] [PubMed]
- Chakrapani, V. Understanding Men Who Have Sex with Men (MSM) and Hijras & Providing HIV/STI Risk Reduction Information. Basic Training for Clinicians and Counselors in Sexual Health/STI/HIV. Trainer’s Manual. 2005. Available online: http://www.indianlgbthealth.info/Training/Downloads/TOT_FINAL_Sep2005.pdf (accessed on 10 October 2022).
- Makadon, H.J.; Mayer, K.H.; Potter, J.; Goldhammer, H. The Fenway Guide to Lesbian, Gay, Bisexual, and Transgender Health; American College of Physicians: Philadelphia, PA, USA, 2008. [Google Scholar]
- IOM. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding; The National Academies Press: Washington, DC, USA, 2011; 366p. [Google Scholar]
- Deutsch, M.B. (Ed.) Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People; UCSF Gender Affirming Health Program, Department of Family and Community Medicine, University of California San Francisco: San Francisco, CA, USA, 2016. [Google Scholar]
- ISEAN. Sexual Orientation, Gender Identity and Expression (SOGIE) Training Package; ISEAN: Jakarta, Indonesia, 2015. [Google Scholar]
- Paluck, E.L.; Porat, R.; Clark, C.S.; Green, D.P. Prejudice Reduction: Progress and Challenges. Annu. Rev. Psychol. 2021, 72, 533–560. [Google Scholar] [CrossRef]
- Hertzog, M.A. Considerations in determining sample size for pilot studies. Res. Nurs. Health 2008, 31, 180–191. [Google Scholar] [CrossRef]
- Donisi, V.; Amaddeo, F.; Zakrzewska, K.; Farinella, F.; Davis, R.; Gios, L.; Sherriff, N.; Zeeman, L.; Mcglynn, N.; Browne, K.; et al. Training healthcare professionals in LGBTI cultural competencies: Exploratory findings from the Health4LGBTI pilot project. Patient Educ. Couns. 2020, 103, 978–987. [Google Scholar] [CrossRef]
- Van der Elst, E.M.; Smith, A.D.; Gichuru, E.; Wahome, E.; Musyoki, H.; Muraguri, N.; Fegan, G.; Duby, Z.; Bekker, L.-G.; Bender, B.; et al. Men who have sex with men sensitivity training reduces homoprejudice and increases knowledge among Kenyan healthcare providers in coastal Kenya. J. Int. AIDS Soc. 2013, 16 (Suppl. S3), 18748. [Google Scholar] [CrossRef]
- Shetty, G.; Sanchez, J.A.; Lancaster, J.M.; Wilson, L.E.; Quinn, G.P.; Schabath, M.B. Oncology healthcare providers’ knowledge, attitudes, and practice behaviors regarding LGBT health. Patient Educ. Couns. 2016, 99, 1676–1684. [Google Scholar] [CrossRef]
- Crisp, C. The Gay Affirmative Practice Scale (GAP): A New Measure for Assessing Cultural Competence with Gay and Lesbian Clients. Social Work 2006, 51, 115–126. [Google Scholar] [CrossRef]
- Herek, G.M.; McLemore, K.A. The Attitudes Toward Lesbians and Gay Men (ATLG) scale. In Handbook of Sexuality-Related Measures, 4th ed.; Fisher, T., Davis, C.M., Yarber, W.L., Davis, S.L., Eds.; Taylor & Francis: New York, NY, USA, 2019; pp. 637–639. [Google Scholar]
- Andrinopoulos, K.; Hembling, J.; Guardado, M.E.; de Maria Hernandez, F.; Nieto, A.I.; Melendez, G. Evidence of the negative effect of sexual minority stigma on HIV testing among MSM and transgender women in San Salvador, El Salvador. AIDS Behav. 2015, 19, 60–71. [Google Scholar] [CrossRef]
- Arvind, R.; Vinay, C. (Eds.) Nothing to Fix: Medicalisation of Sexual Orientation and Gender Identity: A Human Rights Resource Book; SAGE Yoda Press: New Delhi, India, 2016. [Google Scholar]
- McCann, E.; Sharek, D. Survey of lesbian, gay, bisexual, and transgender people’s experiences of mental health services in Ireland. Int. J. Ment. Health Nurs. 2014, 23, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Twisk, J.W.R. Applied Mixed Model Analysis: A Practical Guide, 2nd ed.; Cambridge University Press: Cambridge, UK, 2019. [Google Scholar]
- Suárez, E.; Pérez, C.M.; Rivera, R.; Martínez, M.N. Poisson Regression Models for Cohort Studies. In Applications of Regression Models in Epidemiology; Suárez, E., Pérez, C.M., Rivera, R., Martínez, M.N., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2017; pp. 141–164. [Google Scholar]
- Zou, G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. Am. J. Epidemiol. 2004, 159, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Rabe-Hesketh, S.; Skrondal, A. Multilevel and Longitudinal Modeling Using Stata; Categorical Responses, Counts, and Survival; Stata Press: College Station, TX, USA, 2022; Volume 2. [Google Scholar]
- Twisk, J.W.R. Applied Longitudinal Data Analysis for Epidemiology: A Practical Guide; Cambridge University Press: Cambridge, UK, 2015. [Google Scholar]
- Gitlin, L.N.; Czaja, S.J. Behavioral Intervention Research: Designing, Evaluating, and Implementing; Springer: New York, NY, USA, 2016. [Google Scholar]
- Pratt-Chapman, M.L.; Eckstrand, K.; Robinson, A.; Beach, L.B.; Kamen, C.; Keuroghlian, A.S.; Cook, S.; Radix, A.; Bidell, M.P.; Bruner, D.; et al. Developing Standards for Cultural Competency Training for Healthcare Providers to Care for Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, and Asexual Persons: Consensus Recommendations from a National Panel. LGBT Health 2022, 9, 340–347. [Google Scholar] [CrossRef]
- Hanssmann, C.; Morrison, D.; Russian, E. Talking, gawking, or getting it done: Provider trainings to increase cultural and clinical competence for transgender and gender-nonconforming patients and clients. Sex. Res. Soc. Policy 2008, 5, 5. [Google Scholar] [CrossRef]
- GoI. The Transgender Persons (Protection of Rights) Act, 2019; No. 40; Ministry of Law and Justice, Government of India: New Delhi, India, 2019.
- GoI. The Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome (Prevention and Control) Act, 2017; Ministry of Law and Justice, Government of India: New Delhi, India, 2017.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).