Abstract
Background: Female sex workers (FSWs) are at a higher risk of contracting and transmitting HIV and other sexually transmitted infections (STIs). We aimed to explore the sexual behaviour, knowledge and attitudes towards STIs, barriers, support and intervention for STI screening. Methods: In this community-based, concurrent quantitative–qualitative, exploratory mixed-methods study, we administered 87 semi-structured quantitative and six in-depth interviews to purposively select FSWs in Gulu City, Uganda. The qualitative methodology was based on descriptive phenomenology. Results: The quantitative study included 87 FSWs, with a median age of 28 years. Overall, 87.4% (n = 76) participants reported condom use during their last sexual encounter. Eighty-three (95.4%) participants were aware of their HIV status, with 6% (n = 5) reporting being HIV-positive. Seventy-six (87.4%) participants reported contracting at least one STI during sex work. In addition, 66.7% (n = 58) of the participants reported being screened for STIs in the past three months, with vulvovaginal candidiasis (55.3%, n = 42) and syphilis (32.9%, n = 25) being the most common STIs. However, only 2.3% (n = 2) of the participants reported current STIs symptoms. In the qualitative study, the main themes encompassed sexual behaviour, including condom-use negotiation strategies and challenges, as well as screening facilitators and barriers. Condom-use negotiation tactics involved leveraging health-risk information, increased charges for unprotected sex, and outright refusal. Complex challenges included limited agency in promoting safe sex due to economic reliance, vulnerability to violence, and difficulties in controlling the sexual environment. Facilitators for regular screening included social influences, emotional relief, established testing habits, and accessible clinics, while barriers encompassed cost, stigma, doubts about test accuracy, and inconvenient clinic hours. Conclusions: FSWs face significant vulnerabilities in Gulu City, Uganda, regarding STIs. While encouraging trends such as high HIV awareness and condom usage were observed, persistent challenges in STI screening, negotiation of safe sex practices, and access to prevention and treatment remain evident. To address these concerns, targeted interventions should be developed to enhance STI screening accessibility, empower sex workers with effective negotiation skills, and provide comprehensive support for STI prevention and treatment, thereby contributing to improved overall sexual health and well-being among this marginalized population.
1. Introduction
Sexually transmitted infections (STIs) are a global public health concern, disproportionately affecting marginalised and vulnerable populations such as female sex workers (FSWs) [1,2]. According to the World Health Organization (WHO), more than 1 million STIs are acquired daily worldwide, translating to about 374 million new infections yearly [3]. FSWs are at high risk of acquiring and transmitting STIs due to the nature of their work and related risk behaviours [4]. In fact, in 2021, the prevalence of HIV among sex workers in Uganda was estimated at 31.3%, about five times that of the general Ugandan population (6.3%) [2]. Furthermore, a recent publication from Southern Uganda revealed that about 10.5% of FSWs tested positive for one of three STIs, including Neisseria gonorrhoea, Chlamydia trachomatis and Trichomonas vaginalis [5]. Furthermore, STIs are associated with severe health consequences impacting sexual and reproductive health, such as infertility, pelvic inflammatory disease, increased risk of HIV transmission, and other germs associated with cancers [3].
Despite the known high burden and ruinous effects of STIs among FSWs, the uptake of STI screening among FSWs is still low in Uganda, with rates of testing for other STIs, such as syphilis, being significantly lower than those of HIV [6,7,8]. To address the burden of STIs, the WHO supports countries to implement the global health sector strategies on HIV, viral hepatitis and STIs, 2022–2030, action 89: expand access to STI screening services for priority populations [9]. As such, inexpensive, rapid tests have been made available for STIs such as syphilis and HIV in resource-limited settings such as Uganda [3]. However, several factors still impede FSWs from accessing STI screening services, including stigma, discrimination, limited access to healthcare services, poor-quality services, and often out-of-pocket expenses [3,10].
Regular screening enables timely detection, diagnosis and eventual intervention among FSWs with STIs and prevents the spread of the infections to other individuals [11,12]. However, there are limited data specifically examining STI screening practices in this population in Northern Uganda. Therefore, this study’s findings will inform the development of effective and evidence-based STI screening programs for targeted interventions to address this urgent public health concern. This study aimed to explore the practices of FSWs in Northern Uganda, regarding screening for STIs.
2. Methods
2.1. Study Design
This study was a community-based, concurrent, exploratory mixed-methods study that employed both quantitative and qualitative data collection methods. We adhered to both STROBE [13] AND COREQ [14] guidelines. The study was conducted between February and March 2023.
2.1.1. Study Setting and Participants
The study was conducted in Gulu City, Uganda, a high-risk area for STIs due to its high prevalence of sex work. The study participants were FSWs aged 18 years and above currently working in Gulu City.
2.1.2. Quantitative Data Collection
We used a cross-sectional survey to collect quantitative data from FSWs. We developed a structured questionnaire on socio-demographic characteristics, sexual behaviour, STI knowledge and screening practices. The survey was administered to a convenience sample of 87 FSWs recruited from different hotspots in Gulu City. The survey was conducted face-to-face by trained research assistants fluent in English and Luo, the local language.
2.1.3. Qualitative Data Collection
We used in-depth interviews (IDIs) to collect qualitative data from FSWs. The qualitative interviews were with FSWs who were not included in the quantitative sample. We conducted 6 IDIs with FSWs. The IDIs were conducted in English and Luo and were audio-recorded with consent from the participants. Qualitative interviews explored sexual behaviour, knowledge and attitudes towards STIs, barriers to STI screening, and support and intervention for STI prevention and treatment.
2.1.4. Data Analysis
Quantitative data were analysed using STATA version 17. Descriptive statistics, including frequencies, percentages, median and interquartile range (IQR), means, and standard deviations, were obtained. Qualitative data were transcribed and translated into English. Finally, we used thematic analysis to analyse the qualitative data, which involved identifying and categorising emerging themes from the data.
2.1.5. Ethical Considerations
The study received ethical approval from the Gulu University Research Ethics Committee (approval number: GUREC-2022-414). Informed consent was obtained from all participants before the start of the study. Participants were informed of their right to withdraw from the study at any time and that their participation was voluntary. All data collected were kept confidential and anonymous. The ethical principles outlined in the Declaration of Helsinki were all observed. We also ensured the privacy and confidentiality of the study participants by using pseudonyms and de-identifying the data during analysis and reporting. We provided free STI screening services to the participants who requested them after the study.
3. Results
3.1. Quantitative Results
3.1.1. Socio-Demographic Characteristics
We included 87 participants, with a median age of 28 (IQR: 28–33) years. Most of the participants had a secondary education level (52.9%), lived in urban areas (95.4%) compared to rural areas (4.6%), were married (43.7%), and Catholic (68.8%). The age of first sexual encounter among the participants was 16 years, with an IQR of 15–17 years. About 26.4% (n = 23) of the participants reported that sex work was their primary source of income. The median number of pregnancies was two, ranging from one to four. About 55.2% of the participants reported a history of abortions, Table 1.

Table 1.
Baseline characteristics of the study participants.
3.1.2. Condom Use, HIV and Other STI Screening Practices
Table 2 presents information on condom use, HIV and other STI screening practices among the study participants. Of the 87 FSWs, 96.6% reported using condoms for pregnancy prevention in the last month, while 87.4% reported using a condom during their last sexual encounter. In addition, most of the participants reported occasional condom use (92.0%), while only a few participants reported always using (5.8%) or never using (2.3%) condoms.

Table 2.
Condom use, HIV and other STID screening practices.
Most participants were aware of their HIV status (95.4%). Among those aware of their status, 94% reported being HIV negative, while 6% reported being HIV-positive.
Regarding STI screening practices, 66.7% of the participants reported being screened for STI in the past three months. Among those who were screened, the majority reported screening based on symptoms (90.8%), while only a few reported monthly screening (8.1%) or never being screened (1.2%). Among those who reported having an STI (n = 76), the most reported STIs were vulvovaginal candidiasis (55.3%) and syphilis (32.9%), while Chlamydia and gonorrhoea were reported by fewer participants (6.6% and 5.3%, respectively). Only 2.3% of the participants reported current STI symptoms.
3.2. Qualitative Results
Six participants were interviewed. Their age ranged from 23 to 40 years, and they had been involved in sex work for 2–20 years. They had one to three biological children. Most had only primary or no formal education, while a few had completed secondary education. Most participants solicited clients on the street, in bars/clubs, or in brothels. In addition, some participants solicited clients at lodges or homes. Most participants engaged in sex work full-time, with no other source of income to supplement their income. A few engaged in sex work part-time while also having other income sources or being a student.
3.2.1. Theme 1: Sexual Behaviour
Sub-Theme 1: Condom-Use Negotiation
The data analysis unveiled four distinct categories of strategies that FSWs employed to negotiate condom usage with their clients. These strategies included: requesting and ensuring condom use, leveraging "health-risk information" to either motivate or warn clients about condom use, implementing a higher charge for unprotected sex, and declining to engage in unprotected sexual activities.
Requesting and enforcing the use of a condom: The data revealed that FSWs would produce a condom and show it or give it to a client for enforcement. In addition, FSWs would ask the client about the number of preferred condoms or whether the client had his condom.
“My initial demand is for money, and at the same time, I make it clear that I have a condom on hand”(A 40-year-old, HIV-positive, 20 years of sex work).
“When we enter a room, I ask my client “do you have a condom?” because sometimes clients, when you offer them a condom, will tell you “do not worry, I have my condom.” But some tear the condom up without you noticing, you will realise by the wetness during sex that the condom has burst”(A 34-year-old, HIV-positive, ten years of sex work).
Using the health-risk information to threaten or motivate clients: some FSWs reported using health-risk information as a threat or motivation for the clients to agree to use condoms.
“You are seeing me for the first time… and you already want to have sex without a condom while I do high-risk work?…We (FSWs), when it comes to illnesses, we are topping the list; we are the ones that are killing people (with HIV); why don’t you take care of yourself? I value my life; I do not want to have a relationship with you because I do not want to see myself sick and die, so please listen to me, and we use condoms…”(A 37-year-old, HIV-positive, eight years of sex work).
“…If you do not want to use a condom, you will end up being infected (with HIV and other STIs) because I have had infectious abscesses in the vagina… I have AIDS… and the client puts two condoms on”(40-year-old, HIV-positive, three years of sex work).
Charging more for unprotected sex: In our discussions, the FSWs reported that they have different prices for different types of sex, sex with and without condoms. Sometimes clients offer how much they are willing to pay for non-condom use.
“…the client will offer you 10,000/Ugandan Shillings for not using a condom, wouldn´t you take it? You do not have a choice; you will succumb to the client´s demands…”(34-year-old, HIV-positive, eight years of sex work).
“I am reluctant to use a condom to certain clients who offer me 20,000/Ugandan Shillings or more to have sex without condoms”(40-year-old, HIV-positive, 16 years’ experience of sex work).
Refusing unprotected sex: participants reported that in some instances, they refuse unprotected sex with clients even if they offer them more money and are not concerned about losing the money or clients to another sex worker because they are unwilling to put themselves at risk of contracting HIV/STIs.
“When I first started sex work…, I would agree if a client refuses to use a condom…, but now, if a client does not want to use a condom, I ask him to take his money and leave…”(27- year-old, HIV-positive, six years of sex work).
“…the client will tell you that his penis cannot get an erection if they put on a condom… I tell them to take their money and leave”(30-year-old, HIV-positive, five years of sex work).
Sub-Theme 2: Challenges in Promoting Safe Sex Practices
Low power in relationships: FSWs still have lower power in their relationship, mainly related to condom use. Condoms are still taboo, and they have less power to negotiate condom use with their clients. Only a few sex workers consistently used condoms for two weeks, as reported by the FSWs. The main reason they did not use condoms is that they believe healthy-looking clients cannot spread STIs and have already taken other preventive measures, like antibiotics before sex.
“I am a sex worker fine… but being a woman, sometimes I feel initiating condom use is a taboo since our society says so; therefore this makes me have less power in negotiating condom use in my work”(30-year-old, HIV-negative, two years of sex work).
“…most clients would not want to use condoms, therefore I let them have unprotected sex with me because I always take medicines before I engage in my work; this medicine help in disrupting the sperm from entering my cervix and also in preventing me from contracting STIs, although it does not protect me from HIV”(34-year-old, HIV-positive, 15 years of sex work).
Economic gain is the main contributing factor to FSWs’ risky sexual behaviour. Low economic status and higher living costs encourage FSWs to accept clients’ offers for unprotected sex. The participants noted two main types of logic for not using condoms: economic reasons and romantic relationships. Feeling secure and trusting their clients are the underlying reason these FSWs did not use condoms.
“Financially, I am very unstable in that I cannot survive without selling sex, and I cannot afford to refuse to sell sex to customers who would like to have condomless sex because of the minimal possibility of getting the next customer”(40-year-old, HIV-positive, three years of sex work).
“sex is sweeter without Condoms. I already have regular clients whom I feel intimate with and trust; whenever I am with them, I feel so secure, so there is no need to have sex with a condom”(30-year-old, HIV-negative, two years of sex work).
Lack of control over clients’ behaviour; The sex workers reported that they do not have control over their clients’ behaviours because the sex act is sometimes performed in the bushes, in the clients’ car, at the client’s place, and sometimes in places rented by clients, and or even in the sex workers’ rooms. Being alone with the client in the room, most FSWs are vulnerable and experience all forms of abuse from their clients.
“In most cases, I do not control my client’s behaviour and where he wants to perform sex. However, clients vary in that others would have to take you to the bush, at their home or have sex with you in their cars because of reasons best known to them, which exposes me to any form of treatment like having condomless sex against my will, rape, being beaten or refusing to pay me after sex”(33 years old, HIV-positive, five years’ experience in sex work).
Facing violence and lack of control over where to have sex: The FSWs reported that the street-based environment, which is unregulated, exposed them to risks of being attacked by their clients and a lack of access to healthy infrastructure for supporting safe sex, such as ablutions. General reports among the FSW were that they experienced violence from their clients due to the street-based nature of their work. Although during the interviews we asked the female sex workers about the challenges that they faced in promoting safe sex in their daily work, the FSW reported that the street-based environment, which is unregulated, exposed them to risks of being attacked by their clients and to lack access to healthy infrastructure for supporting safe sex, such as ablutions.
“Sometimes you get a client who is kind to you and take you to the bushes; when you get there, he points a gun at you and tells you that you are going to have sex without the condom and you are going to give in to his demands”(23-year-old, HIV-positive, six years of sex work).
“A client will book you for the whole night…, and take you to his place. He then points a gun at you and forces you to have condomless sex… you end up saying it is better to have condomless sex instead of dying…”(30-year-old, HIV-positive, two years of sex work).
High levels of alcohol consumption: The study also revealed that 80% of FSWs had high levels of alcohol consumption. Consuming alcohol at a high level affects sexual behaviours, including sex without condoms. Study results found a significant relationship between alcohol consumption and STI-risk sexual behaviour among FSWs; it can cause a decrease in the desire to use condoms, a lower ability to remember to use them and a decrease in the capability to use them properly.
“For my case, alcohol use before and during sexual intercourse damages my behavioural abilities needed to negotiate condom use… because I would feel like everything is normal”(23-year-old, HIV-positive, six years of sex work).
“When I consume alcohol, it decreases my desire to use condoms, lowers my ability to remember how to use them and decreases my capability to use them properly. In addition, when I have sexual intercourse under the influence of alcohol, my self-control of sexual behaviours is reduced, leading to impulsive and risky sexual behaviour”(34-year-old, HIV-positive, 15 years of sex work).
Using unsafe tactics to prevent transmission of STIs: FSWs used various materials which are inserted inside the vagina before unprotected sex (a sponge or cotton wool or a stocking) as a strategy to prevent the semen from coming into contact with the cervix, which is perceived to be protective against STIs.
“On the streets, there are clients who refuse to use condoms. The female condom has a sponge inside. Most of us insert the sponge in the vagina. Then, when the client asks to urinate (before sex), you insert the sponge, and he gives you the ten thousand shillings he promised. After he finishes, you remove the sponge”(33 years old, HIV-positive, five years’ experience in sex work).
“…clients have a choice. If a client does not want to use a condom, I insert a sponge”(30 years old, HIV-positive, four years’ experience in sex work).
Hiding blood during menstruation to avoid loss of workdays: Female sex workers reported that they have to work to earn a living, even during their menstruation. They use objects like a sponge, stockings, cotton wool or pills, which they insert into their vaginas to block the menstrual fluids from coming out, and they sell sex as usual.
“If it is towards month end and I have to have money to pay rent and buy food, and I am menstruating, I take these new female condoms which have a sponge. I take out that round sponge and put it inside my vagina, then after three clients, I take it out, wash it, then put it back”(40 years old, HIV-positive, 16 years’ experience of sex work).
“For the client not to notice that I am menstruating, I usually use strawberry-flavoured condoms because the condom is also red”(34 years old, HIV-positive, 15 years’ experience of sex work).
“At first, when I realised that I was menstruating, I took Aspirin and inserted it inside my vagina and within thirty minutes, the blood stopped”(41 years old, HIV-positive, 18 years’ experience of sex work).
3.2.2. Theme 2: Screening for STI
Sub-Theme 1: Facilitators for Regular Screening
Social influences
Some participants reported testing for STIs and HIV due to the influence of a distant partner or boyfriend who lived in a different part of the country. The partners were usually not aware of their participation in sex work. Their testing behaviour was motivated by the request of the partner, for fear of being infected.
“My boyfriend is not aware I do this job… we usually meet once every four months, and normally he insists we must first test for STIs”(23-year-old, HIV-positive, six years of sex work).
Sometimes the demand for unprotected sex by male clients influenced frequent HIV testing behaviour; this occurred among younger participants with strong positive body-image perceptions or marriage intentions.
“I test for HIV whenever a client requests sex without a condom. For example, I am gorgeous, and many clients want to have sex with me “live” (without a condom), but I only agree if the man agrees and tests negative”(30-year-old, HIV negative, two years of sex work).
Emotional relief
A participant reported frequently testing for HIV to avoid anxiety. The fear of contracting HIV after condomless sex caused stress, experiences of anxiety, distress, and uneasiness. Condomless sex generates more earnings than sex with a condom, and FSWs sometimes face a dilemma between needing income and risking HIV infection from unprotected sex. Periodic testing was associated with emotional relief and happiness, mainly if one tested HIV-negative. The desire for psychological and emotional well-being motivated periodic testing for HIV. However, no psychological concerns were reported for STIs.
“I sometimes try to insist on condom use, but clients offer more money for unprotected sex… and sometimes I have nothing to eat or feed my child…so I test for HIV almost every two months to feel relieved”(30 years old, HIV-negative, two years’ experience of sex work).
Similarly, dual STIs and HIV testing were reported among participants with childbearing and marriage intentions. STIs like syphilis and candida were believed to cause infertility. The fear of being unable to bear children promoted syphilis testing.
“In this job, one can easily acquire infections that can affect their private parts (vagina) and even the uterus… for me, at some point, I want to quit this job, get married and have children in future so I normally go to test for STIs and HIV every two months”(30 years old, HIV negative, two years’ experience of sex work).
Periodic testing was associated with emotional relief and happiness, mainly if one tested HIV-negative. The desire for psychological and emotional well-being motivated periodic testing for HIV.
Habitual testing and self-efficacy
HIV testing was described as habitual by most participants. Receipt of previous STI-and HIV-negative test results gave them the courage to test again. In addition, some reported maintaining a diary of testing dates as a reminder.
“I cannot say no to any man who comes with money. I have made it a habit to test for HIV every three months… I keep a diary where I record dates; all I would do is use PEP”(30 years old, HIV-negative, two years’ experience of sex work).
Prior testing for STIs resulted in empowerment and self-efficacy, which was frequently described as a facilitator for engaging in regular HIV testing.
“My parents died of HIV, and so my relatives thought I was HIV positive, but since I tested negative, I have developed the courage to always test for HIV every month and other STIs as well”(30 years old, HIV-negative, two years’ experience of sex work).
We observed that some participants tested for STIs because it was offered at an antenatal clinic.
“I had learnt to test for STIs every three months because when I was pregnant, it was a must to be tested for HIV and STIs”(30-year-old, HIV-positive, five years of sex work).
Availability of many testing clinics for STIs
HIV testing services were reported to be easily accessible in all cities. In addition, all participants cited several testing facilities ranging from free government clinics, NGO clinics, private clinics, and occasionally community-based testing outreaches.
“For me, it is easy to test for STI every three months because there are many testing centres. I used to test from the main hospital, but when healthcare workers know your business (sex work), they take longer to serve you… now I go to the health centre”(41-year-old, HIV-positive, 18 years of sex work).
These facilities provided choices regarding availability, acceptability, convenience, and affordability. The commonly preferred testing sites were FSW-friendly clinics, public health facilities, and NGO-run clinics. Private clinics and community-based outreach campaigns were the least preferred.
“I used to test from a private clinic, but I worried a lot while waiting for results… at the health centre, services are free. Healthcare workers prepare you before (pre-test counselling) and after testing… you get much information about STIs”(30-year-old, secondary school leaver, HIV-positive, five years’ experience of sex work).
Reasons for these preferences included providing a range of STI testing services, availability of testing kits and antibiotics, and approachable and kind HCWs for specific FSW clinics. Public health clinics offered free testing services, health education and pre-test counselling. Private clinics were preferred for being nearby or because they were trusted to provide accurate test results. Outreach campaigns were said to be convenient.
“I do sometimes test for HIV and STIs at the nearby health centre, especially when I want to get PEP… but normally I test from private clinics because they are near or when healthcare workers come and test us from here”(30 years old, HIV-negative, two years’ experience of sex work).
Sub-Theme 2: Barriers to STI Screening
Participants outlined a range of individual and health-system factors that influenced the frequency of STI and HIV testing. Noteworthy personal barriers encompassed a diminished sense of seriousness regarding STIs, misapprehensions about these infections, and the presence of internalized stigmatization related to STIs. On the service delivery front, barriers included the conduct of healthcare providers, shortages of syphilis testing supplies, the financial burden associated with STI testing, instances of stigma and bias, inconvenient clinic hours, and a perceived lack of empathy from HIV service providers, Figure 1.
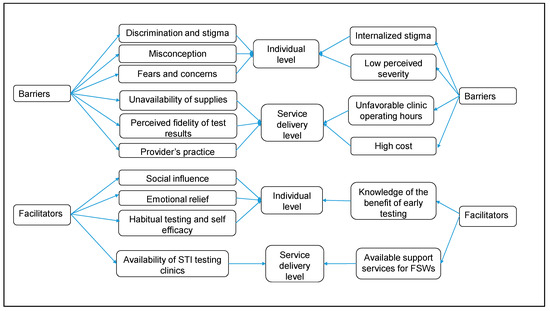
Figure 1.
Barriers and facilitators to sexually transmitted infection screening among female sex workers in Gulu City, Uganda.
Unavailability of supplies and high cost
Some participants cited being discouraged from seeking STI screening due to frequent stockouts of testing kits and medicines. They observed that, unlike HIV, testing kits for syphilis and antibiotics were seldom available at public health facilities.
“Unless you are pregnant, it is not easy to be tested for STIs in public facilities because testing kits and medicines are not available”(30 years old, HIV-negative, two years’ experience of sex work).
STI testing was reported to be more expensive than HIV testing at private clinics. However, the low cost of HIV testing was attributed to the availability of several testing clinics.
“At least for HIV, you can find many cheap testing places; testing for other STIs is very expensive in private clinics”(30-year-old, secondary school leaver, HIV-positive, five years of sex work).
Discrimination and stigma
Discrimination experiences were reported as a barrier to STI testing by all participants. However, this mainly occurred at public health facilities, unlike sex-worker-friendly clinics.
“I used to test for HIV from the main hospital, but once HCW realised you are a sex worker, no one wants to attend to you, or you will be the last to be seen. However, there are many testing centres in Gulu City… So I now test from Reproductive Health Uganda (RHU)”(41 years old, HIV-positive, 18 years’ experience of sex work).
Unfavourable operating clinic hours
Some participants reported unfavourable clinic working hours as a barrier to STI testing, mainly in government-aided facilities.
“Like a week ago, I went to one of the health centres not far from here. I reached there at 3:00 pm to take an STI test… but was told to come the following day because the facility had closed…I was very demoralised”(40 years old, HIV-positive, 16 years’ experience of sex work).
Fears and concerns
Routine STI and HIV testing faced significant hindrances, primarily due to apprehensions and concerns surrounding the potential consequences of these infections on an individual's health, occupation, familial responsibilities, and future prospects. Participants outlined a fear of unexpected illness, the inability to continue working, and fulfilling parental obligations as driving forces behind their consistent testing habits. They conveyed a heightened perception of vulnerability to contracting HIV and other STIs, believing that maintaining physical attractiveness and robustness were vital for surviving in the sex work industry. Consequently, they emphasized undergoing HIV and syphilis testing, viewing good physical health as crucial for attracting and satisfying clients. The motivation for regular testing also lay in the possibility of accessing antiretroviral therapy (ART) and STI treatment in the event of a positive diagnosis. Additionally, testing was mandatory before obtaining a prescription for post-exposure prophylaxis (PEP).
“I fear if I suddenly become sick and stop working… I am in this job for my children. No one will take care of them if I allow myself to become sick. Also, you must test for STIs and other diseases in this job. If found positive, you immediately start medicine; otherwise, you will not be able to satisfy customers and continue working… However, I rarely go for it”(41 years old, HIV-positive, 18 years’ experience in sex work).
Perceived fidelity of test results
Certain participants expressed scepticism regarding the reliability of their negative STI- and HIV-test outcomes, prompting them to seek additional tests from different clinics to verify these results. Several FSWs shared instances where they had unprotected intercourse or had clients who were confirmed to be HIV-positive, yet they consistently tested negative for HIV. Furthermore, doubts surfaced concerning the accuracy of determining their HIV status based on a single drop of blood obtained through a finger prick. In situations where testing was conducted alongside a regular client or partner, some FSWs pursued repeated tests due to concerns that their partner might have influenced clinic personnel to manipulate the test outcomes.
“I do not think a drop of blood from a finger gives correct HIV results… in outreaches, HCW have tested people we know have clients on antiretroviral drugs negative… I have messed up a lot, but they continue to test me negative… I keep testing because I do not believe [my test results]”(34 years old, HIV-positive, 15 years’ experience of sex work).
Sub-Theme 3: Confidential and Non-Judgmental STI Screening Services
Providers’ practice
The practice of syndromic STI management (treating without prior testing) and the presence of healthcare providers with disrespectful and judgmental attitudes were identified as factors restricting the adoption of regular STI testing. This was illustrated by instances where participants were given antibiotics for STIs without undergoing any testing, even when they specifically asked for testing. Moreover, a noticeable disparity emerged: unlike HIV testing, healthcare workers (HCWs) seldom prioritized STI testing in public health facilities unless the individual was pregnant.
“Health workers never emphasise screening for other STIs as they do for HIV… I test for STIs when I visit a private hospital because, in other hospitals, you are asked for signs and symptoms… without testing… after that, they write for you medicines”(34-year-old, HIV-positive, 15 years of sex work).
Among the younger FSWs, there were instances where seeking an STI test proved to be challenging. Unlike HIV testing, requesting an STI test often led to probing inquiries from healthcare providers. Participants were subjected to questions such as, ‘Who told you that you might have an STI?’ or ‘What actions have you taken to contract an STI?’ and ‘What specific symptoms indicate you have an STI?’ Additionally, questions like ‘Do you consider yourself a medical professional in this consultation?’ were posed. These questions were perceived as uncomfortable, lacking in respect, and laden with judgment.
“I felt very small and embarrassed by the health care provider when I requested to be tested for syphilis. It is not easy to ask for a syphilis test. Two months ago, I requested to be tested for syphilis at the hospital, but the doctor looked at me and asked me who told me I had syphilis, what I had done, and which signs… I felt very small, ashamed and insecure”(23 years old, HIV-positive, six years’ experience of sex work).
In contrast, the uncaring attitudes of HCWs were reported to limit the uptake of regular HIV testing. Most participants reported that HCWs were unfriendly or uncaring, especially at public facilities. In addition, HCWs were perceived to be non-responsive and unfriendly to FSWs, which led to long waiting times.
“I went to take an HIV test at a hospital, but the care was not good… doctors were too busy to attend to us that I spend the whole day in the hospital… now I test whenever I go to health centre III”(33 years old, HIV-positive, five years’ experience in sex work).
Sub-Theme 4: Stigmatisation or Discrimination from Healthcare Providers
Low perceived severity, misconceptions, and internalised stigma
In contrast to HIV, many FSWs viewed other STIs as comparatively less-severe health risks. They indicated that a common belief among FSWs was to undergo syphilis testing only once symptoms of the disease had manifested. This perception acted as an obstacle to regular testing practices.
“[other] STIs are not such a big issue as HIV. One can live with syphilis… it is not easy to go and test when you have no signs. I test because when I go to our clinic… I am told to test for syphilis, gonorrhoea, Candida or other diseases”(33-year-old, HIV-positive, five years of sex work).
Descriptions of internalised stigma as a barrier to STI testing were amplified by fears of being seen at clinics or peers spreading rumours about one’s perceived status. In addition, rumour-mongering was associated with the loss of customers and income common among FSWs.
“I sometimes fear finding people I know at the clinic; I do not want them to know I am doing this job. Also, you are given a medical form if you test for STIs… your friends may get to know that you have STIs and other diseases and tell other people, which affects your business…”(41 years old, HIV-positive, 18 years of sex work).
3.2.3. Theme 3: Support and Intervention
Sub-Theme 1: Available Support or Services for FSWs in Gulu City
The availability of clinics tailored to FSWs that provide combined STI and HIV testing, along with outreach programs coordinated by RHU, TASO, and Mariestopes, played a significant role. Integrated STI/HIV testing was primarily made possible through specialized clinics operated by NGOs that focus on FSWs. On a personal level, the decision to undergo testing was largely influenced by various fears and concerns. These included heightened apprehension about contracting HIV, worries about fertility issues, the perception that having STIs could hinder the ability to satisfy or attract clients, the sudden onset of illness, the potential loss of work leading to an inability to support dependents, and psychological distress.
Sub-Theme 2: Support for or Interventions on STI Prevention and Treatment
Respondents mentioned that the presence of dedicated FSW-friendly clinics within Marie Stopes in Uganda supported their regular STI- and HIV- testing practices. They highlighted several factors that made them favour these clinics, such as comprehensive STI testing, easy access to testing equipment and medications, and the compassionate and approachable nature of healthcare staff, among other reasons.
“…I went to a government facility, but the care was not good… nowadays when I want to test [for STIs], I visit Mariestopes because I can explain my problems to doctors… get counselling and be tested for all STIs… they care about us. So I find it convenient”(23-year-old, HIV-positive, six years of sex work).
Some NGO clinics provided integrated services, including STI- and hepatitis-B-virus testing at a low cost, promoting syphilis and HIV testing.
“I usually test at a non-governmental organisation clinic… because even with small money, I am tested for STIs, including HIV and hepatitis B virus…”(30-year-old, HIV-negative, two years of sex work).
4. Discussion
STIs among FSWs are of significant public health concern, with research showing a pronounced prevalence among this population. In this study, we aimed to explore the practices of FSWs in Gulu City, Uganda, regarding screening for STIs. We found that 66.7% of FSWs received STI screening in the last three months, with the majority (90.8%) relying on symptom-based screening, while 8.1% underwent monthly screening, and 1.2% had never been screened. In addition, the commonly reported STIs among the FSWs included vulvovaginal candidiasis (55.3%) and syphilis (32.9%), whereas fewer participants reported Chlamydia and gonorrhoea (6.6% and 5.3%, respectively).
These findings align with results from studies conducted in Iran, China and Uganda where only 57.8%, 68.3% and 56% of FSWs had tested for HIV [15,16,17]. Furthermore, in Canada, approximately 57.9% of FSWs tested for HIV and /or STIs with 45.5% and 44.9% of FSWs reported HIV and STI testing respectively and only 32.6% reported screening for both [18]. Another study conducted in Netherlands revealed that about 67.1% of FSWs tested for STIs [19]. Significantly higher prevalence of STI screening was reported in Switzerland, estimated at 72%, and in England, where 80% of individuals reported being tested for Chlamydia, 75% for gonorrhoea, 93% for HIV, and 79% for syphilis [20,21].
Our study further highlights the strategies used by FSWs in Uganda in negotiation for condom use, including requesting and enforcing condom use, using “health-risk information” to threaten or motivate clients to use condoms, charging more for unprotected sex, and refusing unprotected sex. While these strategies have often been effective for FSWs, they continue to encounter several challenges in maintaining safe-sex practices. These challenges include limited power within relationships, financial incentives for risky behaviours, insufficient control over clients’ actions, exposure to violence, lack of choice in selecting locations for sex work, elevated alcohol consumption, utilization of unsafe methods to prevent STI transmission, and concealing menstrual blood to prevent workday losses. Consequently, these challenges lead to FSWs resorting to unsafe sexual practices and an increased risk of STI transmission [4,22].
In our study, several facilitators contributed to the screening of HIV and other STIs among FSWs, including social influences, emotional relief, habitual testing, self-efficacy, and the availability of numerous testing clinics for STIs. Similarly, another Ugandan study revealed that motivations to stay healthy, marry, and have children, understanding treatment benefits, and partner influence were facilitators at an individual level, while sex-worker clinics and testing-facility availability were facilitators to testing for HIV and syphilis [23]. Conversely, our participants reported several barriers to STI screening, including unavailability of supplies and high costs, discrimination and stigma, unfavourable operating hours, fears and concerns regarding STI testing, and perceived fidelity of test results. Previous studies have shown similar barriers to STI screening among this population, with stigma and misconceptions being the most common [23,24]. Other barriers include cost concerns at an individual level, low perceived severity of syphilis infection and poor and unfriendly provider attitudes, facility shortages, and unfriendly environments within the health system; all of these were reported [23,24]. Moreover, peer education and reminders in the form of text messages have been shown to improve HIV and syphilis screening among FSWs by nearly 50% in three months [24]. Therefore, such interventions hold promise in enhancing the uptake of STI screening services in this population.
The strength of our study lies in the implementation of a mixed-methods approach, which enabled us to comprehensively explore various facets including sexual behaviour, knowledge, attitudes towards STIs, barriers to STI screening, and support and interventions for STI prevention and treatment. Due to the small sample size, our findings are not generalizable to the Ugandan population. In addition, the participants included in the qualitative interviews had different characteristics from those included in the quantitative arm, making triangulation of findings impossible. Furthermore, it is important to acknowledge the potential presence of recall bias among participants, which could introduce inconsistencies in the data and affect the reliability of the findings. However, efforts were made to mitigate this bias through careful question design and participant engagement.
5. Conclusions
Our findings underscore the pronounced vulnerabilities faced by FSWs in Gulu City, Uganda, with regard to STIs. While positive trends in high HIV awareness and consistent condom usage were observed, the persistence of challenges related to STI screening, safe-sex negotiation, and access to prevention and treatment services remains striking. Targeted interventions must be devised to bolster accessibility to STI screening, empower FSWs with effective negotiation skills, and provide comprehensive support for prevention and treatment, thereby fostering enhanced sexual health and well-being within this marginalized demographic. Our study additionally emphasizes the need for urgent efforts to overcome the low prevalence of STI screening among FSWs, necessitating the provision of easily accessible, affordable, and stigma-free STI testing and care services. Concurrently, sustained health education initiatives and dispelling misconceptions surrounding STI screening are crucial for fostering greater acceptance of these services, thereby mitigating the prevalence and transmission risk of STIs in Uganda.
Author Contributions
Conceptualization, F.B., W.K., P.F.P., D.M. and S.O.; methodology, F.B., W.K., P.F.P., F.G.L., J.O., G.M. and S.O.; software, F.B., W.K., P.F.P. and J.O.; validation, F.B., W.K., P.F.P., J.O. and S.O.; formal analysis, F.B., W.K., F.G.L., J.O. and S.O.; investigation, F.B., W.K., F.G.L., G.M. and S.O.; resources, F.B., W.K. and P.F.P.; data curation, F.B., W.K. and S.O.; writing—original draft, F.B., W.K., P.F.P., F.G.L., J.O., F.O.K., G.M., C.S.L.L., S.A., A.N., D.M. and S.O.; writing—review and editing, F.B., W.K., P.F.P., F.G.L., J.O., F.O.K., G.M., C.S.L.L., S.A., A.N., D.M. and S.O.; visualization, F.B.; supervision, F.B., D.M. and S.O.; project administration, P.F.P., F.O.K., G.M., D.M. and S.O.; funding acquisition, F.B. and P.F.P. All authors made substantial contributions to the design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported through a seed grant from the Centre for International Reproductive Health Training (CIRHT) at The University of Michigan, the United States of America. The funder had no role in the design and conduction of this study.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of Gulu University (protocol code GUREC-2022-414 and approved on 21 February 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We would like to acknowledge the study participants.
Conflicts of Interest
The authors declare no competing interest.
References
- Shannon, K.; Strathdee, S.A.; Goldenberg, S.M.; Duff, P.; Mwangi, P.; Rusakova, M.; Reza-Paul, S.; Lau, J.; Deering, K.; Pickles, M.R.; et al. Global epidemiology of HIV among female sex workers: Influence of structural determinants. Lancet 2015, 385, 55–71. [Google Scholar] [CrossRef]
- UNAIDS. Geneva: Joint United Nations Programme on HIV/AIDS 2022. Available online: https://www.unaids.org/sites/default/files/media_asset/data-book-2022_en.pdf (accessed on 3 April 2023).
- World Health Organization. Sexually Transmitted Infections (STIs); WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Llangarí-Arizo, L.M.; Sadiq, S.T.; Márquez, C.; Cooper, P.; Furegato, M.; Zhou, L.; Aranha, L.; Mateo, M.M.; Romero-Sandoval, N. Sexually transmitted infections and factors associated with risky sexual practices among female sex workers: A cross sectional study in a large Andean city. PLoS ONE 2021, 16, e0250117. [Google Scholar] [CrossRef] [PubMed]
- Kiyingi, J.; Nabunya, P.; Bahar, O.S.; Mayo-Wilson, L.J.; Tozan, Y.; Nabayinda, J.; Namuwonge, F.; Nsubuga, E.; Kizito, S.; Nattabi, J.; et al. Prevalence and predictors of HIV and sexually transmitted infections among vulnerable women engaged in sex work: Findings from the Kyaterekera Project in Southern Uganda. PLoS ONE 2022, 17, e0273238. [Google Scholar] [CrossRef] [PubMed]
- Muhindo, R.; Castelnuovo, B.; Mujugira, A.; Parkes-Ratanshi, R.; Sewankambo, N.K.; Kiguli, J.; Tumwesigye, N.M.; Nakku-Joloba, E. Psychosocial correlates of regular syphilis and HIV screening practices among female sex workers in Uganda: A cross-sectional survey. AIDS Res. Ther. 2019, 16, 28. [Google Scholar] [CrossRef] [PubMed]
- Muhindo, R.; Mujugira, A.; Castelnuovo, B.; Sewankambo, N.K.; Parkes-Ratanshi, R.; Kiguli, J.; Tumwesigye, N.M.; Nakku-Joloba, E. Text message reminders and peer education increase HIV and Syphilis testing among female sex workers: A pilot quasi-experimental study in Uganda. BMC Health Serv. Res. 2021, 21, 436. [Google Scholar] [CrossRef] [PubMed]
- Muhindo, R.; Mujugira, A.; Castelnuovo, B.; Sewankambo, N.K.; Parkes-Ratanshi, R.; Kiguli, J.; Tumwesigye, N.M.; Nakku-Joloba, E. HIV and syphilis testing behaviors among heterosexual male and female sex workers in Uganda. AIDS Res. Ther. 2020, 17, 48. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Health Sector Strategies on, Respectively, HIV, Viral Hepatitis and Sexually Transmitted Infections for the Period 2022–2030; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Logie, C.H.; Okumu, M.; Musoke, D.K.; Hakiza, R.; Mwima, S.; Kyambadde, P.; Abela, H.; Gittings, L.; Musinguzi, J.; Mbuagbaw, L.; et al. Intersecting stigma and HIV testing practices among urban refugee adolescents and youth in Kampala, Uganda: Qualitative findings. J. Int. AIDS Soc. 2021, 24, e25674. [Google Scholar] [CrossRef] [PubMed]
- Crowley, J.S.; Geller, A.B.; Vermund, S.H.; National Academies of Sciences, Engineering, and Medicine. Biomedical Tools for STI Prevention and Management. In Sexually Transmitted Infections: Adopting a Sexual Health Paradigm; National Academies Press (US): Washington, DC, USA, 2021. [Google Scholar]
- Crowley, J.S.; Geller, A.B.; Vermund, S.H.; National Academies of Sciences, Engineering, and Medicine. STI Screening and Treatment Guidelines Issued by Health Professional Societies. In Sexually Transmitted Infections: Adopting a Sexual Health Paradigm; National Academies Press (US): Washington, DC, USA, 2021. [Google Scholar]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. 1), S31–S34. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, S.; Khezri, M.; Roshanfekr, P.; Karimi, S.E.; Vameghi, M.; Ali, D.; Ahounbar, E.; Noroozi, M.; Shokoohi, M. HIV testing and its associated factors among street-based female sex workers in Iran: Results of a national rapid assessment and response survey. Subst. Abus. Treat. Prev. Policy 2021, 16, 43. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Luo, J.; Chen, Y.; Chen, L.; Hu, H.; Qiu, T.; Liu, X.; Xu, X.; Chen, Y.; Zhang, Z.; et al. Prevalence of syphilis and chlamydia trachomatis infection among female sex workers in Jiangsu, China: Results from a multicenter cross-sectional and venue-based study. Front. Public Health 2022, 10, 1018724. [Google Scholar] [CrossRef] [PubMed]
- Atuhaire, L.; Shumba, C.S.; Mapahla, L.; Maposa, I.; Nyasulu, P.S. Factors associated with adherence to HIV testing guidelines among HIV-negative female sex workers in Kampala, Uganda. IJID Reg. 2022, 4, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, S.M.; Pearson, J.; Moreheart, S.; Nazaroff, H.; Krüsi, A.; Braschel, M.; Bingham, B.; Shannon, K. Prevalence and structural correlates of HIV and STI testing among a community-based cohort of women sex workers in Vancouver Canada. PLoS ONE 2023, 18, e0283729. [Google Scholar] [CrossRef] [PubMed]
- Kampman, C.J.G.; Peters, C.M.M.; Koedijk, F.D.H.; Berkenbosch, T.S.; Hautvast, J.L.A.; Hoebe, C.J.P.A. Sexual risk and STI testing behaviour among Dutch female and male self-employed sex workers; a cross-sectional study using an Internet based survey. BMC Public Health 2022, 22, 1155. [Google Scholar] [CrossRef]
- Vu, F.; Cavassini, M.; D’Acremont, V.; Greub, G.; Jaton, K.; Masserey, E.; Pongelli, S.; Bouche, L.; Ngarambe, C.; Bize, R.; et al. Epidemiology of sexually transmitted infections among female sex workers in Switzerland: A local, exploratory, cross-sectional study. Swiss Med. Wkly. 2020, 150, w20357. [Google Scholar] [CrossRef] [PubMed]
- Esler, D.; Catriona, O.; Tony, M. Sexual health care for sex workers. Aust. J. Gen. Pract. 2008, 37, 590. [Google Scholar]
- Jung, M. Risk factors of sexually transmitted infections among female sex workers in Republic of Korea. Infect. Dis. Poverty 2019, 8, 6. [Google Scholar] [CrossRef] [PubMed]
- Muhindo, R.; Mujugira, A.; Castelnuovo, B.; Sewankambo, N.K.; Parkes-Ratanshi, R.; Tumwesigye, N.M.; Nakku-Joloba, E.; Kiguli, J. “I felt very small and embarrassed by the health care provider when I requested to be tested for syphilis”: Barriers and facilitators of regular syphilis and HIV testing among female sex workers in Uganda. BMC Public Health 2021, 21, 1982. [Google Scholar] [CrossRef] [PubMed]
- Muhindo, R. Regular STI and HIV Screening Intentions and Practices among Sex Workers in Uganda: The Effect of Text Message Reminders and Peer Education. Ph.D. Thesis, Makerere University, Kampala, Uganda, 2022. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).