Prevalence of Comorbidities and Associated Factors among HIV Patients Attending Antiretroviral Clinics in the Tamale Metropolis, Ghana
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Socio-Demographic Characteristics
3.2. Prevalence of Comorbidities
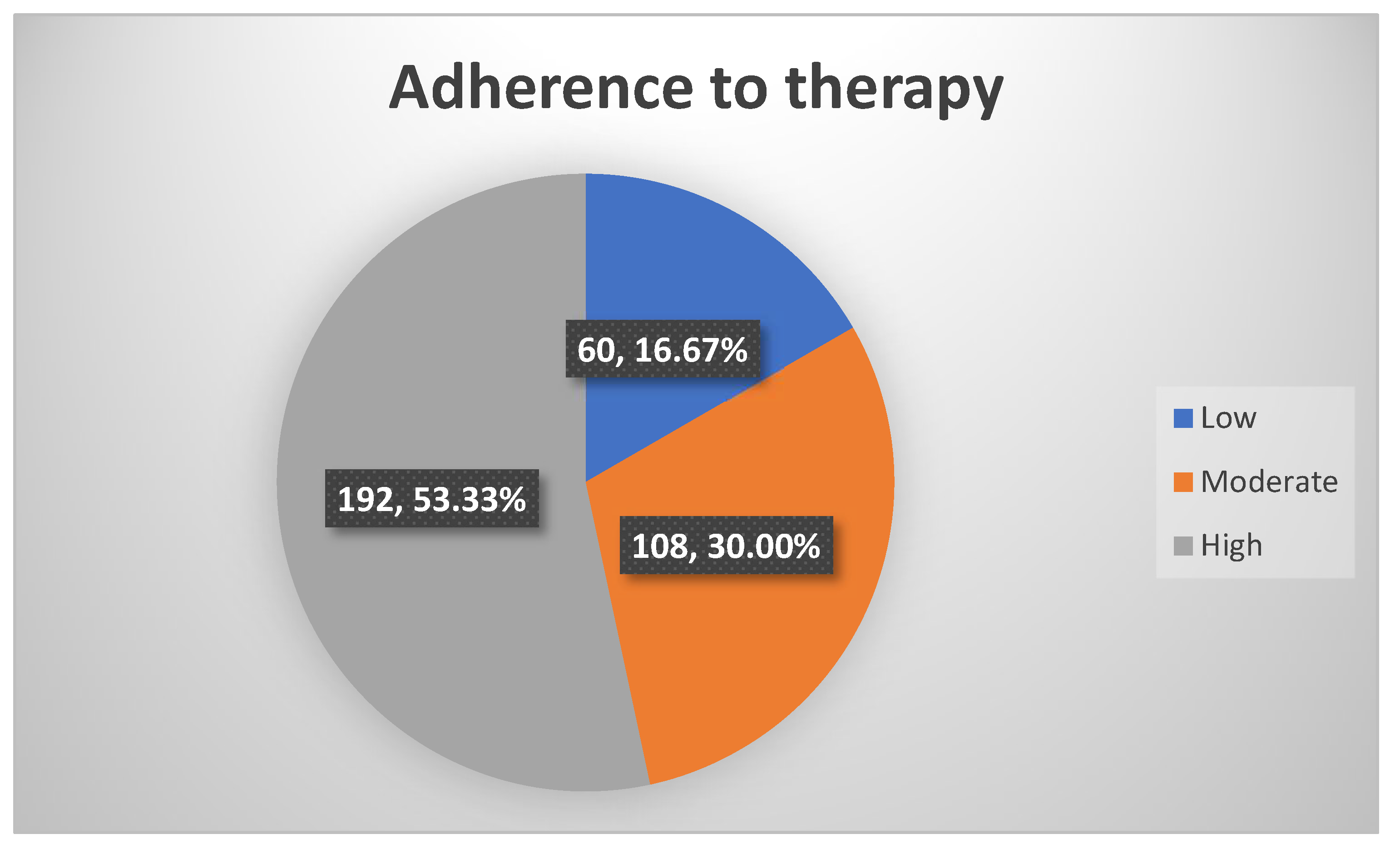
3.3. Adherence to Antiretroviral Therapy
3.4. Quality of Life
3.5. Factors Associated with the Occurrence of Comorbidities among HIV Patients
4. Discussion
4.1. Prevalence of Comorbidities
4.2. Adherence to Antiretroviral Therapy
4.3. Quality of Life
4.4. Prevalence of Comorbidities and Associated Factors
5. Conclusions
- This study confirmed and is consistent with our belief that comorbidities are prevalent in PLWH. This is in line with the research objective. Although from the literature, comorbidities were expected to be prevalent in this group of persons, 30.3% was rather thought to be on the high side for persons who were not actively (that is, taking samples or conducting clinical examinations or measurements on the spot) and routinely being checked for the presence of comorbidities at the ART clinic. This means comorbidities are prevalent amongst PLWH in the Tamale Metropolis. Thus, with active and routine checking, the numbers may be increased, and give individuals the opportunity to seek and get treatment early. Hepatitis B as the most prevalent comorbidity did not come as a surprise because that is what has been widely studied and seen.
- The adherence to ART being high in more than half of the population is in line with the research objective and expected outcomes. This is because these are people who routinely visit the ART clinic and are expected to be concerned about their health and well-being. For such persons, we expect them to be adherent to their medications, and the QoL was excellent for the majority of the respondents in the physical, psychological, independence, relationship, and spiritual domains. The overall QoL and health are good, which translates to an average or moderate score for the majority of the respondents. This is expected because, with adherence and routine check-ups, we assume the QoL of persons should be good, if not excellent.
- The presence of comorbidities seen may have been influenced by marital status, the presence or absence of HIV symptoms, adherence to antiretroviral medications, and the quality of life in the physical, psychological and independence domains. The overall QoL and general health status was one of the justifications for this study. That is, to look at the interplay between these factors. These fulfilled our research objectives and are findings that are consistent with our thoughts at the onset of this study. This can help persons living with the disease to adopt lifestyles healthy enough to help them live close to normal healthy, quality lives. The best form of treatment is prevention. These findings will help us champion the course of preventing comorbidities in these group of persons now that our findings allude to it.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Magodoro, I.M.; Esterhuizen, T.M.; Chivese, T. A cross-sectional, facility based study of comorbid non-communicable diseases among adults living with HIV infection in Zimbabwe. BMC Res. Notes 2016, 9, 379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trickey, A.; May, M.T.; Vehreschild, J.-J.; Obel, N.; Gill, M.J.; Crane, H.M.; Boesecke, C.; Patterson, S.; Grabar, S.; Cazanave, C. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: A collaborative analysis of cohort studies. Lancet HIV 2017, 4, e349–e356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maciel, R.A.; Klück, H.M.; Durand, M.; Sprinz, E. Comorbidity is more common and occurs earlier in persons living with HIV than in HIV-uninfected matched controls, aged 50 years and older: A cross-sectional study. Int. J. Infect. Dis. 2018, 70, 30–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kasher, M.; Freidin, M.B.; Williams, F.M.; Cherny, S.S.; Malkin, I.; Livshits, G. Shared genetic architecture between rheumatoid arthritis and varying osteoporotic phenotypes. J. Bone Miner. Res. 2022, 37, 440–453. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, P.; Gruell, H.; Nogueira, L.; Pai, J.A.; Butler, A.L.; Millard, K.; Lehmann, C.; Suárez, I.; Oliveira, T.Y.; Lorenzi, J.C. Combination therapy with anti-HIV-1 antibodies maintains viral suppression. Nature 2018, 561, 479–484. [Google Scholar] [CrossRef]
- Biraguma, J.; Mutimura, E.; Frantz, J.M. Health-related quality of life and associated factors in adults living with HIV in Rwanda. SAHARA J. Soc. Asp. HIV/AIDS Res. Alliance 2018, 15, 110–120. [Google Scholar] [CrossRef] [Green Version]
- Bonnet, F.; Le Marec, F.; Leleux, O.; Gerard, Y.; Neau, D.; Lazaro, E.; Duffau, P.; Caubet, O.; Vandenhende, M.-A.; Mercie, P. Evolution of comorbidities in people living with HIV between 2004 and 2014: Cross-sectional analyses from ANRS CO3 Aquitaine cohort. BMC Infect. Dis. 2020, 20, 850. [Google Scholar] [CrossRef]
- Adam, A.M. A Study on Sample Size Determination in Survey Research. New Ideas Concern. Sci. Technol. 2021, 4, 125–134. [Google Scholar]
- Louangrath, P. Minimum sample size method based on survey scales. Int. J. Res. Methodol. Soc. Sci. 2017, 3, 44–52. [Google Scholar]
- Klar, S.; Leeper, T.J. Identities and intersectionality: A case for Purposive sampling in Survey-Experimental research. In Experimental Methods in Survey Research: Techniques that Combine Random Sampling with Random Assignment; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2019; pp. 419–433. [Google Scholar]
- Yadegaridehkordi, E.; Nilashi, M.; Shuib, L.; Bin Md Nasir, M.H.N.; Asadi, S.; Samad, S.; Awang, N.F. The impact of big data on firm performance in hotel industry. Electron. Commer. Res. Appl. 2020, 40, 100921. [Google Scholar] [CrossRef]
- Tan, X.; Patel, I.; Chang, J. Review of the four item Morisky medication adherence scale (MMAS-4) and eight item Morisky medication adherence scale (MMAS-8). Innov. Pharm. 2014, 5, 165. [Google Scholar] [CrossRef]
- Lam, W.Y.; Fresco, P. Medication adherence measures: An overview. BioMed Res. Int. 2015, 2015, 217047. [Google Scholar] [CrossRef] [PubMed]
- Cooper, V.; Clatworthy, J.; Harding, R.; Whetham, J. Measuring quality of life among people living with HIV: A systematic review of reviews. Health Qual. Life Outcomes 2017, 15, 1–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, H.; Yang, Z.; Zhu, Z.; Han, S.; Zhang, L.; Hu, Y. Psychometric properties of self-reported measures of health-related quality of life in people living with HIV: A systematic review. Health Qual. Life Outcomes 2022, 20, 1–43. [Google Scholar] [CrossRef]
- Valdelamar-Jiménez, J.; Lins-Kusterer, L.; de Jesus, S.T.G.; Netto, E.M.; Brites, C. Comparison of three health-related quality of life instruments to evaluate symptoms of depression in HIV patients in Brazil. J. Clin. Psychol. Med. Settings 2020, 27, 643–650. [Google Scholar] [CrossRef]
- Lorenc, A.; Ananthavarathan, P.; Lorigan, J.; Banarsee, R.; Jowata, M.; Brook, G. The prevalence of comorbidities among people living with HIV in Brent: A diverse London Borough. Lond. J. Prim. Care 2014, 6, 84–90. [Google Scholar] [CrossRef]
- Gianella, S.; Saloner, R.; Curtin, G.; Little, S.J.; Heaton, A.; Montoya, J.L.; Letendre, S.L.; Marquine, M.J.; Jeste, D.V.; Moore, D.J. A cross-sectional study to evaluate the effects of age and duration of HIV infection on anxiety and depression in cisgender men. AIDS Behav. 2022, 26, 196–203. [Google Scholar] [CrossRef]
- Hoenigl, M.; Green, N.; Camacho, M.; Gianella, S.; Mehta, S.R.; Smith, D.M.; Little, S.J. Signs or symptoms of acute HIV infection in a cohort undergoing community-based screening. Emerg. Infect. Dis. 2016, 22, 532–534. [Google Scholar] [CrossRef] [Green Version]
- Mircioiu, C.; Atkinson, J. A comparison of parametric and non-parametric methods applied to a Likert scale. Pharmacy 2017, 5, 26. [Google Scholar] [CrossRef] [Green Version]
- Vonglao, P. Application of fuzzy logic to improve the Likert scale to measure latent variables. Kasetsart J. Soc. Sci. 2017, 38, 337–344. [Google Scholar] [CrossRef]
- Lin, L.-C.; Yao, G. Validation of the factor structure of the WHOQOL-BREF using meta-analysis of exploration factor analysis and social network analysis. Psychol. Assess. 2022, 34, 660–670. [Google Scholar] [CrossRef] [PubMed]
- Skevington, S.M.; Epton, T. How will the sustainable development goals deliver changes in well-being? A systematic review and meta-analysis to investigate whether WHOQOL-BREF scores respond to change. BMJ Glob. Health 2018, 3, e000609. [Google Scholar] [CrossRef] [PubMed]
- Okagbue, H.I.; Oguntunde, P.E.; Obasi, E.C.; Akhmetshin, E.M. Trends and usage pattern of SPSS and Minitab Software in Scientific research. J. Phys. Conf. Ser. 2021, 1734, 012017. [Google Scholar] [CrossRef]
- Makovec, U.N.; Locatelli, I.; Kos, M. Improved adherence with Medicines Use Review service in Slovenia: A randomized controlled trial. BMC Health Serv. Res. 2021, 21, 266. [Google Scholar]
- Shimels, T.; Asrat Kassu, R.; Bogale, G.; Bekele, M.; Getnet, M.; Getachew, A.; Shewamene, Z.; Abraha, M. Magnitude and associated factors of poor medication adherence among diabetic and hypertensive patients visiting public health facilities in Ethiopia during the COVID-19 pandemic. PLoS ONE 2021, 16, e0249222. [Google Scholar] [CrossRef]
- Minwuyelet, F.; Mulugeta, H.; Tsegaye, D.; Lake, B.; Getie, A.; Tsegaye, B.; Mullu, G. Quality of life and associated factors among patients with epilepsy at specialized hospitals, Northwest Ethiopia; 2019. PLoS ONE 2022, 17, e0262814. [Google Scholar] [CrossRef]
- Mor, Z.; Sheffer, R.; Chemtob, D. Causes of death and mortality trends of all individuals reported with HIV/AIDS in Israel, 1985–2010. J. Public Health 2018, 40, 56–64. [Google Scholar] [CrossRef] [Green Version]
- Wandeler, G.; Johnson, L.F.; Egger, M. Trends in life expectancy of HIV-positive adults on ART across the globe: Comparisons with general population. Curr. Opin. HIV AIDS 2016, 11, 492–500. [Google Scholar] [CrossRef] [Green Version]
- Godongwana, M.; De Wet-Billings, N.; Milovanovic, M. The comorbidity of HIV, hypertension and diabetes: A qualitative study exploring the challenges faced by healthcare providers and patients in selected urban and rural health facilities where the ICDM model is implemented in South Africa. BMC Health Serv. Res. 2021, 21, 647. [Google Scholar] [CrossRef]
- Yang, H.-Y.; Beymer, M.R.; Suen, S.-C. Chronic disease onset among people living with HIV and AIDS in a large private insurance claims dataset. Sci. Rep. 2019, 9, 18514. [Google Scholar] [CrossRef] [Green Version]
- Msomi, N.; Naidoo, K.; Yende-Zuma, N.; Padayatchi, N.; Govender, K.; Singh, J.A.; Abdool-Karim, S.; Abdool-Karim, Q.; Mlisana, K. High incidence and persistence of hepatitis B virus infection in individuals receiving HIV care in KwaZulu-Natal, South Africa. BMC Infect. Dis. 2020, 20, 847. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.N.; Val, F.; Macedo, Á.E.; Cubas-Vega, N.; Tejo, P.L.D.; Marques, M.M.; de Alencar Filho, A.C.; de Lacerda, M.V.G. Increased prevalence of hypertension among people living with HIV: Where to begin? Rev. Soc. Bras. Med. Trop. 2020, 53, e20190564. [Google Scholar] [CrossRef] [PubMed]
- Sarfo, F.S.; Nichols, M.; Singh, A.; Hardy, Y.; Norman, B.; Mensah, G.; Tagge, R.; Jenkins, C.; Ovbiagele, B. Characteristics of hypertension among people living with HIV in Ghana: Impact of new hypertension guideline. J. Clin. Hypertens. 2019, 21, 838–850. [Google Scholar] [CrossRef] [PubMed]
- Eberhardt, K.A.; Sarfo, F.S.; Dompreh, A.; Kuffour, E.O.; Geldmacher, C.; Soltau, M.; Schachscheider, M.; Drexler, J.F.; Eis-Hübinger, A.M.; Häussinger, D. Helicobacter pylori coinfection is associated with decreased markers of immune activation in ART-naive HIV-positive and in HIV-negative individuals in Ghana. Clin. Infect. Dis. 2015, 61, 1615–1623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Archampong, T.N.; Asmah, R.H.; Wiredu, E.K.; Gyasi, R.K.; Nkrumah, K.N. Factors associated with gastro-duodenal disease in patients undergoing upper GI endoscopy at the Korle-Bu Teaching Hospital, Accra, Ghana. Afr. Health Sci. 2016, 16, 611–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sato, Y.; Fukudo, S. Gastrointestinal symptoms and disorders in patients with eating disorders. Clin. J. Gastroenterol. 2015, 8, 255–263. [Google Scholar] [CrossRef] [Green Version]
- Fiseha, T.; Alemu, W.; Dereje, H.; Tamir, Z.; Gebreweld, A. Prevalence of dyslipidaemia among HIV-infected patients receiving combination antiretroviral therapy in North Shewa, Ethiopia. PLoS ONE 2021, 16, e0250328. [Google Scholar] [CrossRef]
- Tilahun, H.; Masyuko, S.J.; Mogaka, J.N.; Temu, T.; Kinuthia, J.; Osoti, A.O.; Nakanjako, D.; Farquhar, C.; Page, S.T. Prevalence and correlates of dyslipidemia in HIV positive and negative adults in Western Kenya: A cross-sectional study. Medicine 2021, 100, e24800. [Google Scholar] [CrossRef]
- Ekrikpo, U.E.; Akpan, E.E.; Ekott, J.U.; Bello, A.K.; Okpechi, I.G.; Kengne, A.P. Prevalence and correlates of traditional risk factors for cardiovascular disease in a Nigerian ART-naive HIV population: A cross-sectional study. BMJ Open 2018, 8, e019664. [Google Scholar] [CrossRef] [Green Version]
- So-Armah, K.; Benjamin, L.A.; Bloomfield, G.S.; Feinstein, M.J.; Hsue, P.; Njuguna, B.; Freiberg, M.S. HIV and cardiovascular disease. Lancet HIV 2020, 7, e279–e293. [Google Scholar] [CrossRef]
- Touloumi, G.; Kalpourtzi, N.; Papastamopoulos, V.; Paparizos, V.; Adamis, G.; Antoniadou, A.; Chini, M.; Karakosta, A.; Makrilakis, K.; Gavana, M. Cardiovascular risk factors in HIV infected individuals: Comparison with general adult control population in Greece. PLoS ONE 2020, 15, e0230730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saad, H.; Ntusi, N.A. HIV-associated cardiovascular disease. In Advances in HIV and AIDS Control; IntechOpen: London, UK, 2018. [Google Scholar] [CrossRef] [Green Version]
- Rajagopaul, A.; Naidoo, M. Prevalence of diabetes mellitus and hypertension amongst the HIV-positive population at a district hospital in eThekwini, South Africa. Afr. J. Prim. Health Care Fam. Med. 2021, 13, 2766. [Google Scholar] [CrossRef] [PubMed]
- Umar, D.M.; Naidoo, P. Prevalence and predictors of diabetes mellitus among persons living with HIV: A retrospective cohort study conducted in 4 public healthcare facilities in KwaZulu-Natal. BMC Public Health 2021, 21, 288. [Google Scholar] [CrossRef] [PubMed]
- Abebe, S.M.; Getachew, A.; Fasika, S.; Bayisa, M.; Demisse, A.G.; Mesfin, N. Diabetes mellitus among HIV-infected individuals in follow-up care at University of Gondar Hospital, Northwest Ethiopia. BMJ Open 2016, 6, e011175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prioreschi, A.; Munthali, R.; Soepnel, L.; Goldstein, J.; Micklesfield, L.; Aronoff, D.; Norris, S. Incidence and prevalence of type 2 diabetes mellitus with HIV infection in Africa: A systematic review and meta-analysis. BMJ Open 2017, 7, e013953. [Google Scholar] [CrossRef] [PubMed]
- Machingura, P.I.; Chindore, A. Diabetes mellitus prevalence in HIV patients on antiretroviral therapy at Parirenyatwa Group of Hospitals Opportunistic Infections Clinic, Harare, Zimbabwe. Texila Int. J. Public Health 2017, 5, 17. [Google Scholar] [CrossRef] [Green Version]
- Huang, X.; Meyers, K.; Liu, X.; Li, X.; Zhang, T.; Xia, W.; Hou, J.; Song, A.; He, H.; Li, C. The double burdens of mental health among AIDS patients with fully successful immune restoration: A cross-sectional study of anxiety and depression in China. Front. Psychiatry 2018, 9, 384. [Google Scholar] [CrossRef] [PubMed]
- Siakwa, M.; Okanlawon, F.; Druye, A.; Ankobil, A.; Aniweh, Y.; Dzah, S. Prevalence of psychiatric disorders in HIV patients in the Central Region of Ghana. J. Community Med. Prim. Health Care 2015, 27, 79–85. [Google Scholar]
- Mills, J.C.; Pence, B.W.; Edmonds, A.; Adedimeji, A.; Schwartz, R.M.; Kassaye, S.; Cocohoba, J.; Cohen, M.H.; Neigh, G.; Fischl, M.A. The impact of cumulative depression along the HIV care continuum in women living with HIV during the era of universal antiretroviral treatment. JAIDS J. Acquir. Immune Defic. Syndr. 2019, 82, 225–233. [Google Scholar] [CrossRef]
- Dinani, A.; Khan, A.; Dieterich, D. Emerging prevalence of fatty liver disease in HIV. Future Virol. 2021, 16, 59–73. [Google Scholar] [CrossRef]
- Torgersen, J.; So-Armah, K.; Freiberg, M.S.; Goetz, M.B.; Budoff, M.J.; Lim, J.K.; Taddei, T.; Butt, A.A.; Rodriguez-Barradas, M.C.; Justice, A.C. Comparison of the prevalence, severity, and risk factors for hepatic steatosis in HIV-infected and uninfected people. BMC Gastroenterol. 2019, 19, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rafiq, N.; Stepanova, M.; Lam, B.; Nader, F.; Srishord, M.; Younossi, Z.M. Predictors of chronic liver disease in individuals with human immunodeficiency virus infection. Ann. Hepatol. 2014, 13, 60–64. [Google Scholar] [CrossRef]
- Agyei-Nkansah, A.; Taylor-Robinson, S. The state of Ghanaian liver medicine. Pan Afr. Med. J. 2021, 39, 148. [Google Scholar] [CrossRef]
- Aidoo, M.; Mohammed, B.S. Distribution and Determinants of Etiologies and Complications of Chronic Liver Diseases among Patients at a Tertiary Hospital in a Lower Economic Region of Ghana. Cent. Afr. J. Public Health 2020, 60, 280–287. [Google Scholar] [CrossRef]
- Kirenga, B.J.; Mugenyi, L.; de Jong, C.; Davis, J.L.; Katagira, W.; van der Molen, T.; Kamya, M.R.; Boezen, M. The impact of HIV on the prevalence of asthma in Uganda: A general population survey. Respir. Res. 2018, 19, 184. [Google Scholar] [CrossRef]
- Kynyk, J.A.; Parsons, J.P.; Para, M.F.; Koletar, S.L.; Diaz, P.T.; Mastronarde, J.G. HIV and asthma, is there an association? Respir. Med. 2012, 106, 493–499. [Google Scholar] [CrossRef] [Green Version]
- de Los Rios, P.; Okoli, C.; Punekar, Y.; Allan, B.; Muchenje, M.; Castellanos, E.; Richman, B.; Corbelli, G.M.; Hardy, W.D.; Young, B. Prevalence, determinants, and impact of suboptimal adherence to HIV medication in 25 countries. Prev. Med. 2020, 139, 106182. [Google Scholar] [CrossRef]
- Spaan, P.; van Luenen, S.; Garnefski, N.; Kraaij, V. Psychosocial interventions enhance HIV medication adherence: A systematic review and meta-analysis. J. Health Psychol. 2020, 25, 1326–1340. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Chen, K.; Kalichman, S.C. Barriers to HIV medication adherence as a function of regimen simplification. Ann. Behav. Med. 2017, 51, 67–78. [Google Scholar] [CrossRef] [Green Version]
- Sarkar, T.; Karmakar, N.; Dasgupta, A.; Saha, B. Quality of life of people living with HIV/AIDS attending antiretroviral clinic in the center of excellence in HIV care in India. J. Educ. Health Promot. 2019, 8, 226. [Google Scholar]
- Osei-Yeboah, J.; Owiredu, W.K.; Norgbe, G.K.; Lokpo, S.Y.; Obirikorang, C.; Allotey, E.A.; Deku, J.G.; Asiamah, E.A.; Manaphraim, N.Y.B.; Senyo Kwasi Nyamadi, P. Quality of life of people living with HIV/AIDS in the Ho Municipality, Ghana: A cross-sectional study. AIDS Res. Treat. 2017, 2017, 6806951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osamika, B.; Mayungbo, O. Quality of Life of People Living with HIV/AIDS: The Roles of Clinical and Demographic Factors. Am. J. Soc. Sci. Humanit. 2019, 4, 233–245. [Google Scholar] [CrossRef]
- Negera, G.Z.; Mega, T.A. Health-related quality of life among admitted HIV/AIDS patients in selected Ethiopian tertiary care settings: A cross-sectional study. Open Public Health J. 2019, 12, 532–540. [Google Scholar] [CrossRef] [Green Version]
- Ma, L.; Xu, P.; Lin, H.; Ju, L.; Lv, F. Quality of life of people living with HIV/AIDS: A cross-sectional study in Zhejiang Province, China. PLoS ONE 2015, 10, e0135705. [Google Scholar]
- Bakiono, F.; Ouédraogo, L.; Sanou, M.; Samadoulougou, S.; Guiguemdé, P.W.L.; Kirakoya-Samadoulougou, F.; Robert, A. Quality of life in people living with HIV: A cross-sectional study in Ouagadougou, Burkina Faso. Springerplus 2014, 3, 372. [Google Scholar] [CrossRef]
- Yaya, I.; Djalogue, L.; Patassi, A.A.; Landoh, D.E.; Assindo, A.; Nambiema, A.; Kolani, K.; Patchali, P.; Bignandi, E.M.; Diallo, A. Health-related quality of life among people living with HIV/AIDS in Togo: Individuals and contextual effects. BMC Res. Notes 2019, 12, 140. [Google Scholar] [CrossRef] [Green Version]
- Petoumenos, K.; Huang, R.; Hoy, J.; Bloch, M.; Templeton, D.J.; Baker, D.; Giles, M.; Law, M.G.; Cooper, D.A. Prevalence of self-reported comorbidities in HIV positive and HIV negative men who have sex with men over 55 years—The Australian Positive & Peers Longevity Evaluation Study (APPLES). PLoS ONE 2017, 12, e0184583. [Google Scholar]
- Farahat, F.M.; Alghamdi, Y.S.; Farahat, A.F.; Alqurashi, A.A.; Alburayk, A.K.; Alabbasi, A.A.; Alsaedi, A.A.; Alshamrani, M.M. The prevalence of comorbidities among adult people diagnosed with HIV infection in a tertiary care hospital in western Saudi Arabia. J. Infect. Public Health 2020, 13, 1699–1704. [Google Scholar] [CrossRef]
- Gallant, J.; Hsue, P.Y.; Shreay, S.; Meyer, N. Comorbidities among US patients with prevalent HIV infection—A trend analysis. J. Infect. Dis. 2017, 216, 1525–1533. [Google Scholar] [CrossRef]
- Schouten, J.; Wit, F.W.; Stolte, I.G.; Kootstra, N.A.; van der Valk, M.; Geerlings, S.E.; Prins, M.; Reiss, P. Cross-sectional comparison of the prevalence of age-associated comorbidities and their risk factors between HIV-infected and uninfected individuals: The AGEhIV cohort study. Clin. Infect. Dis. 2014, 59, 1787–1797. [Google Scholar] [CrossRef]
- Tlou, B. The influence of marital status on HIV infection in an HIV hyperendemic area of rural South Africa, 2000–2017. Afr. J. AIDS Res. 2019, 18, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Penney, A.T.; Iudicello, J.E.; Riggs, P.K.; Doyle, K.; Ellis, R.J.; Letendre, S.L.; Grant, I.; Woods, S.P.; The HIV Neurobehavioral Research Program (HNRP) Group. Co-morbidities in persons infected with HIV: Increased burden with older age and negative effects on health-related quality of life. AIDS Patient Care STDs 2013, 27, 5–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mayer, K.H.; Loo, S.; Crawford, P.M.; Crane, H.M.; Leo, M.; DenOuden, P.; Houlberg, M.; Schmidt, M.; Quach, T.; Ruhs, S. Excess clinical comorbidity among HIV-infected patients accessing primary care in US community health centers. Public Health Rep. 2018, 133, 109–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collins, L.F.; Sheth, A.N.; Mehta, C.C.; Naggie, S.; Golub, E.T.; Anastos, K.; French, A.L.; Kassaye, S.; Taylor, T.; Fischl, M.A. The prevalence and burden of non-AIDS comorbidities among women living with or at risk for human immunodeficiency virus infection in the United States. Clin. Infect. Dis. 2021, 72, 1301–1311. [Google Scholar] [CrossRef]
- de la Hoya Zamácola, P.S.; Alía, C.A.; Marco, A.; Burgos, A.L.; de Juan Ramírez, J.; Matías, A.H.; Sogorb, J.P. The progression of liver fibrosis in prison inmates co-infected by HIV and HCV who started on boosted protease inhibitor therapy. Rev. Esp. Sanid Penit. 2013, 15, 54–62. [Google Scholar]
- Nlooto, M. Comorbidities of HIV infection and health care seeking behavior among HIV infected patients attending public sector healthcare facilities in KwaZulu-Natal: A cross sectional study. PLoS ONE 2017, 12, e0170983. [Google Scholar] [CrossRef] [Green Version]
- Yang, C.-J.; Wang, H.-Y.; Chou, T.-C.; Chang, C.-J. Prevalence and related drug cost of comorbidities in HIV-infected patients receiving highly active antiretroviral therapy in Taiwan: A cross-sectional study. J. Microbiol. Immunol. Infect. 2019, 52, 720–727. [Google Scholar] [CrossRef]
- Funke, B.; Spinner, C.; Wolf, E.; Heiken, H.; Christensen, S.; Stellbrink, H.; Witte, V. High prevalence of comorbidities and use of concomitant medication in treated people living with HIV in Germany–results of the BESIDE study. Int. J. STD AIDS 2021, 32, 152–161. [Google Scholar] [CrossRef]
- Ghiasvand, H.; Waye, K.M.; Noroozi, M.; Harouni, G.G.; Armoon, B.; Bayani, A. Clinical determinants associated with quality of life for people who live with HIV/AIDS: A meta-analysis. BMC Health Serv. Res. 2019, 19, 768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emuren, L.; Welles, S.; Evans, A.A.; Polansky, M.; Okulicz, J.F.; Macalino, G.; Agan, B.K.; the Infectious Disease Clinical Research Program HIV Working Group. Health-related quality of life among military HIV patients on antiretroviral therapy. PLoS ONE 2017, 12, e0178953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niu, M.; Zhang, L.; Wang, Y.; Tu, R.; Liu, X.; Wang, C.; Bie, R. Lifestyle score and genetic factors with hypertension and blood pressure among adults in rural China. Front. Public Health 2021, 9, 687174. [Google Scholar] [CrossRef] [PubMed]
- Romain, A.J.; Marleau, J.; Baillot, A. Impact of obesity and mood disorders on physical comorbidities, psychological well-being, health behaviours and use of health services. J. Affect. Disord. 2018, 225, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Ociskova, M.; Prasko, J.; Latalova, K.; Kamaradova, D.; Grambal, A. Psychological factors and treatment effectiveness in resistant anxiety disorders in highly comorbid inpatients. Neuropsychiatr. Dis. Treat. 2016, 12, 1539–1551. [Google Scholar] [CrossRef] [PubMed]
| Variable | Frequency (N = 360) | %N |
|---|---|---|
| Sex | ||
| Male | 81 | 22.5 |
| Female | 279 | 77.5 |
| Age groups | ||
| 18–29 | 53 | 14.7 |
| 30–39 | 108 | 30.0 |
| 40–49 | 113 | 31.4 |
| >49 | 86 | 23.9 |
| Marital Status | ||
| Married | 190 | 52.8 |
| Divorced | 23 | 6.4 |
| Widowed | 66 | 18.3 |
| Single | 81 | 22.5 |
| Educational Status | ||
| None | 120 | 33.3 |
| Primary | 39 | 10.8 |
| Secondary | 97 | 26.9 |
| Tertiary | 104 | 28.9 |
| Presence/absence of HIV symptoms | ||
| Asymptomatic | 337 | 93.6 |
| Symptomatic | 23 | 6.4 |
| Duration of HIV Infection (since time of infection) | ||
| <5 years | 195 | 54.2 |
| >5 years | 165 | 45.8 |
| Variable | Frequency (N) | %N |
|---|---|---|
| Comorbidity present | 109 | 30.3 |
| Comorbidity absent | 188 | 69.7 |
| Total | 297 | 100 |
| One comorbidity present | 101 | 28.1 |
| Multiple comorbidity | 8 | 2.2 |
| Total | 109 | 30.3 |
| Comorbidities | ||
| Hypertension | 33 | 9.2 |
| Hepatitis B | 73 | 20.3 |
| Other liver disease (fatty liver, HCV) | 4 | 1.1 |
| Peptic ulcer | 11 | 3.1 |
| Cardiovascular diseases | 8 | 2.2 |
| Dyslipidemia | 4 | 1.1 |
| Diabetes | 3 | 0.8 |
| Mental health issues | 2 | 0.6 |
| Asthma | 2 | 0.6 |
| Quality of Life | ||||
|---|---|---|---|---|
| Domain | Poor | Good | Excellent | Average (min–max) |
| Physical | 4 (4.4) | 41 (11.4) | 315 (87.5) | 18.1 ± 2.1 (8–20) |
| Psychological | 0 | 30 (8.8) | 309 (91.2) | 17.8 ± 1.9 (12–20) |
| Independence | 0 | 72 (20.0) | 288 (80.0) | 17.4 ± 2.3 (11–20) |
| Relationship | 3 (0.8) | 106 (29.4) | 251 (69.7) | 16.7 ± 2.4 (8–20) |
| Environment | 1 (0.3) | 229 (68.2) | 106 (31.5) | 14.6 ± 1.9 (9–18.5) |
| Spirituality | 24 (6.7) | 118 (32.8) | 218 (60.6) | 15.8 ± 3.7 (6–20) |
| Overall Health | 27 (7.5) | 180 (50.0) | 153 (42.5) | 4.3 ± 0.7 (1–5) |
| Overall QoL | 42 (11.7) | 169 (46.9) | 149 (41.4) | 4.3 ± 0.7 (1–5) |
| Presence of Comorbidities | ||||
|---|---|---|---|---|
| Variable | Yes (%) | No (%) | χ2 | p-Value |
| Age | 2.1 | 0.54 | ||
| 18–29 | 12 (3.3) | 41 (11.4) | ||
| 30–39 | 32 (8.9) | 76 (21.1) | ||
| 40–49 | 38 (10.6) | 75 (20.8) | ||
| ≥50 | 27 (7.5) | 59 (16.4) | ||
| Education | 1.8 | 0.61 | ||
| None | 36 (10.0) | 84 (23.3) | ||
| Primary | 14 (3.9) | 25 (6.9) | ||
| Secondary | 25 (6.9) | 72 (20.0) | ||
| Tertiary | 34 (9.4) | 70 (19.4) | ||
| Gender | 3.2 | 0.07 | ||
| Male | 18 (5.0) | 63 (17.5) | ||
| Female | 91 (25.3) | 188 (52.2) | ||
| Marital Status | 12.6 | 0.005 | ||
| Married | 54 (15.0) | 136 (37.8) | ||
| Divorced | 9 (2.5) | 14 (3.9) | ||
| Widowed | 30 (8.3) | 36 (10.0) | ||
| Single | 16 (4.4) | 65 (18.1) | ||
| Presence or absence of symptoms of HIV | 22.2 | <0.001 | ||
| Asymptomatic | 92 (25.6) | 245 (68.1) | ||
| Symptomatic | 17 (4.7) | 6 (1.7) | ||
| Years living with HIV (since time of infection) | 0.20 | 0.73 | ||
| ≤5 years | 61 (16.9) | 134 (37.2) | ||
| >5 years | 48 (13.3) | 117 (32.5) | ||
| Adherence to therapy | 9.45 | 0.009 | ||
| Low | 27 (7.5) | 33 (9.2) | ||
| Moderate | 35 (9.7) | 73 (20.3) | ||
| High | 47 (13.1) | 145 (40.3) | ||
| QoL Physical domain | 12.46 | 0.002 | ||
| Poor | 4 (1.1) | 0 | ||
| Good | 17 (4.7) | 24 (6.7) | ||
| Excellent | 88 (24.4) | 227 (63.1) | ||
| QoL Psychological domain | 10.16 | 0.002 | ||
| Good | 17 (5.0) | 13 (3.8) | ||
| Excellent | 88 (26.0) | 221 (65.2) | ||
| QoL Independence domain | 6.96 | 0.010 | ||
| Good | 31 (8.6) | 41 (11.4) | ||
| Excellent | 78 (21.7) | 210 (58.3) | ||
| QoL Relationship domain | 0.61 | 0.76 | ||
| Poor | 1 (0.3) | 2 (0.6) | ||
| Good | 29 (8.1) | 77 (21.4) | ||
| Excellent | 79 (21.9) | 172 (47.8) | ||
| QoL Environment domain | 0.47 | 0.79 | ||
| Poor | 0 | 1 (0.3) | ||
| Good | 69 (20.5) | 160 (47.6) | ||
| Excellent | 33 (9.8) | 73 (21.7) | ||
| QoL Spirituality Domain | 4.48 | 0.11 | ||
| Poor | 9 (2.5) | 15 (4.2) | ||
| Good | 43 (11.9) | 75 (20.8) | ||
| Excellent | 57 (15.6) | 161 (44.7) | ||
| General Health status | 7.13 | 0.028 | ||
| Poor | 9 (2.5) | 18 (5.0) | ||
| Good | 43 (11.9) | 137 (38.1) | ||
| Excellent | 57 (15.8) | 96 (26.7) | ||
| Overall QoL | 6.60 | 0.038 | ||
| Poor | 15 (4.2) | 27 (7.5) | ||
| Good | 40 (11.1) | 129 (35.8) | ||
| Excellent | 54 (15.0) | 95 (26.4) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hattoh, K.A.; Sienso, B.A.; Kuugbee, E.D. Prevalence of Comorbidities and Associated Factors among HIV Patients Attending Antiretroviral Clinics in the Tamale Metropolis, Ghana. Venereology 2023, 2, 1-15. https://doi.org/10.3390/venereology2010001
Hattoh KA, Sienso BA, Kuugbee ED. Prevalence of Comorbidities and Associated Factors among HIV Patients Attending Antiretroviral Clinics in the Tamale Metropolis, Ghana. Venereology. 2023; 2(1):1-15. https://doi.org/10.3390/venereology2010001
Chicago/Turabian StyleHattoh, Kingsley Aseye, Bryan Aapentuo Sienso, and Eugene Dogkotenge Kuugbee. 2023. "Prevalence of Comorbidities and Associated Factors among HIV Patients Attending Antiretroviral Clinics in the Tamale Metropolis, Ghana" Venereology 2, no. 1: 1-15. https://doi.org/10.3390/venereology2010001
APA StyleHattoh, K. A., Sienso, B. A., & Kuugbee, E. D. (2023). Prevalence of Comorbidities and Associated Factors among HIV Patients Attending Antiretroviral Clinics in the Tamale Metropolis, Ghana. Venereology, 2(1), 1-15. https://doi.org/10.3390/venereology2010001






