Abstract
Background: We examined the characteristics of Kawasaki disease (KD) patients who presented with limited and faint principal clinical features. Methods: We retrospectively reviewed the clinical records of 62 KD patients who presented with limited and faint clinical features at admission. A clinical feature that was recognizable by even junior doctors was defined as a definite feature (d-Feature), and a feature that was faint and recognizable by only experienced doctors was defined as a faint feature (f-Feature). Results: At admission, 82% of patients presented with fever and ≤1 d-Feature. Two days later, the d-Features increased in number and diagnoses of KD were established in 32 patients with fever and ≥4 d-Features. In 30 patients with ≤3 d-Features, experienced doctors recognized f-Features and diagnosed KD in 22 patients because of fever and ≥4 features. Among eight patients with ≤3 features, experienced doctors diagnosed six patients as incomplete KD considering their faint abnormal echocardiographic findings. For the remaining two patients, experienced doctors decided to commence KD treatments considering the patients’ clinical course. Conclusions: Sufficient clinical experience is essential during the diagnosis of KD in patients presenting with limited and f-Features. Educational programs for junior doctors on how to recognize f-Features and evaluate faint abnormal coronary artery findings are necessary.
1. Background
Kawasaki disease (KD) is an acute, self-limited febrile illness of unknown cause that predominantly affects children <5 years of age [1,2,3]. The most serious problem in KD is coronary artery abnormality (CAA), which has been reported worldwide and is the leading cause of acquired heart disease in children of developed countries [1,2,3]. To reduce the incidence of CAAs in KD patients, the appropriate timing of treatment initiation with aspirin and high dose intravenous immunoglobulin (IVIG) is important. Therefore, a timely KD diagnosis is crucial, and a delay of diagnosis should be avoided.
The diagnosis of KD is based on the presence of five or six principal clinical features (fever, conjunctivitis, oral changes, cervical lymphadenopathy, rash, erythema, and change of the extremities) according to the Japanese guidelines [1]. It is also based on the presence of ≥5 days of fever and the presence of up to four of the five principal clinical features according to the guidelines of American Heart Association [2]. Since the principal clinical features other than fever cannot be measured and relatively subjective, it is not unusual for patients with KD to present with limited and faint principal clinical features at admission. In these patients, differential diagnosis of KD should be considered, however, their limited or faint features make it difficult to establish the diagnosis of KD. They usually show elevated white blood cell counts and C-reactive protein values; therefore, treatment with antibiotics is usually initiated [2]. A few days later, additional principal features develop and a diagnosis of KD is established in many patients. A few patients, however, do not present additional features and have a subsequent risk for a delayed diagnosis and the development of CAAs. Examination of the diagnostic process in patients who presented with limited and faint principal features will provide useful information for avoiding delayed diagnoses in these patients.
The American Heart Association statement showed an incomplete KD diagnostic algorithm (iKD-algorithm) for patients with prolonged fever in childhood [4]. This algorithm uses laboratory examinations and echocardiographic findings for patients who have two or three clinical features. When positive specific laboratory or echocardiographic findings are obtained, KD treatment is recommended. This algorithm is reported to be useful in the diagnostic process in the United States [5], and is also expected to be useful in Japan in the diagnosis of patients with limited and faint features. However, it is applied for children when fever persists for five or more days or infants when fever persists for seven or more days [4]. Since the situation of the diagnostic process of KD in the United States is different from that in Japan, its usefulness in Japan cannot be the same as in the United States.
The aims of this study are to examine the characteristics of KD patients with limited and faint principal clinical features, and the usefulness of the iKD-algorithm in diagnosing those patients.
2. Patients and Methods
Subjects were patients with KD who were admitted to our hospital between January 2011 and December 2016. Among them, we used the patients who were diagnosed with an infectious disease at admission and given antibiotics as their initial treatments because of their limited and faint principal clinical features. Medical examinations and treatments of these patients were performed by young trainees (second year junior residents or senior residents in pediatric training from third to sixth year doctors) under the supervision of two experienced doctors (Y.N. and K.M.). The principal clinical features of KD patients were evaluated and recorded by young trainees initially. After that, their features were re-checked and recorded by an experienced doctor. We retrospectively reviewed the clinical records of patients and collected the following information: admission day of illness, diagnosis at admission, day of illness when the diagnosis of KD was established (diagnosis day of illness), and principal clinical features of KD. The first illness day was defined as the day when fever was first observed. Clinical features were categorized as a definite (d-Feature) or a faint (f-Feature) feature. A d-Feature was defined as a clinical feature that was recognizable even for young doctors, and, thus, recognizable for all doctors, while an f-Feature was defined as a feature that was faint and only recognizable by experienced doctors. Total features (t-Features) consisted of d- and f-Features. The number of clinical features, except fever, was counted; therefore, five was the maximum number of clinical features.
Echocardiography of all patients was performed by two experienced doctors (Y.N. and K.M.) two or three times a week during admission and at every outpatient clinic visit after discharge. CAAs were defined as a coronary artery diameter z score [6] ≥2.5 (small aneurysm, 2.5–5.0; aneurysm, ≥5.0). Perivascular brightness (PB) was defined as elevated brightness in the coronary arterial wall [4].
To examine the usefulness of the iKD-algorithm, we applied the iKD-algorithm to patients who had ≤3 d-Features on the day when KD treatment was initiated.
A difference in the incidences between groups was estimated using Fisher’s exact probability test. All p values presented were two-sided, and values of p < 0.05 were considered statistically significant. Data were processed using a statistical program SPSS 25.0 (IBM Japan, Inc., Tokyo, Japan).
3. Results
During the study period, 383 KD patients were admitted and treated in our hospital. Of these, 62 KD patients (16%; 37 males and 25 females) presented with limited and faint clinical features and were diagnosed with a disease other than KD at admission. They were initiated antibiotic treatment at admission. The average age of these patients was 30 ± 27 months, and 24 patients (39%) were infants.
3.1. Admission Day of Illness and Initial Diagnoses
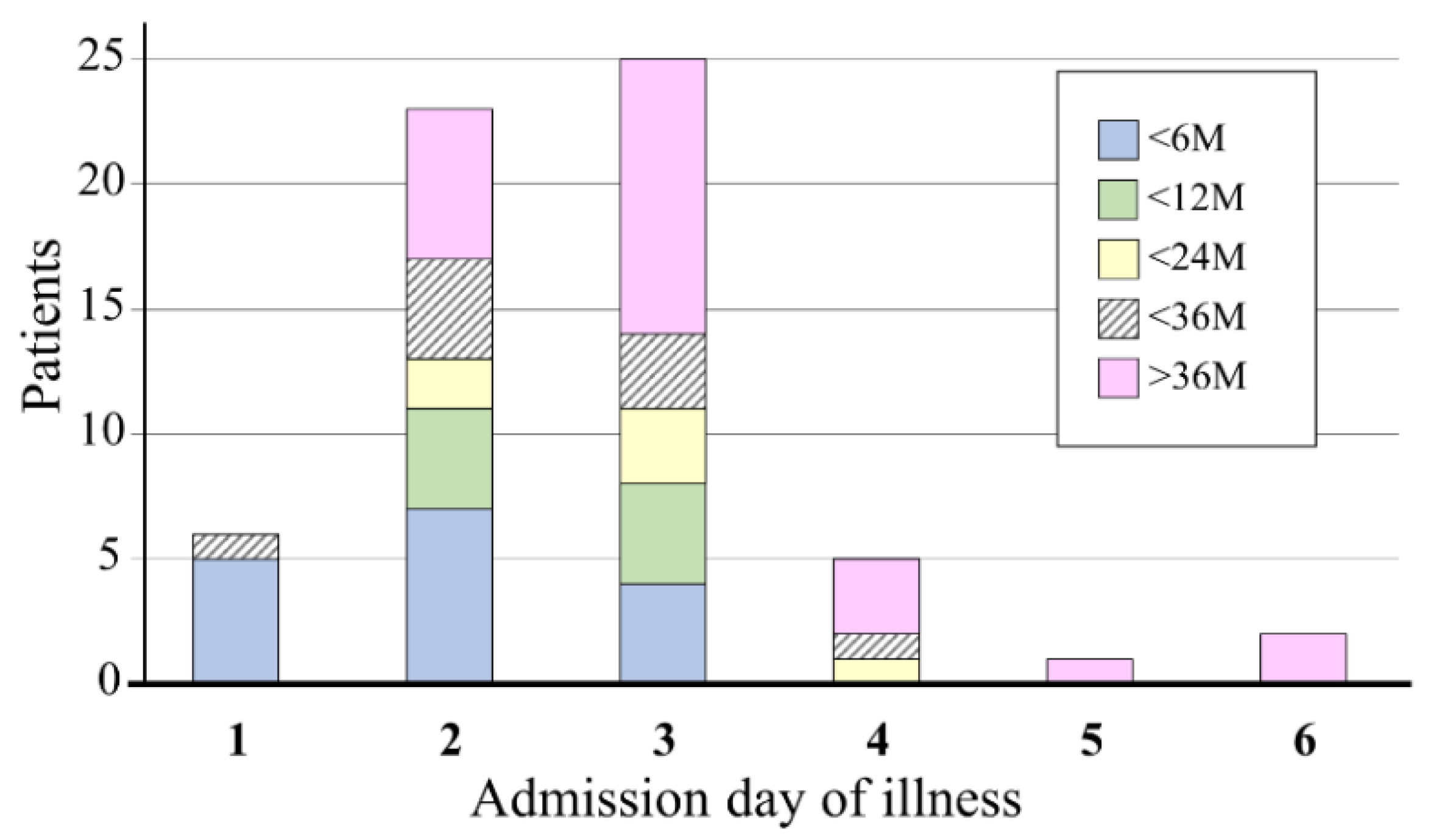
The relationship between the admission day of illness and patient age is shown in Figure 1. All subjects were admitted before the seventh day of illness. The median (interquartile range (IQR)) admission day of illness was day 3 (2,3), and 54 patients (87%) were admitted within the third day of illness. Of the patients admitted within the third day of illness, 44% patients were infants, and all infants were admitted within the third day of illness. Of the patients admitted after the third day of illness, 75% patients were ≥3 years old.
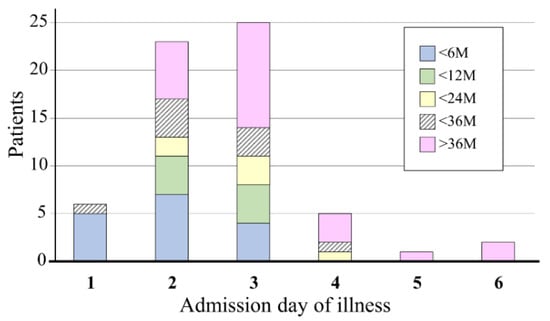
Figure 1.
Distribution of the admission day of illness. Most patients (87%) were admitted within the third day of illness. Of these, 44% of the patients were infants, and all infants were admitted within the third day of illness. Among patients who were admitted after the third day of illness, 75% were ≥3 years old.
The most frequent initial diagnosis was cervical lymphadenitis (27 patients, 44%) (Table 1). Seventeen patients (27%) were diagnosed with a respiratory tract infection (RTI), 14 (23%) were diagnosed with an unknown focus infection (UFI) (including suspected sepsis), and four patients (6%) were diagnosed with a urinary tract infection (UTI) (Table 1). Among them, patients with lymphadenitis as the initial diagnosis were the oldest, followed by patients with RTIs and UFIs (Table 1). Four patients with a UTI were between two and four months old. Most patients (89%) diagnosed with lymphadenitis were ≥1 year old. Among patients ≥1 year old, the incidence of patients diagnosed with lymphadenitis was 63%, which was significantly higher than that among infants (13%; p < 0.0001). Of the patients diagnosed with a UFI, 71% were infants. Among infants, the incidence of UFI was 42%, while that among patients ≥1 year old was 11%; this difference was also statistically significant (p = 0.011).

Table 1.
Initial diagnosis of patients.
The admission day of illness varied according to the disease diagnosed at admission. It was slightly earlier in patients diagnosed with a UTI or UFI than in those with a RTI or lymphadenitis (Table 1). Of the 14 patients diagnosed with a UFI, 11 patients (79%) were admitted between the first and second day of illness. Among patients admitted between the first and second day of illness, 11 patients (38%) were diagnosed with a UFI at admission, whereas among patients admitted on the third day of illness or later, three patients (3%) were diagnosed with a UFI; this difference was statistically significant (p = 0.0131). Among 29 patients admitted between the first and second day of illness, 10 patients (34%) were diagnosed with lymphadenitis, whereas among 33 patients admitted on the third day of illness or later 17 patients (52%) were diagnosed with lymphadenitis. This difference was not statistically significant (p = 0.207).
3.2. Clinical Principal Features of Kawasaki Disease
Forty-six patients (74%) had their clinical features evaluated by the second-year junior residents, seven patients (11%) were evaluated by the third or fourth-year senior residents, and nine patients (15%) were evaluated by the fifth or sixth-year senior residents.
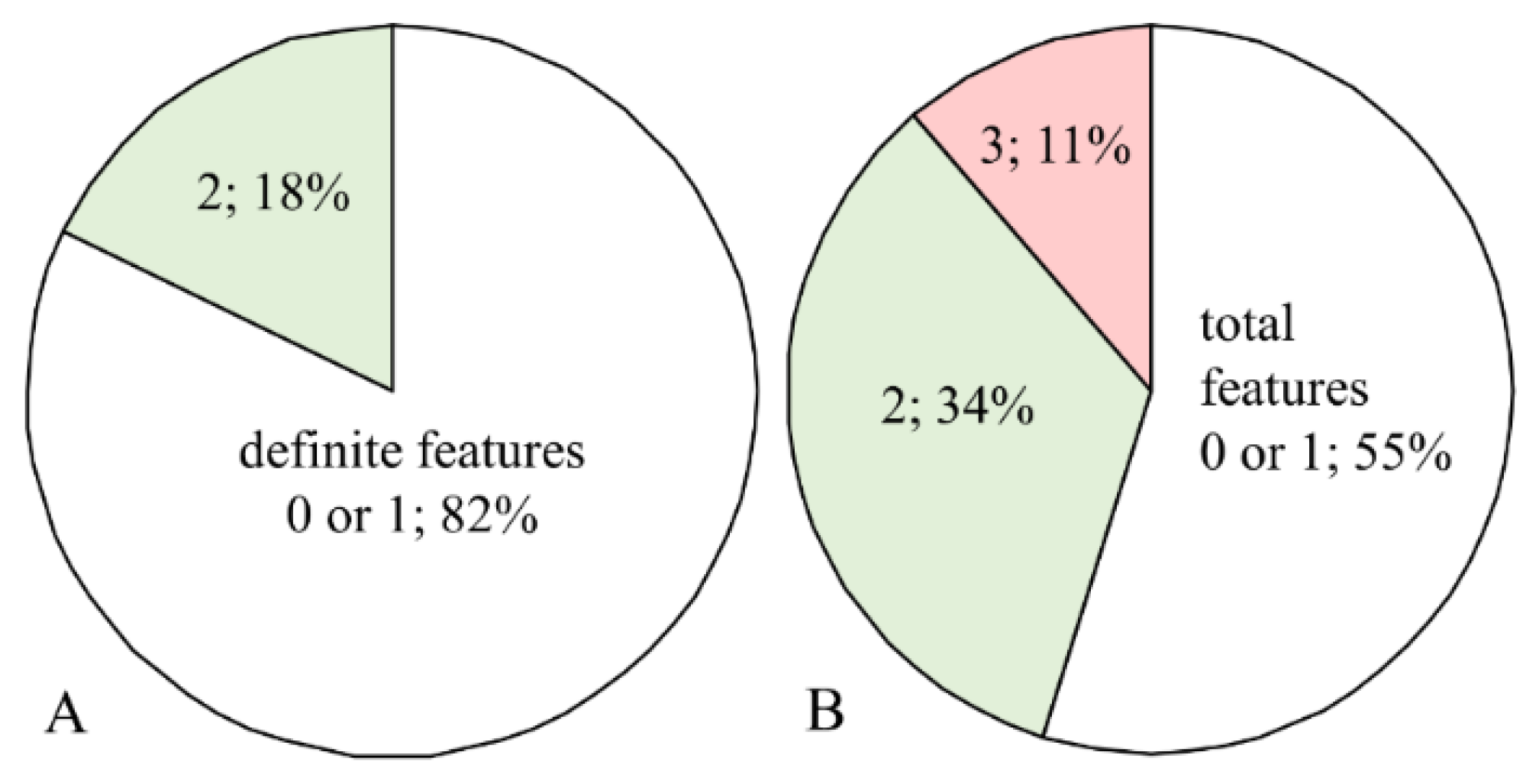
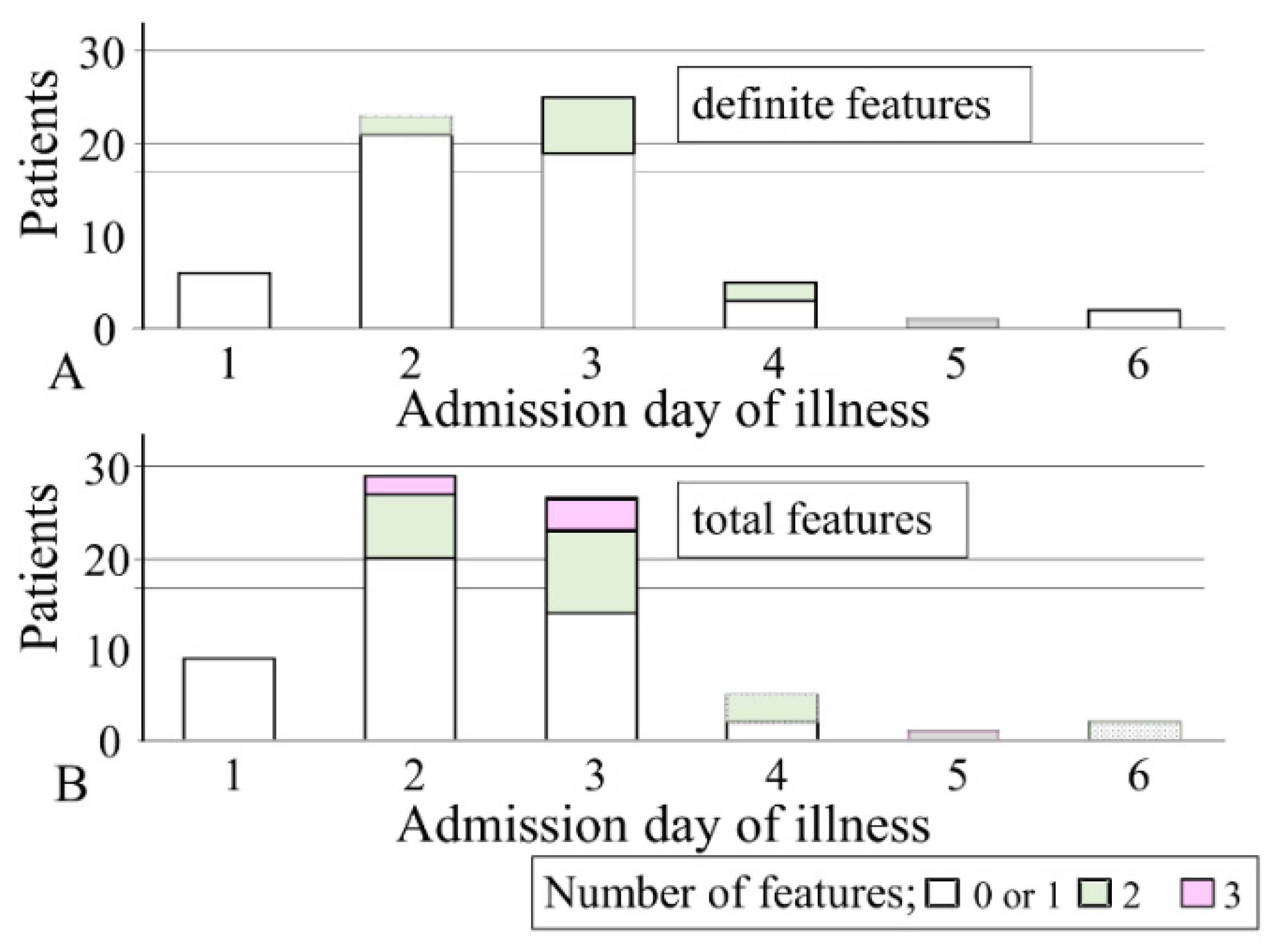
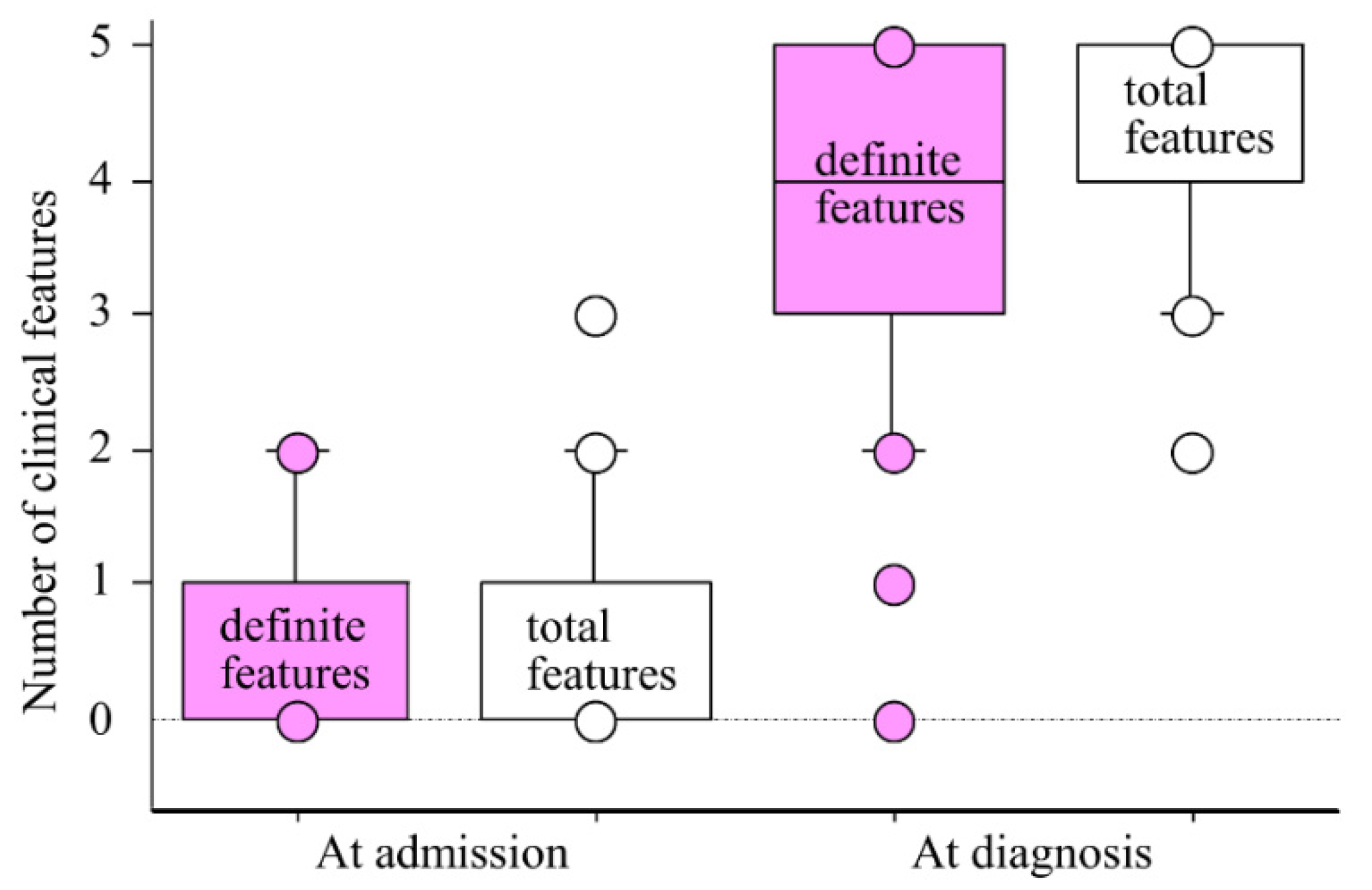
At admission, 51 patients (82%) presented with ≤1 d-Features except for fever (Figure 2A). The remaining patients presented with two d-Features. When counting f-Features, the incidence of patients with one or no features decreased to 55% (Figure 2B). The proportion of patients who presented with two t-Features was 34%. Therefore, most patients (89%) presented with ≤2 t-Features. The relationship between the admission day of illness and number of clinical features is shown in Figure 3. Among the 54 patients who were admitted within the third day of illness, 46 patients (85%) presented with ≤1 d-Features, and 32 patients (59%) presented with ≤1 t-Features. Among the seven patients who presented with three t-Features, six patients were admitted on the second or third day of illness and one patient was admitted on the sixth day of illness.
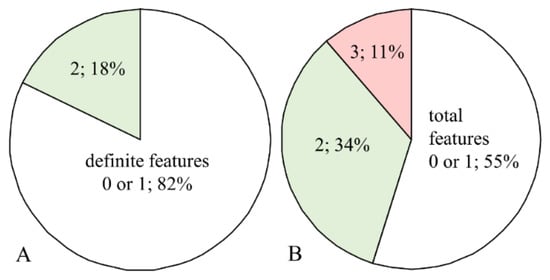
Figure 2.
Proportion of clinical features of Kawasaki disease at admission. (A) Proportion of patients with each number of definite features. (B) Proportion of patients with each number of total features. For definite features, 82% patients presented with one or no definite features and 18% of patients presented with two definite features. For total features, 89% of patients presented with one or two features at admission.
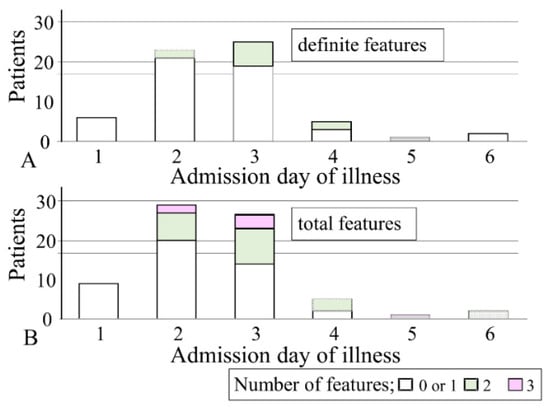
Figure 3.
Number of clinical features of Kawasaki disease at admission and the admission day of illness. (A) Number of definite features and (B) number of total features. Among patients who were admitted within the third day of illness, many patients presented with one or no clinical features (definite features, 85%; total features, 59%). Among eight patients admitted after the third day of illness, the proportion of patients who presented with one or no features decreased to 63% for definite features and 25% for total features.
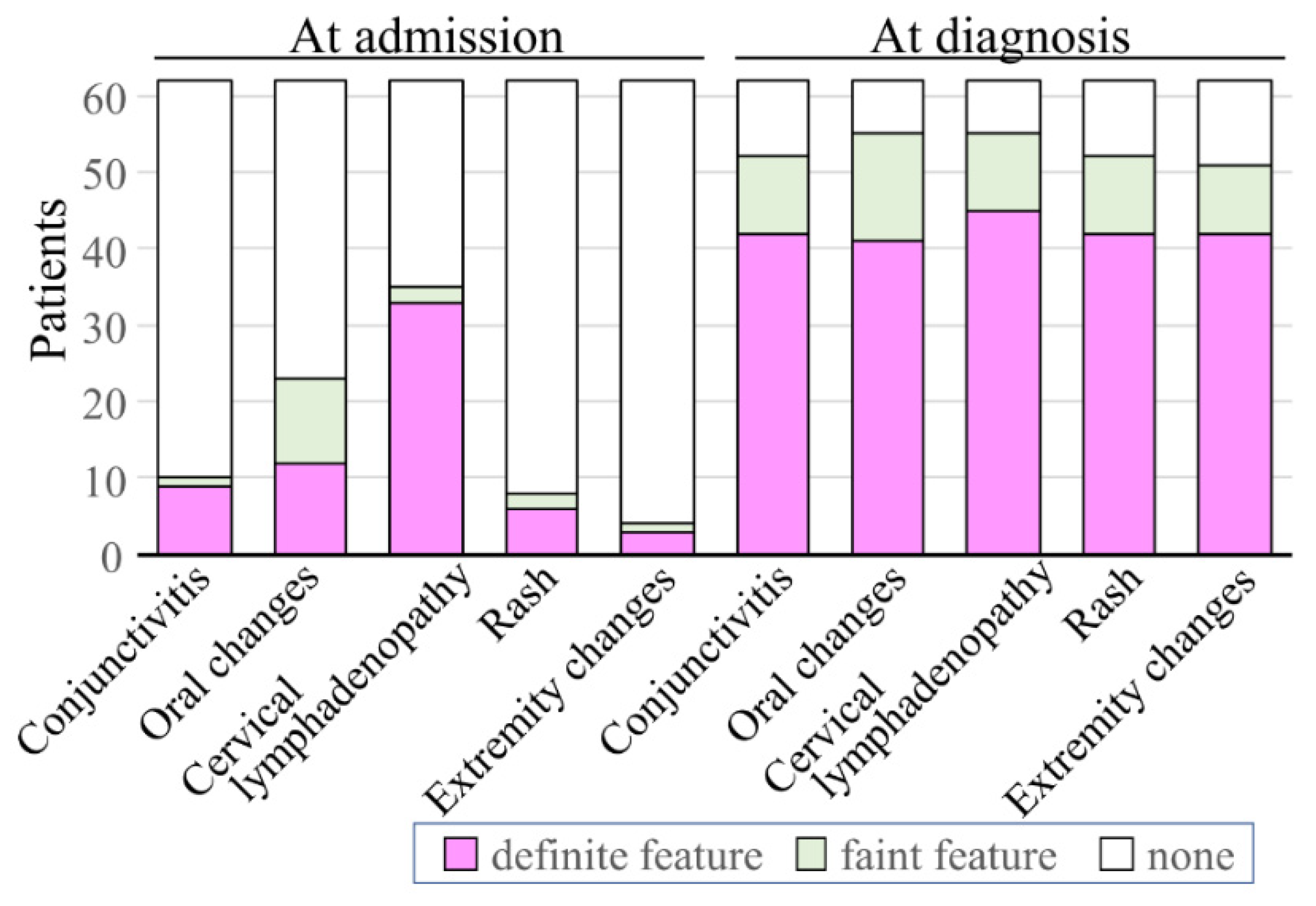
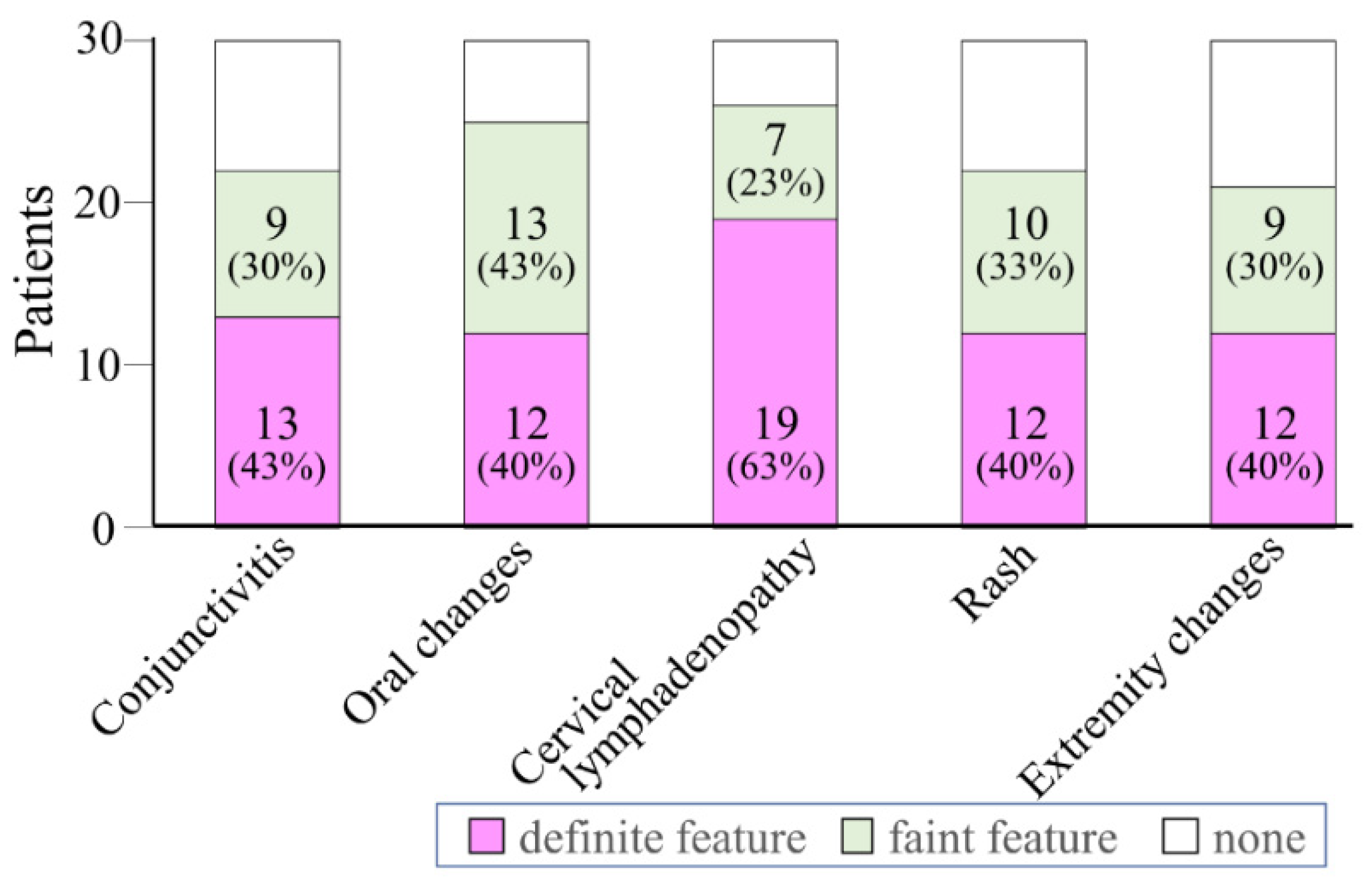
Among the d-Features at admission, cervical lymphadenopathy was the most common (53%), followed by oral changes (19%) and conjunctivitis (15%) (Figure 4). Rash or extremity changes were rarely observed as a d-Feature (3% and 2%, respectively). Most f-Features were rarely observed (2–6%), except for oral changes (18%) (Figure 4). The number of d-Features at admission among each initial diagnosis was not different when lymphadenopathy was excluded.
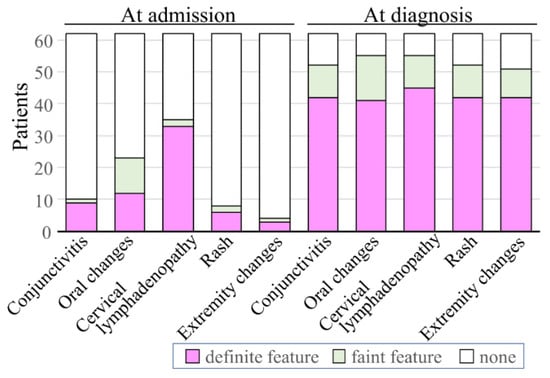
Figure 4.
Proportion of clinical features of Kawasaki disease presented at admission and diagnosis. Cervical lymphadenopathy presented at admission accounted for 53% of definite features, while oral changes and conjunctivitis accounted for 19% and 15%, respectively. Rash or extremity changes were rare (3% and 2%, respectively). The prevalence of oral changes among faint features was 18%, whereas other features were lower (2–6%). At diagnosis, the proportion of definite features was around 70%. Among faint features, oral changes were the most frequently presented (23%) while other features were less frequently observed (15–16%).
The median number (IQR) of d- and f-Features at admission was 1 (0–1) and 1 (1–2), respectively (Figure 5). Two days after admission (5 (4–5) day of illness), the number of d-Features increased to 4 (3–5), and the number of t-Features of increased to 5 (4–5). At this time point, the proportions of all d-Features were around 70% (Figure 4). Oral changes were the most frequently observed f-Feature (23%), and the prevalence of the other features was 15–16%. Due to this increased number of features, KD diagnoses were established and treatments for KD were commenced. IVIG treatments were effective, but 19 patients (31%) needed an additional IVIG treatment. Only one patient developed CAAs at one month of illness; a 2-year-old boy was initiated IVIG treatment on the fourth day of illness. After a re-emerged fever subsided after the second IVIG, a small aneurysm developed and was still observed at one month of illness; it regressed by the sixth month of illness.
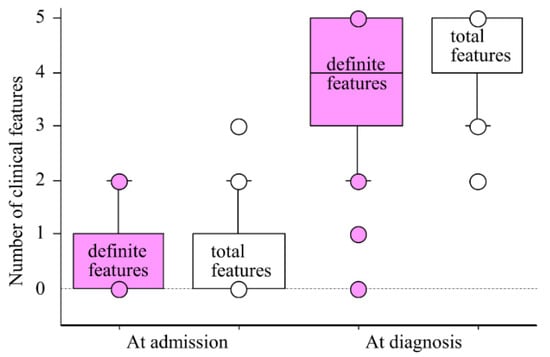
Figure 5.
Number of clinical features at admission and diagnosis. The number of clinical features at admission were minimal (definite features, 1 (0–1); total features, 1 (1–2)). Two days later, the number increased and diagnoses of Kawasaki disease were established (definite features,4 (3–5); total features, 5 (4–5)). Number of features are expressed as the median (interquartile ranges).
3.3. Diagnostic Process of Kawasaki Disease
Thirty-two patients (52%) presented with fever and four or five d-Features, and KD diagnoses were easily established. Although the remaining 30 patients, (48%) presented with ≤3 d-Features; experienced doctors decided to commence KD treatments. The initial diagnoses of these 30 patients were cervical lymphadenitis (n = 12, 40%), RTI (n = 8, 27%), UFI (n = 8, 27%), and UTI (n = 2, 7%). Figure 6 shows the clinical features of these 30 patients at diagnosis. d-Features accounted for approximately 40% of features, and cervical lymphadenopathy was the most common (63%). For f-Features, the proportion of oral changes was the highest (43%) among that of other f-Features (23–33%). Considering these f-Features, four or five t-Features were observed in 14 patients with three d-Features, seven patients with two d-Features, and one patient with one d-feature (Table 2). In total, experienced doctors diagnosed 22 patients with KD and commenced IVIG. Four patients presented with three t-Features, and experienced doctors diagnosed them with incomplete KD and decided to commence KD treatments. Among the four patients with two t-Features, two patients showed a small aneurysm on the eighth or 10th day of illness, and they were treated with IVIG and their coronary arteries normalized by the first month of illness. In the remaining two patients, one patient showed PB on the fifth day of illness, and the other patient did not show any abnormal echocardiographic findings. The experienced doctors decided to commence KD treatment by considering the patients’ clinical courses, and the treatments were effective.
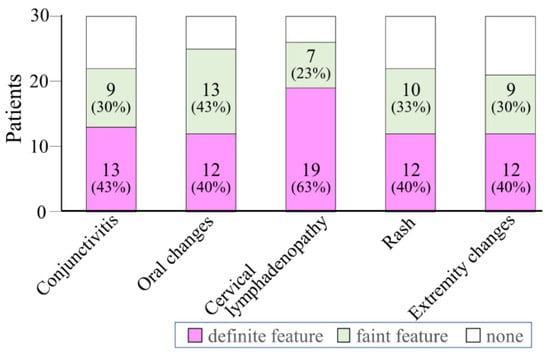
Figure 6.
Proportion of clinical features in patients who presented with ≤3 definite features at diagnosis. Among 30 patients who presented with ≤3 definite features at diagnosis, cervical lymphadenopathy accounted for 63% of definite features, whereas other features accounted for around 40%. Oral changes account for 43% of faint features, whereas conjunctivitis, rash, or extremity changes accounted for around 30%.

Table 2.
Diagnostic process for 30 patients with three or fewer definite features at diagnosis.
3.4. Usefulness of Echocardiographic Findings
Results of the examination of usefulness of echocardiographic findings are shown in Table 2. PBs were identified in 16 of the 30 patients with ≤3 d-Features. Coronary artery findings of 15 patients with two or three t-Features were especially useful in their diagnostic process as the findings of PB in seven patients (47%) helped to diagnose KD. Among eight patients with two or three t-Features, a small aneurysm was identified in two patients and PB was identified in four patients. In total, abnormal echocardiographic findings were identified in six patients (75%). There were four patients who presented with ≤1 d-Features, and all of them had abnormal echocardiographic findings (a small aneurysm and three PBs).
3.5. Usefulness of the iKD-Algorithm
Thirty patients presented with ≤3 d-Features on the day KD treatments were initiated (fifth day of illness). Of these, 14 patients were infants and 13 were diagnosed with KD within the fifth day of illness. The remaining infant was diagnosed on the eighth day of illness. Of 16 children, three patients were diagnosed before the fifth day of illness and 13 were diagnosed on the fifth day of illness or later. Therefore, 14 patients (47%, an infant and 13 children) among 30 patients with ≤3 d-Features at diagnosis met the fever duration criterion of the iKD-algorithm.
The usefulness of the iKD-algorithm was examined among above 30 patients. A small aneurysm was observed in two children (eighth and tenth day of illness), one infant showed four abnormal laboratory findings (eighth day of illness), and four children showed three abnormal laboratory findings (one patient in the fourth day of illness, two in the fifth illness day, and one in the sixth illness day). Without considering their duration of fever, the iKD-algorithm recommended KD treatment for seven patients. Therefore, the sensitivity of the iKD-algorithm was 23%. When we examine the sensitivity among 14 patients who met the criterion of fever duration for the iKD-algorithm, it increased to 43%.
4. Discussion
The diagnosis of incomplete KD should be considered in any infants or children with prolonged unexplained fever and ≤3 principal clinical features [2]. However, diagnosing KD in patients with incomplete presentation is not easy. In the present study, 16% of total KD patients were difficult diagnose as having KD at admission. They were diagnosed with infectious diseases and treated with antibiotics as their initial treatments. It has been known that the presence of fever and pyuria in an infant or young child can be mistakenly attributed to a UTI [2]. Patients with cervical lymphadenopathy as the primary clinical manifestation can be misdiagnosed as having bacterial adenitis [2]. These misdiagnoses were associated with their age as diagnoses of UTI were observed in early infants, those of UFI were mainly observed in infants, and those of cervical lymphadenitis were mainly observed in patients ≥1 year old. These patterns may facilitate adequate diagnoses of KD in patients who showed persistent fever against antibiotics treatments.
Two days after the initiation of antibiotic treatments, 32 patients presented with ≥4 d-Features and KD diagnoses were easily established. For the remaining 30 patients presented with ≤3 d-Features, KD diagnoses were not established by the young doctors, but the experienced doctors decided to commence KD treatments. Such incomplete presentation of KD is a risk for delayed diagnosis and the development of CAAs [2]. In the present study, only three patients received delayed treatment (after the seventh day of illness), but none of them had CAAs at one month of illness. The diagnostic process of these patients showed that sufficient clinical experience is essential for KD patients presenting with limited and/or faint clinical features. Thirty patients with ≤3 d-Features were diagnosed on the fifth day of illness. Therefore, only a few days were left in these patients to avoid delayed diagnoses. Without the efforts of experienced doctors, delayed diagnoses would have occurred and CAAs would have developed in some patients.
At diagnosis, oral changes were the most frequent f-Features identified by the experienced doctors (Figure 5). Minich et al. [7] have reported that patients with iKD, particularly those <6 months of age and those lacking eye or oral mucosal changes, may experience significant delays in diagnosis. From our results and those of Minich et al. [7], checking for oral changes in patients with other clinical features is crucial in the diagnosis of KD.
For the diagnosis of iKD, Yellen et al. [5] reported the usefulness of the iKD-algorithm. Of the patients to whom the iKD-algorithm was applied, 97% were referred for IVIG treatment. In the present study, the iKD-algorithm was not sufficiently useful (sensitivity was 23%). The median day of illness when the algorithms were applied was also different between studies; five days in the present study compared to six to eight in Yellen’s study. Early application of the algorithm reduced its sensitivity in the present study; thus, it is natural that the sensitivity increased in patients who met the criterion of fever duration, and the iKD-algorithm may help us in the diagnostic process regardless of the day of illness at application. Laboratory and echocardiographic findings in the iKD-algorithm may be useful in the diagnostic process of KD in Japan. Echocardiographic findings are particularly useful in the present study as coronary artery dilatation resulted in the diagnosis of KD in two patients. Although they presented with two d-Features, IVIG was initiated, and this timing of treatment resulted in the regression of their coronary arterial dilatations by one month of illness. Additionally, PB was suggested as a useful diagnostic sign of incomplete presentation of KD in the 2004 AHA diagnostic guideline [4]. However, Yu et al. [8] did not confirm the utility of PB, and Rabinowitz et al. [9] reported similar results. In the present study, among patients with ≤3 d-Features, two patients showed a small aneurysm and 17 patients showed PB. Particularly, among eight patients with ≤3 t-Features, a small aneurysm was identified in two patients and PB was identified in four patients. In total, abnormal echocardiographic findings were identified in six patients (75%). The echocardiographic findings of the coronary arteries helped in the diagnosing of KD. Through these results, we hypothesized that PB could be used as a complementary finding for the diagnosis of KD in some patients, especially those with limited and faint clinical features.
5. Limitations
One of the limitations of present study was that the examined findings were not objective. Since KD is diagnosed based on clinical principal features, subjective factors must be included. Furthermore, each symptom is categorized subjectively, possibly causing issues concerning subjectively. The evaluation of PB is also subjective. However, this is a single-center study and was evaluated by two experienced doctors; therefore, we believe that the subjective evaluations were reliable and the results of patients with limited and faint features would aid in the diagnostic process of KD.
In Japan, many KD infants and young children are admitted earlier than in other countries; hence, the course of illness in Japanese KD patients is different from that in KD patients in other countries. However, information on the relationship between age, admission day of illness, and diagnosis, as well as information on clinical features that were easily unrecognized must be valuable for junior doctors in Japan and other countries.
6. Conclusions
Diagnosing KD is difficult in some patients during the early phage of KD. To establish a diagnosis of KD, recognizing f-Features, correctly evaluating faint coronary artery findings, and, finally, making timely treatment decisions are necessary. These sufficient clinical experiences are essential. For junior doctors, educational programs on how to recognize f-Features, especially oral changes, and evaluate faint abnormal coronary artery findings are necessary to complement clinical experience is necessary. Although the iKD-algorithm was not sufficiently useful in Japan, its laboratory and echocardiographic findings may be helpful in the general diagnostic process of KD.
Author Contributions
Y.N. designed the study and drafted the manuscript; Y.M. and K.M. designed the study and collected and analyzed data and critically reviewed the manuscript; Y.K., N.N., H.I., M.H. and R.K. collected data and critically reviewed the manuscript; K.S. checked the study design and critically reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study received no external funding.
Institutional Review Board Statement
This study was approved by the Ethical Board of Kagoshima City Hospital, Kagoshima, Japan (22 January 2020, No. 2019-60).
Informed Consent Statement
The information of the study is shown at the Homepage of Kagoshima City Hospital to provide a means to opt out.
Conflicts of Interest
The authors declare no conflict of interest.
References
- JCS Joint Working Group. Guidelines for diagnosis and management of cardiovascular sequelae in Kawasaki disease (JCS 2013). Circ. J. 2014, 78, 2521–2562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCrindle, B.W.; Rowley, A.H.; Newburger, J.W.; Burns, J.C.; Bolger, A.F.; Gewitz, M.; Baker, A.L.; Jackson, M.A.; Takahashi, M.; Shah, P.B.; et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals from the American Heart Association. Circulation 2017, 135, e927–e999. [Google Scholar] [CrossRef] [PubMed]
- Roweley, A.H.; Shulman, S.T. Kawasaki disease. In Textbook of Pediatrics, 18th ed.; Kliegman, R.M., Behrman, R.E., Jenson, H.B., Stanton, B.F., Eds.; PWB Saunders: Philadelphia, PA, USA, 2007; pp. 1036–1042. [Google Scholar]
- Newburger, J.W.; Takahashi, M.; Gerber, M.A.; Gewitz, M.H.; Tani, L.Y.; Burns, J.C.; Shulman, S.T.; Bolger, A.F.; Ferrieri, P.; Baltimore, R.S.; et al. Diagnosis, treatment, and long-term management of Kawasaki disease: A statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 2004, 110, 2747–2771. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yellen, E.S.; Gauvreau, K.; Takahashi, M.; Burns, J.C.; Shulman, S.; Baker, A.L.; Innocentini, N.; Zambetti, C.; Pancheri, J.M.; Ostrow, A.; et al. Performance of 2004 American Heart Association recommendations for treatment of Kawasaki disease. Pediatrics 2010, 125, e234–e241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kobayashi, T.; Fuse, S.; Sakamoto, N.; Mikami, M.; Ogawa, S.; Hamaoka, K.; Arakaki, Y.; Nakamura, T.; Nagasawa, H.; Kato, T.; et al. A new Z score curve of the coronary arterial internal diameter using the lambda-mu-sigma method in a pediatric population. J. Am. Soc. Echocardiogr. 2016, 29, 794–801.e29. [Google Scholar] [CrossRef] [PubMed]
- Minich, L.L.; Sleeper, L.A.; Atz, A.M.; McCrindle, B.W.; Lu, M.; Colan, S.D.; Printz, B.F.; Klein, G.L.; Sundel, R.P.; Takahashi, M.; et al. Pediatric Heart Network Investigators. Delayed diagnosis of Kawasaki disease: What are the risk factors? Pediatrics 2007, 120, e1434–e1440. [Google Scholar] [CrossRef]
- Yu, J.J.; Jang, W.S.; Ko, H.K.; Han, M.K.; Kim, Y.H.; Ko, J.K.; Park, I.S. Perivascular brightness of coronary arteries in Kawasaki disease. J. Pediatr. 2011, 159, 454–457.e1. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, E.J.; Rubin, L.G.; Desai, K.; Hayes, D.A.; Tugertimur, A.; Kwon, E.N.; Dhanantwari, P.; Misra, N.; Stoffels, G.; Blaufox, A.D.; et al. Examining the utility of coronary artery lack of tapering and perivascular brightness in incomplete Kawasaki disease. Pediatr. Cardiol. 2019, 40, 147–153. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).