Nutritional Intake in Hospitalized Patients Receiving Texture-Modified Diets: Preliminary Results from an Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. Settings
- (i)
- Soft diet: A balanced and normo-energetic diet consisting of semolina, blended proteins (fish, meat), vegetable cream soup—all composed of natural foods with smooth consistency (level 4 according to IDSSI)—and fruit mousse.
- (ii)
- Minced diet: A balanced and normo-energetic diet consisting of soup, chopped proteins (meat, fish, eggs), chopped vegetables, and stewed fruit. All foods have a chopped consistency (level 6 according to IDSSI).
- (iii)
- Standard diet: A balanced and normo-energetic diet consisting of pasta or rice, proteins (meat, fish, cheese, eggs), side dishes, and fruit.
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Demographic Data of Patients
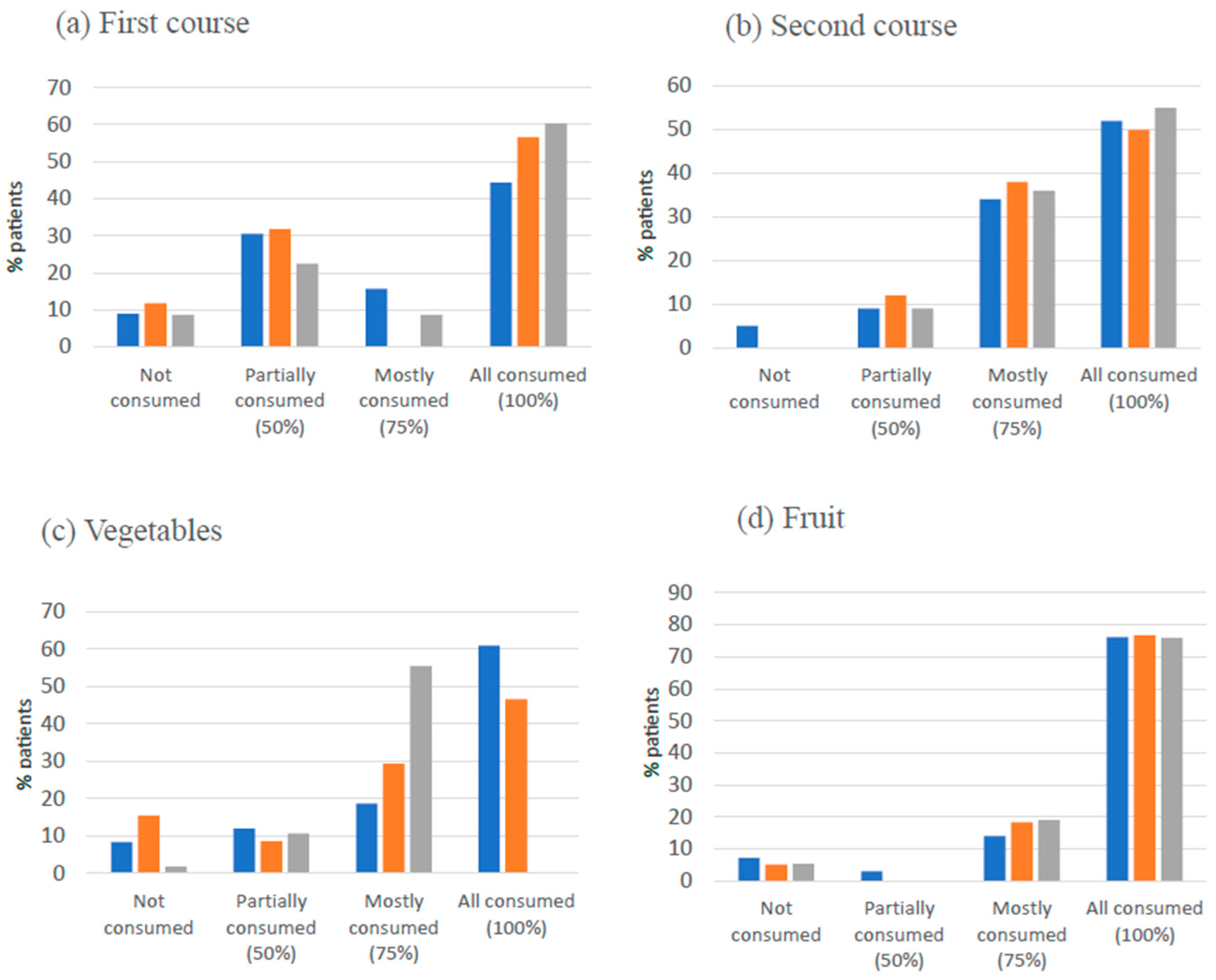
3.2. Patients’ Dietary Intake and Diet Type
3.3. Levels of Patients’ Satisfaction with Food Quality and Food Service
3.3.1. Satisfaction with Food Service
3.3.2. Satisfaction with Food Quality
- -
- Integrity (tray/plates/cutlery): standard: 92.3%, minced: 90.0%, soft: 93.1;
- -
- Breakfast smell (standard: 37.4%, minced: 40.0%, soft: 44.8%), breakfast temperature (standard: 72.3%, minced: 73.3%, soft: 77.6%), breakfast presentation (standard: 36.1%, minced: 46.7%, soft: 44.9%) and quantity provision of the breakfast (standard: 69.9%, minced: 63.3%, soft: 67.2%);
- -
- First course smell (standard: 37.9%, minced: 36.7%, soft: 25.9%), first course temperature (standard: 69.1%, minced: 68.3%, soft: 81.0%), cooking degree of the first course (standard: 41.7%, minced: 58.3%, soft: 55.2%);
- -
- Second course smell (standard: 31.9%, minced: 43.3%, soft: 32.7%), second course temperature (standard: 75.6%, minced: 73.3%, soft: 77.6%), cooking degree of the second course (standard: 49.4%, minced: 50.0%, soft: 55.2%), quantity of the second course (standard: 59.5%, minced: 60.0%, soft: 70.7%);
- -
- Vegetables smell (standard: 37.9%, minced: 33.3%, soft: 37.9%), temperature of the vegetables (standard: 72.9%, minced: 60.0%, soft: 76.8%), cooking degree of the vegetables (standard: 51.2%, minced: 46.7%, soft: 55.2%), quantity of the vegetables (standard: 56.0%, minced: 50.0%, soft: 67.2%).
3.3.3. Association Between the Different Diets and Food Quality Criteria
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
Abbreviations
| CI | Confidence intervals |
| IDDSI | International Dysphagia Diet Standardization Initiative |
| LARN | Reference Intake of Nutrients and Energy for the Italian Population |
| OR | Odds ratio |
| SD | Standard deviation |
| TMDs | Texture-modified diets |
References
- Wong, A.; Lin, H.; Chau, J.P.C. A Cost–Consequence Analysis of Nutritional Interventions Used in Hospital Settings for Older Adults with or at Risk of Malnutrition. Healthcare 2024, 12, 1041. [Google Scholar] [CrossRef] [PubMed]
- Rinninella, E.; Pizzoferrato, M.; Mele, M.C.; Cintoni, M.; Anselmi, G.; Caporossi, A.; Gasbarrini, A.; Costamagna, G.; Miggiano, G.A.D. COntrolling NUTritional Status (CONUT) as Predictive Score of Hospital Length of Stay (LOS) and Mortality: A Prospective Cohort Study in an Internal Medicine and Gastroenterology Unit in Italy. Nutrients 2023, 15, 1472. [Google Scholar] [CrossRef]
- Kaegi-Braun, N.; Frei, A.; Faessler, L.; Thomann, R.; Rasmussen, H.H.; Gomes, F.; Tribolet, P.; Bischoff, S.C.; Schuetz, P. Association of Nutritional Support With Clinical Outcomes Among Medical Inpatients Who Are Malnourished or at Nutritional Risk: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2033437. [Google Scholar] [CrossRef]
- Böhne, S.E.J.; Hiesmayr, M.; Sulz, I.; Tarantino, S.; Wirth, R.; Volkert, D. Recent and current low food intake-prevalence and associated factors in hospital patients from different medical specialities. Eur. J. Clin. Nutr. 2022, 76, 1440–1448. [Google Scholar] [CrossRef] [PubMed]
- Feng, H.Y.; Zhang, P.P.; Wang, X.W. Presbyphagia: Dysphagia in the elderly. World J. Clin. Cases 2023, 11, 2363–2373. [Google Scholar] [CrossRef]
- Mai, S.; Nan, Y.; Peng, L.; Wu, Y.; Chen, Q. Controlling nutritional status score in the prediction of cardiovascular disease prevalence, all-cause and cardiovascular mortality in chronic obstructive pulmonary disease population: NHANES 1999–2018. BMC Pulm. Med. 2024, 24, 356. [Google Scholar] [CrossRef]
- Edwards, J.S.; Hartwell, H.J. Hospital food service: A comparative analysis of systems and introducing the ‘Steamplicity’ concept. J. Hum. Nutr. Diet. 2006, 19, 421–430. [Google Scholar] [CrossRef]
- Osman, N.S.; Md Nor, N.; Md Sharif, M.S.; Hamid, S.B.A.; Rahamat, S. Hospital Food Service Strategies to Improve Food Intakes among Inpatients: A Systematic Review. Nutrients 2021, 13, 3649. [Google Scholar] [CrossRef]
- Bailey, R.L. Overview of dietary assessment methods for measuring intakes of foods, beverages, and dietary supplements in research studies. Curr. Opin. Biotechnol. 2021, 70, 91–96. [Google Scholar] [CrossRef]
- Rinninella, E.; Raoul, P.; Maccauro, V.; Cintoni, M.; Cambieri, A.; Fiore, A.; Zega, M.; Gasbarrini, A.; Mele, M.C. Hospital Services to Improve Nutritional Intake and Reduce Food Waste: A Systematic Review. Nutrients 2023, 15, 310. [Google Scholar] [CrossRef]
- Raheem, D.; Carrascosa, C.; Ramos, F.; Saraiva, A.; Raposo, A. Texture-Modified Food for Dysphagic Patients: A Comprehensive Review. Int. J. Environ. Res. Public Health 2021, 18, 5125. [Google Scholar] [CrossRef]
- Wu, X.S.; Miles, A.; Braakhuis, A. Nutritional Intake and Meal Composition of Patients Consuming Texture Modified Diets and Thickened Fluids: A Systematic Review and Meta-Analysis. Healthcare 2020, 8, 579. [Google Scholar] [CrossRef] [PubMed]
- Cichero, J.A.; Lam, P.; Steele, C.M.; Hanson, B.; Chen, J.; Dantas, R.O.; Duivestein, J.; Kayashita, J.; Lecko, C.; Murray, J.; et al. Development of International Terminology and Definitions for Texture-Modified Foods and Thickened Fluids Used in Dysphagia Management: The IDDSI Framework. Dysphagia 2017, 32, 293–314. [Google Scholar] [CrossRef]
- Razalli, N.H.; Cheah, C.F.; Mohammad, N.M.A.; Abdul Manaf, Z. Plate waste study among hospitalised patients receiving texture-modified diet. Nutr. Res. Pract. 2021, 15, 655–671. [Google Scholar] [CrossRef] [PubMed]
- Dahl, W.J.; Whiting, S.J.; Tyler, R.T. Protein content of puréed diets: Implications for planning. Can. J. Diet. Pract. Res. 2007, 68, 99–102. [Google Scholar] [CrossRef]
- Hadde, E.K.; Chen, J. Texture and texture assessment of thickened fluids and texture-modified food for dysphagia management. J. Texture Stud. 2021, 52, 4–15. [Google Scholar] [CrossRef]
- Naithani, S.; Whelan, K.; Thomas, J.; Gulliford, M.C.; Morgan, M. Hospital Inpatients’ Experiences of Access to Food: A Qualitative Interview and Observational Study. Health Expect. 2009, 12, 389–400. [Google Scholar] [CrossRef]
- Williams, P.; Walton, K. Plate Waste in Hospitals and Strategies for Change. e-SPEN Eur. e-J. Clin. Nutr. Metab. 2011, 6, e235–e241. [Google Scholar] [CrossRef]
- Mills, S.; Whitehead, K.A.; Jacob, C.J.; Williams, T. Hospital Food Service: A Comparative Analysis of System Performance and Patient Satisfaction in the UK and Australia. Nutr. Diet. 2018, 75, 264–271. [Google Scholar]
- Società Italiana di Nutrizione Umana. LARN. Livelli di Assunzione di Riferimento di Nutrienti ed Energia per la Popolazione Italiana. V Revisione; Biomedia: Singapore, 2024. [Google Scholar]
- Montgomery, R. Sample Size Justification in Feasibility Studies: Moving Beyond Published Guidance. Pilot Feasibility Stud. 2025, 11, 88. [Google Scholar] [CrossRef]
- Massoulard, A.; Bonnabau, H.; Gindre-Poulvelarie, L.; Baptistev, A.; Preux, P.M.; Villemonteix, C.; Javerliat, V.; Fraysse, J.L.; Desport, J.C. Analysis of the food consumption of 87 elderly nursing home residents, depending on food texture. J. Nutr. Health Aging 2011, 15, 192–195. [Google Scholar] [CrossRef]
- Dupertuis, Y.M.; Kossovsky, M.P.; Kyle, U.G.; Raguso, C.A.; Genton, L.; Pichard, C. Food intake in 1707 hospitalised patients: A prospective comprehensive hospital survey. Clin. Nutr. 2003, 22, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Pichard, C.; Lochs, H.; Pirlich, M. Disease-related malnutrition: An evidence-based approach to treatment. Clin. Nutr. 2008, 27, 577–584. [Google Scholar]
- Keller, H.H.; Carrier, N.; Duizer, L.; Lengyel, C.; Slaughter, S.; Steele, C. Making the Most of Mealtimes (M3): Grounding Mealtime Interventions with a Framework to Enhance Mealtime Experiences in Long-Term Care. J. Am. Med. Dir. Assoc. 2014, 15, 158–161. [Google Scholar] [CrossRef]
- Sieske, L.; Janssen, G.; Babel, N.; Volkert, D.; Wirth, R.; Pourhassan, M. Factors Associated with Food Intake in Hospitalized Older Adults: A Cross-Sectional Observational Study. Clin. Nutr. 2019, 38, 307–313. [Google Scholar]
- Shahar, S.; Chee, K.Y.; Wan Chik, W.C. Food intakes and preferences of hospitalised geriatric patients. BMC Geriatr. 2002, 2, 3. [Google Scholar] [CrossRef]
- Tamby Chik, C.; Adilah Zulkiply, N.; Bachok, S.; Mohi, Z.; Mohd Shahril, A. Plate waste in public hospitals foodservice management in Selangor, Malaysia. Indian. J. Sci. Technol. 2019, 11, 1–5. [Google Scholar]
- Schiffman, S.S.; Graham, B.G. Taste and smell perception affect appetite and immunity in the elderly. Eur. J. Clin. Nutr. 2000, 54, S54–S63. [Google Scholar] [CrossRef]
- Palese, A.; Grassetti, L.; Bressan, V.; Decaro, A.; Kasa, T.; Longobardi, M.; Hayter, M.; Watson, R. A path analysis on the direct and indirect effects of the unit environment on eating dependence among cognitively impaired nursing home residents. BMC Health Serv. Res. 2019, 19, 775. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.S.; Miles, A.; Braakhuis, A.J. Texture-Modified Diets, Nutritional Status and Mealtime Satisfaction: A Systematic Review. Healthcare 2021, 9, 624. [Google Scholar] [CrossRef]
- Carnevale, S.; Vitale, A.; Razzi, M.; Onori, C.; Cornacchia, G.; Grispo, O.; Corsinovi, E.; Rossi, L.; Spinetti, E.; Tosi, M.; et al. Non-Evidence-Based Dietary Restrictions in Hospital Nutrition and Their Impact on Malnutrition: A Narrative Review of International and National Guidelines. Dietetics 2024, 3, 568–587. [Google Scholar] [CrossRef]
| Energy (kcal) | |||||
| Diet type | First course | Second course | Vegetables | Fruit | Total |
| Standard | 440 | 115 | 60 | 90 | 705 |
| Soft | 360 | 115 | 30 | 90 | 595 |
| Minced | 350 | 115 | 60 | 90 | 585 |
| Protein (g) | |||||
| Diet Type | First course | Second course | Vegetables | Fruit | Total |
| Standard | 15 | 23 | 4 | <0.5 | 42 |
| Soft | 10 | 23 | 4 | <0.5 | 37 |
| Minced | 10 | 23 | 4 | <0.5 | 37 |
| First Course Mean ± SD | Second Course Mean ± SD | Vegetables Mean ± SD | Fruit Mean ± SD | Total * | ||
|---|---|---|---|---|---|---|
| Standard diet N = 168 | Energy (kcal) | 322.1 ± 144.1 | 84.4 ± 31.4 | 28.9 ± 14.6 | 75.4 ± 28.0 | 501.2 |
| Protein (g) | 10.7 ± 4.8 | 16.8 ± 6.3 | 2.9 ± 1.5 | tr. | 30.6 | |
| Minced diet N = 60 | Energy (kcal) | 283.9 ± 124.6 | 86.7 ± 33.7 | 24.5 ± 15.7 | 77.3 ± 25.0 | 454.2 |
| Protein (g) | 7.2 ± 2.9 | 17.3 ± 6.7 | 2.5 ± 1.6 | tr. | 26.0 | |
| Soft diet N = 58 | Energy (kcal) | 264.0 ± 99.0 | 92.2 ± 30.8 | 24.2 ± 11.9 | 76.8 ± 25.3 | 464.9 |
| Protein (g) | 7.5 ± 2.8 | 18.4 ± 6.2 | 2.4 ± 1.2 | tr. | 36.4 |
| Diet Type | Energy Requirements n (%) | Protein Requirements n (%) | ||||
|---|---|---|---|---|---|---|
| <513 kcal * | ≥513 kcal * | p-value | <30 g * | >30 g * | p-value | |
| Standard | 80 (47.6) | 88 (52.4) | >0.05 | 79 (47.1) | 89 (52.9) | >0.05 |
| Minced | 32 (53.3) | 28 (46.7) | 25 (43.1) | 33 (56.9) | ||
| Soft | 30 (51.7) | 28 (48.3) | 34 (56.7) | 26 (43.3) | ||
| Contributing Factors | Standard Diet | Minced Diet | Soft Diet | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Breakfast—smell ≤Suff. vs. ≥Good | 0.82 (0.49–1.38) | 0.45 | 0.75 (0.43–1.31) | 0.31 | 0.88 (0.51–1.55) | 0.67 |
| Breakfast—temperature ≤Suff. vs. ≥Good | 1.23 (0.43–3.53) | 0.69 | 1.38 (0.48–3.99) | 0.55 | 1.39 (0.48–4.08) | 0.54 |
| Breakfast—palatability ≤Suff. vs. ≥Good | 2.12 (1.26–3.58) | <0.01 * | 2.22 (1.27–3.87) | <0.01 * | 2.03 (1.16–3.57) | <0.02 * |
| Breakfast—quantity ≤Suff. vs. ≥Good | 2.48 (1.24–4.97) | 0.01 * | 1.68 (0.77–3.65) | 0.19 | 2.56 (1.23–5.29) | <0.02 * |
| First course—smell ≤Suff. vs. ≥Good | 1.39 (0.49–1.84) | 0.46 | 1.01 (0.64–1.59) | 0.96 | 0.97 (0.61–1.53) | 0.91 |
| First course—cooking degree ≤Suff. vs. ≥Good | 0.95 (0.49–1.84) | 0.88 | 0.94 (0.58–1.52) | 0.80 | 0.86 (0.54–1.39) | 0.56 |
| First course—temperature ≤Suff. vs. ≥Good | 0.48 (0.14–1.72) | 0.26 | 0.31 (0.11–0.88) | 0.03 | 0.35 (0.12–1.03) | 0.06 |
| First course—palatability ≤Suff. vs. ≥Good | 1.36 (0.64–2.89) | 0.41 | 0.97 (0.64–1.49) | 0.91 | 1.08 (0.70–1.66) | 0.70 |
| First course—quantity ≤Suff. vs. ≥Good | 1.47 (0.71–3.06) | 0.29 | 1.13 (0.62–2.08) | 0.67 | 0.97 (0.52–1.79) | 0.93 |
| Second course—smell ≤Suff. vs. ≥Good | 1.95 (0.75–5.08) | 0.17 | 1.00 (0.65–1.56) | 0.98 | 1.34 (0.86–2.09) | 0.18 |
| Second course—degree cooking ≤Suff. vs. ≥Good | 0.62 (0.27–1.46) | 0.28 | 0.71 (0.41–1.23) | 0.23 | 0.67 (0.39–1.15) | 0.15 |
| Second course—temperature ≤Suff. vs. ≥Good | 0.84 (0.26–2.61) | 0.76 | 1.28 (0.51–3.21) | 0.59 | 1.22 (0.47–3.14) | 0.67 |
| Second course—palatability ≤Suff. vs. ≥Good | 0.69 (0.31–1.53) | 0.36 | 0.87 (0.57–1.32) | 0.52 | 0.76 (0.49–1.15) | 0.19 |
| Second course—quantity ≤Suff. vs. ≥Good | 0.87 (0.37–2.05) | 0.77 | 1.14 (0.61–2.15) | 0.67 | 0.97 (0.52–1.81) | 0.93 |
| Vegetables—smell ≤Suff. vs. ≥Good | 0.99 (0.41–2.41) | 0.99 | 1.03 (0.65–1.63) | 0.89 | 1.02 (0.65–1.61) | 0.92 |
| Vegetables—cooking degree ≤Suff. vs. ≥Good | 0.95 (0.39–2.34) | 0.91 | 1.12 (0.59–2.09) | 0.72 | 1.09 (0.57–2.06) | 0.79 |
| Vegetables—temperature ≤Suff. vs. ≥Good | 2.64 (0.52–13.48) | 0.24 | 1.13 (0.40–3.21) | 0.81 | 1.24 (0.42–3.68) | 0.68 |
| Vegetables palatability ≤Suff. vs. ≥Good | 1.16 (0.49–2.71) | 0.73 | 0.73 (0.48–1.11) | 0.14 | 0.80 (0.53–1.21) | 0.29 |
| Vegetables: quantity ≤Suff. vs. ≥Good | 1.42 (0.59–2.29) | 0.42 | 1.65 (0.79–3.43) | 0.18 | 1.53 (0.74–3.21) | 0.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raoul, P.C.; Cintoni, M.; De Rossi, C.; Leonardi, E.; Ribaudi, E.; Rinninella, E.; Giaquinto, A.; Nuzzo, C.; Gasbarrini, A.; Mele, M.C. Nutritional Intake in Hospitalized Patients Receiving Texture-Modified Diets: Preliminary Results from an Observational Study. Dietetics 2025, 4, 40. https://doi.org/10.3390/dietetics4030040
Raoul PC, Cintoni M, De Rossi C, Leonardi E, Ribaudi E, Rinninella E, Giaquinto A, Nuzzo C, Gasbarrini A, Mele MC. Nutritional Intake in Hospitalized Patients Receiving Texture-Modified Diets: Preliminary Results from an Observational Study. Dietetics. 2025; 4(3):40. https://doi.org/10.3390/dietetics4030040
Chicago/Turabian StyleRaoul, Pauline Celine, Marco Cintoni, Chiara De Rossi, Elena Leonardi, Eleonora Ribaudi, Emanuele Rinninella, Antonio Giaquinto, Carmen Nuzzo, Antonio Gasbarrini, and Maria Cristina Mele. 2025. "Nutritional Intake in Hospitalized Patients Receiving Texture-Modified Diets: Preliminary Results from an Observational Study" Dietetics 4, no. 3: 40. https://doi.org/10.3390/dietetics4030040
APA StyleRaoul, P. C., Cintoni, M., De Rossi, C., Leonardi, E., Ribaudi, E., Rinninella, E., Giaquinto, A., Nuzzo, C., Gasbarrini, A., & Mele, M. C. (2025). Nutritional Intake in Hospitalized Patients Receiving Texture-Modified Diets: Preliminary Results from an Observational Study. Dietetics, 4(3), 40. https://doi.org/10.3390/dietetics4030040









