Abstract
Diet has long been identified as a major determinant of cardiovascular and other chronic diseases. In this study, we assess the relation between adherence to different dietary patterns and biochemical and metabolic parameters as well as the 10-year risk of major cardiovascular diseases (CVDs) in a community of blood donors in Northern Italy. We assess their adherence to four dietary patterns, namely, the Dietary Approach to Stop Hypertension (DASH) diet, the Mediterranean diet through the Greek and Italian Mediterranean Indices (GMI and IMI) and the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet, using a validated semi-quantitative food frequency questionnaire (FFQ). We then assess their association with blood parameters and the 10-year risk of major CVD using a spline regression model. We found an inverse association between the DASH and MIND diets and total and LDL cholesterol, and triglyceride and HDL cholesterol values for the Mediterranean diets (IMI and GMI). Additionally, according to our sex-stratified analyses, men who have greater adherence to dietary patterns have a decreased risk of major CVD for all patterns. The results suggest that greater adherence to dietary patterns positively influences blood biochemical and metabolic parameters, thus reducing the risk of developing cardiovascular disease and delaying the use of drug treatments.
1. Introduction
Cardiovascular diseases (CVDs) are a group of disorders of the heart and blood vessels and include coronary heart disease, cerebrovascular disease (ischemic and hemorrhagic stroke) and other conditions. More than four out of five CVD deaths are due to heart attacks and strokes, and one-third of these deaths occur prematurely in people under 70 years of age [1]. CVD remains the leading cause of mortality in industrialized countries and is rapidly becoming a primary cause of death worldwide. To prevent CVD, it is critical to identify proper public health interventions. High sodium and low potassium intakes are associated with increased blood pressure levels and risk of CVD. Thus, the evaluation of eating habits helps to assess intake and adherence to healthy diet recommendations as an important lifestyle factor to reduce the risk of developing CVD and other chronic diseases [2,3,4,5,6,7]. Dietary changes are considered the most effective and critical intervention [8,9,10].
The most frequent cause of ischemic heart disease is the process of atherosclerosis. Changing lifestyle habits is one of the first strategies to overcoming atherosclerosis, mainly focusing on a healthy diet [11]. It has been shown that high cholesterol levels and hypertension are often correlated [12], and it has been demonstrated that the simultaneous treatment of both can improve the individual cardiovascular risk profile [13].
At least three-quarters of the world’s deaths from CVDs occur due to an unhealthy diet, physical inactivity, tobacco use, and harmful use of alcohol [1]. Inappropriate behavioral factors, such as a lack of physical activity and unhealthy dietary habits, are the leading causes of dyslipidemia characterized by high levels of triglycerides and Low-Density Lipoprotein (LDL) cholesterol and low levels of High-Density Lipoprotein (HDL) cholesterol, as well as increased blood pressure, hyperglycemia and overweight/obesity [14]. Therefore, it becomes essential to promote a healthy diet and a series of habits that generally lead to a healthy lifestyle [15,16].
The Mediterranean diet closely reflects the principles of healthy nutrition [17]. Indeed, it is a dietary pattern characterized by the high consumption of plant-based foods (cereals, fruits, vegetables, legumes, tree nuts, seeds and olives), with olive oil as the principal source of added fat, along with high to moderate intakes of fish and seafood; moderate consumption of eggs, poultry and dairy products (e.g., cheese and yogurt); low consumption of red meat and a moderate intake of alcohol, mainly wine during meals [18]. For these reasons, it is considered an ideal diet for the achievement of a good state of health (e.g., reduced mortality) and for the prevention of chronic diseases [19], especially CVD, in high-income countries [18,20,21,22,23]. It contributes to significant reductions in the incidence and mortality of CVDs [24,25,26,27], neoplastic diseases [28,29] and neurodegenerative diseases; thus, it is associated with a significant improvement in health status [30,31].
In addition to the Mediterranean diet, another dietary pattern included in the WHO recommendations to reduce cardiovascular risk and hypertension is the Dietary Approaches to Stop Hypertension (DASH) diet. Initially conceived by the US National Heart, Lung and Blood Institute in the 90s, the DASH diet is the dietary regimen recommended to reduce hypertension and CVDs [32,33,34,35]. The DASH diet is comparable to the Mediterranean diet as it limits saturated fats (red meat, cheese, sweets) and high-sodium foods (a person with hypertension should not exceed 1500 mg per day), preferring instead vegetables, fruits, low-fat dairy products, cereals (preferably whole grain), fish, olive oil and nuts. Finally, the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet is a hybrid dietary regimen of the Mediterranean and DASH diets with selected modifications based on the most compelling evidence in the diet-dementia field [36,37,38,39]. It features the consumption of vegetables (particularly green leafy vegetables), berries, extra-virgin olive oil, nuts, whole grains and low-fat protein sources. Previous observational studies showed that greater adherence to the MIND diet was related to a lower cognitive decline [40,41,42] and recently also CVDs [43].
In this study, we investigate the relation between diet quality through adherence to different dietary patterns and blood biochemical and metabolic parameters in a ‘healthy’ Italian population to evaluate the possible preventive strategies to decrease their risk of developing CVDs.
2. Materials and Methods
2.1. Study Population and Procedures
We recruited healthy blood donors aged between 30 and 60 years without a history of chronic disease or cancer from the Reggio Emilia AUSL-IRCCS Transfusion Medicine Unit. Each participant was asked to complete a questionnaire concerning medical history and personal information [44]. We measured their height and weight to calculate body mass index (BMI) and systolic and diastolic blood pressure levels with a manual sphygmomanometer during the medical examination prior to blood donation. Subjects who declared they were currently smokers were excluded.
2.2. Dietary Assessment
We administered a detailed food frequency questionnaire (FFQ) using a validated semi-quantitative FFQ developed as part of the European Prospective Investigation in Cancer (EPIC) project. The version used was specifically validated for the population of Northern Italy [45,46]. The EPIC-FFQ was designed to estimate the intake of 188 food items over the previous year in terms of frequency and amount. Photos of portion sizes were also used to assist with proper completion of the questionnaire by participants. Foods and beverages were categorized into major food groups and subgroups based on the common EPIC-SOFT classification [47,48]. We also calculated scores for four diet quality patterns defined a priori, as previously described [49,50,51]. The DASH diet is based on 8 components: fruits, vegetables, nuts and legumes, low-fat dairy products and whole grains with a high intake yielding high DASH scores, and sodium, sweetened beverages, and red and processed meats with a low intake yielding high scores. Participants were classified into quintiles according to the intake of each component, then the component scores were summed to obtain the DASH score with an overall possible range of 8–40. The Greek Mediterranean Index (GMI) was based on the Mediterranean diet scale [52]. The GMI scoring was based on the intake of 9 items: vegetables, legumes, fruit and nuts, dairy products, cereals, meat and meat products, fish and alcohol. Participants were classified according to the intake above or below the median value: the range of possible scores is 0–9, with higher scores indicating greater adherence. The Italian Mediterranean Index (IMI) was developed by adapting the GMI to typical Italian eating behavior [25]. The score was based on the intake of 11 items: 6 specific Mediterranean foods or food groups (pasta; typical Mediterranean vegetables, such as raw tomatoes, leafy vegetables, onion and garlic, salad, and fruiting vegetables; fruit; legumes; olive oil and fish), 4 non-Mediterranean foods (soft drinks, butter, red meat and potatoes) and alcohol consumption. Participants were classified according to tertiles of intake of each component, and one point was given for consumption of each typical Mediterranean food in the upper tertile and for consumption of each non-Mediterranean food in the lower tertile; alcohol received 1 point for intake up to 12 g/day; abstainers and persons who consumed >12 g/day did not receive any points. The range of possible scores was 0–11 [50]. Finally, the MIND diet score was based on the intake of 15 items, namely, whole grains, green leafy and other vegetables, berries, red meat, poultry, fish, legumes, nuts, fast/fried food, olive oil and other fats, cheese, sweets and alcohol/wine. Scores ranged from 0 to 15, with higher scores representing greater adherence [49].
2.3. Blood Biochemical and Metabolic Parameter Measurements
We collected fasting blood samples in the morning at the Reggio Emilia AUSL-IRCCS Transfusion Medicine Unit. We analyzed them on collection day at the central AUSL-IRCCS laboratory. We assessed the following metabolic parameters using automated laboratory procedures as previously described [44]: complete blood count, including mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), red blood cell distribution width (RDW), reticulocyte count, platelet count (PLT), white blood cell or leukocyte count, hemoglobin (Hb), ferritin, blood glucose, alanine aminotransferase (ALT) and lipid profile (total cholesterol, HDL-cholesterol, triglycerides); creatinine; and total protein. In particular, we quantified the total cholesterol, HDL cholesterol, triglyceride and glucose levels using an AEROSET c8000 system (Abbott Diagnostic, IL, USA) [53]. We calculated levels of LDL cholesterol through the Friedewald formula. We used an Atellica® analyzer (Siemens Healthcare Diagnostic, NY, USA) to quantify TSH levels [54]. To determine ALT concentration, we used an automated enzymatic colorimetric assay [44]. Laboratory reference values for biochemical parameters are shown in Table S1. Finally, we collected a urine sample and excluded those with cotinine levels >30 μg/L, which was deemed inconsistent with a self-declared non-smoking status [55,56].
2.4. Risk of Major Cardiovascular Diseases
We evaluated cardiovascular risk using the Cardiovascular Risk Chart tool made available by the CUORE project of the National Italian Institute of Health [57]. Specifically, we used the online tool (https://www.cuore.iss.it/valutazione/calc-rischio, accessed on 30 April 2022) to estimate the 10-year risk of major CVDs through the values of certain individual factors: sex, age, systolic blood pressure levels, total and HDL cholesterol levels, presence of diabetes and smoking habits.
2.5. Data Analysis
Adherence to the investigated dietary patterns was determined through a previously developed routine from the amount and frequency of consumption of the individual components assessed through the FFQ [49,50]. We modeled the relation between adherence to the investigated dietary patterns and the biochemical and metabolic parameters using restricted cubic spline regression multivariable analysis with three knots at fixed cutpoints (10th, 50th and 90th percentiles) to evaluate the possible nonlinear association according to Harrell’s recommendations [58]. We used a multivariable model adjusted for the following variables: age, sex, BMI, urinary cotinine, alcohol intake, fiber intake and total energy intake. Similarly, we assessed the relation between adherence to dietary patterns and the 10-year risk of major cardiovascular events using the same spline regression analysis with three knots at fixed cutpoints and using a multivariable model adjusted as before but excluding sex, which is already included in the 10-year CVD risk calculation. We used STATA-SE statistical software (Version 17.0, Stata Corp., College Station, TX, USA, 2021) for all data processing and analysis, using ‘mkspline’ and ‘xbrcsplinei’ commands.
3. Results
3.1. Characteristics of the Study Population
We recruited 148 subjects; after excluding four individuals who did not provide informed consent and a further seven individuals who were current smokers based on cotinine levels ≥30 µg/L, our population eventually comprised 137 healthy blood donors, 62 men and 75 women, whose main characteristics are summarized in Table 1. The mean age was 47.4 (46.8 for men/47.9 for women). The age distribution shows that 58.4% of recruited subjects were <50 years and 41.6% were ≥50; we observed a predominance of men under the age of 50 years (62.9% of men compared to 54.7% of women) and a predominance of women over 50 years of age (37.1% vs. 45.3%). Regarding BMI, half of the participants were a normal weight (54.0%), 36.5% overweight and 9.5% obese. Women showed slightly higher values than men regarding the percentage of normal weight (56% versus 51.6%) and lower for overweight (30.7% versus 43.6%). However, women accounted for more than double the percentage of obese subjects (13.3% versus 4.8%). In our sample of 137 individuals, 101 were never smokers and 36 were former smokers, of which 17 were men and 19 were women. The mean count of years of smoking for former smokers was 12.7 (SD 10.4), and the mean count of years since quitting smoking was 17.6 (SD 11.2). In general, similar values for smoking habits were observed for both sexes. The highest educational level was a high-school diploma or more in 84% of subjects (48.2% high-school diploma and 35.8% college or more, respectively), while the remainder were educated at middle and primary school levels. Lastly, the occupations with the highest percentages were clerical support workers (31.4%), professionals (19%) and technicians/associate professionals (15.3%); all other occupations were below 10%, including managers (6.6%), service and sales workers (8%), craft and related trades workers (7.3%), plant and machine operators (8%) and elementary occupations (4.4%).

Table 1.
Characteristics of the study population. Values are numbers and percentages (%) when not otherwise reported.
3.2. Blood Biochemical and Metabolic Parameters
Table 2 presents the median and interquartile range of blood biochemical and metabolic parameters according to sex. The complete blood count shows all the parameters examined within the reference values; blood glucose shows a median value of 86 mg/dL with 81–91 of IQR; all parameters show minimal differences between the two sexes. Total cholesterol of the entire sample recorded a median value of 204 mg/dL (slightly above the maximum recommended value of 200 mg/dL) with values referring to the first and third quartiles of 184 and 224 mg/dL, respectively. In particular, women showed higher values than men: 210 versus 192 mg/dL. The median value of HDL cholesterol was 59 mg/dL in the whole sample: 52 for men and 67 mg/dL for women.

Table 2.
The median and interquartile range of dietary pattern and blood biochemical and metabolic parameters.
Both results are above the recommended values of 50 mg/dL, while a median LDL cholesterol value of 123.9 mg/dL was found in the whole sample, which is slightly above the recommended mean of 120 mg/dL. In both sexes, LDL cholesterol levels were in the normal range for the first quartile, while the levels were different for the third quartile (141.80 mg/dL for men and 145.80 mg/dL for women). Triglyceride levels had a median value of 78 mg/dL, completely in the range of normal values. Ferritin had a median value of 36.39 ng/mL; thus, in the normal range, men showed higher levels than women (47.43 ng/mL vs. 30.37 ng/mL). All other parameters showed values within the normal ranges with no substantial differences shown by the sex-stratified analysis.
3.3. Dietary Habits
The intake of foods divided into the main categories is presented in Table S2. The overall mean energy intake was 2039 Kcal/day, higher in men than in women (2190 Kcal/day and 1915 Kcal/day). The mean intake of specific food categories was similar in both sexes, except for the slightly lower consumption by women of cereal products (240.2 g/day vs. 190.7 g/day), bread and rolls (108.0 g/day vs. 77.9 g/day), meat (88.0 g/day vs. 59.5 g/day) and beverages (mainly due to wine: 132.8 g/day vs. 56.8 g/day). In comparison, men had a lower consumption of milk and dairy products (167.2 g/day vs. 191.0 g/day), coffee and tea (126.5 g/day vs. 139.1 g/day) and a slightly lower intake of vegetables (145.3 g/day vs. 180.4 g/day).
In Table 3, we present the distribution of adherence to dietary patterns. In relation to the DASH diet, we found a median adherence value of 24 (IQR: 21–28). For the GMI, the median adherence value was 4 (IQR: 3–6) with a substantially identical score (median 4, IQR: 3–5) for the IMI. For the MIND diet, the median adherence value was 7.5 (IQR: 6.5–8.5). We found a comparable score for adherence to dietary patterns in both sexes, except for the higher score in women than men (27 versus 22) for the DASH diet. Figure S1 reports the spline regression analysis for the correlation between the indices of adherence to dietary patterns. All the indices investigated were positive and almost linearly correlated with each other.

Table 3.
The median and interquartile range of dietary pattern adherence in the study population. Data are median (50th) and interquartile range (IQR).
3.4. Spline Regression Analysis between Dietary Pattern and Biochemical and Metabolic Parameters
The spline regression analysis for the associations between adherence to dietary patterns and blood cell counts and biochemistry is reported in Figures S2–S5. Red blood cell count, hemoglobin and hematocrit were almost entirely inversely correlated with all dietary patterns. There was an inverted U-shaped relation between platelets and DASH (direct association up to a score of 25, inverse above that) and MIND (slight direct association up to the score of 8, inverse above that). In contrast, null associations emerged between the GMI and IMI, though for the latter an inverse relation was observed for scores above eight.
No substantial differences emerged in the analysis stratified by sex (Figures S6–S21) with some exceptions. For the DASH diet, the relation with hemoglobin was almost linear, while in men it decreased above high levels of adherence (>25) only. In addition, the inverted U-shaped relation between DASH and platelets was confirmed in men, while a linear increase can be noted in women (Figures S6 and S7).
The spline regression analysis for the association between adherence to dietary patterns and metabolic parameters is presented in Figure 1, Figure 2, Figure 3 and Figure 4. For glycemia, no substantial association was found for any of the patterns, while total cholesterol showed an inverse association for scores above median values for DASH (≥25), GMI (≥4) and IMI (≥4). Conversely, an inverse linear association emerged for the MIND diet. HDL cholesterol was found to be directly associated, almost linearly, with increasing scores of the DASH diet and the IMI. At the same time, the relation was almost null for the GMI and U-shaped for the MIND diet, slightly decreasing at below-median adherence and again increasing for scores above it. For LDL cholesterol, we found comparable results for all dietary patterns with inverse associations, especially for scores indicating high adherence, except for the DASH diet, with a slight but imprecise increase up to the median score (25), after which they started to decrease. Similarly for triglyceride levels, we found an almost inverse association for the IMI and MIND diet but null with the GMI and comparable to the shape of LDL cholesterol for the DASH diet. ALT showed a U-shaped association with the DASH diet (inverse up to a score of 25 and direct above that). Likewise, for the GMI diet, an increase in ALT was noted but only for high scores (≥4), while both the MIND diet and the IMI showed an almost null association. TSH showed an inverse relation with the DASH and MIND diets, while the relation was almost null with a slight decrease for high adherence scores for the GMI and U-shaped for the IMI with the median value (4) being the turning point of the curve. Creatinine showed a U-shaped relation with the DASH and IMI diets, with an inverse relation up to median adherence values. Conversely, the GMI was inversely associated, while the MIND diet had an almost null association. Ferritin showed a nearly linear direct association with all patterns except for the GMI, the latter demonstrating a null relation. In addition, a plateau was reached at a higher adherence score for the DASH diet. Total protein levels showed inverse associations with all dietary patterns, especially at high adherence scores for the MIND diet, while the effects seemed to wane for the DASH diet.
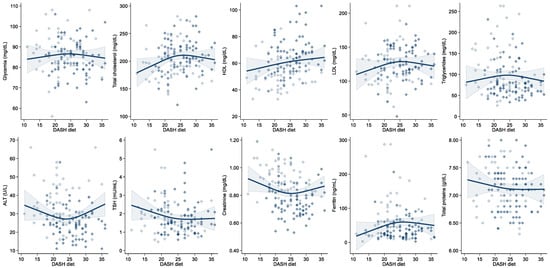
Figure 1.
Spline regression analysis of the association between adherence to the Dietary Approaches to Stop Hypertension (DASH) diet and levels of metabolic parameters in the study population. Hollow and solid diamonds indicate men and women, respectively. Solid line indicates multivariable analysis adjusted for age, sex, body mass index, urinary cotinine, alcohol intake, fiber intake and total energy intake, while shaded area represents confidence interval with upper and lower limits.
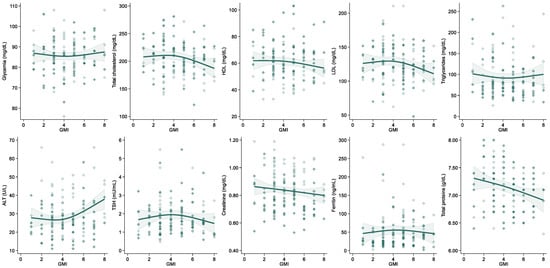
Figure 2.
Spline regression analysis of the association between adherence to the Greek Mediterranean Index (GMI) and levels of metabolic parameters in the study population. Hollow and solid diamonds indicate men and women, respectively. Solid line indicates multivariable analysis adjusted for age, sex, body mass index, urinary cotinine, alcohol intake, fiber intake and total energy intake, while shaded area represents confidence interval with upper and lower limits.
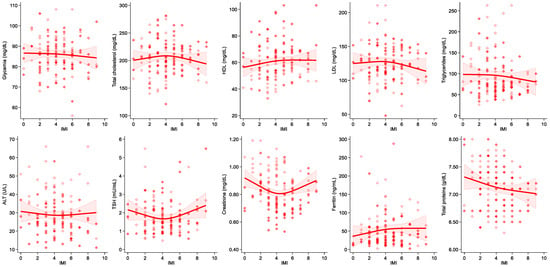
Figure 3.
Spline regression analysis of the association between adherence to the Italian Mediterranean Index (IMI) and levels of metabolic parameters in the study population. Hollow and solid diamonds indicate men and women, respectively. Solid line indicates multivariable analysis adjusted for age, sex, body mass index, urinary cotinine, alcohol intake, fiber intake and total energy intake, while shaded area represents confidence interval with upper and lower limits.
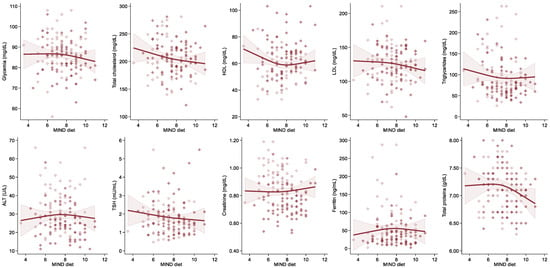
Figure 4.
Spline regression analysis of the association between adherence to the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet and levels of metabolic parameters in the study population. Hollow and solid diamonds indicate men and women, respectively. Solid line indicates multivariable analysis adjusted for age, sex, body mass index, urinary cotinine, alcohol intake, fiber intake and total energy intake, while shaded area represents confidence interval with upper and lower limits.
Sex-stratified analyses are presented in Figures S14–S21, indicating overall similar trends compared to the entire sample. The direct association between DASH and HDL-cholesterol was steeper in women than men, while the association with triglyceride levels was inverse in women for values >25 (Figures S14 and S15). Additionally, the U-shaped relation between the DASH diet and IMI and creatinine was confirmed in women, while a linear decrease was found in men (Figures S14, S15, S18 and S19). The inverse relation between the MIND diet and triglyceride levels was steeper in women, while almost null in men. Finally, for blood glucose we found a null association in men but an inverse one in women (Figures S20 and S21).
3.5. Risk of Major Cardiovascular Events and Association with Dietary Pattern
Overall, the median 10-year risk of major cardiovascular events in the whole population is 1% (IQR: 0.5–1.7%), more than double in men compared to women (1.7%, IQR 1.1–3.0% versus 0.6%, IQR 0.4–0.9%, respectively). The spline regression analysis performed on the overall subjects showed an inverse relation between the DASH and MIND diets and the 10-year risk of major CVDs, while the relation seems null for both the GMI and IMI (Figure 5). Conversely, in the sex-stratified analysis, an inverse relation between all dietary patterns with CVD risk can be observed in men, but only at high levels of adherence (Figure S22). In contrast, the inverse relation in women is comparable, though not as strong as in the overall population (Figure S23).
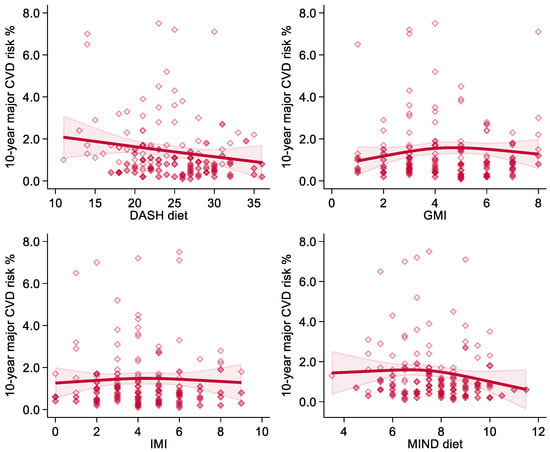
Figure 5.
Spline regression analysis of the association between adherence to dietary patterns (Dietary Approaches to Stop Hypertension-DASH diet; Greek Mediterranean Index-GMI; Italian Mediterranean Index-IMI; Mediterranean-DASH Intervention for Neurodegenerative Delay-MIND diet) and the 10-year risk of major cardiovascular events (10-year CVD risk) in the overall population. Hollow and solid diamonds indicate men and women, respectively. Solid line indicates spline analysis. Shaded area represents confidence interval with upper and lower limits.
4. Discussion
Several foods and nutrients have been linked to CVDs, but their effects may be best investigated by considering the overall dietary habits of individuals. Thus, we investigated the association between adherence to four a priori-defined dietary patterns [25] and biochemical and metabolic factors linked to the risk of CVDs, especially the lipid profile.
In this study, we found that the investigated population had an overall medium to moderate adherence to the IMI and GMI as 50% of the study subjects scored four points in accordance with other studies conducted on populations from the same area [59]. These levels of adherence are in line with what has previously been described in other populations residing in the same geographical area [60]. In particular, our results are comparable with what has been described by studies conducted on other European populations [52], according to the greater adherence found in women compared to men. Additionally, our study shows a good adherence to the DASH dietary pattern with 50% of subjects scoring between 21 and 28 points, also in line with previous studies [60]. The same can be observed for the MIND diet, which showed a medium adherence rate with 50% of subjects scoring between 6.5 and 8.5 points, substantially comparable with a previous Italian study [49], but slightly higher compared to studies carried out on American populations [41,42].
In our study, we observed positive and almost linear associations between the adherence to the four dietary patterns. Nonetheless, some differences emerged in their relation with biochemical parameters. Such discrepancies may be explained by the specific features of the DASH and MIND diets, namely, the low intake of sodium and of saturated fats, also characterizing the Mediterranean diet but not specifically recommended as in the other dietary regimens for the prevention of CVDs [35]. The increased adherence to the Mediterranean diet was associated with decreased total and LDL cholesterol levels and is in line with several studies indicating a 2% reduction in total cholesterol and a 1% reduction in LDL cholesterol [61,62,63]. For HDL cholesterol and triglyceride values, our study showed a direct correlation with increasing adherence to the Mediterranean pattern (IMI and GMI), in line with what has been observed in previous studies [61,63,64,65]. On the contrary, the increased adherence to the DASH diet showed a substantially null effect on HDL cholesterol levels, in line with previous evidence [61,66,67]. However, a positive impact of the DASH diet on both total and HDL cholesterol has also been described [68]. In addition, in our study for the DASH diet we found a direct correlation between total cholesterol and an improvement in the LDL fraction in line with previous studies [32,64,66,69]. Finally, our results only partially confirmed the inverse association between the MIND diet and reduced levels of HDL cholesterol [70], as such a relation emerged only at high levels of adherence in our population.
Our findings agree with previous studies indicating that greater adherence to both measurements of the Mediterranean diet (IMI and GMI) has a slightly positive impact on CVDs compared with the DASH diet [61,65,66]. A greater adherence corresponds to a reduction in cardiovascular risk of about 19% [24]. Thus, correlations between adherence to dietary patterns and metabolic parameters showed that greater adherence to the DASH and MIND diets might be effective in controlling specific parameters, especially the lipid profile with total cholesterol and HDL and LDL cholesterol levels [68,70]; it has been shown how the DASH diet can affect the lipid profile and consequently cardiovascular risk [9,71,72] and reduce cardiovascular events only in subjects who adhere modestly or totally to the recommended dietary plan and lifestyle [15]. Therefore, those who do not comply fully with it maintain a very high cardiovascular risk [73]. Additionally, a recent study suggested that subjects with a high MIND diet score have 12% lower odds of having metabolic syndrome [70].
Regarding the 10-year risk of major CVDs, we found that most of the study subjects had a very low risk (<4%), with only a few participants demonstrating a higher risk (6–7%). In particular, it should be noted that the median values of total and LDL cholesterol (204 and 124 mg/dL) are slightly above the reference values (<200 and <120 mg/dL) with approximately half of the subjects having higher values, thus increasing their CVD risk, especially for the few with very high levels.
The spline regression analysis between dietary patterns and risk of major CVDs confirms the substantial beneficial effects in the overall population of higher adherence to healthy dietary patterns, including the DASH [35,67], Mediterranean [23,24] and MIND [43] diets. This finding is of particular interest since it has been found in a substantially healthy population with almost all metabolic values within the reference values. For this reason, we can hypothesize that additional and stronger beneficial effects could be achieved in subjects who are disease-affected or at higher risk of developing CVDs due to out-of-reference metabolic parameters.
The strengths of our study include the recruitment of a sample population from the Emilia-Romagna region having similar characteristics compared with previously investigated communities within the study area [74,75]. In addition, for the evaluation of dietary habits, we used a food questionnaire specifically validated for Northern Italy [76]. Although the dietary characteristics could be generally similar to those of other Italian populations, some distinctive characteristics may be present due to the regional differences that have been taken into account in the final version of the FFQ [77,78]. Another strength is that it was possible to perform stratified analyses to highlight possible sex-specific effects, as well as the minimal invasiveness of our study due to blood sampling that is already part of a programmed annual pathway, where the participants are donors of blood and derivatives [44]. In addition, recruitment was conducted over approximately two calendar years (March 2017 to April 2019), so distortionary effects due to the season in which the questionnaire was completed by participants could be partially ruled out, also because the EPIC questionnaire contains specific questions that focus on the seasonality of foods consumed, especially fruits and vegetables [79,80,81].
However, our study had limitations that should be mentioned. The study cross-sectional design did not allow a causal interpretation of results because the participants were recruited from the Reggio Emilia AUSL-IRCCS Transfusion Medicine Unit from among blood donors and it was not possible to exclude the presence of a volunteer bias. However, since the collection procedure did not add further invasive examinations to those already scheduled as part of the blood donation, this should have minimized the risk of selection bias for non-participation in the study. Finally, the sample size was relatively small, thus affecting the statistical precision of the estimates.
5. Conclusions
This study provided a direct association between greater adherence to the DASH and MIND diets and to a lesser extent to the GMI and IMI and levels of biochemical parameters. Such improvements in blood biochemical and metabolic parameters focus on the lipid profile of the related cardiovascular risk and possible implications for public health. The results suggest that it may be possible to modify and improve the lipid profile, reducing cardiovascular risk with a healthy and normal lifestyle, thus delaying the use of pharmacological treatments.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/dietetics1020010/s1, Table S1: Laboratory reference ranges for blood biochemical and metabolic parameters; Table S2: Mean and standard deviation of dietary intake of foods and beverages of the overall population and divided by sex. Values are expressed in g/day. Figure S1: Spline regression analysis of the associations between indices of adherence to the different dietary patterns in the study population. Hollow and solid diamonds indicate men and women, respectively (Dietary Approaches to Stop Hypertension-DASH diet; Greek Mediterranean Index-GMI; Italian Mediterranean Index-IMI; Mediterranean-DASH Intervention for Neurodegenerative Delay-MIND diet). Figure S2: Spline regression analysis of the associations between adherence to the Dietary Approaches to Stop Hypertension (DASH) diet and blood cell count and biochemistry in the study population. Hollow and solid diamonds indicate men and women, respectively. Figure S3: Spline regression analysis of the associations between adherence to the Greek Mediterranean Index (GMI) and blood cell count and biochemistry in the study population. Hollow and solid diamonds indicate men and women, respectively. Figure S4: Spline regression analysis of the associations between adherence to the Italian Mediterranean Index (IMI) and blood cell count and biochemistry in the study population. Hollow and solid diamonds indicate men and women, respectively. Figure S5: Spline regression analysis of the associations between adherence to the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet and blood cell count and biochemistry in the study population. Hollow and solid diamonds indicate men and women, respectively. Figure S6: Spline regression analysis of the association between adherence to the Dietary Approaches to Stop Hypertension (DASH) diet and blood cell count and biochemistry in men. Figure S7: Spline regression analysis of the association between adherence to the Dietary Approaches to Stop Hypertension (DASH) diet and blood cell count and biochemistry in women. Figure S8: Spline regression analysis of the association between adherence to the Greek Mediterranean Index (GMI) and blood cell count and biochemistry in men. Figure S9: Spline regression analysis of the association between adherence to the Greek Mediterranean Index (GMI) and blood cell count and biochemistry in women. Figure S10: Spline regression analysis of the association between adherence to the Italian Mediterranean Index (IMI) and blood cell count and biochemistry in men. Figure S11: Spline regression analysis of the association between adherence to the Italian Mediterranean Index (IMI) in women. Figure S12: Spline regression analysis of the association between adherence to the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet and blood cell count and biochemistry in men. Figure S13: Spline regression analysis of the association between adherence to the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet and blood cell count and biochemistry in women. Figure S14: Spline regression analysis of the association between adherence to the Dietary Approaches to Stop Hypertension (DASH) diet and levels of metabolic parameters in men. Figure S15: Spline regression analysis of the association between adherence to the Dietary Approaches to Stop Hypertension (DASH) diet and levels of metabolic parameters in women. Figure S16: Spline regression analysis of the association between adherence to the Greek Mediterranean Index (GMI) and levels of metabolic parameters in men. Figure S17: Spline regression analysis of the association between adherence to the Greek Mediterranean Index (GMI) and levels of metabolic parameters in women. Figure S18: Spline regression analysis of the association between adherence to the Italian Mediterranean Index (IMI) and levels of metabolic parameters in men. Figure S19: Spline regression analysis of the association between adherence to the Italian Mediterranean Index (IMI) and levels of metabolic parameters in women. Figure S20: Spline regression analysis of the association between adherence to the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet and levels of metabolic parameters in men. Figure S21: Spline regression analysis of the association between adherence to the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet and levels of metabolic parameters in women. Figure S22: Spline regression analysis of the association between adherence to dietary patterns (Dietary Approaches to Stop Hypertension-DASH diet; Greek Mediterranean Index-GMI; Italian Mediterranean Index-IMI; Mediterranean-DASH Intervention for Neurodegenerative Delay-MIND diet) and the 10-year risk of major cardiovascular events (10-year CVD risk) in men. Figure S23: Spline regression analysis of the association between adherence to dietary patterns (Dietary Approaches to Stop Hypertension-DASH diet; Greek Mediterranean Index-GMI; Italian Mediterranean Index-IMI; Mediterranean-DASH Intervention for Neurodegenerative Delay-MIND diet) and the 10-year risk of major cardiovascular events (10-year CVD risk) in women.
Author Contributions
Conceptualization, T.F. and M.V.; methodology, T.F. and M.V.; formal analysis, T.U. and T.F.; resources and recruitment, D.L., T.D.L., A.S. and R.B.; data curation, M.C., T.U., M.M., C.B., S.G., C.A., S.S., S.F. and T.A.P.; writing—original draft preparation, M.C., T.U. and T.F.; writing—review and editing, all authors; supervision, A.S., R.B., T.A.P. and M.V.; funding acquisition, R.B., M.V. and T.F. All authors have read and agreed to the published version of the manuscript.
Funding
Filippini, Malavolti, Urbano and Vinceti were supported by a grant “Dipartimenti di Eccellenza 2018–2022” to the UNIMORE Department of Biomedical, Metabolic and Neural Sciences from the Italian Ministry of Education, University and Research. Vinceti was supported by the Reggio Emilia Health Authority of the National Health Service. Filippini was supported by grant “UNIMORE FAR 2020 and 2021 Mission Oriented, Linea FOMO-Fondazione di Modena”.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Reggio Emilia Ethics Committee (Approval No. 2016/0022799).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The underlying research materials related to this paper may be available from the corresponding author upon reasonable request. The Data are not publicly available due to privacy and legal restrictions.
Acknowledgments
We acknowledge the collaboration of Reggio Emilia Hospital Transfusion Medicine Unit personnel, Reggio Emilia AVIS-Section staff and volunteers, and all blood donors who participated in this study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- WHO. Cardiovascular Diseases (CVDs); WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Aridi, Y.S.; Walker, J.L.; Wright, O.R.L. The association between the Mediterranean dietary pattern and cognitive health: A systematic review. Nutrients 2017, 9, 674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filippini, T.; Malavolti, M.; Whelton, P.K.; Naska, A.; Orsini, N.; Vinceti, M. Blood pressure effects of sodium reduction: Dose-response meta-analysis of experimental studies. Circulation 2021, 143, 1542–1567. [Google Scholar] [CrossRef] [PubMed]
- Filippini, T.; Malavolti, M.; Whelton, P.K.; Vinceti, M. Sodium intake and risk of hypertension: A systematic review and dose-response meta-analysis of observational cohort studies. Curr. Hypertens. Rep. 2022, 24, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Luong, R.; Ribeiro, R.V.; Cunningham, J.; Chen, S.; Hirani, V. The short- and long-term effects of dietary patterns on cardiometabolic health in adults aged 65 years or older: A systematic review. Nutr. Rev. 2022, 80, 329–350. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Penalvo, J.L.; Cudhea, F.; Imamura, F.; Rehm, C.D.; Mozaffarian, D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA 2017, 317, 912–924. [Google Scholar] [CrossRef] [Green Version]
- Vinceti, M.; Filippini, T.; Crippa, A.; de Sesmaisons, A.; Wise, L.A.; Orsini, N. Meta-analysis of potassium intake and the risk of stroke. J. Am. Heart Assoc. 2016, 5, e004210. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; Campbell, N.R.C.; He, F.J.; Jacobson, M.F.; MacGregor, G.A.; Antman, E.; Appel, L.J.; Arcand, J.; Blanco-Metzler, A.; Cook, N.R.; et al. Sodium and health: Old myths and a controversy based on denial. Curr. Nutr. Rep. 2022, 11, 172–184. [Google Scholar] [CrossRef]
- Hu, F.B.; Willett, W.C. Optimal diets for prevention of coronary heart disease. JAMA 2002, 288, 2569–2578. [Google Scholar] [CrossRef]
- Russo, G.L.; Siani, A.; Fogliano, V.; Geleijnse, J.M.; Giacco, R.; Giampaoli, S.; Iacoviello, L.; Kromhout, D.; Lionetti, L.; Naska, A.; et al. The Mediterranean diet from past to future: Key concepts from the second “Ancel Keys” International Seminar. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 717–732. [Google Scholar] [CrossRef]
- Torres, N.; Guevara-Cruz, M.; Velazquez-Villegas, L.A.; Tovar, A.R. Nutrition and Atherosclerosis. Arch. Med. Res. 2015, 46, 408–426. [Google Scholar] [CrossRef]
- Cicero, A.F.G.; Fogacci, F.; Giovannini, M.; Grandi, E.; D’Addato, S.; Borghi, C.; Brisighella Heart Study Group. Interaction between low-density lipoprotein-cholesterolaemia, serum uric level and incident hypertension: Data from the Brisighella Heart Study. J. Hypertens 2019, 37, 728–731. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K. Reflections on the U.S. Preventive Services Task Force recommendations for screening for hypertension and hypercholesterolemia. J. Gen. Intern. Med. 1990, 5, S17–S19. [Google Scholar] [CrossRef] [PubMed]
- Bruckert, E.; Rosenbaum, D. Lowering LDL-cholesterol through diet: Potential role in the statin era. Curr. Opin. Lipidol. 2011, 22, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corra, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
- de Moraes, M.M.; Oliveira, B.; Afonso, C.; Santos, C.; Torres, D.; Lopes, C.; Miranda, R.C.; Rauber, F.; Antoniazzi, L.; Levy, R.B.; et al. Dietary patterns in Portuguese children and adolescent population: The UPPER project. Nutrients 2021, 13, 3851. [Google Scholar] [CrossRef]
- Naska, A.; Trichopoulou, A. Back to the future: The Mediterranean diet paradigm. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 216–219. [Google Scholar] [CrossRef]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [Green Version]
- Panico, S.; Mattiello, A.; Panico, C.; Chiodini, P. Mediterranean dietary pattern and chronic diseases. Cancer Treat. Res. 2014, 159, 69–81. [Google Scholar] [CrossRef]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet; A Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef] [Green Version]
- Vitiello, V.; Germani, A.; Capuzzo Dolcetta, E.; Donini, L.M.; Del Balzo, V. The new modern Mediterranean diet Italian pyramid. Ann Ig 2016, 28, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean diet, its components, and cardiovascular disease. Am. J. Med. 2015, 128, 229–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosato, V.; Temple, N.J.; La Vecchia, C.; Castellan, G.; Tavani, A.; Guercio, V. Mediterranean diet and cardiovascular disease: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2019, 58, 173–191. [Google Scholar] [CrossRef] [PubMed]
- Agnoli, C.; Krogh, V.; Grioni, S.; Sieri, S.; Palli, D.; Masala, G.; Sacerdote, C.; Vineis, P.; Tumino, R.; Frasca, G.; et al. A priori-defined dietary patterns are associated with reduced risk of stroke in a large Italian cohort. J. Nutr. 2011, 141, 1552–1558. [Google Scholar] [CrossRef] [Green Version]
- Tektonidis, T.G.; Akesson, A.; Gigante, B.; Wolk, A.; Larsson, S.C. A Mediterranean diet and risk of myocardial infarction, heart failure and stroke: A population-based cohort study. Atherosclerosis 2015, 243, 93–98. [Google Scholar] [CrossRef]
- Violi, F.; Pastori, D.; Pignatelli, P.; Carnevale, R. Nutrition, thrombosis, and cardiovascular disease. Circ. Res. 2020, 126, 1415–1442. [Google Scholar] [CrossRef]
- Agnoli, C.; Grioni, S.; Sieri, S.; Palli, D.; Masala, G.; Sacerdote, C.; Vineis, P.; Tumino, R.; Giurdanella, M.C.; Pala, V.; et al. Italian Mediterranean Index and risk of colorectal cancer in the Italian section of the EPIC cohort. Int. J. Cancer 2013, 132, 1404–1411. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Mediterranean dietary pattern, inflammation and endothelial function: A systematic review and meta-analysis of intervention trials. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 929–939. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean diet and health status: Meta-analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef] [Green Version]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appel, L.J.; Brands, M.W.; Daniels, S.R.; Karanja, N.; Elmer, P.J.; Sacks, F.M.; American Heart, A. Dietary approaches to prevent and treat hypertension: A scientific statement from the American Heart Association. Hypertension 2006, 47, 296–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petersen, K.S.; Kris-Etherton, P.M. Diet quality assessment and the relationship between diet quality and cardiovascular disease risk. Nutrients 2021, 13, 4305. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.M.; Lovegrove, J.A.; Griffin, B.A. Dietary patterns and cardiovascular disease. Proc. Nutr. Soc. 2013, 72, 407–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gillette Guyonnet, S.; Abellan Van Kan, G.; Andrieu, S.; Barberger Gateau, P.; Berr, C.; Bonnefoy, M.; Dartigues, J.F.; de Groot, L.; Ferry, M.; Galan, P.; et al. IANA task force on nutrition and cognitive decline with aging. J. Nutr. Health Aging 2007, 11, 132–152. [Google Scholar]
- Liu, X.; Morris, M.C.; Dhana, K.; Ventrelle, J.; Johnson, K.; Bishop, L.; Hollings, C.S.; Boulin, A.; Laranjo, N.; Stubbs, B.J.; et al. Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) study: Rationale, design and baseline characteristics of a randomized control trial of the MIND diet on cognitive decline. Contemp. Clin. Trials 2021, 102, 106270. [Google Scholar] [CrossRef]
- Morris, M.C. Nutritional determinants of cognitive aging and dementia. Proc. Nutr. Soc. 2012, 71, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Morris, M.C.; Tangney, C.C. Dietary fat composition and dementia risk. Neurobiol. Aging 2014, 35 (Suppl. 2), S59–S64. [Google Scholar] [CrossRef] [Green Version]
- Morris, M.C.; Tangney, C.C.; Wang, Y.; Sacks, F.M.; Barnes, L.L.; Bennett, D.A.; Aggarwal, N.T. MIND diet slows cognitive decline with aging. Alzheimers Dement. 2015, 11, 1015–1022. [Google Scholar] [CrossRef] [Green Version]
- Morris, M.C.; Tangney, C.C.; Wang, Y.; Sacks, F.M.; Bennett, D.A.; Aggarwal, N.T. MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimers Dement. 2015, 11, 1007–1014. [Google Scholar] [CrossRef] [Green Version]
- Hosking, D.E.; Eramudugolla, R.; Cherbuin, N.; Anstey, K.J. MIND not Mediterranean diet related to 12-year incidence of cognitive impairment in an Australian longitudinal cohort study. Alzheimers Dement. 2019, 15, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Golzarand, M.; Mirmiran, P.; Azizi, F. Adherence to the MIND diet and the risk of cardiovascular disease in adults: A cohort study. Food Funct. 2022, 13, 1651–1658. [Google Scholar] [CrossRef] [PubMed]
- Urbano, T.; Filippini, T.; Wise, L.A.; Lasagni, D.; De Luca, T.; Sucato, S.; Polledri, E.; Malavolti, M.; Rigon, C.; Santachiara, A.; et al. Associations of urinary and dietary cadmium with urinary 8-oxo-7,8-dihydro-2’-deoxyguanosine and blood biochemical parameters. Environ. Res. 2022, 210, 112912. [Google Scholar] [CrossRef]
- Pala, V.; Sieri, S.; Palli, D.; Salvini, S.; Berrino, F.; Bellegotti, M.; Frasca, G.; Tumino, R.; Sacerdote, C.; Fiorini, L.; et al. Diet in the Italian EPIC cohorts: Presentation of data and methodological issues. Tumori 2003, 89, 594–607. [Google Scholar] [CrossRef]
- Pasanisi, P.; Berrino, F.; Bellati, C.; Sieri, S.; Krogh, V. Validity of the Italian EPIC questionnaire to assess past diet. IARC Sci. Publ. 2002, 156, 41–44. [Google Scholar] [PubMed]
- Filippini, T.; Michalke, B.; Wise, L.A.; Malagoli, C.; Malavolti, M.; Vescovi, L.; Salvia, C.; Bargellini, A.; Sieri, S.; Krogh, V.; et al. Diet composition and serum levels of selenium species: A cross-sectional study. Food Chem. Toxicol. 2018, 115, 482–490. [Google Scholar] [CrossRef]
- Malavolti, M.; Fairweather-Tait, S.J.; Malagoli, C.; Vescovi, L.; Vinceti, M.; Filippini, T. Lead exposure in an Italian population: Food content, dietary intake and risk assessment. Food Res. Int. 2020, 137, 109370. [Google Scholar] [CrossRef]
- Filippini, T.; Adani, G.; Malavolti, M.; Garuti, C.; Cilloni, S.; Vinceti, G.; Zamboni, G.; Tondelli, M.; Galli, C.; Costa, M.; et al. Dietary habits and risk of early-onset dementia in an Italian case-control study. Nutrients 2020, 12, 3682. [Google Scholar] [CrossRef] [PubMed]
- Malagoli, C.; Malavolti, M.; Agnoli, C.; Crespi, C.M.; Fiorentini, C.; Farnetani, F.; Longo, C.; Ricci, C.; Albertini, G.; Lanzoni, A.; et al. Diet quality and risk of melanoma in an Italian population. J. Nutr. 2015, 145, 1800–1807. [Google Scholar] [CrossRef] [Green Version]
- Malavolti, M.; Naska, A.; Fairweather-Tait, S.J.; Malagoli, C.; Vescovi, L.; Marchesi, C.; Vinceti, M.; Filippini, T. Sodium and potassium content of foods consumed in an Italian population and the ompact of adherence to a Mediterranean diet on their intake. Nutrients 2021, 13, 2681. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [Green Version]
- Vurro, F.; Merolle, L.; Marraccini, C.; Parisi, M.; Canovi, L.; Erta, B.; Santachiara, A.; Bonvicini, L.; Giorgi Rossi, P.; Baricchi, R.; et al. Quantitative assessment of the anticoagulant in plasma units collected by plasmapheresis. Transfusion 2019, 59, 2113–2120. [Google Scholar] [CrossRef] [PubMed]
- Fasano, T.; Bedini, J.L.; Fle, P.A.; Jlaiel, M.; Hubbert, K.; Datta, H.; Chicha-Cattoir, V.; Mansour, H.; Mira, A.; de la Presa, B.G.; et al. Multi-site performance evaluation and Sigma metrics of 20 assays on the Atellica chemistry and immunoassay analyzers. Clin. Chem. Lab. Med. 2019, 58, 59–68. [Google Scholar] [CrossRef]
- Campo, L.; Polledri, E.; Bechtold, P.; Gatti, G.; Ranzi, A.; Lauriola, P.; Goldoni, C.A.; Bertazzi, P.A.; Fustinoni, S. Determinants of active and environmental exposure to tobacco smoke and upper reference value of urinary cotinine in not exposed individuals. Environ. Res. 2016, 148, 154–163. [Google Scholar] [CrossRef]
- Urbano, T.; Filippini, T.; Lasagni, D.; De Luca, T.; Sucato, S.; Polledri, E.; Bruzziches, F.; Malavolti, M.; Baraldi, C.; Santachiara, A.; et al. Associations between urinary and dietary selenium and blood metabolic parameters in a healthy Northern Italy population. Antioxidants 2021, 10, 1193. [Google Scholar] [CrossRef]
- National Italian Institute of Health. What is CuoreData; National Italian Institute of Health: Roma, Italy, 2022. [Google Scholar]
- Harrell, F.E. Regression Modeling Strategies. With Applications to Linear Models, Logistic Regression, and Survival Analysis; Springer: New York, NY, USA, 2001. [Google Scholar]
- Malagoli, C.; Malavolti, M.; Farnetani, F.; Longo, C.; Filippini, T.; Pellacani, G.; Vinceti, M. Food and beverage consumption and melanoma risk: A population-Based case-control study in Northern Italy. Nutrients 2019, 11, 2206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bendinelli, B.; Masala, G.; Bruno, R.M.; Caini, S.; Saieva, C.; Boninsegni, A.; Ungar, A.; Ghiadoni, L.; Palli, D. A priori dietary patterns and blood pressure in the EPIC Florence cohort: A cross-sectional study. Eur. J. Nutr. 2019, 58, 455–466. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H.; Salas-Salvado, J.; Rahelic, D.; Kendall, C.W.; Rembert, E.; Sievenpiper, J.L. Dietary patterns and cardiometabolic outcomes in diabetes: A summary of systematic reviews and meta-analyses. Nutrients 2019, 11, 2209. [Google Scholar] [CrossRef] [Green Version]
- Meslier, V.; Laiola, M.; Roager, H.M.; De Filippis, F.; Roume, H.; Quinquis, B.; Giacco, R.; Mennella, I.; Ferracane, R.; Pons, N.; et al. Mediterranean diet intervention in overweight and obese subjects lowers plasma cholesterol and causes changes in the gut microbiome and metabolome independently of energy intake. Gut 2020, 69, 1258–1268. [Google Scholar] [CrossRef] [Green Version]
- Psaltopoulou, T.; Hatzis, G.; Papageorgiou, N.; Androulakis, E.; Briasoulis, A.; Tousoulis, D. Socioeconomic status and risk factors for cardiovascular disease: Impact of dietary mediators. Hellenic. J. Cardiol. 2017, 58, 32–42. [Google Scholar] [CrossRef]
- Estruch, R.; Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Ruiz-Gutierrez, V.; Covas, M.I.; Fiol, M.; Gomez-Gracia, E.; Lopez-Sabater, M.C.; Vinyoles, E.; et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: A randomized trial. Ann. Intern. Med. 2006, 145, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Trautwein, E.A.; McKay, S. The role of specific components of a plant-based diet in management of dyslipidemia and the impact on cardiovascular risk. Nutrients 2020, 12, 2671. [Google Scholar] [CrossRef] [PubMed]
- Salas-Salvado, J.; Becerra-Tomas, N.; Garcia-Gavilan, J.F.; Bullo, M.; Barrubes, L. Mediterranean diet and cardiovascular disease prevention: What do we know? Prog. Cardiovasc. Dis. 2018, 61, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Siervo, M.; Lara, J.; Chowdhury, S.; Ashor, A.; Oggioni, C.; Mathers, J.C. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: A systematic review and meta-analysis. Br. J. Nutr. 2015, 113, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Obarzanek, E.; Sacks, F.M.; Vollmer, W.M.; Bray, G.A.; Miller, E.R., 3rd; Lin, P.H.; Karanja, N.M.; Most-Windhauser, M.M.; Moore, T.J.; Swain, J.F.; et al. Effects on blood lipids of a blood pressure-lowering diet: The Dietary Approaches to Stop Hypertension (DASH) trial. Am. J. Clin. Nutr. 2001, 74, 80–89. [Google Scholar] [CrossRef]
- Toledo, E.; Hu, F.B.; Estruch, R.; Buil-Cosiales, P.; Corella, D.; Salas-Salvado, J.; Covas, M.I.; Aros, F.; Gomez-Gracia, E.; Fiol, M.; et al. Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: Results from a randomized controlled trial. BMC Med. 2013, 11, 207. [Google Scholar] [CrossRef] [Green Version]
- Mohammadpour, S.; Ghorbaninejad, P.; Janbozorgi, N.; Shab-Bidar, S. Associations between adherence to MIND diet and metabolic syndrome and general and abdominal obesity: A cross-sectional study. Diabetol. Metab. Syndr. 2020, 12, 101. [Google Scholar] [CrossRef]
- Chiavaroli, L.; Viguiliouk, E.; Nishi, S.K.; Blanco Mejia, S.; Rahelic, D.; Kahleova, H.; Salas-Salvado, J.; Kendall, C.W.; Sievenpiper, J.L. DASH dietary pattern and cardiometabolic outcomes: An umbrella review of systematic reviews and meta-analyses. Nutrients 2019, 11, 338. [Google Scholar] [CrossRef] [Green Version]
- Yu, E.; Malik, V.S.; Hu, F.B. Cardiovascular disease prevention by diet modification: JACC health promotion series. J. Am. Coll. Cardiol. 2018, 72, 914–926. [Google Scholar] [CrossRef]
- Soltani, S.; Arablou, T.; Jayedi, A.; Salehi-Abargouei, A. Adherence to the dietary approaches to stop hypertension (DASH) diet in relation to all-cause and cause-specific mortality: A systematic review and dose-response meta-analysis of prospective cohort studies. Nutr. J. 2020, 19, 37. [Google Scholar] [CrossRef] [Green Version]
- Iacobellis, G.; Ribaudo, M.C.; Zappaterreno, A.; Iannucci, C.V.; Leonetti, F. Prevalence of uncomplicated obesity in an Italian obese population. Obes. Res. 2005, 13, 1116–1122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vinceti, M.; Grill, P.; Malagoli, C.; Filippini, T.; Storani, S.; Malavolti, M.; Michalke, B. Selenium speciation in human serum and its implications for epidemiologic research: A cross-sectional study. J. Trace Elem. Med. Biol. 2015, 31, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Pala, V.; Berrino, F.; Vineis, P.; Palli, D.; Celentano, E.; Tumino, R.; Krogh, V. How vegetables are eaten in Italy EPIC centres: Still setting a good example? IARC Sci. Publ. 2002, 156, 119–121. [Google Scholar] [PubMed]
- Pisani, P.; Faggiano, F.; Krogh, V.; Palli, D.; Vineis, P.; Berrino, F. Relative validity and reproducibility of a food frequency dietary questionnaire for use in the Italian EPIC centres. Int. J. Epidemiol. 1997, 26, S152–S160. [Google Scholar] [CrossRef] [Green Version]
- Salvia, C.; Donfrancesco, C.; Palmieri, L.; Lo Noce, C.; Vanuzzo, D.; Vinceti, M.; Bargellini, A.; Borella, P.; Giampaoli, S. The Health Examination Survey at regional level: The Emilia-Romagna Region (Northern Italy) example. Epidemiol. Prev. 2020, 44, 40–47. [Google Scholar] [CrossRef]
- Agudo, A.; Slimani, N.; Ocke, M.C.; Naska, A.; Miller, A.B.; Kroke, A.; Bamia, C.; Karalis, D.; Vineis, P.; Palli, D.; et al. Consumption of vegetables, fruit and other plant foods in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohorts from 10 European countries. Public Health Nutr. 2002, 5, 1179–1196. [Google Scholar] [CrossRef] [Green Version]
- Fabrice Elegbede, C.; Papadopoulos, A.; Kolbaum, A.E.; Turrini, A.; Mistura, L.; Lindtner, O.; Sirot, V. TDS exposure project: How and when to consider seasonality in a total diet study? Food Chem. Toxicol. 2017, 105, 119–126. [Google Scholar] [CrossRef]
- Halkjaer, J.; Olsen, A.; Bjerregaard, L.J.; Deharveng, G.; Tjonneland, A.; Welch, A.A.; Crowe, F.L.; Wirfalt, E.; Hellstrom, V.; Niravong, M.; et al. Intake of total, animal and plant proteins, and their food sources in 10 countries in the European Prospective Investigation into Cancer and Nutrition. Eur. J. Clin. Nutr. 2009, 63, S16–S36. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).