Psychological Interventions for Higher Education Students in Europe: A Systematic Literature Review
Abstract
1. Introduction
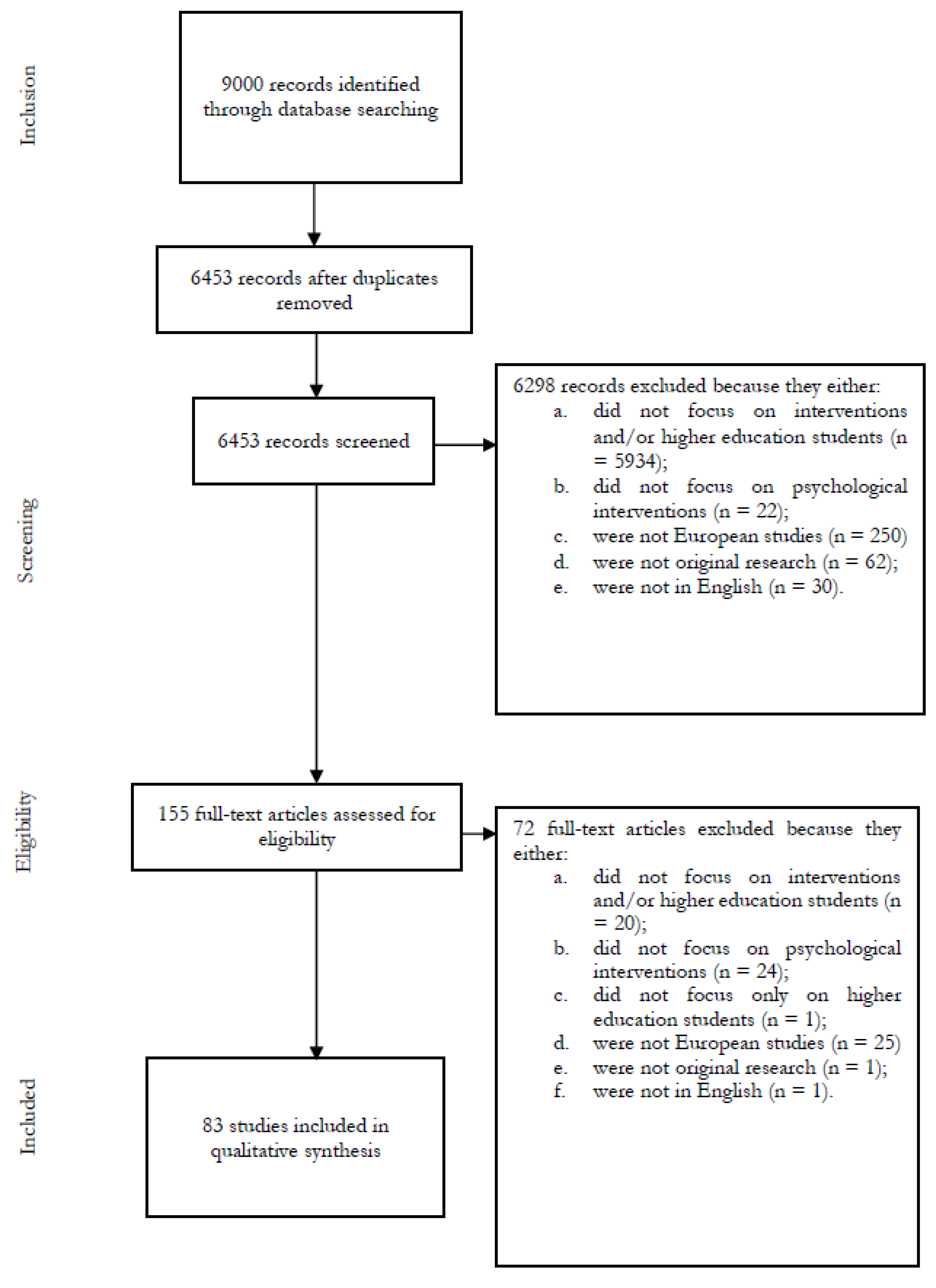
2. Materials and Methods
2.1. Search Strategies
- (1)
- Title, abstract, and keywords for Scopus.
- (2)
- All fields for PubMed.
- (3)
- The topic for WoS.
- (4)
- Subject terms for the PsychINFO and PsycARTICLES databases.
2.2. Selection Criteria
- The study was quantitative or qualitative original research.
- The research study made explicit reference to psychological and psychotherapeutic interventions addressed to higher education students.
- The research study was published within the given time interval (January 2010–April 2020).
- The study was written in the English language only.
- The study did not report original results (reviews, letters, editorials, and comments).
- Dissertations.
- The study focused on mentoring programs.
- The study focused on self-help interventions and peer education.
3. Results
- Section 3.1 Counseling and Group Counseling (eight papers).
- Section 3.2 Psychodynamic (six papers).
- Section 3.3 Cognitive–Behavioral (fifteen papers).
- Section 3.4 Other Psychological (eighteen papers).
- Section 3.5 Mindfulness (nine papers).
- Section 3.6 Online (seventeen papers).
- Section 3.7 App and Mobile (ten papers).
3.1. Counseling and Group Counseling
3.2. Psychodynamic Interventions
3.3. Cognitive–Behavioral Interventions
3.4. Other Psychological Interventions
3.5. Mindfulness
3.6. Online Interventions
3.7. App and Mobile Interventions
4. Discussion
Limitations of the Study
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arnett, J.J. Emerging adulthood. A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Arnett, J.J.; Žukauskienė, R.; Sugimura, K. The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. Lancet Psychiatry 2014, 1, 569–576. [Google Scholar] [CrossRef]
- Hochberg, Z.E.; Konner, M. Emerging Adulthood, a Pre-adult Life-History Stage. Front. Endocrinol. 2020, 10, 918. [Google Scholar] [CrossRef] [PubMed]
- Engelbertink, M.M.; Colomer, J.; Woudt-Mittendorff, K.M.; Alsina, Á.; Kelders, S.M.; Ayllón, S.; Westerhof, G.J. The reflection level and the construction of professional identity of university students. Reflective Pract. 2021, 22, 73–85. [Google Scholar] [CrossRef]
- Kelly, R.; Garr, O.M.; Leahy, K.; Goos, M. An investigation of university students and professionals’ professional STEM identity status. J. Sci. Educ. Technol. 2020, 29, 536–546. [Google Scholar] [CrossRef]
- Schechter, M.; Herbstman, B.; Ronningstam, E.; Goldblatt, M.J. Emerging adults, identity development, and suicidality: Implications for psychoanalytic psychotherapy. Psychoanal. Study Child 2018, 71, 20–39. [Google Scholar] [CrossRef]
- Kreß, V.; Sperth, M.; Hofmann, F.H.; Holm-Hadulla, R.M. Psychological complaints of students: A comparison of field samples with clients of a counseling service at a typical German University. Ment. Health Prev. 2015, 3, 41–47. [Google Scholar] [CrossRef]
- Jones, P.J.; Park, S.Y.; Lefevor, G.T. Contemporary college student anxiety: The role of academic distress, financial stress, and support. J. Coll. Couns 2018, 21, 252–264. [Google Scholar] [CrossRef]
- Sharp, J.; Theiler, S. A review of psychological distress among university students: Pervasiveness, implications and potential points of intervention. Int. J. Adv. Couns. 2018, 40, 193–212. [Google Scholar] [CrossRef]
- Oksanen, A.; Laimi, K.; Björklund, K.; Löyttyniemi, E.; Kunttu, K. A 12-year trend of psychological distress: National study of finnish university students. Cent. Eur. J. Public Health 2017, 25, 113–119. [Google Scholar] [CrossRef]
- Shankland, R.; Kotsou, I.; Vallet, F.; Bouteyre, E.; Dantzer, C.; Leys, C. Burnout in university students: The mediating role of sense of coherence on the relationship between daily hassles and burnout. High Educ. 2018, 78, 91–113. [Google Scholar] [CrossRef]
- Lun, K.W.; Chan, C.K.; Ip, P.K.; Ma, S.Y.; Tsai, W.W.; Wong, C.S.; Wong, C.H.; Wong, T.W.; Yan, D. Depression and anxiety among university students in Hong Kong. Hong Kong Med. J. 2018, 24, 466–472. [Google Scholar] [CrossRef]
- January, J.; Madhombiro, M.; Chipamaunga, S.; Ray, S.; Chingono, A.; Abas, M. Prevalence of depression and anxiety among undergraduate university students in low-and middle-income countries: A systematic review protocol. Syst. Rev. 2018, 7, 1–5. [Google Scholar] [CrossRef]
- Cheung, K.; Tam, K.Y.; Tsang, M.H.; Zhang, L.W.; Lit, S.W. Depression, anxiety and stress in different subgroups of first-year university students from 4-year cohort data. J. Affect. Disord. 2020, 274, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Franzoi, I.G.; D’Ovidio, F.; Costa, G.; D’Errico, A.; Granieri, A. Self-Rated Health and Psychological Distress among Emerging Adults in Italy: A Comparison between Data on University Students, Young Workers and Working Students Collected through the 2005 and 2013 National Health Surveys. Int. J. Environ. Res. 2021, 18, 6403. [Google Scholar] [CrossRef] [PubMed]
- Tariku, G.H.; Zerihun, A.A.; Bisrat, Z.S.; Adissu, G.G.; Jini, D. Mental Distress and its Associated Factors among Students of Mizan Aman Health Science College, Ethiopia. J. Med. Sci. 2017, 17, 61–67. [Google Scholar] [CrossRef]
- Mboya, I.B.; John, B.; Kibopile, E.S.; Mhando, L.; George, J.; Ngocho, J.S. Factors associated with mental distress among undergraduate students in northern Tanzania. BMC Psychiatry 2020, 20, 28. [Google Scholar] [CrossRef]
- Holm-Hadulla, R.M.; Koutsoukou-Argyraki, A. Mental health of students in a globalized world: Prevalence of complaints and disorders, methods and effectivity of counseling, structure of mental health services for students. Ment. Health Prevent. 2015, 3, 1–4. [Google Scholar] [CrossRef]
- Harrer, M.; Adam, S.H.; Baumeister, H.; Cuijpers, P.; Karyotaki, E.; Auerbach, R.P.; Kessler, R.C.; Bruffaerts, R.; Berking, M.; Ebert, D.D. Internet interventions for mental health in university students: A systematic review and meta-analysis. J. Methods Psychiatr. Res. 2019, 28, e1759. [Google Scholar] [CrossRef]
- Rudnik, A.; Anikiej-Wiczenbach, P.; Szulman-Wardal, A.; Conway, P.; Bidzan, M. Offering psychological support to university students in Poland during the COVID-19 pandemic: Lessons learned from an initial evaluation. Front. Psychol. 2021, 3884, 635378. [Google Scholar] [CrossRef]
- Adamo, S.M.G.; Fontana, M.R.; Preti, E.; Prunas, A.; Riffaldi, M.L.; Sarno, I. At the border: Reflections on psychoanalytically oriented counseling in an Italian university setting. Br. J. Guid. Counc. 2012, 40, 5–14. [Google Scholar] [CrossRef]
- Huang, J.; Nigatu, Y.T.; Smail-Crevier, R.; Zhang, X.; Wang, J. Interventions for common mental health problems among university and college students: A systematic review and meta-analysis of randomized controlled trials. J. Psychiatr. Res. 2018, 107, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lipson, S.K.; Lattie, E.G.; Eisenberg, D. Increased rates of mental health service utilization by U.S. college students: 10-year population-level trends (2007–2017). Psychiatr. Serv. 2019, 70, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Franzoi, I.G.; Sauta, M.D.; Carnevale, G.; Granieri, A. Student Counseling Centers in Europe: A Retrospective Analysis. Front. Psychol. 2022, 13, 894423. [Google Scholar] [CrossRef] [PubMed]
- Biasi, V.; Patrizi, N.; Mosca, M.; De Vincenzo, C. The effectiveness of university counseling for improving academic outcomes and well-being. Br. J. Guid. Couns. 2017, 45, 248–257. [Google Scholar] [CrossRef]
- Galante, J.; Dufour, G.; Vainre, M.; Wagner, A.P.; Stochl, J.; Benton, A.; Lathia, N.; Howarth, E.; Jones, P.B. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): A pragmatic randomised controlled trial. Lancet Glob. Health 2018, 3, e72–e81. [Google Scholar] [CrossRef]
- Franzoi, I.G.; Sauta, M.D.; Granieri, A. State and Trait Anxiety Among University Students: A Moderated Mediation Model of Negative Affectivity, Alexithymia, and Housing Conditions. Front. Psychol. 2020, 11, 1255. [Google Scholar] [CrossRef]
- Monk, E.M. Student mental health. Part 2: The main study and reflection of significant issues. Couns. Psychol. Q. 2004, 17, 33–43. [Google Scholar] [CrossRef]
- Koutra, A.; Katsiadrami, A.; Diakogiannis, G. The effect of group psychological counseling in Greek university students’ anxiety. Eur. J. Psychother. Couns. Health 2010, 2, 101–111. [Google Scholar] [CrossRef]
- Pillay, J. Suicidal behaviour among university students: A systematic review. S Afr. J. Psychol. 2021, 51, 54–66. [Google Scholar] [CrossRef]
- Institute for Public Policy Research. Not by Degrees: Improving Student Mental Health in the UK’s Universities. 2017. Available online: https://www.ippr.org/research/publications/not-by-degrees (accessed on 2 May 2022).
- Hubbard, K.; Reohr, P.; Tolcher, L.; Downs, A. Stress, Mental Health Symptoms, and Help-Seeking in College Students. Psi Chi J. Psychol. Res. 2018, 23, 293–305. [Google Scholar] [CrossRef]
- Fischbein, R.; Bonfine, N. Pharmacy and Medical Students’ Mental Health Symptoms, Experiences, Attitudes and Help-Seeking Behaviors. Am. J. Pharm. Educ. 2019, 83, 7558. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, J.K.; Rabon, J.K.; Reynolds, E.E.; Barton, A.L.; Chang, E.C. Perceived stress and suicidal behaviors in college students: Conditional indirect effects of depressive symptoms and mental health stigma. Stigma Health 2019, 4, 98–106. [Google Scholar] [CrossRef]
- Granieri, A.; Casale, S.; Sauta, M.D.; Franzoi, I.G. Suicidal Ideation among University Students: A Moderated Mediation Model Considering Attachment, Personality, and Sex. Int. J. Environ. Res. Public Health 2022, 19, 6167. [Google Scholar] [CrossRef] [PubMed]
- Granieri, A.; Bonafede, M.; Marinaccio, A.; Iavarone, I.; Marsili, D.; Franzoi, I.G. SARS-CoV-2 and Asbestos Exposure: Can Our Experience with Mesothelioma Patients Help Us Understand the Psychological Consequences of COVID-19 and Develop Interventions? Front. Psychol. 2020, 11, 584320. [Google Scholar] [CrossRef]
- Granieri, A.; Franzoi, I.G.; Chung, M.C. Editorial: Psychological Distress Among University Students. Front. Psychol. 2021, 12, 647940. [Google Scholar] [CrossRef]
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The psychological impact of COVID-19 on the mental health in the general population. Int. J. Med. 2020, 113, 531–537. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Bourion-Bédès, S.; Tarquinio, C.; Batt, M.; Tarquinio, P.; Lebreuilly, R.; Sorsana, C.; Legrand, K.; Rousseau, H.; Baumann, C. Stress and associated factors among French university students under the COVID-19 lockdown: The results of the PIMS-CoV 19 study. J. Affect. Disord. 2021, 283, 108–114. [Google Scholar] [CrossRef]
- Demirdogen, E.S.; Orak, I.; Cansever, O.M.; Warikoo, N.; Yavuz, M. The associations between metacognition problems, mindfulness, and internalizing symptoms in university students quarantined due to COVID-19 in Turkey. Perspect. Psychiatr. Care 2022, 58, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Mosleh, S.M.; Shudifat, R.M.; Dalky, H.F.; Almalik, M.M.; Alnajar, M.K. Mental health, learning behaviour and perceived fatigue among university students during the COVID-19 outbreak: A cross-sectional multicentric study in the UAE. BMC Psychol. 2022, 10, 47. [Google Scholar] [CrossRef] [PubMed]
- Hagedorn, R.L.; Wattick, R.A.; Olfert, M.D. “My entire world stopped”: College students’ psychosocial and academic frustrations during the COVID-19 pandemic. Appl. Res. Qual. Life 2022, 17, 1069–1090. [Google Scholar] [CrossRef] [PubMed]
- Woolston, C. Signs of depression and anxiety soar among US graduate students during pandemic. Nature 2020, 585, 147–148. [Google Scholar] [CrossRef] [PubMed]
- Odriozola-González, P.; Planchuelo-Gómez, L.; Irurtia, M.J.; de Luis-García, R. Psychological symptoms of the outbreak of the COVID-19 confinement in Spain. J. Health Psychol. 2020, 27, 825–835. [Google Scholar] [CrossRef] [PubMed]
- Essadek, A.; Rabeyron, T. Mental health of French students during the COVID-19 pandemic. J. Affect. Disord. 2020, 277, 392–393. [Google Scholar] [CrossRef]
- Nurunnabi, M.; Almusharraf, N.; Aldeghaither, D. Mental health and well-being during the COVID-19 pandemic in higher education: Evidence from G20 countries. Am. J. Public Health Res. 2021, 9 (Suppl. S1). [Google Scholar] [CrossRef]
- Tchounwou, P.B. Psychological impacts and post-traumatic stress disorder among people under COVID-19 quarantine and isolation: A global survey. Int. J. Environ. Res. 2021, 18, 5719. [Google Scholar]
- Healthy Minds Network. Healthy Minds Study. 2018. Available online: https://healthymindsnetwork.org/research/hms (accessed on 2 May 2022).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Hofmann, F.H.; Sperth, M.; Holm-Hadulla, R.M. Methods and effects of integrative counseling and short-term psychotherapy for students. Ment. Health Prev. 2015, 3, 57–65. [Google Scholar] [CrossRef]
- Strepparava, M.; Bani, M.; Zorzi, F.; Corrias, D.; Dolce, R.; Rezzonico, G. Cognitive counseling intervention: Treatment effectiveness in an Italian university centre. Br. J. Guid. Counc. 2015, 44, 423–433. [Google Scholar] [CrossRef]
- McKenzie, K.; Murray, K.R.; Murray, A.L.; Richelieu, M. The effectiveness of university counseling for students with academic issues. Couns. Psychother. Res. 2015, 15, 284–288. [Google Scholar] [CrossRef]
- Østergård, O.K.; Fenger, M.; Hougaard, E. Symptomatic distress and effectiveness of psychological treatments delivered at a nationwide student counseling service. Couns. Psychol. Q. 2019, 32, 150–168. [Google Scholar] [CrossRef]
- Esposito, G.; Marano, D.; Freda, M.F. Supportive and interpretative interventions in fostering mentalisation during counseling. Br. J. Guid. Counc. 2020, 48, 314–332. [Google Scholar] [CrossRef]
- Maselli, M.; Gobbi, E.; Carraro, A. Effectiveness of individual counseling and activity monitors to promote physical activity among university students. J. Sports Med. Phys. Fitness 2019, 59, 132–140. [Google Scholar] [CrossRef]
- Vassilopoulos, S.P.; Brouzos, A. A pilot person-centred group counseling for university students: Effects on social anxiety and self-esteem. Hell. J. Psychol. 2012, 9, 222–239. [Google Scholar]
- Vescovelli, F.; Melani, P.; Ruini, C.; Ricci Bitti, P.E.; Monti, F. University counseling service for improving students’ mental health. Psychol. Serv. 2017, 14, 470–480. [Google Scholar] [CrossRef]
- Monti, F.; Tonetti, L.; Ricci Bitti, P.E. Comparison of cognitive-behavioural therapy and psychodynamic therapy in the treatment of anxiety among university students: An effectiveness study. Br. J. Guid. Counc. 2014, 42, 233–244. [Google Scholar] [CrossRef]
- Monti, F.; Tonetti, L.; Ricci Bitti, P.E. Effectiveness of psychological treatments delivered at a counseling service for students. Psychol. Rep. 2013, 113, 955–968. [Google Scholar] [CrossRef]
- Monti, F.; Tonetti, L.; Ricci Bitti, P.E. Short-term effectiveness of psychotherapy treatments delivered at a university counseling service. Br. J. Guid. Counc. 2016, 44, 414–422. [Google Scholar] [CrossRef]
- Cerutti, R.; Fontana, A.; Ghezzi, V.; Menozzi, F.; Spensieri, V.; Tambelli, R. Exploring psychopathological distress in Italian university students seeking help: A picture from a university counseling service. Curr. Psychol. 2020, 41, 1382–1394. [Google Scholar] [CrossRef]
- Amodeo, A.L.; Picariello, S.; Valerio, P.; Bochicchio, V.; Scandurra, C. Group psychodynamic counseling with final-year undergraduates in clinical psychology: A clinical methodology to reinforce academic identity and psychological well-being. Psychodyn. Pract. 2017, 23, 161–180. [Google Scholar] [CrossRef]
- Rozental, A.; Forsström, D.; Lindner, P.; Nilsson, S.; Mårtensson, L.; Rizzo, A.; Andersson, G.; Carlbring, P. Treating procrastination using cognitive behavior therapy: A pragmatic randomized controlled trial comparing treatment delivered via the internet or in groups. Behav. Ther. 2018, 49, 180–197. [Google Scholar] [CrossRef] [PubMed]
- Bernhardsdottir, J.; Vilhjalmsson, R.; Champion, J.D. Evaluation of a brief cognitive behavioral group therapy for psychological distress among female Icelandic University students. Issues Ment. Health Nurs. 2013, 34, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Reiss, N.; Warnecke, I.; Tibubos, A.N.; Tolgou, T.; Luka-Krausgrill, U.; Rohrmann, S. Effects of cognitive-behavioral therapy with relaxation vs. imagery rescripting on psychophysiological stress responses of students with test anxiety in a randomized controlled trial. Psychother. Res. 2019, 29, 974–985. [Google Scholar] [CrossRef] [PubMed]
- Reiss, N.; Warnecke, I.; Tolgou, T.; Krampen, D.; Luka-Krausgrill, U.; Rohrmann, S. Effects of cognitive behavioral therapy with relaxation vs. imagery rescripting on test anxiety: A randomized controlled trial. J. Affect. Disord. 2017, 208, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Vázquez, F.L.; Torres, A.; Blanco, V.; Díaz, O.; Otero, P.; Hermida, E. Comparison of relaxation training with a cognitive-behavioural intervention for indicated prevention of depression in university students: A randomized controlled trial. J. Psychiatr. Res. 2012, 46, 1456–1463. [Google Scholar] [CrossRef]
- Thorgeirsdottir, M.T.; Bjornsson, A.S.; Arnkelsson, G.B. Group climate development in brief group therapies: A comparison between cognitive-behavioral group therapy and group psychotherapy for social anxiety disorder. Theory Res. Pract. 2015, 19, 200–209. [Google Scholar] [CrossRef]
- Bernhardsdottir, J.; Champion, J.D.; Skärsäter, I. The experience of participation in a brief cognitive behavioural group therapy for psychologically distressed female university students. J. Psychiatr. Ment. Health Nurs. 2014, 21, 679–686. [Google Scholar] [CrossRef]
- Martín-Pérez, C.; Navas, J.F.; Perales, J.C.; López-Martín, Á.; Cordovilla-Guardia, S.; Portillo, M.; Maldonado, A.; Vilar-López, R. Brief group-delivered motivational interviewing is equally effective as brief group-delivered cognitive-behavioral therapy at reducing alcohol use in risky college drinkers. PLoS ONE 2019, 14, e0226271. [Google Scholar] [CrossRef]
- Thorisdottir, A.S.; Tryggvadottir, A.; Saevarsson, S.T.; Bjornsson, A.S. Brief report: Sudden gains in cognitive-behavioral group therapy and group psychotherapy for social anxiety disorder among college students. Cogn. Behav. Ther 2018, 47, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Marrero, R.J.; Carballeira, M.; Martín, S.; Mejías, M.; Hernández, J.A. Effectiveness of a positive psychology intervention combined with cognitive behavioral therapy in university students. Ann. Psychol. 2016, 32, 728–740. [Google Scholar] [CrossRef]
- Terp, U.; Hjärthag, F.; Bisholt, B. Effects of a cognitive behavioral-based stress management program on stress management competency, self-efficacy and self-esteem experienced by nursing students. Nurse Educ. 2019, 44, E1–E5. [Google Scholar] [CrossRef]
- Larsson, A.; Hooper, N.; Osborne, L.A.; Bennett, P.; McHugh, L. Using brief cognitive restructuring and cognitive defusion techniques to cope with negative thoughts. Behav. Modif. 2016, 40, 452–482. [Google Scholar] [CrossRef]
- Van der Oord, S.; Boyer, B.E.; Van Dyck, L.; Mackay, K.J.; De Meyer, H.; Baeyens, D. A randomized controlled study of a cognitive behavioral planning intervention for college students with adhd: An effectiveness study in student counseling services in flanders. J. Atten. Disord. 2020, 24, 849–862. [Google Scholar] [CrossRef] [PubMed]
- Schuck, K.; Keijsers, G.P.; Rinck, M. The effects of brief cognitive-behaviour therapy for pathological skin picking: A randomized comparison to wait-list control. Behav. Res. Ther. 2011, 49, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Biolcati, R.; Agostini, F.; Mancini, G. Analytical psychodrama with college students suffering from mental health problems: Preliminary outcomes. Res. Psychother. 2017, 20, 272. [Google Scholar] [CrossRef] [PubMed]
- Ouweneel, E.; Le Blanc, P.M.; Schaufeli, W.B. On being grateful and kind: Results of two randomized controlled trials on study-related emotions and academic engagement. J. Psychol. 2014, 148, 37–60. [Google Scholar] [CrossRef]
- McCarthy, B.; Trace, A.; O’Donovan, M.; O’Regan, P.; Brady-Nevin, C.; O’Shea, M.; Martin, A.-M.; Murphy, M. Coping with stressful events: A pre-post-test of a psycho-educational intervention for undergraduate nursing and midwifery students. Nurse Educ. Today 2018, 61, 273–280. [Google Scholar] [CrossRef]
- Victor, P.P.; Teismann, T.; Willutzki, U. A Pilot evaluation of a strengths-based cbt intervention module with college students. Behav. Cogn. Psychother. 2017, 45, 427–431. [Google Scholar] [CrossRef]
- Krispenz, A.; Dickhäuser, O. Effects of an inquiry-based short intervention on state test anxiety in comparison to alternative coping strategies. Front. Psychol. 2018, 9, 201. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.; McIntyre, R.; Rimes, K.A. Compassion-focused intervention for highly self-critical individuals: Pilot study. Behav. Cogn. Psychother. 2018, 46, 583–600. [Google Scholar] [CrossRef] [PubMed]
- Binder, P.E.; Dundas, I.; Stige, S.H.; Hjeltnes, A.; Woodfin, V.; Moltu, C. Becoming aware of inner self-critique and kinder toward self: A Qualitative study of experiences of outcome after a brief self-compassion intervention for university level students. Front. Psychol. 2019, 10, 2728. [Google Scholar] [CrossRef] [PubMed]
- Matteucci, M.C. Attributional retraining and achievement goals: An exploratory study on theoretical and empirical relationship. Eur. Rev. Appl. Psychol. 2017, 67, 279–289. [Google Scholar] [CrossRef]
- Marksteiner, T.; Janke, S.; Dickhäuser, O. Effects of a brief psychological intervention on students’ sense of belonging and educational outcomes: The role of students’ migration and educational background. J. Sch. Psychol. 2019, 75, 41–57. [Google Scholar] [CrossRef]
- Pinto, J.C.; Loureiro, N.; Taveira, M. Psychological intervention in portuguese college students: Effects of two career self-management seminars. J. Coll. Stud. Dev. 2015, 56, 518–524. [Google Scholar] [CrossRef]
- Otermin-Cristeta, S.; Hautzinger, M. Developing an intervention to overcome procrastination. J. Prev. Interv. Community 2018, 46, 171–183. [Google Scholar] [CrossRef]
- Härkäpää, K.; Junttila, O.; Lindfors, O.; Jarvikoski, A. Changes in studying abilities as perceived by students attending psychotherapy. Br. J. Guid. Couns. 2014, 42, 166–180. [Google Scholar] [CrossRef]
- Ciucur, D. A Transactional analysis group psychotherapy programme for improving the qualities and abilities of future psychologists. Procedia Soc. Behav. Sci. 2013, 78, 576–580. [Google Scholar] [CrossRef]
- Ostafin, B.D.; Palfai, T.P. When wanting to change is not enough: Automatic appetitive processes moderate the effects of a brief alcohol intervention in hazardous-drinking college students. Addict. Sci. Clin. Pract. 2012, 7, 25. [Google Scholar] [CrossRef]
- McClatchey, K.; Boyce, M.; Dombrowski, S.U. Alcohol Brief Intervention in a university setting: A small-scale experimental study. J. Health Psychol. 2017, 22, 886–895. [Google Scholar] [CrossRef] [PubMed]
- Clarke, N.C.; Field, M.; Rose, A.K. Evaluation of a brief personalised intervention for alcohol consumption in college students. PLoS ONE 2015, 10, e0131229. [Google Scholar] [CrossRef] [PubMed]
- Grajfoner, D.; Harte, E.; Potter, L.M.; McGuigan, N. The effect of dog-assisted intervention on student well-being, mood, and anxiety. Int. J. Environ. Res. Public Health 2017, 14, 483. [Google Scholar] [CrossRef] [PubMed]
- Wood, E.; Ohlsen, S.; Thompson, J.; Hulin, J.; Knowles, L. The feasibility of brief dog-assisted therapy on university students stress levels: The PAwS study. J. Ment. Health 2018, 27, 263–268. [Google Scholar] [CrossRef]
- Lynch, S.; Gander, M.; Nahar, A.; Kohls, N.; Walach, H. Mindfulness-Based coping with university life: A randomized wait-list controlled study. Sage Open 2018, 8, 1–7. [Google Scholar] [CrossRef]
- Ștefan, C.A.; Căpraru, C.; Szilágyi, M. Investigating effects and mechanisms of a mindfulness-based stress reduction intervention in a sample of college students at risk for social anxiety. Mindfulness 2018, 9, 1509–1521. [Google Scholar] [CrossRef]
- Halland, E.; De Vibe, M.; Solhaug, I.; Friborg, O.; Rosenvinge, J.H.; Tyssen, R.; Sørlie, T.; Bjørndal, A. Mindfulness training improves problem-focused coping in psychology and medical students: Results from a randomized controlled trial. Coll. Stud. J. 2015, 49, 387–398. [Google Scholar]
- Gallego, J.; Aguilar-Parra, J.M.; Cangas, A.J.; Langer, Á.I.; Mañas, I. Effect of a mindfulness program on stress, anxiety and depression in university students. Span. J. Psychol. 2015, 17, E109. [Google Scholar] [CrossRef]
- Shuai, R.; Bakou, A.E.; Hardy, L.; Hogarth, L. Ultra-brief breath counting (mindfulness) training promotes recovery from stress-induced alcohol-seeking in student drinkers. Addict. Behav. 2020, 102, 106141. [Google Scholar] [CrossRef]
- Haukaas, R.B.; Gjerde, I.B.; Varting, G.; Hallan, H.E.; Solem, S. A randomized controlled trial comparing the attention training technique and mindful self-compassion for students with symptoms of depression and anxiety. Front. Psychol. 2018, 9, 827. [Google Scholar] [CrossRef]
- Recabarren, R.E.; Gaillard, C.; Guillod, M.; Martin-Soelch, C. Short-Term effects of a multidimensional stress prevention program on quality of life, well-being and psychological resources. A randomized controlled trial. Front. Psychol. 2019, 10, 88. [Google Scholar] [CrossRef] [PubMed]
- Räsänen, P.; Lappalainen, P.; Muotka, J.; Tolvanen, A.; Lappalainen, R. An online guided ACT intervention for enhancing the psychological wellbeing of university students: A randomized controlled clinical trial. Behav. Res. Ther. 2016, 78, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Turner, L.; Galante, J.; Vainre, M.; Stochl, J.; Dufour, G.; Peter, B. Immune dysregulation among students exposed to exam stress and its mitigation by mindfulness training: Findings from an exploratory randomised trial. Sci. Rep. 2020, 10, 5812. [Google Scholar] [CrossRef] [PubMed]
- Kvillemo, P.; Brandberg, Y.; Bränström, R. Feasibility and outcomes of an internet-based mindfulness training program: A pilot randomized controlled trial. JMIR Ment. Health 2016, 3, e33. [Google Scholar] [CrossRef]
- Epton, T.; Norman, P.; Dadzie, A.-S.; Harris, P.R.; Webb, T.L.; Sheeran, P.; Julious, S.A.; Ciravegna, F.; Brennan, A.; Meier, P.S. A theory-based online health behaviour intervention for new university students (U@Uni): Results from a randomised controlled trial. BMC Public Health 2014, 14, 563. [Google Scholar] [CrossRef]
- Cameron, D.; Epton, T.; Norman, P.; Sheeran, P.; Harris, P.R.; Webb, T.L.; Julious, S.A.; Brennan, A.; Thomas, C.; Petroczi, A. A theory-based online health behaviour intervention for new university students (U@Uni:LifeGuide): Results from a repeat randomized controlled trial. Trials 2015, 16, 555. [Google Scholar] [CrossRef]
- Lindenberg, K.; Moessner, M.; Harney, J.; McLaughlin, O.; Bauer, S. E-health for individualized prevention of eating disorders. Clin. Pract. Epidemiol. Ment. Health 2011, 7, 74–83. [Google Scholar] [CrossRef][Green Version]
- Richards, D.; Timulak, L.; Rashleigh, C.; McLoughlin, O.; Colla, A.; Joyce, C.; Doherty, G.; Sharry, J.; Duffy, D.; Anderson-Gibbons, M. Effectiveness of an internet-delivered intervention for generalized anxiety disorder in routine care: A randomised controlled trial in a student population. Internet Interv. 2016, 6, 80–88. [Google Scholar] [CrossRef]
- Cook, L.; Mostazir, M.; Watkins, E. Reducing Stress and Preventing Depression (RESPOND): Randomized controlled trial of web-based rumination-focused cognitive behavioral therapy for high-ruminating university students. J. Med. Internet Res 2019, 21, e11349. [Google Scholar] [CrossRef]
- Sharry, J.; Davidson, R.; McLoughlin, O.; Doherty, G. A service-based evaluation of a therapist-supported online cognitive behavioral therapy program for depression. J. Med. Internet Res 2013, 15, e121. [Google Scholar] [CrossRef]
- Saleh, D.; Camart, N.; Sbeira, F.; Romo, L. Can we learn to manage stress? A randomized controlled trial carried out on university students. PLoS ONE 2018, 13, e0200997. [Google Scholar] [CrossRef] [PubMed]
- Horgan, A.; McCarthy, G.; Sweeney, J. An evaluation of an online peer support forum for university students with depressive symptoms. Arch. Psychiatr. Nurs. 2013, 27, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Kählke, F.; Berger, T.; Schulz, A.; Baumeister, H.; Berking, M.; Cuijpers, P.; Bruffaerts, R.; Auerbach, R.P.; Kessler, R.C.; Ebert, D.D. Efficacy and cost-effectiveness of an unguided, internet-based self-help intervention for social anxiety disorder in university students: Protocol of a randomized controlled trial. BMC Psychiatry 2019, 19, e1766. [Google Scholar] [CrossRef]
- Bruijniks, S.; Sijbrandij, M.; Huibers, M. The effects of retrieval versus rehearsal of online problem-solving therapy sessions on recall, problem-solving skills and distress in distressed individuals: An experimental study. J. Behav. Ther. Exp. Psychiatry 2019, 66, 101485. [Google Scholar] [CrossRef] [PubMed]
- Canale, N.; Vieno, A.; Santinello, M.; Chieco, F.; Andriolo, S. The efficacy of computerized alcohol intervention tailored to drinking motives among college students: A quasi-experimental pilot study. Am. J. Drug Alcohol Abuse 2015, 41, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Bewick, B.M.; West, R.; Gill, J.; O’May, F.; Mulhern, B.; Barkham, M.; Hill, A.J. Providing web-based feedback and social norms information to reduce student alcohol intake: A multisite investigation. J. Med. Internet Res. 2010, 12, e59. [Google Scholar] [CrossRef]
- Bewick, B.M.; West, R.M.; Barkham, M.; Mulhern, B.; Marlow, R.; Traviss, G.; Hill, A.J. The effectiveness of a Web-based personalized feedback and social norms alcohol intervention on United Kingdom university students: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e137. [Google Scholar] [CrossRef]
- Tello, N.; Bocage-Barthélémy, Y.; Dandaba, M.; Jaafari, N.; Chatard, A. Evaluative conditioning: A brief computer-delivered intervention to reduce college student drinking. Addict. Behav. 2018, 82, 14–18. [Google Scholar] [CrossRef]
- Norman, P.; Cameron, D.; Epton, T.; Webb, T.L.; Harris, P.R.; Millings, A.; Sheeran, P. A randomized controlled trial of a brief online intervention to reduce alcohol consumption in new university students: Combining self-affirmation, theory of planned behaviour messages, and implementation intentions. Br. J. Health Psychol. 2018, 23, 108–127. [Google Scholar] [CrossRef]
- Broglia, E.; Millings, A.; Barkham, M. Counseling with guided use of a mobile well-being app for students experiencing anxiety or depression: Clinical outcomes of a feasibility trial embedded in a student counseling service. JMIR mHealth uHealth 2019, 7, e14318. [Google Scholar] [CrossRef]
- Harrer, M.; Adam, S.H.; Fleischmann, R.J.; Baumeister, H.; Auerbach, R.; Bruffaerts, R.; Cuijpers, P.; Kessler, R.C.; Berking, M.; Lehr, D.; et al. Effectiveness of an internet- and app-based intervention for college students with elevated stress: Randomized controlled trial. J. Med. Internet Res. 2018, 20, e136. [Google Scholar] [CrossRef] [PubMed]
- Ponzo, S.; Morelli, D.; Kawadler, J.M.; Hemmings, N.R.; Bird, G.; Plans, D. Efficacy of the digital therapeutic mobile app biobase to reduce stress and improve mental well-being among university students: Randomized controlled trial. JMIR mHealth uHealth 2020, 8, e17767. [Google Scholar] [CrossRef] [PubMed]
- Richards, D.; Timulak, L.; Hevey, D. A comparison of two online cognitive-behavioural interventions for symptoms of depression in a student population: The role of therapist responsiveness. Couns. Psychother. Res 2012, 13. [Google Scholar] [CrossRef]
- Pérez-Jorge, D.; Barragán-Medero, F.; Gutiérrez-Barroso, J.; Castro-León, F. A synchronous tool for innovation and improvement of university communication, counseling and tutoring: The WhatsApp experience. Eurasia J. Math. Sci. Technol. Educ. 2018, 14, 2737–2743. [Google Scholar] [CrossRef]
- Bendtsen, M.; Müssener, U.; Linderoth, C.; Thomas, K. A mobile health intervention for mental health promotion among university students: Randomized controlled Trial. JMIR mHealth uHealth 2020, 8, e17208. [Google Scholar] [CrossRef]
- Noone, C.; Hogan, M.J. A randomised active-controlled trial to examine the effects of an online mindfulness intervention on executive control, critical thinking and key thinking dispositions in a university student sample. BMC Psychol. 2018, 6, 13. [Google Scholar] [CrossRef]
- Gajecki, M.; Andersson, C.; Rosendahl, I.; Sinadinovic, K.; Fredriksson, M.; Berman, A.H. Skills training via smartphone app for university students with excessive alcohol consumption: A randomized controlled trial. Int. J. Behav. Med. 2017, 24, 778–788. [Google Scholar] [CrossRef]
- Bendtsen, M.; Bendtsen, P. Feasibility and user perception of a fully automated push-based multiple-session alcohol intervention for university students: Randomized controlled trial. JMIR mHealth uHealth 2014, 2, e30. [Google Scholar] [CrossRef]
- Müssener, U.; Bendtsen, M.; Karlsson, N.; White, I.R.; McCambridge, J.; Bendtsen, P. Effectiveness of short message service text-based smoking cessation intervention among university students: A randomized clinical trial. JAMA Intern. Med. 2016, 176, 321–328. [Google Scholar] [CrossRef]
- Cheng, H.L.; Wang, C.; McDermott, R.C.; Kridel, M.; Rislin, J.L. Self-stigma, mental health literacy, and attitudes toward seeking psychological help. J. Couns. Dev. 2018, 96, 64–74. [Google Scholar] [CrossRef]
- Baik, C.; Larcombe, W.; Brooker, A. How universities can enhance student mental wellbeing: The student perspective. High. Educ. Res. Dev. 2019, 38, 674–687. [Google Scholar] [CrossRef]
- Oswalt, S.B.; Lederer, A.M.; Chestnut-Steich, K.; Day, C.; Halbritter, A.; Ortiz, D. Trends in college students’ mental health diagnoses and utilization of services, 2009–2015. J. Am. Coll. Health 2020, 68, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Wilson, O.W.; Bopp, C.M.; Papalia, Z.; Duffey, M.; Bopp, M. College Students’ Experiences and Attitudes Toward Physical Activity Counseling. J. Nurse Pract. 2020, 16, 623–628. [Google Scholar] [CrossRef]
- Garza, K.B.; Hohmann, N.S.; Kavookjian, J.; Kleppinger, E.L. Assessment of student performance on a mock new prescription counseling session and an objective structured clinical examination across five years. Curr. Pharm. Teach. Learn. 2020, 12, 1046–1055. [Google Scholar] [CrossRef] [PubMed]
- Broglia, E.; Millings, A.; Barkham, M. Challenges to addressing student mental health in embedded counseling services: A survey of UK higher and further education institutions. Br. J. Guid. Couns. 2018, 46, 441–455. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Mental Health, Substance Use, and Wellbeing in Higher Education: Supporting the Whole Student; The National Academies Press: Washington, DC, USA, 2021. [Google Scholar] [CrossRef]
- Woolston, C. ‘The problem is greater than it’s ever been’: US universities urged to invest in mental-health resources. Nature 2021, 590, 171–172. [Google Scholar] [CrossRef]
- Sun, S.; Goldberg, S.B.; Lin, D.; Qiao, S.; Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Glob. Health 2021, 17, 15. [Google Scholar] [CrossRef]
- Husky, M.M.; Kovess-Masfety, V.; Swendsen, J.D. Stress and anxiety among university students in France during COVID-19 mandatory confinement. Compr. Psychiatry 2020, 102, 152191. [Google Scholar] [CrossRef]
- Anderson, G.; Coping with a Pandemic. Inside Higher Ed. 31 March 2020. Available online: https://www.insidehighered.com/news/2020/03/31/mental-health-support-systems-coping-pandemic (accessed on 4 April 2022).
- Martinez, A.; Nguyen, S. The Impact of COVID-19 on College Student Well-Being. ACHA. 31 March 2020. Available online: http://hdl.handle.net/10919/99741 (accessed on 4 April 2022).
- Benton, S.A.; Robertson, J.M.; Tseng, W.C.; Newton, F.B.; Benton, S.L. Changes in counseling center client problems across 13 years. Prof. Psychol. Res. Pract. 2003, 34, 66. [Google Scholar] [CrossRef]
- Berger, H.; Franke, G.H.; Hofmann, F.H.; Sperth, M.; Holm-Hadulla, R.M. Mental health of students and its development between 1994 and 2012. Ment. Health Prev. 2015, 3, 48–56. [Google Scholar] [CrossRef]
- Connell, J.; Barkham, M.; Mellor-Clark, J. The effectiveness of UK student counseling services: An analysis using the CORE System. Br. J. Guid. Couns. 2008, 36, 1–18. [Google Scholar] [CrossRef]
- Buchanan, B.G.; Le, Q.V.; Rishi, M. Foreign direct investment and institutional quality: Some empirical evidence. IRFA 2012, 21, 81–89. [Google Scholar] [CrossRef]
- Granieri, A.; Guglielmucci, F.; Costanzo, A.; Caretti, V.; Schimmenti, A. Trauma-Related Dissociation Is Linked with Maladaptive Personality Functioning. Front. Psychol. 2018, 9, 206. [Google Scholar] [CrossRef] [PubMed]
- Sommantico, M.; de Rosa, B.; Parrello, S. Counseling University Students: A Psychoanalytic Approach. Mediterr. J. Clin. Psychol. 2017, 5. [Google Scholar] [CrossRef]
- Baskin, T.W.; Slaten, C.D.; Sorenson, C.; Glover-Russell, J.; Merson, D.N. Does youth psychotherapy improve academically related outcomes? A meta-analysis. J. Couns. Psychol. 2010, 57, 290–296. [Google Scholar] [CrossRef]
- Regehr, C.; Glancy, D.; Pitts, A. Interventions to reduce stress in university students: A review and meta-analysis. J. Affect. Disord. 2013, 148, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Adamo, S.M.G.; Sarno, I.; Preti, E.; Fontana, R.M.; Prunas, A. Brief psychodynamic counseling in a university setting. Procedia Soc. 2010, 5, 1151–1159. [Google Scholar] [CrossRef]
- Andersson, C.; Johnsson, K.O.; Berglund, M.; Ojehagen, A. Alcohol involvement in Swedish university freshmen related to gender, age, serious relationship and family history of alcohol problems. Alcohol Alcohol. 2007, 42, 448–455. [Google Scholar] [CrossRef]
- Engs, R.C.; Diebold, B.A.; Hanson, D.J. The drinking patterns and problems of a national sample of college students, 1994. Alcohol Drug Educ. 1996, 41, 13–33. [Google Scholar]
- Heather, N.; Partington, S.; Partington, E.; Longstaff, F.; Allsop, S.; Jankowski, M.; Wareham, H.; St Clair Gibson, A. Alcohol use disorders and hazardous drinking among undergraduates at english universities. Alcohol Alcohol. 2011, 46, 270–277. [Google Scholar] [CrossRef]
- Butler, L.H.; Correia, C.J. Brief alcohol intervention with college student drinkers: Face-to-face versus computerized feedback. Psychol. Addict. Behav 2009, 23, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Carey, R.O.; Migliaccio, K.W.; Li, Y.; Schaffer, B.; Kiker, G.A.; Brown, M.T. Land use disturbance indicators and water quality variability in the Biscayne Bay Watershed, Florida. Ecol. Indic. 2011, 11, 1093–1104. [Google Scholar] [CrossRef]
- Schaus, J.F.; Sole, M.L.; McCoy, T.P.; Mullett, N.; O’Brien, M.C. Alcohol screening and brief intervention in a college student health center: A randomized controlled trial. JSAD 2009, s16, 131–142. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Palfai, T.P.; Zisserson, R.; Saitz, R. Using personalized feedback to reduce alcohol use among hazardous drinking college students: The moderating effect of alcohol-related negative consequences. Addict. Behav. 2011, 36, 539–542. [Google Scholar] [CrossRef]
- Bewick, B.; Koutsopoulou, G.; Miles, J.; Slaa, E.; Barkham, M. Changes in undergraduate students’ psychological well-being as they progress through university. Stud. High Educ. 2010, 35, 633–645. [Google Scholar] [CrossRef]
- Albaladejo, C.B.; Aznar, A.B.; Cabañero, M.C.; Pérez, N.F.; Pastor, E.I.; Carbonell, S.J.; Fuentes, M.M.M.; Martín, A.R.; Gómez, B.R. Educación y Asesoramiento del Alumno Para el Correcto uso de las Tutorías. [Formazione e Consulenza dello Studente per il Corretto Utilizzo dei Tutor]. Investigación y Propuestas Innovadoras de Redes UA Para la Mejora Docente, 2015, pp. 204–218. Available online: http://hdl.handle.net/10045/48606 (accessed on 13 April 2022).
- García, D. M-Learning. Posibilidades Educativas de Whatsapp. 2014. Available online: https://www.youtube.com/watch?v=vMtU4ZdW264 (accessed on 13 April 2022).
- Garzozi, R. Experiencia del uso de las TIC en la tutoría del trabajo final de titulación de la Maestría de Auditoría Integral. [Esperienza nell’utilizzo delle ICT nel tutoraggio del progetto di laurea finale del Master in Auditing Integrale]. In Proceedings of the Conferencias LACLO, Maceió, Brazil, 26–30 October 2015, 6, p. 351. Available online: http://brie.org/pub/index.php/teste/article/view/5818/4108 (accessed on 4 April 2022).
- Gómez, B.R.; Albaladejo, C.B.; Cabañero, M.C.; Pérez, N.F.; Pastor, E.I.; Carbonell, S.J.; Fuentes, M.M.; Aznar, A.B. La Adquisición de Competencias y su Evaluación a Través de la Participación del Alumno. [L’Acquisizione di Competenze e la loro Valutazione Attraverso la Partecipazione dello Studente]. XIII Jornadas de Redes de Investigación en Docencia Universitaria 2015, pp. 2560–2574. Available online: http://hdl.handle.net/10045/48708 (accessed on 13 April 2022).
- Sanz, J.J. Whatsapp: Potencialidad Educativa versus Dependencia y Adicción. 2014 [WhatsApp: Potenziale Educativo Contro Dipendenza e Dipendenza]. Available online: http://dim.pangea.org/revistaDIM30/docs/OC30whatsapp.pdf (accessed on 13 April 2022).
- Bränström, R. Minority stress factors as mediators of sexual orientation disparities in mental health treatment: A longitudinal population-based study. J. Epidemiol. Community Health 2016, 71, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Savarese, G.; Curcio, L.; D’Elia, D.; Fasano, O.; Pecoraro, N. Online University Counseling Services and Psychological Problems among Italian Students in Lockdown Due to COVID-19. Healthcare 2020, 8, 440. [Google Scholar] [CrossRef]
- El Morr, C.; Ritvo, P.; Ahmad, F.; Moineddin, R. Effectiveness of an 8-Week Web-Based Mindfulness Virtual Community Intervention for University Students on Symptoms of Stress, Anxiety, and Depression: Randomized Controlled Trial. JMIR Ment. Health 2020, 7, e18595. [Google Scholar] [CrossRef]
- Liu, S.; Yang, L.; Zhang, C.; Xiang, Y.T.; Liu, Z.; Hu, S.; Zhang, B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e17–e18. [Google Scholar] [CrossRef]
- Priestley, M.; Broglia, E.; Hughes, G.; Spanner, L. Student Perspectives on improving mental health support Services at university. Couns. Psychother. Res. 2021, 22, 1–10. [Google Scholar] [CrossRef]
- Pinto, J.C.; Faria, L.; Pinto, H.R.; Taveira, M.D.C. Identificação de necessidades de intervenção psicológica: Um estudo-piloto no ensino superior português. Psicol. USP 2016, 27, 459–472. [Google Scholar] [CrossRef]
- Seppälä, E.M.; Bradley, C.; Moeller, J.; Harouni, L.; Nandamudi, D.; Brackett, M.A. Promoting Mental Health and Psychological Thriving in University Students: A Randomized Controlled Trial of Three Well-Being Interventions. Front. Psychiatry 2020, 11, 590. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franzoi, I.G.; Sauta, M.D.; Barbagli, F.; Avalle, C.; Granieri, A. Psychological Interventions for Higher Education Students in Europe: A Systematic Literature Review. Youth 2022, 2, 236-257. https://doi.org/10.3390/youth2030017
Franzoi IG, Sauta MD, Barbagli F, Avalle C, Granieri A. Psychological Interventions for Higher Education Students in Europe: A Systematic Literature Review. Youth. 2022; 2(3):236-257. https://doi.org/10.3390/youth2030017
Chicago/Turabian StyleFranzoi, Isabella Giulia, Maria Domenica Sauta, Francesca Barbagli, Cristiana Avalle, and Antonella Granieri. 2022. "Psychological Interventions for Higher Education Students in Europe: A Systematic Literature Review" Youth 2, no. 3: 236-257. https://doi.org/10.3390/youth2030017
APA StyleFranzoi, I. G., Sauta, M. D., Barbagli, F., Avalle, C., & Granieri, A. (2022). Psychological Interventions for Higher Education Students in Europe: A Systematic Literature Review. Youth, 2(3), 236-257. https://doi.org/10.3390/youth2030017






