Use of Patterns of Service Utilization and Hierarchical Survival Analysis in Planning and Providing Care for Overdose Patients and Predicting the Time-to-Second Overdose
Abstract
1. Introduction
1.1. Use of Patterns of Service Utilization in Planning and Providing Care to Complex Patients
1.2. Evidence-Based Care: Machine Learning and Statistical Analysis
1.3. Objectives
- Using PSUs, to what extent can we determine whether the opioid overdose cohort is homogeneous or not with respect to determinants of risk?
- How many communities constitute the opioid overdose cohort, based on how patients within this cohort interact with the host organization’s cross-continuum service system?
- To what extent can we determine the risk of a subsequent opioid overdose based on the community an opioid overdose patient belongs to and quantify it using survival analysis?
2. Methods
2.1. Addressing Data Granularity Issues
2.2. Community Detection
2.3. Survival Models
2.4. Combining Community Detection and Survival Analysis
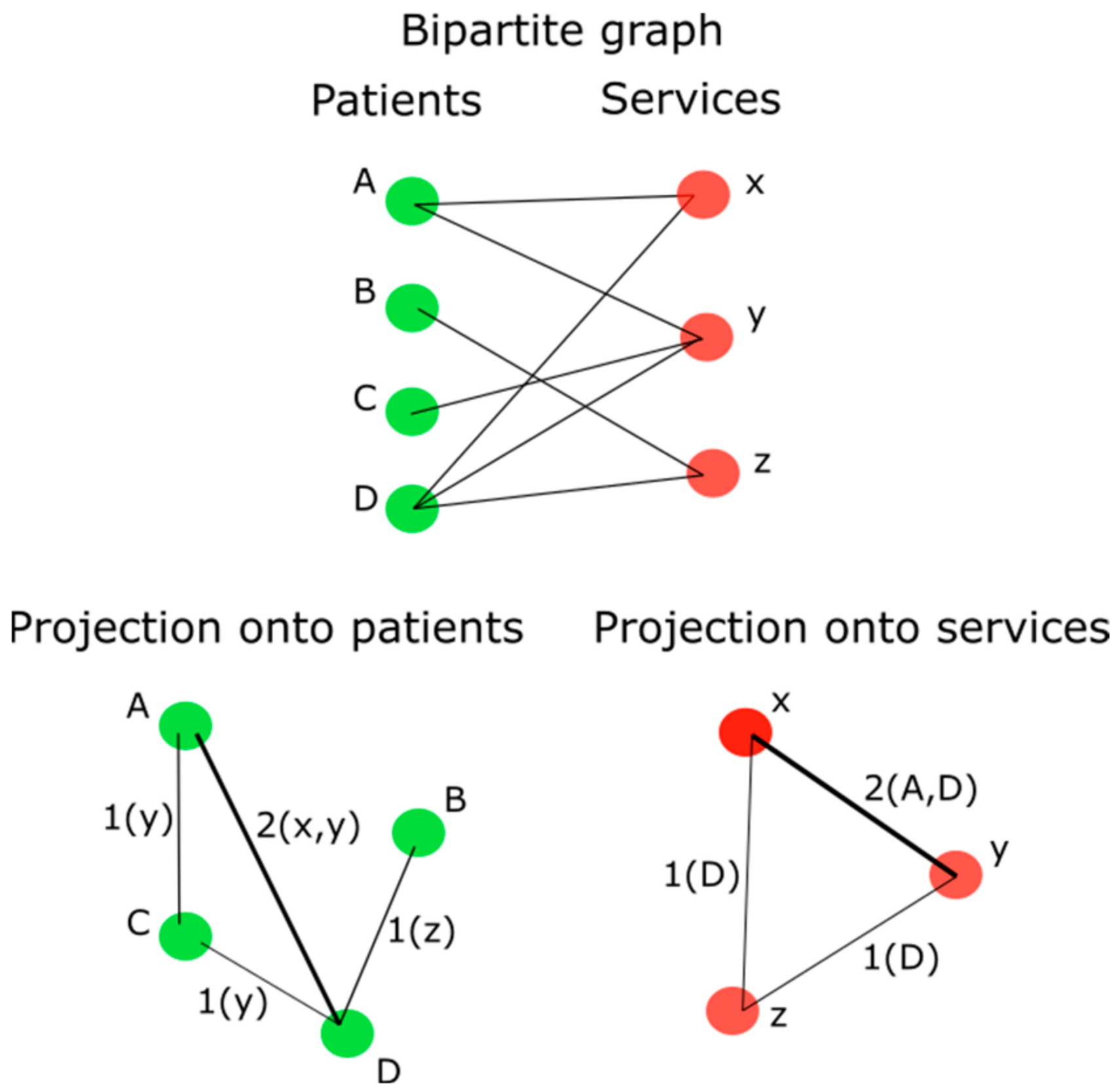
- The encounter data were engineered as a bipartite graph consisting of nodes with edges connecting patients to Service Classes. A patient (node) is connected to a Service Class (node) when they use a service represented by the Service Class. Recall that roughly two hundred Service Classes employed for modeling in this paper consist of equivalence classes formed by the application of six code sets to the host organization Service Units to reduce granularity.
- A bipartite projection onto patients was applied (Figure 1) to the bipartite graph to create a weighted graph, where the number of services that were used by two connected patients became the weight of the edge.
- The Louvain community detection algorithm was applied to the weighted graph to uncover the communities of patients that reflect high-prevalent PSUs by Service Classes.
- For each of the generated communities, both the service engagement profile and the diagnosis profile were appended.
- Collaborating with team members with clinical backgrounds, each community of patients was labeled based on their prevalent service engagement and diagnosis profile.
- Using community belonging as a characteristic of a patient, survival analysis was used to quantify the risk of a second overdose.
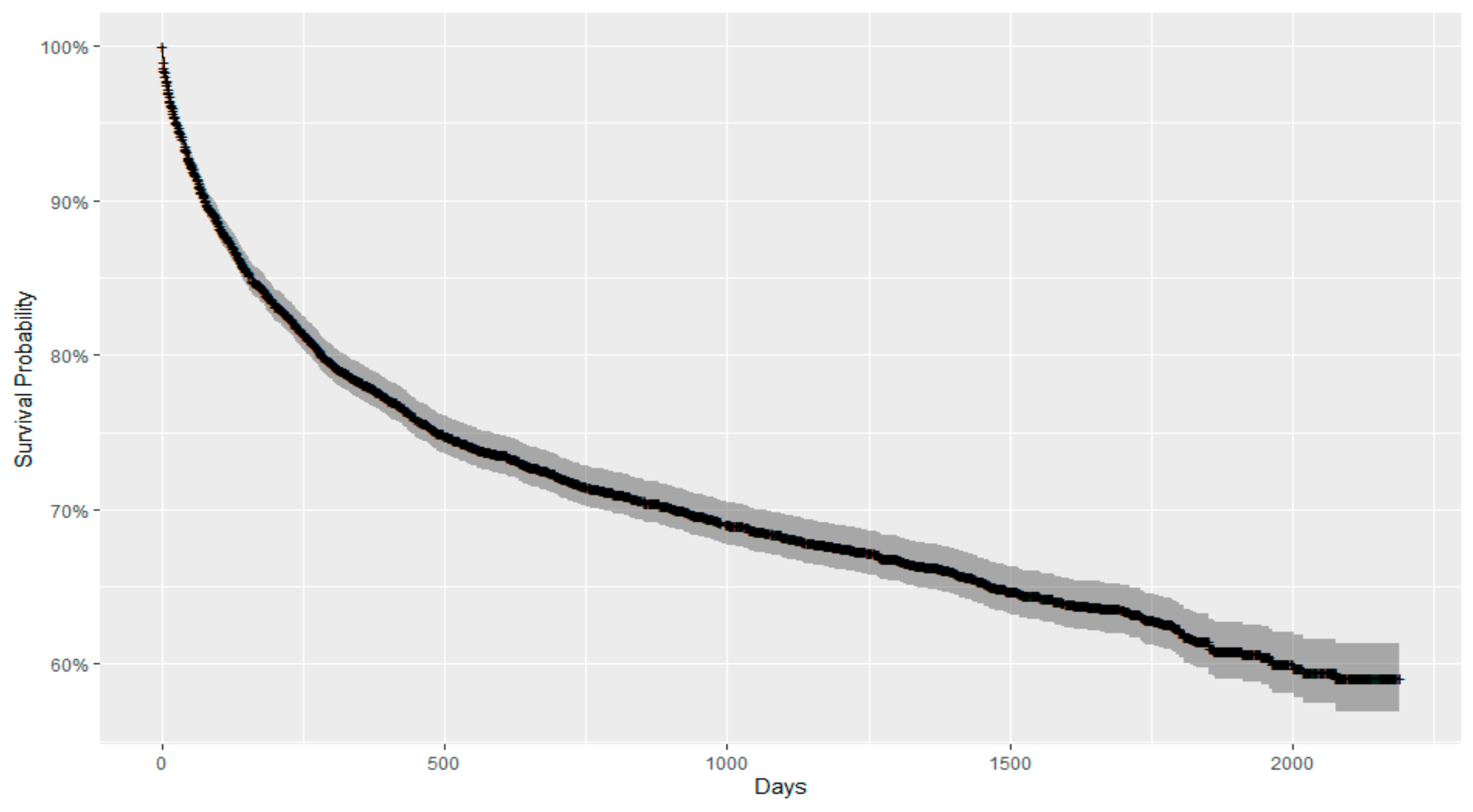
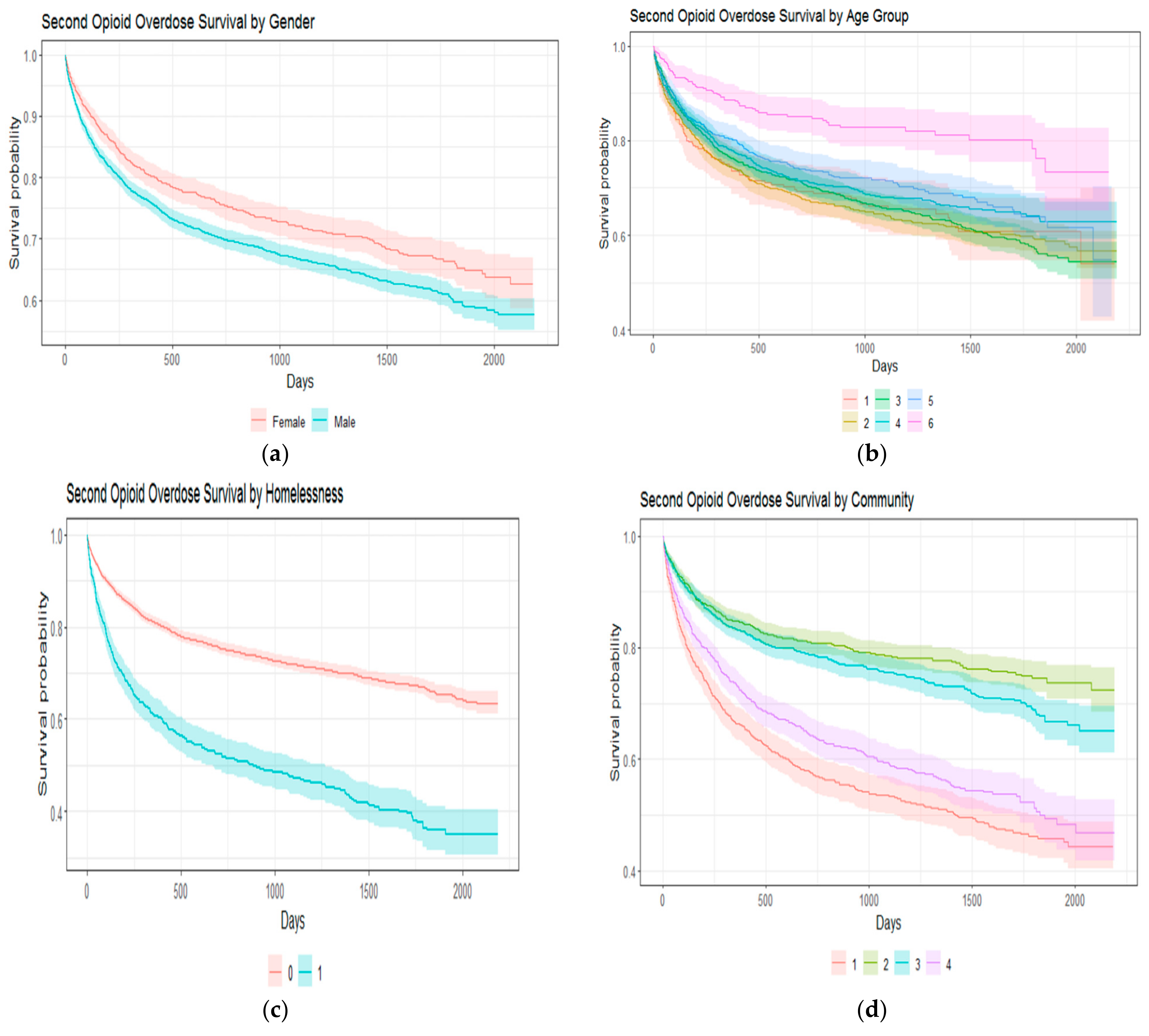
- Using other patient-related characteristics, such as age, gender, and homelessness status, survival analysis was used to further quantify the risk of a second overdose.
3. Analysis
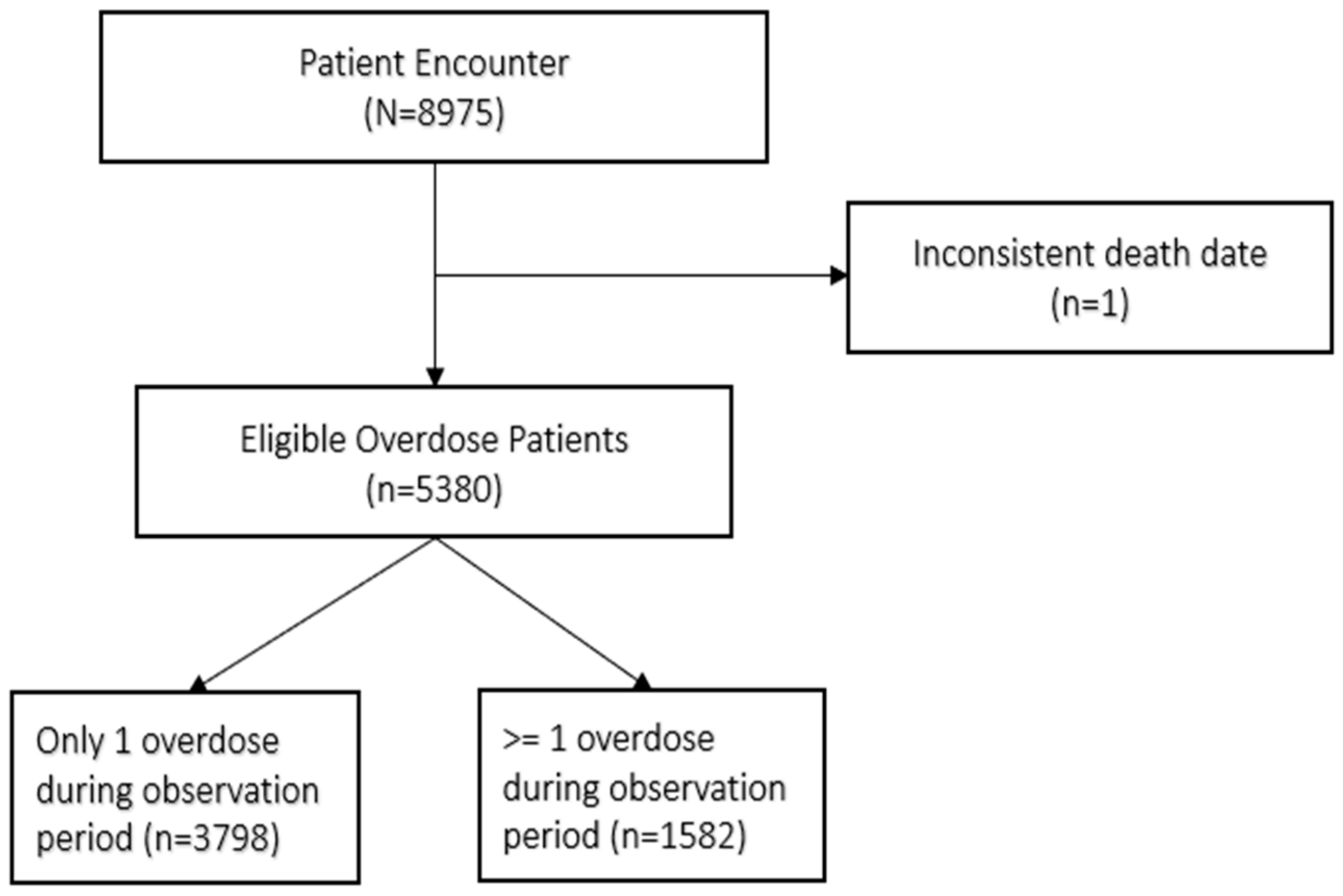
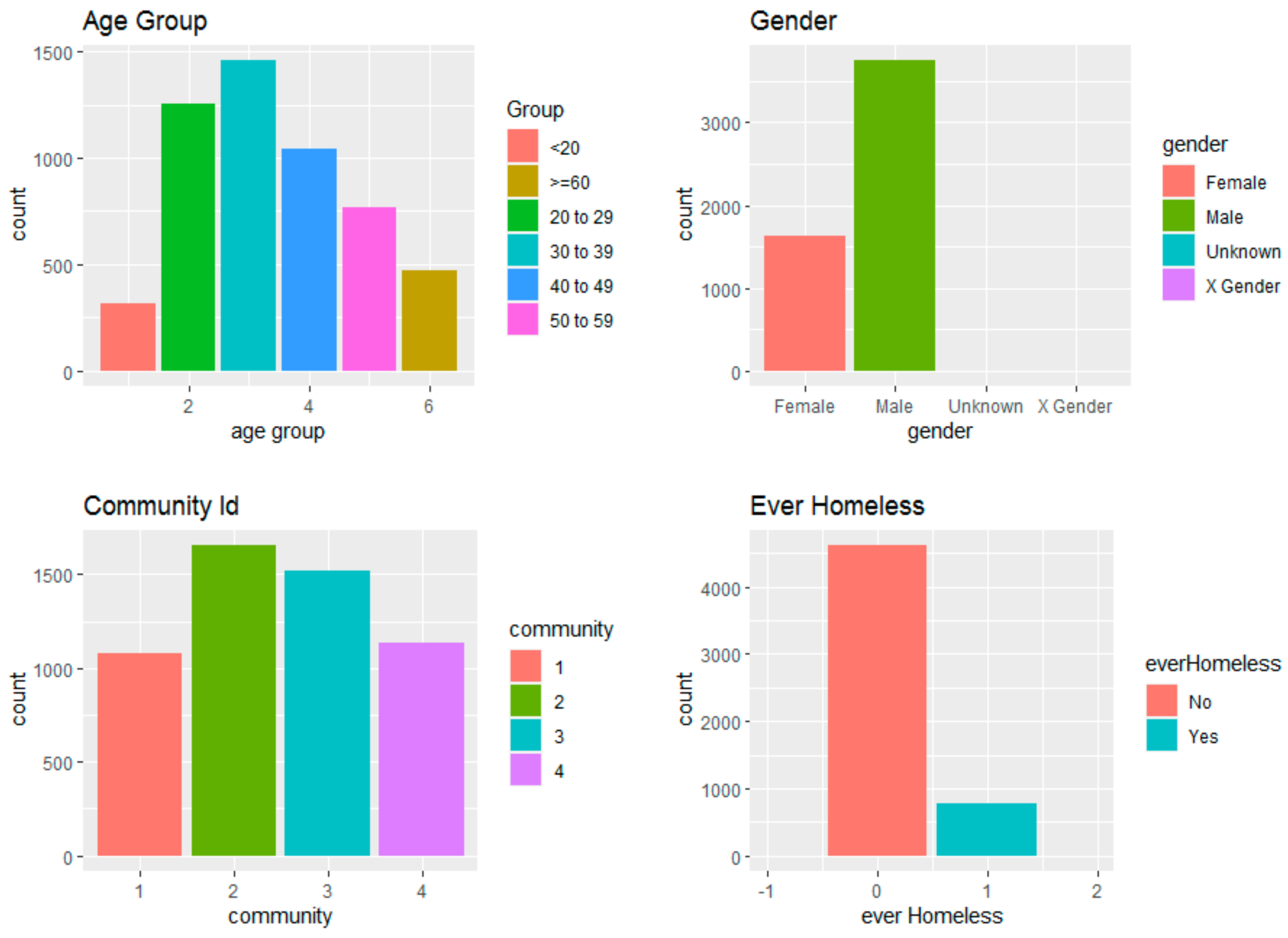
3.1. Patient Characteristics
3.2. Community Characteristics
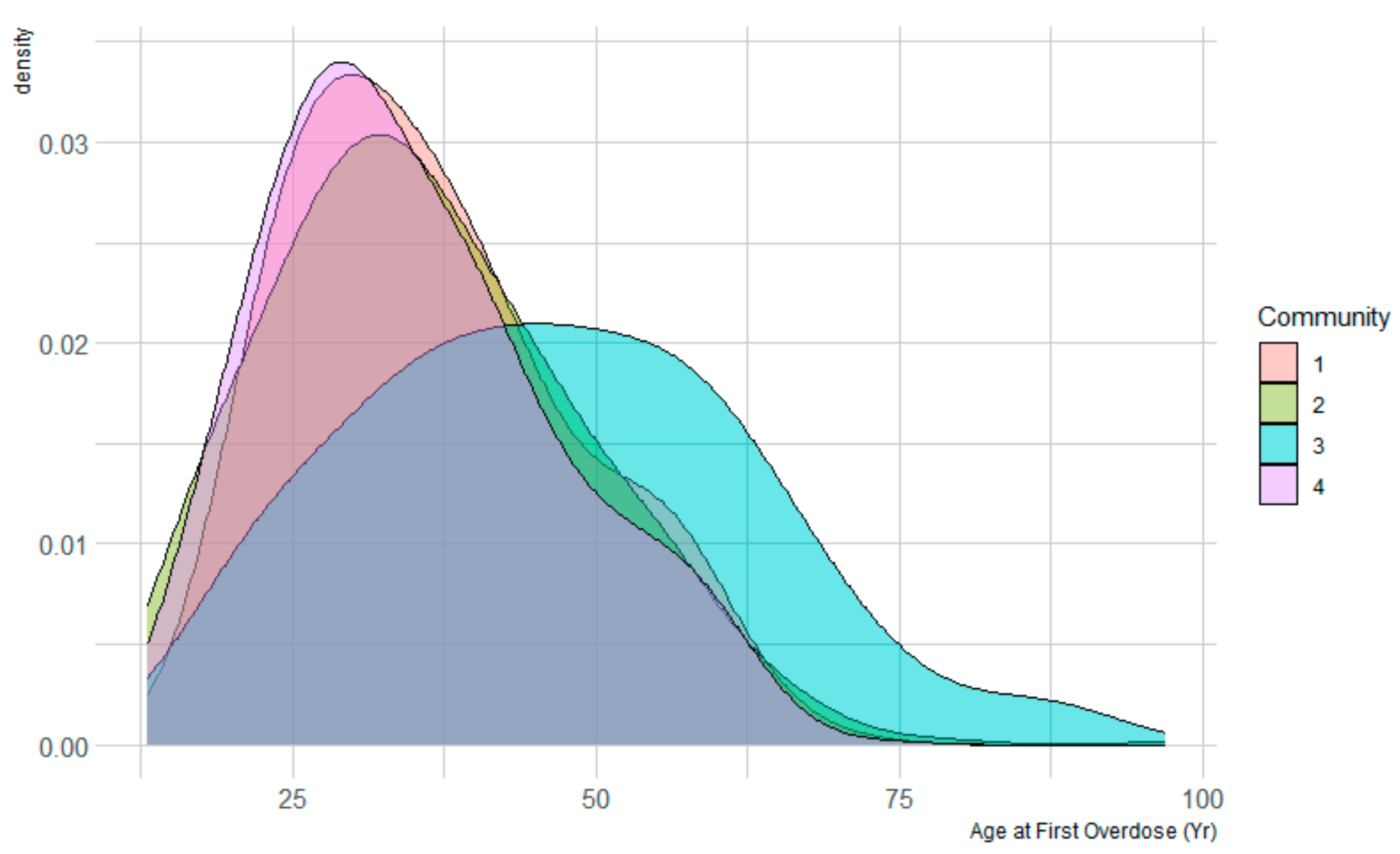
- Community one, termed the “reciprocal group”, exhibited a proactive approach to accessing health services, for example, self-referred ambulatory addiction services. They demonstrated higher utilization rates within the service system overall, including Mental Health, and Substance Use (MHSU) and Medical/Surgical (Med/Surg) services. Notably, 80% of patients in this community utilized MHSU clinical intake and addiction clinical intake services. Predominant diagnoses within this group centered around severe addiction issues, with minimal occurrences of schizophrenia-related diagnoses. The average age of patients in this community was years.
- Community two, characterized as the “service-disengaged group”, displayed lower engagement with the service system compared to other communities. They accessed overdose-related and addiction outreach services prior to the overdose events. Diagnostic profiles within this group were not pronounced, with only 8% reporting homelessness and an average age of years.
- Community three, labeled as the “group with complex/serious health problems”, exhibited a higher frequency of encounters with Med/Surg services, particularly laboratory and medical imaging procedures. Engagement with MHSU services was comparatively lower, indicating that their engagement with the service system focused on addressing complex medical conditions rather than substance use. Diagnostic data suggested a variety of medical issues, including high rates of palliative care and alterations of awareness. The average age within this community was 46 years, with a considerable number of patients being 60 years or older.
- Community four, characterized as the “group with severe psychiatric issues”, demonstrated a high engagement with psychiatric services but low involvement with addiction services. This group exhibited a younger average age of 35 years and a notably high prevalence of schizophrenia diagnoses. Engagement with MHSU services was more prominent than with Med/Surg services.
3.3. Statistical Analyses
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dalgleish, T.; Black, M.; Johnston, D.; Bevan, A. Transdiagnostic approaches to mental health problems: Current status and future directions. J. Consult. Clin. Psychol. 2020, 88, 179–195. (In English) [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Berkman, L. Social cohesion, social capital, and health. Soc. Epidemiol. 2000, 174, 290–319. [Google Scholar]
- Chandler, R.K.; Villani, J.; Clarke, T.; McCance-Katz, E.F.; Volkow, N.D. Addressing opioid overdose deaths: The vision for the HEALing communities study. Drug Alcohol Depend. 2020, 217, 108329. [Google Scholar] [CrossRef] [PubMed]
- Larochelle, M.R.; Slavova, S.; Root, E.D.; Feaster, D.J.; Ward, P.J.; Selk, S.C.; Knott, C.; Villani, J.; Samet, J.H. Disparities in opioid overdose death trends by race/ethnicity, 2018–2019, from the HEALing communities study. Am. J. Public Health 2021, 111, 1851–1854. [Google Scholar] [CrossRef]
- Drake, J.; Charles, C.; Bourgeois, J.W.; Daniel, E.S.; Kwende, M. Exploring the impact of the opioid epidemic in Black and Hispanic communities in the United States. Drug Sci. Policy Law 2020, 6, 2050324520940428. [Google Scholar] [CrossRef]
- Altekruse, S.F.; Cosgrove, C.M.; Altekruse, W.C.; Jenkins, R.A.; Blanco, C. Socioeconomic risk factors for fatal opioid overdoses in the United States: Findings from the Mortality Disparities in American Communities Study (MDAC). PLoS ONE 2020, 15, e0227966. [Google Scholar] [CrossRef] [PubMed]
- Mitra, A.; Ahsan, H.; Li, W.; Liu, W.; Kerns, R.D.; Tsai, J.; Becker, W.; Smelson, D.A.; Yu, H. Risk factors associated with nonfatal opioid overdose leading to intensive care unit admission: A cross-sectional study. JMIR Med. Inform. 2021, 9, e32851. [Google Scholar] [CrossRef] [PubMed]
- Bohnert, A.S.B.; Ilgen, M.A.; Ignacio, R.V.; McCarthy, J.F.; Valenstein, M.; Blow, F.C. Risk of death from accidental overdose associated with psychiatric and substance use disorders. Am. J. Psychiatry 2012, 169, 64–70. [Google Scholar] [CrossRef]
- Yule, A.M.; Carrellas, N.W.; DiSalvo, M.; Lyons, R.M.; McKowen, J.W.; Nargiso, J.E.; Bergman, B.G.; Kelly, J.F.; Wilens, T.E. Risk factors for overdose in young people who received substance use disorder treatment. Am. J. Addict. 2019, 28, 382–389. [Google Scholar] [CrossRef]
- Karmali, R.N.; Ray, G.T.; Rubinstein, A.L.; Sterling, S.A.; Weisner, C.M.; Campbell, C.I. The role of substance use disorders in experiencing a repeat opioid overdose, and substance use treatment patterns among patients with a non-fatal opioid overdose. Drug Alcohol Depend. 2020, 209, 107923. [Google Scholar] [CrossRef]
- Van Draanen, J.; Tsang, C.; Mitra, S.; Phuong, V.; Murakami, A.; Karamouzian, M.; Richardson, L. Mental disorder and opioid overdose: A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 57, 647–671. [Google Scholar] [CrossRef]
- Yamamoto, A.; Needleman, J.; Gelberg, L.; Kominski, G.; Shoptaw, S.; Tsugawa, Y. Association between homelessness and opioid overdose and opioid-related hospital admissions/emergency department visits. Soc. Sci. Med. 2019, 242, 112585. [Google Scholar] [CrossRef] [PubMed]
- Gjersing, L.; Amundsen, E. Increasing trend in accidental pharmaceutical opioid overdose deaths and diverging overdose death correlates following the opioid prescription policy liberalization in Norway 2010–2018. Int. J. Drug Policy 2022, 108, 103785. [Google Scholar] [CrossRef]
- Mueller, S.R.; Glanz, J.M.; Nguyen, A.P.; Stowell, M.; Koester, S.; Rinehart, D.J.; Binswanger, I.A. Restrictive opioid prescribing policies and evolving risk environments: A qualitative study of the perspectives of patients who experienced an accidental opioid overdose. Int. J. Drug Policy 2021, 92, 103077. [Google Scholar] [CrossRef]
- Yarborough, B.J.H.; Stumbo, S.P.; Janoff, S.L.; Yarborough, M.T.; McCarty, D.; Chilcoat, H.D.; Coplan, P.M.; Green, C.A. Understanding opioid overdose characteristics involving prescription and illicit opioids: A mixed methods analysis. Drug Alcohol Depend. 2016, 167, 49–56. [Google Scholar] [CrossRef]
- Bahji, A.; Bajaj, N. Opioids on trial: A systematic review of interventions for the treatment and prevention of opioid overdose. Can. J. Addict. 2018, 9, 26–33. [Google Scholar] [CrossRef]
- Chu, K.; Carriere, G.; Garner, R.; Bosa, K.; Hennessy, D.; Sanmartin, C. Exploring the intersectionality of characteristics among those who experienced opioid overdoses: A cluster analysis. Health Rep. 2023, 34, 3–14. [Google Scholar] [PubMed]
- Bzdok, D.; Altman, N.; Krzywinski, M. Statistics versus machine learning. Nat. Methods 2018, 15, 233–234. [Google Scholar] [CrossRef]
- Clark, T.G.; Bradburn, M.J.; Love, S.B.; Altman, D.G. Survival Analysis Part I: Basic concepts and first analyses. Br. J. Cancer 2003, 89, 232–238. [Google Scholar] [CrossRef]
- Ohno-Machado, L. Modeling medical prognosis: Survival analysis techniques. J. Biomed. Inform. 2001, 34, 428–439. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, N.; Biswas, B.; Singh, C.; Nair, R.; Mounica, G.; Jha, A.R.; Das, K.M. Early Determinants of Length of Hospital Stay: A Case-Control Survival Analysis among COVID-19 Patients Admitted in a Tertiary Healthcare Facility of East India. J. Prim. Care Community Health 2021, 12, 21501327211054281. [Google Scholar] [CrossRef]
- Ho, S.-H. Survival analysis of living arrangements and health care utilization in terms of total mortality among the middle-aged and elderly in Taiwan. J. Nurs. Res. 2008, 16, 160–168. [Google Scholar] [CrossRef]
- Bambi, J.; Santoso, Y.; Sadri, H.; Moselle, K.; Rudnick, A.; Robertson, S.; Chang, E.; Kuo, A.; Howie, J.; Dong, G.Y.; et al. A Methodological Approach to Extracting Patterns of Service Utilization from a Cross-Continuum High Dimensional Healthcare Dataset to Support Care Delivery Optimization for Patients with Complex Problems. BioMedInformatics 2024, 4, 946–965. [Google Scholar] [CrossRef]
- Bambi, J.; Sadri, H.; Moselle, K.; Chang, E.; Santoso, Y.; Howie, J.; Rudnick, A.; Elliott, L.T.; Kuo, A. Approaches to Generating Patterns of Service Utilization for Patients with Complex Conditions: Graph Community Detection vs Natural Language Processing Clustering. BioMedInformatics 2024, 4, 1884–1900. [Google Scholar] [CrossRef]
- Bambi, J.; Santoso, Y.; Moselle, K.; Robertson, S.; Rudnick, A.; Chang, E.; Kuo, A. Analyzing Patterns of Service Utilization Using Graph Topology to Understand the Dynamic of the Engagement of Patients with Complex Problems with Health Services. BioMedInformatics 2024, 4, 1071–1084. [Google Scholar] [CrossRef]
- Bambi, J.; Dong, G.Y.; Santoso, Y.; Moselle, K.; Dugas, S.; Olobatuyi, K.; Rudnick, A.; Chang, E.; Kuo, A. Patterns of Service Utilization across the Full Continuum of Care: Using Patient Journeys to Assess Disparities in Access to Health Services. Knowledge 2024, 4, 252–264. [Google Scholar] [CrossRef]
- Park, T.W.; Lin, L.A.; Hosanagar, A.; Kogowski, A.; Paige, K.; Bohnert, A.S.B. Understanding risk factors for opioid overdose in clinical populations to inform treatment and policy. J. Addict. Med. 2016, 10, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Tseregounis, I.E.; Henry, S.G. Assessing opioid overdose risk: A review of clinical prediction models utilizing patient-level data. Transl. Res. 2012, 234, 74–87. [Google Scholar] [CrossRef] [PubMed]
- Suffoletto, B.; Zeigler, A. Risk and protective factors for repeated overdose after opioid overdose survival. Drug Alcohol Depend. 2020, 209, 107890. [Google Scholar] [CrossRef]
- Government of British Columbia. Health Authorities. Available online: https://www2.gov.bc.ca/gov/content/health/about-bc-s-health-care-system/partners/health-authorities (accessed on 20 June 2024).
- Koval, A.; Moselle, K. Clinical Context Coding Scheme—Describing Utilisation of Services of Island Health between 2007–2017. In Proceedings of the Conference of the International Population Data Linkage Association, Banf, AB, Canada, 12–14 September 2018. [Google Scholar]
- Blondel, V.D.; Guillaume, J.-L.; Lambiotte, R.; Lefebvre, E. Fast unfolding of communities in large networks. J. Stat. Mech. Theory Exp. 2008, 2008, P10008. [Google Scholar] [CrossRef]
- Klein, J.P.; Moeschberger, M.L. Survival Analysis: Techniques for Censored and Truncated Data; Springer: Berlin/Heidelberg, Germany, 2003. [Google Scholar]
- Li, Y.; Rakesh, V.; Reddy, C.K. Project success prediction in crowdfunding environments. In Proceedings of the Ninth ACM International Conference on Web Search and Data Mining, San Francisco, CA, USA, 22–25 February 2016; pp. 247–256. [Google Scholar]
- Dunn, O.J.; Clark, V.A. Basic Statistics: A Primer for the Biomedical Sciences; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Zupan, B.; Demšar, J.; Kattan, M.W.; Beck, J.R.; Bratko, I. Machine learning for survival analysis: A case study on recurrence of prostate cancer. Artif. Intell. Med. 2000, 20, 59–75. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, E.L.; Meier, P. Nonparametric estimation from incomplete observations. J. Am. Stat. Assoc. 1958, 53, 457–481. [Google Scholar] [CrossRef]
- Lee, E.T.; Wang, J. Statistical Methods for Survival Data Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2003. [Google Scholar]
- Allison, P.D. Survival Analysis Using SAS: A Practical Guide; SAS Institute: Cary, NC, USA, 2010. [Google Scholar]
- Bohnert, A.S.; Valenstein, M.; Bair, M.J.; Ganoczy, D.; McCarthy, J.F.; Ilgen, M.A.; Blow, F.C. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 2011, 305, 1315–1321. [Google Scholar] [CrossRef] [PubMed]
- Paulozzi, L.J.; Kilbourne, E.M.; Shah, N.G.; Nolte, K.B.; Desai, H.A.; Landen, M.G.; Harvey, W.; Loring, L.D. A history of being prescribed controlled substances and risk of drug overdose death. Pain Med. 2012, 13, 87–95. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical: Vienna, Austria, 2008. [Google Scholar]
- Horwitz, R.I.; Horwitz, S.M. Adherence to treatment and health outcomes. Arch. Intern. Med. 1993, 153, 1863–1868. [Google Scholar] [CrossRef]

| Groups | Total OD % | No Second OD | Second OD | Hazard Ratio |
|---|---|---|---|---|
| %(n) (N = 5380) | %(n) (N = 3798) | %(n) (N = 1582) | (95% CI) | |
| Age | ||||
| 0−20 | 05.84 (314) | 05.58 (212) | 06.45 (102) | 1.00 |
| 20–29 | 23.35 (1256) | 21.70 (823) | 27.37 (433) | 0.77 (0.61, 0.97) |
| 30–39 | 27.06 (1456) | 25.70 (977) | 30.28 (479) | 0.77 (0.61, 0.97) |
| 40–49 | 19.33 (1040) | 19.50 (742) | 18.84 (298) | 0.67 (0.52, 0.85) |
| 50–59 | 14.28 (768) | 14.90 (565) | 12.84 (203) | 0.64 (0.50, 0.83) |
| 60–100 | 08.75 (471) | 10.60 (404) | 04.24 (67) | 0.45 (0.32, 0.62) |
| Gender | ||||
| Male | 69.65 (3747) | 68.14 (2588) | 73.30 (1159) | 1.34 (1.18, 1.51) |
| Female | 30.29 (1630) | 31.78 (1207) | 26.70 (423) | 1.00 |
| Unknown | 00.06 (3) | 00.08 (3) | − | − |
| Community ID | ||||
| Community ID 1 | 20.00 (1076) | 15.70 (0595) | 30.40 (481) | 1.00 |
| Community ID 2 | 30.72 (1653) | 35.00 (1331) | 20.40 (322) | 0.49 (0.42, 0.58) |
| Community ID 3 | ||||
| Community ID 4 | ||||
| Ever Homeless | ||||
| No (0) | ||||
| Yes (1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bambi, J.; Olobatuyi, K.; Santoso, Y.; Sadri, H.; Moselle, K.; Rudnick, A.; Dong, G.Y.; Chang, E.; Kuo, A. Use of Patterns of Service Utilization and Hierarchical Survival Analysis in Planning and Providing Care for Overdose Patients and Predicting the Time-to-Second Overdose. Knowledge 2024, 4, 444-461. https://doi.org/10.3390/knowledge4030024
Bambi J, Olobatuyi K, Santoso Y, Sadri H, Moselle K, Rudnick A, Dong GY, Chang E, Kuo A. Use of Patterns of Service Utilization and Hierarchical Survival Analysis in Planning and Providing Care for Overdose Patients and Predicting the Time-to-Second Overdose. Knowledge. 2024; 4(3):444-461. https://doi.org/10.3390/knowledge4030024
Chicago/Turabian StyleBambi, Jonas, Kehinde Olobatuyi, Yudi Santoso, Hanieh Sadri, Ken Moselle, Abraham Rudnick, Gracia Yunruo Dong, Ernie Chang, and Alex Kuo. 2024. "Use of Patterns of Service Utilization and Hierarchical Survival Analysis in Planning and Providing Care for Overdose Patients and Predicting the Time-to-Second Overdose" Knowledge 4, no. 3: 444-461. https://doi.org/10.3390/knowledge4030024
APA StyleBambi, J., Olobatuyi, K., Santoso, Y., Sadri, H., Moselle, K., Rudnick, A., Dong, G. Y., Chang, E., & Kuo, A. (2024). Use of Patterns of Service Utilization and Hierarchical Survival Analysis in Planning and Providing Care for Overdose Patients and Predicting the Time-to-Second Overdose. Knowledge, 4(3), 444-461. https://doi.org/10.3390/knowledge4030024










