Abstract
Healthcare organizations have a contractual obligation to the public to address population-level inequities to health services access and shed light on them. Various studies have focused on achieving equitable access to healthcare services for vulnerable patients. However, these studies do not provide a nuanced perspective based on the local reality across the full continuum of care. In previous work, graph topology was used to provide visual depictions of the dynamics of patients’ movement across a complex healthcare system. Using patients’ encounters data represented as a graph, this study expands on previous work and proposes a methodology to identify and quantify cohort-specific disparities in accessing healthcare services across the continuum of care. The result has demonstrated that a more nuanced approach to assessing access-to-care disparity is doable using patients’ patterns of service utilization from a longitudinal cross-continuum healthcare dataset. The proposed method can be used as part of a toolkit to support healthcare organizations that wish to structure their services to provide better care to their vulnerable populations based on the local realities. This provides a first step in addressing inequities for vulnerable patients in accessing healthcare services. However, additional steps need to be considered to fully address these inequities.
1. Introduction
1.1. Disparities in Accessing Healthcare Services
According to Whitehead and Dahlgren, echoing the World Health Organization constitution [1], “equity in health implies that everyone could ideally attain their full health potential, and that no one should be disadvantaged from achieving this potential because of their social position or other socially determined circumstance”. Healthcare organizations operate on the assumption that they have a contractual obligation to the public, requiring them to address population-level inequities and shed light on them. Furthermore, these organizations are committed to addressing the methodological challenges associated with establishing the causal mechanisms, determinants, or correlations of these inequities. The aim is to identify factors within the control of the healthcare system that can be influenced. Should there be disparities in accessing healthcare services, the hosting organization bears the responsibility to rectify them. If healthcare service organizations wish to become effective for health interventions, organizations need to prioritize locally relevant strategies that are oriented to working with vulnerable groups [2]. Consequently, the challenge lies in tracing these inequities back to their root causes or determinants and relating them to factors that fall within the organization’s purview.
Certain groups of patients considered vulnerable have been extensively examined, with considerable research focusing on achieving equitable access to healthcare services. Health inequality affects all Canadians, but for vulnerable populations, it has a much stronger impact on their health [3]. Several studies, including [4,5], have demonstrated that vulnerable patients tend to have an overall lower quality of life and health. Additionally, access to care is one of the most significant challenges affecting the quality of life of vulnerable populations [6]. The lack of proper access to healthcare can potentially lead to a reduced life span compared to the general population. Such population groups include individuals affected by, e.g., psychiatric issues such as schizophrenia [7,8]. Research has shown that individuals with schizophrenia have an exceptionally short life expectancy, averaging approximately 20 years below that of the general population [8]. Moreover, high mortality is found in all age groups, with two-thirds of this excess mortality caused by natural deaths [7,8]. One of the factors that influence this reduction in life expectancy include the fact that common physical illness are diagnosed late and do not receive sufficient treatment, in spite of the fact that people with schizophrenia tend to live an unhealthy lifestyle with regards to diet, smoking, alcohol consumption, and lack of physical exercises [8].
People with mental health and substance use (MHSU) [9] and those suffering from homelessness [9,10] as well as physical mobility [11] and neurocognitive disorders [12] tend to have less access to healthcare services. Lack of access to proper services for serious/chronic mental health issues has also been shown to be one of the major challenges in treating those mental health and addictions issues that lead to homelessness and an excessive use of some services such as emergency departments [10,13]. Moreover, mobility limitations is especially true for older adults [14,15] and may be due to chronic conditions, including arthritis and chronic lung problems [16,17]. Access to physicians and sub-specialty care has also been shown to be more difficult for patients with mobility impairment [18], hence compromising their quality of care delivery. Furthermore, despite the fact that neurocognitive disorders represent a growing major concern in the world, with a growing aging population, treatment and management of neurocognitively impaired patients remains suboptimal due to inadequate treatment and poor quality of care, increasing the risks of adverse outcome [12].
Various stigmatization are also known to negatively impact access to healthcare services [16,19,20]. There are various types of stigmas, including health condition-related stigma and non-health-related stigma. Health condition-related stigma affects people living with a specific disease or health condition, including leprosy, epilepsy, mental health disorders, cancer, HIV, and obesity/overweight [21]. Non-health-related stigma include socio-economic status, age, gender, race, and sexual orientation [22]. A stigma can be a barrier to care for patients seeking support to maintain a healthy quality of life, seeking disease prevention service, or treatment for acute or chronic healthcare conditions [23]. In health facilities, the manifestation of stigma may result in subtle forms of deprivation such as longer waits for services or being referred to junior providers [23,24]. It may also manifest in an outright denial of services, physical or verbal abuse, or provision of sub-standard care [23]. As a result, stigma within healthcare may undermine access to diagnosis and treatment and result in poor or unsuccessful health outcomes [23,25,26,27].
The above-cited studies capture the typical reality of cohorts of patients accessing specific services. The challenge is the fact that these studies do not provide a nuanced perspective based on the local reality across the full care continuum. It is common to look at differences in access to certain services, such as how often a cohort of patients accesses the emergency department. It is also common to look at differential access to a specific service within a medical specialty such as cardiovascular. However, a view of patient access from a cross-continuum, including secondary and tertiary services, is what is lacking from these studies. If the goal is to address disparities in access to services for vulnerable patients that may be affected by a diverse array of needs, there is no need to restrict one’s view to a limited number of services, but one should rather provide visibility to all services across the continuum of care. Using local data to capture the local reality, the advocated approach provides the opportunity to (1) determine whether the disparity shows up consistently across areas or is specific to some services and not others and (2) facilitate the determination of whether the disparity in access lies with the patients’ capacity to advocate for services and/or initiate/maintain access to services or with the service system structure or a combination of the two factors. This provides a potential for a tangible solution to address the disparity.
Moreover, if we are concerned with disparities in access, there is an immediate problem that need to be addressed. Addressing disproportionately high rates of access to a given service, e.g., large numbers of emergency department visits for persons in a specific demographic or contending with a specific underlying condition, is methodologically straightforward. However, when addressing disparities in access, our efforts frequently involve compiling aggregate counts for events that have yet to occur. To do this, we need some sort of reference standard or expected value, enabling us to interpret measured rates effectively and transform disparities into inequities. The problem is that for many cohorts and for many services, such standards may not exist, or they may be imprecise and therefore poorly positioned as a basis for determining when rates of service access fall “out of range”. For example, how many cardiovascular-related investigative procedures should be performed for persons with schizophrenia who are not yet displaying obvious signs/symptoms of cardiovascular illness? Such information may or may not be found in the literature. If we further partition that group into persons with schizophrenia and a comorbid substance use disorder vs. persons with schizophrenia without a comorbid substance use disorder, will the reference standard be readily available in the literature as well? Operating on the assumption that externally supplied reference standards are generally not going to be available for a method that must be general in scope, we may resort to cohort comparison design—using rates for other groups as a proxy for external reference standards.
Prior works [28,29,30] have developed methodologies to extract patterns of service utilization (PSUs) from longitudinal electronic healthcare records to optimize healthcare services. Expanding on this by (1) using source data consisting of longitudinal transactional service encounter data provided by one of the health authorities in Canada and (2) relying on a cohort comparison design, this paper proposes a methodology that uses patients’ encounter data represented as a graph to analyze access to healthcare services for a set of patient cohorts with varied levels of vulnerabilities, as chosen by clinical subject-matter experts (SMEs). The goal is to corroborate previous findings and offer a more nuanced perspective on access inequities. Providing this type of analysis will help facilitate the identification of the factors that are within the control of the host organization to address the inequities. Moreover, the focus of the paper is methodological, and a host organization can apply the proposed methodology to any cohort of interest.
1.2. Objectives
This paper illustrates a method for locating cohort-specific disparities in health service access within large and sparse high-dimensional, full cross-continuum health service datasets that span hospital and community sectors for medical/surgical as well as mental health and/or substance use/addictions services. These disparities are important when they are not commensurate with need or risk, as they then become markers for inequities in health service access. Ethically, healthcare organizations are obligated to acknowledge and address these inequities by shedding light on them and identifying factors within their control. This study illustrates a specific instance of a broader methodology that utilizes a set of longitudinal health service encounter data to identify and quantify cohort-specific disparities in access to healthcare services.
Using a cross-continuum healthcare dataset from a regional health authority, the goal is to provide a more nuanced understanding of healthcare access disparity, focusing on a chosen set of patient cohorts with distinguishing levels of vulnerabilities. Also, the work does not assume that the identified disparities arise solely from clinical cohort-defining characteristics of persons, in which case disparities would be expected to show up consistently across the service area. In keeping with the working hypothesis that disparities are a joint function of features of persons and features of service system structures and functions, the study looks for disparities in both medical/surgical and MHSU service areas.
To summarize, the work presented in the paper is organized around three overarching substantive questions:
- Are there disparities in service access or patterns of service utilization (PSUs) that are associated with cohort membership? For the work in this paper, cohorts are distinguishable on the basis of expected differential capacity to initiate access to anything other than low-barrier access services, e.g., emergency departments, and remain connected to services over time. The term “vulnerable” is used in this paper to refer to that capacity.
- Do identified disparities in access show up consistently across service areas?
- To what extent can we use PSUs to identify healthcare access inequities and provide a more refined approach in assessing the cause of the inequity?
To address the above questions, from a methodological perspective, the following approaches are used:
- Cohort comparison: Patients in the chosen cohorts of interest are users of medical/surgical and/or MHSU services. However, one of the cohorts is made of patients that are considered more vulnerable than the other. Using PSUs, the cohort of more vulnerable patients will be compared to a cohort of patients with less severe vulnerability in terms of access to various healthcare services. When measuring access disparities for the above cohorts, both empirical and statistical approaches will be used, and the results will be compared;
- Consultation with SMEs will be conducted to review the results and to answer the questions that were raised earlier regarding determinants of access.
2. Methodology
2.1. Source Data
The source data used in this paper consist of retrospective longitudinal transactional service encounter data contents extracted from a single instance of a Clinical Information System (CIS) deployed across the continuum of services provided by one of the health authorities within Canada (hereinafter referred to as “host organization”). It provides a comprehensive array of secondary and tertiary health services for all ages, for persons contending with medical/surgical issues and/or mental health/substance use issues. This includes acute care/intensive care services, hospital and community-based emergency response, ambulatory services, residential care services for older adults or persons contending with mental health issues, case management services, and a range of addiction harm reduction or rehab and recovery-oriented services. The encounter data accessed by this study consist of approximately 10 million encounters over 7 years for approximately 1 million patients. Except for a few restricted services where the data are strictly embargoed (e.g., services for persons who are victims of sexual assault), this represents data for all service recipients. To access the source data, a certificate of approval was provided by the University of Victoria Research Ethics Board (REB), following the British Columbia, Canada, ethics harmonization guideline.
2.2. Data Pre-Processing: Addressing Data Granularity and Nomenclature Issues
The services provided by the host organization are encapsulated into an array of roughly 2000 service units within a location built of the host organization CIS. The service units may vary widely with regard to granularity; for example, multiple beds will appear as a single unit within an acute care facility, but multiple beds in a large array of family care homes for frail elderly will show up as multiple service units. Additionally, service unit names within the local clinical information system are often opaque. For example, an addiction post-withdrawal stabilization unit appears in this location as “Holly”, or there is a service unit named “Clinics” that provides ambulatory services for children and youths with physical disabilities. There are large numbers of service units where the unit names are uninterpretable, or interpretation is a matter of guessing. This renders them unsuitable for any analysis that requires meaningfully labelled data. In modeling the structure and dynamics of patient interaction with services, meaningful distinctions between functions performed by services must be preserved.
The clinical context coding scheme (CCCS) [31] is a semantic layer that was developed as a flexible solution to address issues of data granularity and nomenclature. This scheme is organized around six sets of codes, constituting a semantic layer applied to all 2000+ service units. The roughly 200 service classes employed for the modeling in this paper consist of equivalence classes formed by the application of these code sets to those service units. Also, each service class has a name that bears some discernible relationship to the functions performed by the component service units. The modeling activities reported in this paper are performed on patient–service encounters with service classes.
2.3. Cohort Selection
Cohort selection is based on access to services that target specific classes of diagnoses as well as the capacity to seek out and access services. The classes of diagnoses can be distinguished on the basis of broad-based impact on psychosocial functioning and on chronicity. In this paper, the term “vulnerable” relates to the impact of a condition on the person’s functioning. The term “more vulnerable” is used to refer to the cohort of persons contending with the more severe MSHU chronic and pervasively impactful class of conditions. These impacts include limited capacity to seek out and maintain access to services. The term “less vulnerable” is used to refer to the cohort of persons contending with a class of MHSU problems that are episodic and less inherently pervasive in their impact on the person and the ability to seek out and maintain access to services. Members of the “less vulnerable” cohort are expected to be more capable of seeking out and maintaining accessing to services.
These cohorts are not mutually exclusive. There are some patients with membership in both cohorts, reflecting the co-occurrence of qualifying diagnoses for the two different cohorts. For these patients, if they met the criteria for inclusion in the more vulnerable cohort, they were treated as members of that cohort only.
Two cohorts were considered: One consists of patients with a chronic MHSU disorder. The second consists of patients with a less serious episodic MHSU disorder. Cohort 1 was defined as the group of more vulnerable patients and cohort 2 as the group of less vulnerable patients. The less vulnerable cohort comprises 21,180 patients, and the more vulnerable cohort comprises 1829 patients. Of these, 182 patients belong to both cohorts and were thus assigned to the more vulnerable cohort.
2.4. Representing Patient access to Healthcare Services System as a Graph and Estimating Transition Probabilities between Services
In this paper, patients’ encounter data are modeled using a directed graph, and logistic regression is used to estimate transition probabilities in state space models. In the encounter dataset, there are patients and records of their interactions with service classes. One patient typically uses several service classes throughout his/her journey. A given patient may also access a given service class on more than one occasion, e.g., repeat admissions to an emergency department or routine repeated blood work. If the records of a patient are arranged sequentially in chronological order, one service can be connected to another by a “next service” relationship. Suppose patient A used service class 1, then 2, then 2 again, then 3, and then 2. This sequence can be depicted as a directed graph with the service classes as nodes and directed edges that reflect the transitions. This is illustrated in Figure 1, where the edge labels are for the sequence order. Patient A’s journey can then be coded as 12232.
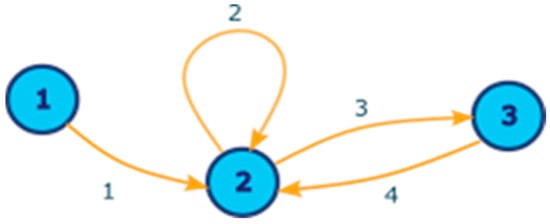
Figure 1.
A directed graph of three nodes (representing service class 1, 2, and 3) and four edges, depicting a patient journey from service class 1 to 2, to 2 again, to 3, and back to 2. Here, the edge labels are for the sequence order.
Now, among the service classes, we may be interested in only some of them. Thus, we can label them as 1 if it is a service class of interest or 0 otherwise. Suppose that in the example shown in Figure 1, we are interested in service class 2 only; then, we relabel service class 1 as 0, service class 2 as 1, and service class 3 as 0. This is shown in Figure 2. The patient’s journey can now be read as 01101.
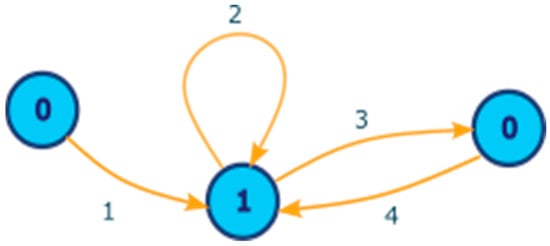
Figure 2.
The directed graph from Figure 1 with the nodes relabeled as either 1 (if it is a service class of interest–service class 1) or 0 (if it is not a service class of interest–service class 0).
Graphs can be thought of as state space models, where each node is a state. This has been carried out in several fields, including rainfall data [32], transportation systems [33], and in forestry [34], and, more recently, patterns of service utilization [28,30]. Logistic regression is used to model binary outcomes encoded as 0 or 1 by assuming a linear relationship between the dependent variables and the log-odds of the outcome. That is, if Y is the outcome variable, we use the following model:
Here, it is used to model transition probabilities between services.
Using the direct graph where service classes are arranged by the date and time of the interaction so that each patient’s journey through the healthcare system is encoded as a sequence of service classes, we pick service classes of interest and then model the probability of transition to these services. Given this set of service classes, we can encode each patient’s journey as a sequence of 0 s (if not in the group of interest) or 1 s (if inside the group of interest). Logistic regression is used to model the transition probabilities. Fitting of the logistic regression is performed via the glm() function, which fits generalized linear models, including logistic regression (see [35] for details) in R v4.1.3 [36]. The demographic information we use includes the gender and age of the patients. In this analysis, age is treated as a categorical variable with three categories: 18–40, 41–64, and 65+. In some of the analyses that follow, values of NA are reported when there were no observations within that age group for the specific service class. However, for consistency between analyses, age groupings are kept the same for all service classes. Specifically, the data pre-processing is carried out following the steps below:
- Obtain the list of patient transitions from the patient analysis tool from each of the cohorts that need to be compared;
- Encode all the services in the class of interest with a 1 and all other services with a 0. For example, if a patient has a service history of “0 0 0 1 1 0 0”, the patient accessed the service of interest at their fourth and fifth encounters only;
- To account for differing underlying morbidity rates between the two cohorts, we consider transitions after and including the first transition to a service of interest. These biases have the potential to affect the trajectory that patients follow when engaging with the health services. The above would then become “0 1 1 0 0”. That is, we remove all except one leading 0;
- We count the number of 2-g. The above string would yield 01, 11, 10, 00;
- The number of 2-g from all individuals in each cohort is summed; grouping by demographic information such as age and gender is possible if the effect of these factors is of interest.
We then fit a logistic regression model for transition probabilities. That is, we aim to predict the probability of transition from each state Y from the previous state . The covariates for prediction are the previous state , cohort membership, and optional demographic information.
Without demographic information, the transition probabilities can be modeled as the probability of a 0-to-1 transition, denoted as the following:
and the probability of a 1-to-1 transition, denoted as the following:
where is 1 if the patient is in the cohort of interest and 0 otherwise; the expit function is as follows:
An alternative formulation requiring only one equation is as follows:
To show that the above formulations are equivalent, we can use the following definitions to go between the two formulations. We set the following:
With demographic information, we simply write the following:
Additional demographic information can be added similarly. Model selection for choosing which demographic information to include is performed with backwards stepwise selection using AIC, using the step() function in R. For the purposes of this paper, since multiple comparisons are made for a variety of service classes, two models are used for the sake of consistency: (1) the model where predictors are , cohort membership, gender, and age and (2) the model with neither gender or age, using only and cohort membership as predictors. In practice, model selection should be done and additional demographic information included, if relevant, to ensure the best model fit.
In the case where we only consider the transitions and the cohort membership (and not any demographic information), if we assume an interaction term between cohort and transition, then the probability will be equal to the empirical probability, which is just the ratio of the transition event counts, as there are four transition probabilities ( and for the two cohorts) to estimate and four parameters for estimation (). In this case, if the estimated probabilities are the only values of interest (rather than, say, the coefficients themselves), it can be simpler to calculate the empirical probabilities rather than fitting the model. So, for example, the probability of a 01 transition would be as given:
where is the number of transitions from state a to state b. This is the empirical probability of a transition if currently we are in state 0 to be in state 1 after the transition.
3. Analysis and Results
As previously stated, two cohorts were considered, comprising 21,180 patients from the less vulnerable cohort and 1829 patients from the more vulnerable cohort. Additionally, the 182 patients belonging to both cohorts were assigned to the more vulnerable cohort. It should be noted that not all patients accessed every service, and as such, not all patients are included in the analyses below.
First, a collection of cardiovascular services was taken as the focus and includes age and gender as features in addition to cohort and previous state. It was found that age and gender are not significant, as shown by the result below in Table 1:

Table 1.
Cardiovascular.
For this reason, age and gender were excluded in the analysis of the result shown in Table 2. Taking only previous state and cohort membership, we obtain the following:

Table 2.
Cardiovascular transition probabilities, including previous state and cohort only.
From Table 2, the probabilities of both 0-to-1 and 1-to-1 transitions are higher in cohort 2 compared to cohort 1, which corresponds with a positive fitted effect for cohort 2 membership. Next, the focus of service classes was shifted onto residential care (Table 3), assertive community treatment -ACT (Table 4), psychiatric emergency services -PES (Table 5), and MHSU acute care (Table 6). For these service classes, there is a negative fitted effect corresponding with cohort 2 membership, implying that transitions to the service class of interest are more likely to occur for patients in cohort 1.

Table 3.
Residential Care.

Table 4.
ACT.

Table 5.
PES.

Table 6.
MHSU Acute Care.
In our next analyses, we compare the transition probabilities for each cohort considered in our study. To have a fair comparison among the focus sets, we removed age and gender to be able to list the transition probabilities for each cohort. Table 7 shows that for residential care, ACT, PES, and MHSU acute care, the probabilities of both 0-to-1 and 1-to-1 transitions are lower in cohort 2 compared to cohort 1.

Table 7.
Transition probabilities.
The results demonstrate that there is a disparity in access to cardiovascular service between cohort 1 and cohort 2. The probability for a patient in cohort 2 of having a follow-up cardiovascular service is thrice as much as for a patient in cohort 1.
Moreover, as previously mentioned, the goal is to provide a more nuanced understanding of healthcare access disparities affecting vulnerable patients. Using a cross-continuum dataset and expanding the analysis to other services, including residential services, ACT, PES, and MHSU acute care, the following was noted:
- 1.
- For residential service, the probability of a patient in cohort 1 to access this service is more than double the probability for patients in cohort 2;
- 2.
- For ACT, we notice the same trend: a patient in cohort 1 is more likely to access ACT than a patient in cohort 2;
- 3.
- Access to PES is also higher for patients in cohort 1 than patients in cohort 2;
- 4.
- For MHSU acute care, once again, patients in cohort 1 have a higher probability of accessing this service than patients in cohort 2.
Based on the above, patients in cohort 1 tend to benefit from MSHU wrap-around services more than patients in cohort 2. It should also be noted that within MHSU, there are services where there is virtually no disparity in access between the two cohorts. An example of such a service is case management.
4. Discussion
The purpose of this paper is to supply a demonstration of a more general method to identify and measure cohort-specific disparities in service access. Focusing on disparities in access to one set of services may produce a compelling set of results, but they may not reproduce across service sectors. We cannot necessarily assume that access within one sector can be treated as a proxy for full-service system utilization. In other words, looking for disparities in one service sector is only half the method. The full method entails an examination of service utilization across the continuum of care.
Analysis of PSUs within and across cohorts paints a clear picture of a health service system composed of functionally distinguishable clusters of services and service pathways that connect them. The channels that are etched, sometimes quite deeply, across the service system landscape will have an impact on who accesses what services within a given timeframe. Patient factors have some say as to where those pathways are located. Also, service system factors, e.g., span of influence, clinical practice guidelines, and administrative leaders, within program areas will partially determine where those channels are located and how deeply they are etched.
Graph transition probabilities were modelled with logistic regression, where covariates explain variation in transition probabilities of individuals within different classes over time. These covariates often account for differences in the prevalence of transition probabilities over time. This approach is often employed when assessing possible influences on the transition probabilities and is of great importance. Previously, ref. [37] incorporated categorical covariates to model transition probabilities. Also, transition probabilities LR formulated by [37] took into account continuous or time-varying covariates in the analysis of their transitions. They further outlined regression models in which covariates are used to predict individuals’ class membership and their next transitions.
This paper proposes a flexible methodology using longitudinal cross-continuum healthcare data where data are treated as a graph, and then, transition probabilities are modeled using logistic regression. The proposed method allows for patients’ encounter date to be used and provides a simple method that is easily adaptable to use with other data sources or other cohorts or to find different disparities of interest.
Based on the results of the analysis, we can see that there are differences in access between the group of vulnerable patients and the group of less vulnerable patients. However, these disparities in access do not show up consistently across service areas. For those services where vulnerable patients have less access, it is not clear whether this reflects limited capacity for this group to navigate access the services, is due to processes within the health services system, or is a combination of the two. On one hand, there is a vast amount of literature concerned with one of the categories of vulnerable patients that is consistent with the factor of limited capacity to navigate access to services or sustaining relationships with the service system. On the other hand, the MSHU wrap-around service that this category of vulnerable patients benefits from is a clear demonstration that it is possible for a service system to be structured in a way that addresses the limitations of a vulnerable population. This could be a model that could be replicated outside MHSU as well.
The results have demonstrated that there are group differences regarding access to some of the services. However, the results do not explain why these differences are occurring in the first place. Is this a reflection of limited capacity to navigate access to services on the part of persons within the vulnerable cohort? Alternatively, does the difference emanate in some fashion from persons or processes within the health service system? Or is the difference a reflection of both factors? Moreover, one must consider the possibility that the cohorts may differ regarding factors other than those that one thinks may be “causing” the inequity. These could be distal factors not captured in the dataset. This is a limitation of this study. To address this, further analyses need to be conducted taking into consideration other potentially contributing factors and involving various clinical and social SMEs and additional datasets beyond patients encounter data, which may not be readily available within a health service clinical information system.
The work laid out in this paper is methodological, demonstrating a method to detect potential inequities in access to services. For privacy issues, the exact diagnosis or the nature of the vulnerability was not disclosed. However, the paper demonstrates that a more nuanced approach to assessing disparity in access to care is doable using PSUs from a longitudinal cross-continuum healthcare dataset. Any organization that wishes to structure their services to provide better care to its vulnerable population can use the proposed approach as part of their toolkit in assessing the services that need to be restructured or integrated. The information generated from the proposed methodology can be valuable knowledge in the hands of quality assurance/quality improvement in guiding organizations to implement a more equitable healthcare system.
5. Conclusions
When patient factors and service system factors come together, inequities may arise, even when both patients and the service system are doing their best. That is, these are emergent characteristics that may run counter to the intent of all parties involved. Our paper outlines a general methodology that provides a nuanced approach to assess and measure access disparity using PSUs based on the local reality across the full care continuum. This provides a first step in addressing inequities for a healthcare organization. The methodology introduced in this paper is also easily extensible to other cohorts or services of interest and with data from a variety of data sources.
Additional steps need to be considered to fully address these inequities. These include (1) the understanding of additional factors, including patients’ distal determinants of health and social determinants of health that may affect timely access to appropriate healthcare services and (2) the undertaking of specific, localized, and measurable actions developed and sustained through ongoing engagement with the communities, supportive leadership, dedicated resources, accountability, and transparency.
Author Contributions
Conceptualization, J.B., Y.S., G.Y.D., A.R. and A.K.; methodology, J.B., Y.S., and G.Y.D.; software, Y.S. and G.Y.D.; validation, J.B., K.M. and E.C.; formal analysis, J.B., Y.S., G.Y.D. and K.M.; investigation, J.B., Y.S. and G.Y.D.; resources, J.B. and K.M.; data curation, Y.S. and G.Y.D.; writing—original draft preparation, J.B., Y.S. and G.Y.D.; writing—review and editing, J.B., Y.S., G.Y.D., S.D., K.O., K.M., A.R., E.C. and A.K.; visualization, J.B., Y.S., G.Y.D. and K.M.; supervision, J.B., K.M., A.R. and A.K.; project administration, J.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
A certificate of approval was provided by the University of Victoria Research Ethics Board (REB), following the British Columbia, Canada, ethics harmonization guideline. The REB number is H21-02817.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets presented in this article are unavailable because of privacy or ethical restrictions. Requests to access the datasets require a certificate of approval by the University of Victoria Research Ethics Board, following the British Columbia, Canada, ethics harmonization guideline.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Whitehead, M.; Dahlgren, G.R.; World Health Organization. Levelling Up (Part 1): A Discussion Paper on Concepts and Principles for Tackling Social Inequities in Health; WHO Regional Office for Europe: Copenhagen, Denmark, 2006. [Google Scholar]
- Browne, A.J.; Varcoe, C.M.; Wong, S.T.; Smye, V.L.; Lavoie, J.; Littlejohn, D.; Tu, D.; Godwin, O.; Krause, M.; Khan, K.B.; et al. Closing the health equity gap: Evidence-based strategies for primary health care organizations. Int. J. Equity Health 2012, 11, 59. [Google Scholar] [CrossRef] [PubMed]
- Gilliland, J.A.; Shah, T.I.; Clark, A.; Sibbald, S.; Seabrook, J.A. A geospatial approach to understanding inequalities in accessibility to primary care among vulnerable populations. PLoS ONE 2019, 14, e0210113. [Google Scholar] [CrossRef] [PubMed]
- Laursen, T.M.; Munk-Olsen, T.; Vestergaard, M. Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr. Opin. Psychiatry 2012, 25, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Waisel, D.B. Vulnerable populations in healthcare. Curr. Opin. Anaesthesiol. 2013, 26, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Riley, W.J. Health disparities: Gaps in access, quality and affordability of medical care. Trans. Am. Clin. Climatol. Assoc. 2012, 123, 167. [Google Scholar] [PubMed]
- Auquier, P.; Lançon, C.; Rouillon, F.; Lader, M. Mortality in schizophrenia. Pharmacoepidemiol. Drug Saf. 2007, 16, 1308–1312. [Google Scholar] [CrossRef] [PubMed]
- Laursen, T.M.; Nordentoft, M.; Mortensen, P.B. Excess Early Mortality in Schizophrenia. Annu. Rev. Clin. Psychol. 2014, 10, 425–448. [Google Scholar] [CrossRef] [PubMed]
- Narendorf, S.C. Intersection of homelessness and mental health: A mixed methods study of young adults who accessed psychiatric emergency services. Child. Youth Serv. Rev. 2017, 81, 54–62. [Google Scholar] [CrossRef]
- Baker, J.; Travers, J.L.; Buschman, P.; Merrill, J.A. An Efficient Nurse Practitioner-Led Community-Based Service Model for Delivering Coordinated Care to Persons With Serious Mental Illness at Risk for Homelessness. J. Am. Psychiatr. Nurses Assoc. 2018, 24, 101. [Google Scholar] [CrossRef] [PubMed]
- Robine, J.M.; Ritchie, K. Healthy life expectancy: Evaluation of global indicator of change in population health. BMJ 1991, 302, 457–460. [Google Scholar] [CrossRef] [PubMed]
- Amjad, H.; Carmichael, D.; Austin, A.M.; Chang, C.-H.; Bynum, J.P.W. Continuity of Care and Health Care Utilization in Older Adults With Dementia in Fee-for-Service Medicare. JAMA Intern. Med. 2016, 176, 1371–1378. [Google Scholar] [CrossRef] [PubMed]
- Narendorf, S.C.; Cross, M.B.; Santa Maria, D.; Swank, P.R.; Bordnick, P.S. Relations between mental health diagnoses, mental health treatment, and substance use in homeless youth. Drug Alcohol Depend. 2017, 175, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Courtney-Long, E.A.; Carroll, D.D.; Zhang, Q.C.; Stevens, A.C.; Griffin-Blake, S.; Armour, B.S.; Campbell, V.A. Prevalence of Disability and Disability Type Among Adults—United States, 2013. MMWR. Morb. Mortal. Wkly. Rep. 2015, 64, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Jefferis, B.J.; Merom, D.; Sartini, C.; Wannamethee, S.G.; Ash, S.; Lennon, L.T.; Iliffe, S.; Kendrick, D.; Whincup, P.H. Physical Activity and Falls in Older Men. Med. Sci. Sports Exerc. 2015, 47, 2119–2128. [Google Scholar] [CrossRef] [PubMed]
- Iezzoni, L.I.; McCarthy, E.P.; Davis, R.B.; Siebens, H. Mobility impairments and use of screening and preventive services. Am. J. Public Health 2000, 90, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Zhao, G.; Ford, E.S.; Li, C.; Crews, J.E.; Mokdad, A.H. Disability and its correlates with chronic morbidities among U.S. adults aged 50−<65 years. Prev. Med. 2008, 48, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Lagu, T.; Hannon, N.S.; Rothberg, M.B.; Wells, A.S.; Green, K.L.; Windom, M.O.; Dempsey, K.R.; Pekow, P.S.; Avrunin, J.S.; Chen, A.; et al. Access to subspecialty care for patients with mobility impairment. Ann. Intern. Med. 2013, 158, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Christiani, A.; Hudson, A.L.; Nyamathi, A.; Mutere, M.; Sweat, J. Attitudes of Homeless and Drug-Using Youth Regarding Barriers and Facilitators in Delivery of Quality and Culturally Sensitive Health Care. J. Child Adolesc. Psychiatr. Nurs. 2008, 21, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Cradock-O’Leary, J.; Young, A.S.; Yano, E.M.; Wang, M.; Lee, M.L. Use of General Medical Services by VA Patients With Psychiatric Disorders. Psychiatr. Serv. 2002, 53, 874–878. [Google Scholar] [CrossRef] [PubMed]
- Stangl, A.L.; Earnshaw, V.A.; Logie, C.H.; Van Brakel, W.; Simbayi, L.C.; Barré, I.; Dovidio, J.F. The Health Stigma and Discrimination Framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019, 17, 31. [Google Scholar] [CrossRef] [PubMed]
- Joint United Nations Programme on HIV/Aids. Protocol for the identification of discrimination against people living with HIV. In Protocol for the Identification of Discrimination against People Living with HIV; Joint United Nations Programme on HIV/Aids: Geneva, Switzerland, 2000; p. 40. [Google Scholar]
- Nyblade, L.; Stockton, M.A.; Giger, K.; Bond, V.; Ekstrand, M.L.; Mc Lean, R.; Mitchell, E.M.H.; Nelson, L.R.E.; Sapag, J.C.; Siraprapasiri, T.; et al. Stigma in health facilities: Why it matters and how we can change it. BMC Med. 2019, 17, 25. [Google Scholar] [CrossRef]
- Ross, C.A.; Goldner, E.M. Stigma, negative attitudes and discrimination towards mental illness within the nursing profession: A review of the literature. J. Psychiatr. Ment. Health Nurs. 2009, 16, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Katz, I.T.; Ryu, A.E.; Onuegbu, A.G.; Psaros, C.; Weiser, S.D.; Bangsberg, D.R.; Tsai, A.C. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. J. Int. AIDS Soc. 2013, 16, 18640. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, E.M.; Budd, G.M. Obesity stigma: A newly recognized barrier to comprehensive and effective type 2 diabetes management. J. Am. Assoc. Nurse Pract. 2010, 22, 527–533. [Google Scholar] [CrossRef]
- Rueda, S.; Mitra, S.; Chen, S.; Gogolishvili, D.; Globerman, J.; Chambers, L.; Wilson, M.; Logie, C.H.; Shi, Q.; Morassaei, S.; et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: A series of meta-analyses. BMJ Open 2016, 6, e011453. [Google Scholar] [CrossRef] [PubMed]
- Bambi, J.; Santoso, Y.; Sadri, H.; Moselle, K.; Rudnick, A.; Robertson, S.; Chang, E.; Kuo, A.; Howie, J.; Dong, G.Y.; et al. A Methodological Approach to Extracting Patterns of Service Utilization from a Cross-Continuum High Dimensional Healthcare Dataset to Support Care Delivery Optimization for Patients with Complex Problems. BioMedInformatics 2024, 4, 53. [Google Scholar] [CrossRef]
- Bambi, J.; Santoso, Y.; Moselle, K.; Robertson, S.; Rudnick, A.; Chang, E.; Kuo, A. Analyzing Patterns of Service Utilization Using Graph Topology to Understand the Dynamic of the Engagement of Patients with Complex Problems with Health Services. BioMedInformatics 2024, 4, 60. [Google Scholar] [CrossRef]
- Bambi, J.; Sadri, H.; Moselle, K.; Chang, E.; Santoso, Y.; Howie, J.; Rudnick, A.; Elliott, L.; Kuo, A. Approaches to Generating Patterns of Service Utilization for Patients with Complex Conditions: Graph Community Detection vs Natural Language Processing Clustering. 2024. [Google Scholar]
- Moselle, K.; Koval, A. Mapping Clinical Contents onto Longitudinal Depictions of Cross-Continuum Service Events in Island Health. Int. J. Popul. Data Sci. 2018, 3. [Google Scholar] [CrossRef]
- Sinha, N.C.; Islam, M.A.; Ahamed, K.S. Logistic regression models for higher order transition probabilities of Markov chain for analyzing the occurrences of daily rainfall data. J. Mod. Appl. Stat. Methods 2011, 10, 337–348. [Google Scholar] [CrossRef]
- Kozłowski, E.; Borucka, A.; Świderski, A. Application of the logistic regression for determining transition probability matrix of operating states in the transport systems. Eksploat. Niezawodn.-Maint. Reliab. 2020, 22, 192–200. [Google Scholar] [CrossRef]
- Rößiger, G.; Kulla, L.; Bošeľa, M. Changes in growth caused by climate change and other limiting factors in time affect the optimal equilibrium of close-to-nature forest management. For. J. 2019, 65, 180–190. [Google Scholar] [CrossRef]
- Glm: Fitting Generalized Linear Models. Available online: https://www.rdocumentation.org/packages/stats/versions/3.6.2/topics/glm (accessed on 17 February 2024).
- R. C. Team. R: A language and environment for statistical computin. In R Foundation for Statistical Computing; R. C. Team: Vienna, Austria, 2013. [Google Scholar]
- Pfeffermann, D.; Skinner, C.; Humphreys, K. The estimation of gross flows in the presence of measurement error using auxiliary variables. J. R. Stat. Soc. Ser. A (Stat. Soc.) 1998, 161, 13–32. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).