1. Introduction
Heat is a notable environmental stressor of human physiology, and both heat acclimation (HA, i.e., artificially induced heat adaptation) and acclimatization (Haz, i.e., natural heat exposure), have been shown to lead to physiological adaptations that increase tolerance and exercise performance under hot conditions [
1], but the effect of the adaptive response to heat on exercise performance in cooler conditions has not been as extensively investigated. Recently, athletes have undertaken HA and HAz training as an ergogenic aid with the intent of enhancing performance in both hot and temperate conditions [
2,
3,
4,
5]. Research has focused extensively on adaptations that improve performance under hot conditions, mid- to longer-term protocols, and active HA strategies, with endurance performance being the predominant outcome measure [
6,
7,
8,
9]. There exists a paucity of research examining the actual ergogenic effect of such induced HA adaptations under temperate conditions [
2,
10], and even fewer investigating the effect of short-term passive HA strategies on anaerobic performance [
1,
11].
Standard exercise HA techniques typically involve increasing the core temperature for 1 to 2 h each day over the course of 5–16 days in an artificially hot setting [
12,
13]. HA techniques can be active or passive in nature. Commonly used active HA strategies include thermal clamping (“controlled hyperthermia technique”), “constant work rate technique”, and the “self-regulated technique” [
14,
15]. Conversely, passive HA could involve resting in an environmental heat chamber, sauna or hot bath. Previous research has investigated the use of hot-water immersion (HWI) protocols up to the level of the neck [
5,
16,
17] or waist [
18] anywhere between 6 and 21 consecutive days, [
5,
17] or every other day [
18]. HWI was either carried out following an exercise bout at a predetermined workload in a temperate laboratory [
5,
17] or independently [
16,
18]. The typical duration used for a HWI session was 30–60 min [
5,
16,
18].
A review by Heathcote et al. [
19] highlighted that passive HA strategies (sauna, HWI, and environmental chambers) can successfully induce heat adaptations, evidenced by reports of improved exercise performance, thermoregulatory, cardiovascular, and perceptual responses accompanying such interventions. According to the authors, an exercise bout should be undertaken prior to passive heat stress, rather than passive heating alone, with minimal delay between the exercise and heat stress. The heating intervention should be at least 30 min per session and be carried out on consecutive days with a minimum of 6–7 exposures to induce adaptation. However, there is no clear consensus on the precise session duration for a given heat exposure [
20]. The dominant area of interest has been whether active or passive HA can improve endurance performance under conditions of heat stress [
5,
7,
21]. However, there has been curiosity about the potential for an ergogenic effect of HA on performance under temperate conditions—a similar concept to high-altitude training, whereby athletes typically “live high, train low”, ultimately competing at sea-level whilst benefiting from the physiological adaptations accrued at altitude [
5,
10,
22]. To this end, heat training has been informally termed “the poor man’s altitude training” [
23].
To date, no study has investigated whether short-term (<7 days) daily HWI following an exercise bout in temperate conditions induces heat acclimation and improvements in anaerobic exercise performance under temperate conditions. While some studies have demonstrated the potential effectiveness of short-term HA (about 5 days) [
24], none have assessed anaerobic performance. Furthermore, the literature has used as few as 4 days of exposure to assess ergogenic benefits [
24]. Therefore, the novelty of this research was to investigate the acute effect of a short-term (two-day) passive HA protocol on anaerobic performance.
2. Methods
2.1. Participants
A total of 28 recreationally active college students volunteered to participate in this study. The participants were college students, male or female, aged 18–30 years. Participant- and group-specific demographics are presented in
Table 1. The participants were deemed eligible to be included in this study if they did not present with existing orthopedic injuries; had no medically diagnosed cardiovascular, metabolic or pulmonary condition(s); and had not been residing in a hot climate or frequently utilizing other heat acclimation strategies (e.g., sauna) within the last three months. The participants underwent screening via a Physical Activity Readiness Questionnaire (PARQ), and a thorough medical history questionnaire. All participants provided written informed consent prior to participation and the study design was conducted in accordance with the ethical principles of the Declaration of Helsinki, and it was reviewed and approved by the institutional review board for human research at Adelphi University, in accordance with the Collaborative Institutional Training Initiative (CITI Program) and the Federal Common Rule to maintain the safety of human participants.
Participants were set up on a Monark Ergomedic 828 E cycle ergometer (Monark Exercise AB, Vansbro, Sweden) such that they had a ±30° bend in their knee on a full downstroke. The Monark cycle ergometer was calibrated using a 1 kg weight prior to use. The seat height for each participant was recorded to be used for the protocol. For titration, the participants were asked to begin pedaling at 50–60 revolutions per minute (RPM) and the braking load was initially set to 1.5 kp for females and 2.0 kp for males. Heart rate was monitored continuously using the Polar Beat iPhone application (Polar Electro Oy, Kempele, Finland), with the resistance and/or RPM adjusted until the desired heart rate (HR) range (50–60% HRR) was reached and maintained for at least 3 min. The desired HRR was determined using the Karvonen formula. The individual target RPM and kp (kilopond) combination was recorded for use during the protocol.
The participants then had a 5 min break before completing the Wingate Anaerobic Power test (WAnT) familiarization. The WAnT was performed on a Lode Excalibur Sport ergometer (Lode B.V., Groningen, The Netherlands) and individual bike measurements were adjusted and recorded (seat height, seat fore-aft, handlebar height, handlebar fore-aft) for replication on subsequent tests. A torque factor of 0.70 of body mass (kg) was used for all participants. The WAnT protocol consisted of a 3 min warm-up @ 60 RPM, 50 W, followed by a 30 s all-out effort. Participants were notified one minute, 30 s, and 10 s prior to the beginning of the 30 s all-out bout. The researchers involved offered verbal encouragement throughout the 30 s effort. At the conclusion of the test, participant peak heart rate was recorded, and the participants were instructed to continue pedaling at an easy RPM for 1 min @ 50 W. They were then seated at rest for the remaining 2 min, after which a 3 min post lactate measurement was obtained via the application of a sterile lancet to the fingertip, preceded by the cleansing of the finger surface with alcohol. A single drop of blood was obtained from the surface incision and placed directly onto the Lactate Plus test strip (Lactate Plus, Nova Biomedical Corporation, Waltham, MA, USA). Before leaving, the participants were reminded of their scheduled testing time for the next day and instructed not to eat within two hours prior to returning for their Day 2 testing.
The acclimation protocol was conducted in a hydrostatic weighing tank with water temperature ranging from 38.5 to 40 °C. The participants were instructed to immerse themselves in the warm-water tank up to neck level for an additional 25 min no later than 10 min after completing their submaximal cycle. The researchers monitored the participants’ HR response during water immersion using the Polar Beat iPhone application and continuously checked in with the participants regarding their tolerance and/or discomfort levels in the warm water to mitigate against any potential, yet unlikely, adverse reactions. The participants were instructed to keep all parts of the body (except the head) immersed for the full 25 min. Following water immersion, the participants exited the tank and were seated and monitored for at least five minutes before leaving.
2.2. Protocol
The participants were randomly assigned to one of two conditions, intervention (INT) or control (CON). The submaximal cycling portion of the protocol and Wingate Anaerobic Tests (WAnT) were performed in a temperate laboratory (ambient temperature = 21–23 °C, humidity 60–65%). The water immersion (WI) intervention was conducted in a hydrostatic weighing tank located in the same building as the laboratory (water temperature = 38.5–40 °C). The first visit involved participant screening, informed consent, medical history, titration of submaximal cycling workload and familiarization with the WAnT. After initial participant intake and signing of the informed consent, basic anthropometric measurements of height (cm) using a wall-mounted stadiometer (seca GmbH & Co. KG. Hamburg, Germany) and body mass (kg) (Befour, Inc., Saukville, WI, USA) were obtained. Additionally, resting heart rate (bpm) (Polar Pro Soft chest strap & ANT+ Bluetooth H10 monitor) was also obtained.
Day 1, Titration and Familiarization:
The participants were set up and familiarized with the aforementioned submaximal bike and WAPT. Seat heights for submaximal bike and WAPT were obtained, followed by initial familiarization with the respective protocols.
Day 2, Intervention Session 1:
The participants arrived the next day within a 2 h period of their familiarization the previous day. They were fitted with a soft Polar Pro chest strap for continuous HR monitoring. The Lode Excalibur Sport ergometer was set up according to individual participant specifications, as obtained on Day 1. A pretest WAnT was then completed following the same protocol utilized in the familiarization trial (outlined above) followed by a three-minute post-lactate measurement. Thereafter, participants cycled on the Monark cycle ergometer for 25 min @ 50–60% of their calculated HRR. Heart rate was monitored continuously to ensure they stayed within the required range. Following the 25 min cycle, the participants in the INT group proceeded to immerse themselves in the warm-water tank up to neck level for an additional 25 min no later than 10 min after completing their submaximal cycle. The researchers monitored the participants’ HR response during water immersion using the Polar Beat iPhone application and continuously checked in with the participants regarding their tolerance and/or discomfort levels in the warm water to mitigate against any potential, yet unlikely, adverse reactions. The participants were instructed to keep all parts of the body (except the head) immersed for the full 25 min. Following water immersion, the participants exited the tank and were seated and monitored for at least five minutes before leaving. The CON group completed the same pretest WAnT trial followed by 25 min submaximal cycling without subsequent warm water immersion.
Day 3, Intervention Session 2: The participants arrived on Day 3 within a 24 h (±2 h) period of when they were tested the day prior. They were fitted with a soft Polar Pro HR chest strap for continuous HR monitoring, whereafter they began with their second day of 25 min of submaximal cycling on the Monark cycle ergometer @ 50–60% HRR. Following the 25 min of submaximal cycling, the participants in the INT group again proceeded to immerse themselves in the warm water tank up to neck level for 25 min, no later than 10 min after completing their submaximal cycle. The participants were instructed and monitored as per Day 2. The CON group did not immerse themselves in any water following their 25 min submaximal cycle. Following water immersion (INT) and submaximal cycle (CON), the participants underwent an acute posttest WAnT (within 10 min of exiting the water/finishing their submaximal cycle). The Lode Excalibur Sport ergometer was set up according to each individual participants’ specifications prior to the test, as obtained on Day 1.
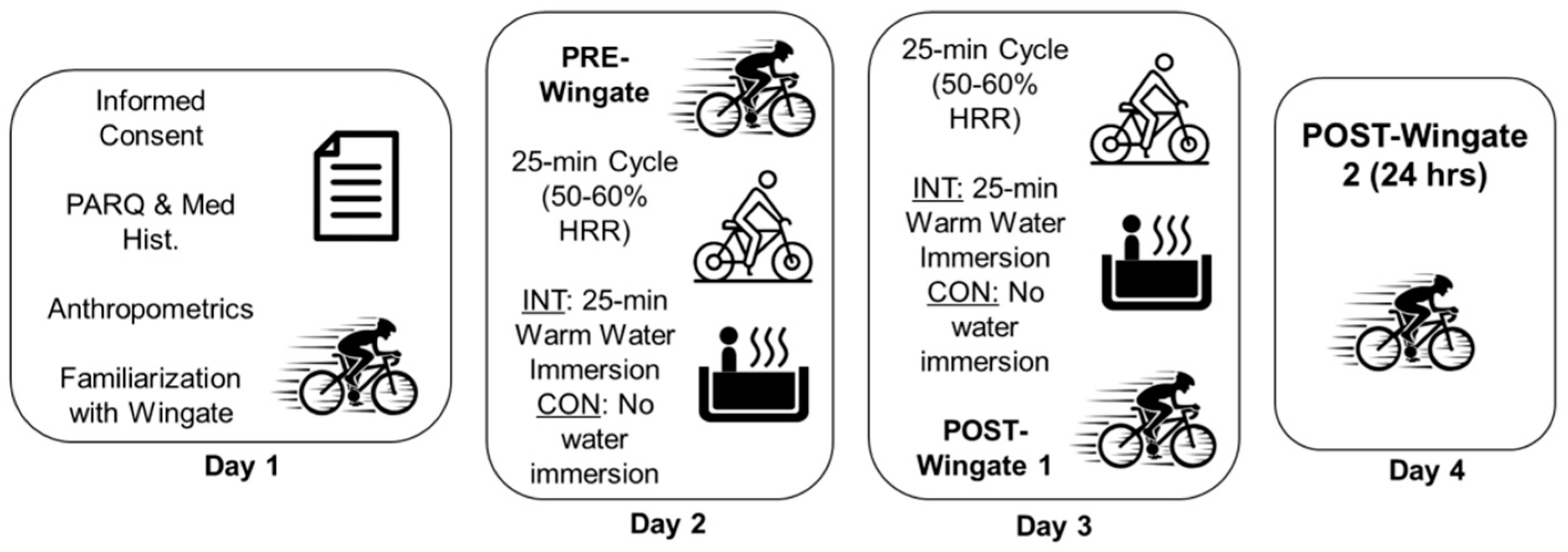
Day 4, 24 h Posttest WAnT: All participants in the INT and CON groups underwent their final post-test WAnT on the fourth and final consecutive day of testing. The participants arrived on Day 4 within a 24 h period (±2 h) of when they were tested a day prior. Once again, the participants were fitted with a soft Polar Pro HR chest strap for continuous HR monitoring, and the Lode Excalibur Sport ergometer was set up according to individual participant specifications. Peak HR was recorded following their 30 s all-out effort and a three-minute post lactate was obtained. Once the lactate reading was obtained, their testing was completed, and they were free to leave. The protocol can be seen in
Figure 1.
2.3. Statistical Analysis
Statistical analyses were conducted using IBM
® SPSS
® Statistics (Version 29). This was a between and within, repeated-measures design. Power analysis conducted using G*Power (version 3.1.9.2; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany), determined that a sample size of 26 participants was necessary for this study. The statistical power was set at 0.80 with a significance level set at 0.05 [
21]. The key outcome measures assessed were as follows: peak power (PP [W]), mean power (MP [W]), relative peak power (RPP [W/kg], fatigue index (FI [%]), and total work (TW [kJ]). A factorial ANOVA was conducted to compare the main effects of time (i.e., trial) and group (i.e., INT or CON), and the interaction effect between time and group on PP, MP, RPP, FI, and TW. Data are presented as the mean (SD), and statistical significance was accepted at
p < 0.05. Post hoc partial eta-squared effect sizes were also calculated for all dependent variables.
3. Results
After statistical analysis of the collected data (
Table 2), no significant differences were noted, with no main effects for group (INT vs. CON) or time (Trials 1–4) and no significant interaction across all measured variables (
p > 0.05), as reflected in
Table 3 and
Table 4. The means ± standard deviations for the key outcome variables for the intervention and control groups are outlined in
Table 2.
Effects on Peak Power: the multivariate statistical analysis demonstrates that there was no significant difference (p = 0.991) in Peak Power (W) between the intervention group exposed to HWI post-exercise, and the control group (not exposed to HWI post-exercise) across the various testing timepoints—Pre; immediate post; and 24 h post intervention.
Effects on Relative Peak Power: additionally, there was no significant difference (p = 0.845) noted in Relative Peak Power (W/kg) between the control group and the intervention group across the same testing timepoints outlined above.
Effects on Mean Power: The factorial ANOVA further indicated that there was no significant difference (p = 0.995) noted in Mean Power (W) between the group exposed to the HWI post-exercise and the group exposed only to the exercise stimulus. This non-significant result was consistent across the various testing timepoints.
Effects on Fatigue Index: similarly, there was no significant difference (p = 0.746) noted in Fatigue Index (%) between the control group and the intervention group across the testing timepoints.
Effects on Total Work: lastly, and unsurprisingly, there was no significant difference (p = 0.998) noted in total work (kJ) between the two groups across the testing trials.
A post hoc effect size was calculated to understand the applicability of these results to the general public. The outcome of the effect sizes is reported in
Table 3. The effect sizes for all measured dependent variables of anaerobic power combined ranged from 0.041 to 0.080. These very small effect sizes are consistent with the insignificant differences demonstrated by the p values reported in the FANOVA.
4. Discussion
To date, and to the authors’ knowledge, this study represents an inaugural attempt to investigate the effect of a short-term (two-day) passive HA protocol on anaerobic performance. The main findings were that a two-day post-exercise HWI protocol did not significantly affect measures of anaerobic power in college students between any specific testing time (familiarization, pre, acute post and 24 h post) or when compared to a control group. There are a few possible explanations for this finding, namely, the specificity of adaptations to anaerobic performance, the intervention timeframe, and the suitability of the chosen test.
The thermoregulatory and perceptual challenge imposed by a hot (±30–40 °C) and humid (>65%) environment poses a more significant challenge for endurance athletes, by elevating their risk of experiencing heat illnesses and decreased performance—particularly in athletes who are unaccustomed to such conditions [
11,
25]. This is attributed to an increased demand on thermoregulatory adjustments required to allow for heat dissipation via increased sweat rate and cutaneous circulation [
8]. Effective HA protocols result in several key physiological adaptations: decreased resting and exercising T
core and heart rate, expansion of plasma volume, earlier onset of sweating, increased sweat output and reduced perception of thermal strain [
14,
24,
26]. Expansion of blood volume (hypervolemia) has been well documented in the literature as a consequence of endurance exercise training, and as an adaptation to heat [
27]. However, erythrocyte volume (EV) does not appear to be altered by heat acclimation, with plasma volume (PV) expansion commonly—but not always—evident after repeated heat acclimation [
27]. Hypervolemia is advantageous for two key reasons: (1) increased body fluid for heat dissipation, allowing for enhanced thermoregulatory stability, and (2) larger vascular volume and filling pressure for greater cardiac stroke volume and reduced heart rate during exercise. Since blood volume (both PV and EV) was not measured during this study, it is unclear whether an expansion in PV is possible with a two-day passive HA protocol, and if it would provide any thermoregulatory benefit to the anaerobic athlete. Previous research has indicated potential benefits of passive HA protocols on aerobic exercise performance under both hot and temperate conditions [
2,
5], but there is a paucity of research assessing the effect of passive (and active) HA on anaerobic performance under similar conditions. This is likely due to the fact that endurance performance is more limited by heat stress than anaerobic performance; therefore, it stands to reason that any intervention or adaptation that serves to mitigate the negative effects of heat stress will be far more beneficial and applicable to an endurance athlete; so, the desire for investigation into an anaerobic application is understandably diminished.
This study employed a controlled hyperthermic technique to ensure equal thermal strain is placed upon participants. This was achieved by having the preceding 25 min exercise undertaken at the same relative intensity for all participants (50–60% HRR) and maintaining of the water temperature at 38.5–40 °C. The utilization of water as a modality to provide a heat effect allowed for a controlled environmental temperature. However, a disadvantage was the inability to allow exercise to occur concurrently with the hot environment. Furthermore, the lack of measurement of the physiological indices of body temperature or sweat rate limit our capacity to discuss how well the modality served a way to maintain a heat effect. This is an important consideration for future HA research as it has been established that exercise alone is an inadequate stimulus for heat adaptation in the absence of a sufficiently elevated body temperature [
28], which we were unable to reliably measure in the present study.
The WAnT has been validated as a testing protocol by comparing it to laboratory findings and sports performances, and the results show that it is an accurate and valid indicator of anaerobic capacity and power [
29]. However, a suggestion for a more relevant test to measure the effect of passive HA on anaerobic performance under hot and/or temperate conditions would be a repeated intermittent sprint performance test, as this would more closely replicate real-world sport-specific demands. Reduced intermittent cycling sprint performance in the heat has been found to be associated with increased T
core and T
muscle, thermal strain, and reduced power output [
30,
31,
32,
33]. However, another study has demonstrated improved power outputs with prior sauna exposures [
34]. The potential of HA as an ergogen for intermittent sprint exercise (running or cycling) in hot and cool conditions is not well understood or extensively researched, but there is some evidence that an active HA regimen can improve peak power output during a 40 min Cycling Intermittent Sprint Protocol [
30] and improve total distance covered during the Loughborough Intermittent Shuttle Test [
4]. However, the effect of passive HA on intermittent cycling and anaerobic running performance is still to be elucidated and is a promising area for future research, specifically including potential perceptual effects [
35]. Furthermore, exploring potential sport-specific performance effects should also continue to be studied [
36]. It is evident that the dynamic nature of sport leads to multifaceted considerations associated with the effects of HA. Specifically, future research should consider performance during intermittent activities, distance covered in sport, and the potential cognitive implications associated [
36]. This study used a sample of college students; so, generalizations to an elite population are limited. The WAnT is an all-out, effort-based test, and it is only reliable if the participant exerts a truly maximal effort, which is not verifiable. Thus, it is only assumed that each participant exerted a true maximal effort for all four trials. Fatigue may have also impacted the outcome between trials. Although it was for 30 s, the participants were not accustomed to the degree of exercise intensity and frequency of testing that was required; so, residual effects may have impacted subsequent test performance.
This study is not without limitations. The heterogeneous fitness level of the participants could have made the results difficult to normalize. Titration of the submaximal workload was a challenge, as we relied on potentially inaccurate resting HR measurements to calculate HRR. The workload we set for each participant based on Day 1 titration then needed to be adjusted on Day 2 as they performed their 25 min submaximal cycle after completing the Wingate test, which elevated their HR and made it difficult to maintain it within the range of their predicted 50–60% HRR. It may also be necessary for the exercise undertaken prior to the application of heat stress to more closely replicate the type of exercise undertaken during testing. In this study, the exercise component was a submaximal cycle for 25 min prior to water immersion. However, the outcome measure was anaerobic performance. Thus, the submaximal cycle may not be the most appropriate option and could be replaced with an anaerobic-based training activity as the exercise component. An additional potential limitation of the study design could be the lack of monitoring heart rate variability and repeat lactate assessment between conditions.
Additionally, the protocol undertaken may have been too short. HA protocols have been categorized into three time-frames—short-term (ST ≤ 7 days), medium-term (MT 8–14 days) and long-term (LT ≥ 15 days) [
24]. The literature has also overwhelmingly found that, for endurance endeavors in particular, MT-to-LT protocols reap the most rewards in terms of physiological adaptation and performance benefit—it is unclear if this holds true for anaerobic performance too [
3,
5,
14,
18,
25]. We did not measure physiological variables related to thermoregulation or hemodynamics; so, we cannot speculate on the degree to which heat adaptation (if any) occurred, regardless of the apparent lack of performance benefit. Furthermore, the lack of measurement of internal and external body temperature also serves as a limitation to this study.