Comparison of Blood Flow Characteristics in Young Healthy Males between High-Intensity Interval and Moderate-Intensity Continuous Exercise
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Power Calculations
2.2. Screening and Overview
2.3. Maximal Exercise Test
2.4. Exercise Visits
2.5. Brachial Artery Ultrasound
2.6. Statistical Analysis
3. Results
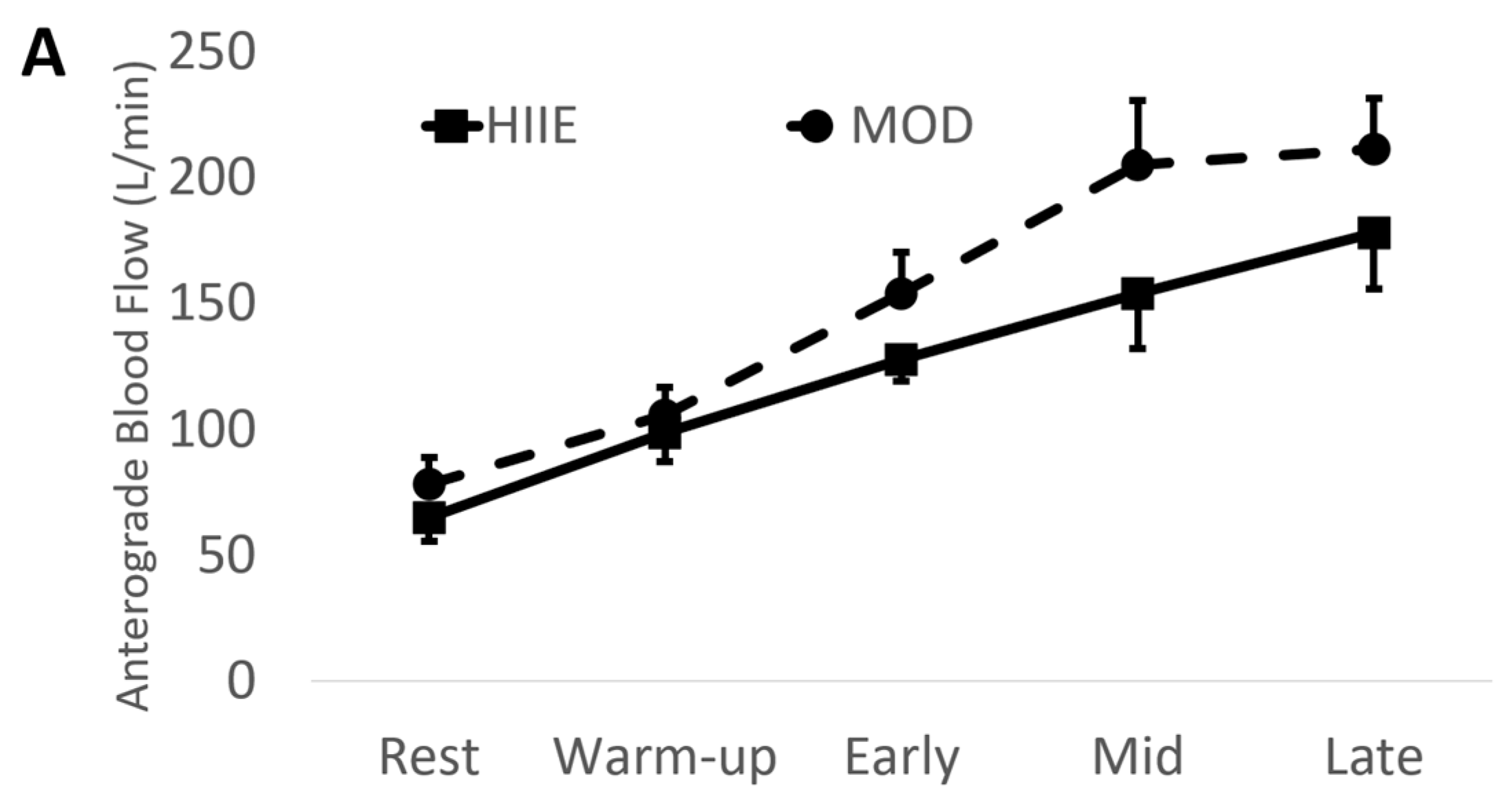
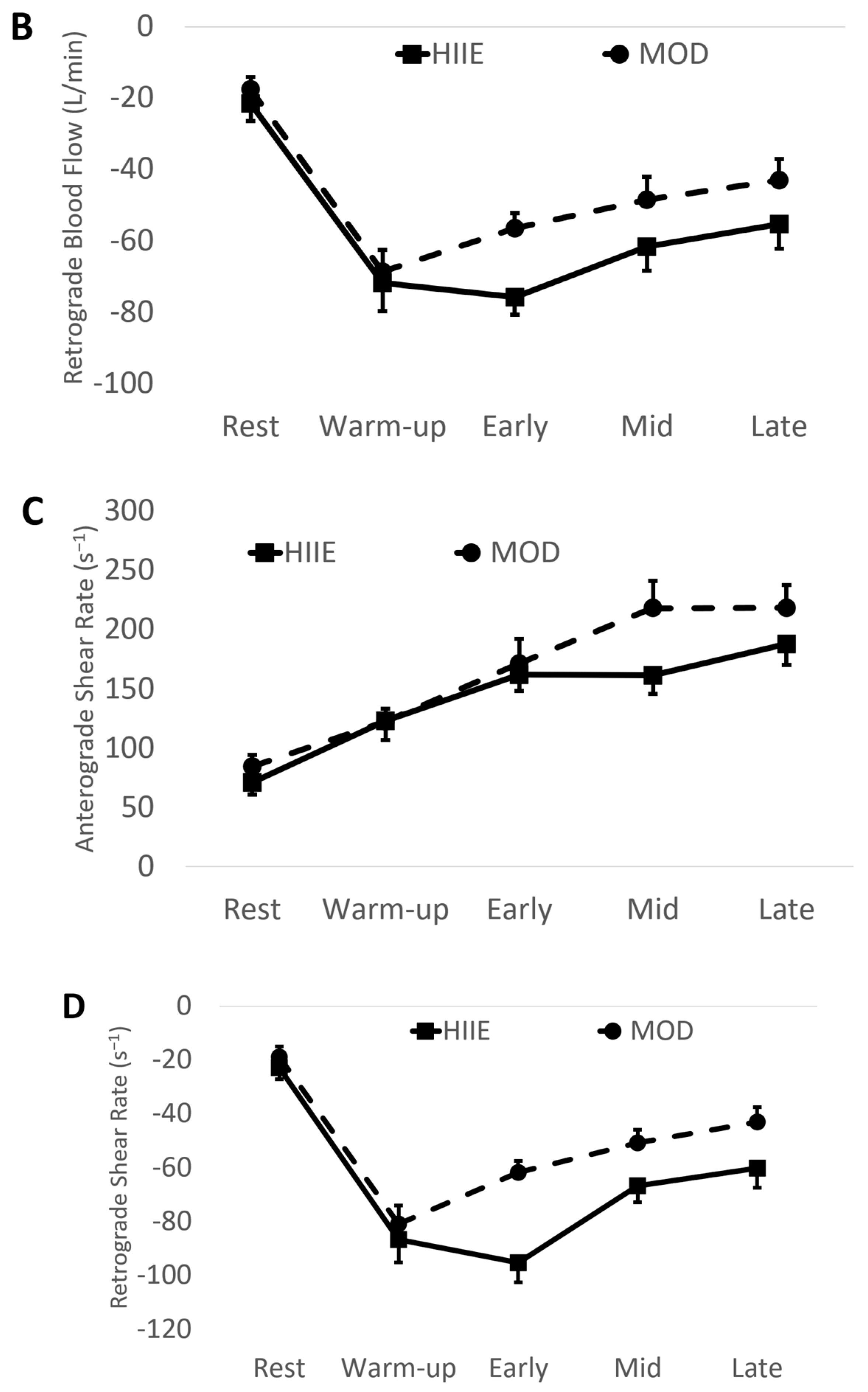
3.1. During Exercise
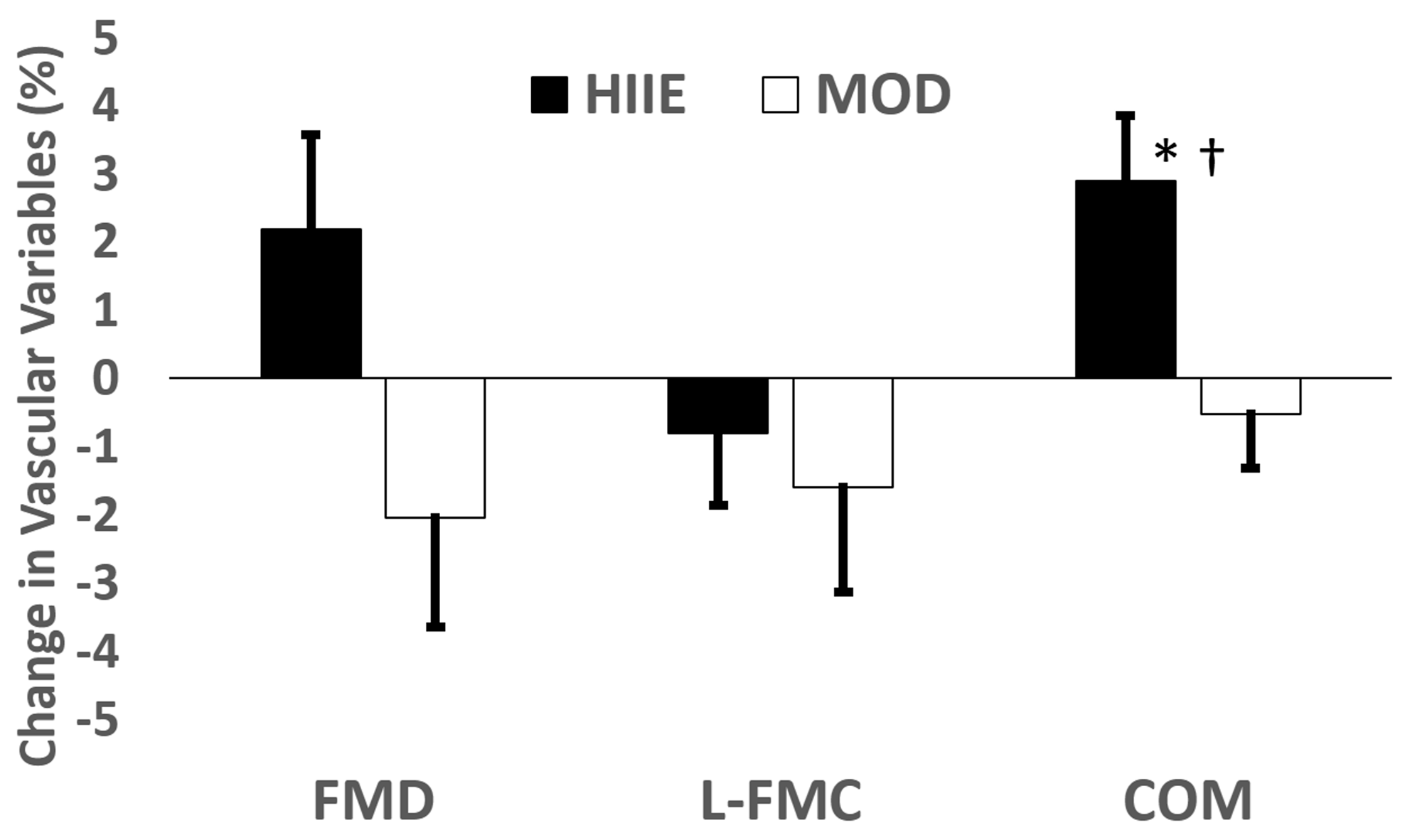
3.2. Vascular Measures
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vanhoutte, P.M. Endothelial dysfunction: The first step toward coronary arteriosclerosis. Circ. J. 2009, 73, 595–601. [Google Scholar] [CrossRef]
- Celermajer, D.S.; Sorensen, K.E.; Gooch, V.M.; Spiegelhalter, D.J.; Miller, O.I.; Sullivan, I.D.; Lloyd, J.K.; Deanfield, J.E. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992, 340, 1111–1115. [Google Scholar] [CrossRef]
- Inaba, Y.; Chen, J.A.; Bergmann, S.R. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: A meta-analysis. Int. J. Cardiovasc. Imaging 2010, 26, 631–640. [Google Scholar] [CrossRef]
- Ras, R.T.; Streppel, M.T.; Draijer, R.; Zock, P.L. Flow-mediated dilation and cardiovascular risk prediction: A systematic review with meta-analysis. Int. J. Cardiol. 2013, 168, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Green, D.J. Exercise training as vascular medicine: Direct impacts on the vasculature in humans. Exerc. Sport. Sci. Rev. 2009, 37, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Thijssen, D.H.; Maiorana, A.J.; O’Driscoll, G.; Cable, N.T.; Hopman, M.T.; Green, D.J. Impact of inactivity and exercise on the vasculature in humans. Eur. J. Appl. Physiol. 2010, 108, 845–875. [Google Scholar] [CrossRef]
- Ramos, J.S.; Dalleck, L.C.; Tjonna, A.E.; Beetham, K.S.; Coombes, J.S. The impact of high-intensity interval training versus moderate-intensity continuous training on vascular function: A systematic review and meta-analysis. Sports Med. 2015, 45, 679–692. [Google Scholar] [CrossRef]
- Hollekim-Strand, S.M.; Bjørgaas, M.R.; Albrektsen, G.; Tjønna, A.E.; Wisløff, U.; Ingul, C.B. High-intensity interval exercise effectively improves cardiac function in patients with type 2 diabetes mellitus and diastolic dysfunction: A randomized controlled trial. J. Am. Coll. Cardiol. 2014, 64, 1758–1760. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, B.J.; Tucker, W.J.; Bhammar, D.M.; Ryder, J.R.; Sweazea, K.L.; Gaesser, G.A. Effects of high-intensity interval training and moderate-intensity continuous training on endothelial function and cardiometabolic risk markers in obese adults. J. Appl. Physiol. (1985) 2016, 121, 279–288. [Google Scholar] [CrossRef]
- Currie, K.D.; Dubberley, J.B.; McKelvie, R.S.; MacDonald, M.J. Low-volume, high-intensity interval training in patients with CAD. Med. Sci. Sports Exerc. 2013, 45, 1436–1442. [Google Scholar] [CrossRef]
- Klonizakis, M.; Moss, J.; Gilbert, S.; Broom, D.; Foster, J.; Tew, G.A. Low-volume high-intensity interval training rapidly improves cardiopulmonary function in postmenopausal women. Menopause 2014, 21, 1099–1105. [Google Scholar] [CrossRef] [PubMed]
- Mitranun, W.; Deerochanawong, C.; Tanaka, H.; Suksom, D. Continuous vs interval training on glycemic control and macro- and microvascular reactivity in type 2 diabetic patients. Scand. J. Med. Sci. Sports 2014, 24, e69–e76. [Google Scholar] [CrossRef] [PubMed]
- Moholdt, T.; Aamot, I.L.; Granøien, I.; Gjerde, L.; Myklebust, G.; Walderhaug, L.; Brattbakk, L.; Hole, T.; Graven, T.; Stølen, T.O.; et al. Aerobic interval training increases peak oxygen uptake more than usual care exercise training in myocardial infarction patients: A randomized controlled study. Clin. Rehabil. 2012, 26, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Tinken, T.M.; Thijssen, D.H.; Black, M.A.; Cable, N.T.; Green, D.J. Time course of change in vasodilator function and capacity in response to exercise training in humans. J. Physiol. 2008, 586, 5003–5012. [Google Scholar] [CrossRef] [PubMed]
- Dinenno, F.A.; Tanaka, H.; Monahan, K.D.; Clevenger, C.M.; Eskurza, I.; DeSouza, C.A.; Seals, D.R. Regular endurance exercise induces expansive arterial remodelling in the trained limbs of healthy men. J. Physiol. 2001, 534, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Shenouda, N.; Gillen, J.B.; Gibala, M.J.; MacDonald, M.J. Changes in brachial artery endothelial function and resting diameter with moderate-intensity continuous but not sprint interval training in sedentary men. J. Appl. Physiol. (1985) 2017, 123, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Spence, A.L.; Carter, H.H.; Naylor, L.H.; Green, D.J. A prospective randomized longitudinal study involving 6 months of endurance or resistance exercise. Conduit artery adaptation in humans. J. Physiol. 2013, 591, 1265–1275. [Google Scholar] [CrossRef] [PubMed]
- Green, D.J.; Spence, A.; Halliwill, J.R.; Cable, N.T.; Thijssen, D.H. Exercise and vascular adaptation in asymptomatic humans. Exp. Physiol. 2011, 96, 57–70. [Google Scholar] [CrossRef]
- Birk, G.K.; Dawson, E.A.; Atkinson, C.; Haynes, A.; Cable, N.T.; Thijssen, D.H.; Green, D.J. Brachial artery adaptation to lower limb exercise training: Role of shear stress. J. Appl. Physiol. (1985) 2012, 112, 1653–1658. [Google Scholar] [CrossRef]
- Birk, G.K.; Dawson, E.A.; Batterham, A.M.; Atkinson, G.; Cable, T.; Thijssen, D.H.; Green, D.J. Effects of exercise intensity on flow mediated dilation in healthy humans. Int. J. Sports Med. 2013, 34, 409–414. [Google Scholar] [CrossRef]
- Green, D.; Cheetham, C.; Reed, C.; Dembo, L.; O’Driscoll, G. Assessment of brachial artery blood flow across the cardiac cycle: Retrograde flows during cycle ergometry. J. Appl. Physiol. (1985) 2002, 93, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Green, D.J.; Bilsborough, W.; Naylor, L.H.; Reed, C.; Wright, J.; O’Driscoll, G.; Walsh, J.H. Comparison of forearm blood flow responses to incremental handgrip and cycle ergometer exercise: Relative contribution of nitric oxide. J. Physiol. 2005, 562, 617–628. [Google Scholar] [CrossRef] [PubMed]
- Padilla, J.; Simmons, G.H.; Vianna, L.C.; Davis, M.J.; Laughlin, M.H.; Fadel, P.J. Brachial artery vasodilatation during prolonged lower limb exercise: Role of shear rate. Exp. Physiol. 2011, 96, 1019–1027. [Google Scholar] [CrossRef] [PubMed]
- Simmons, G.H.; Padilla, J.; Young, C.N.; Wong, B.J.; Lang, J.A.; Davis, M.J.; Laughlin, M.H.; Fadel, P.J. Increased brachial artery retrograde shear rate at exercise onset is abolished during prolonged cycling: Role of thermoregulatory vasodilation. J. Appl. Physiol. (1985) 2011, 110, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Thijssen, D.H.; Dawson, E.A.; Black, M.A.; Hopman, M.T.; Cable, N.T.; Green, D.J. Brachial artery blood flow responses to different modalities of lower limb exercise. Med. Sci. Sports Exerc. 2009, 41, 1072–1079. [Google Scholar] [CrossRef] [PubMed]
- Tinken, T.M.; Thijssen, D.H.; Hopkins, N.; Dawson, E.A.; Cable, N.T.; Green, D.J. Shear stress mediates endothelial adaptations to exercise training in humans. Hypertension 2010, 55, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Ozaki, K.; Hori, T.; Ishibashi, T.; Nishio, M.; Aizawa, Y. Effects of chronic cigarette smoking on endothelial function in young men. J. Cardiol. 2010, 56, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Corretti, M.C.; Anderson, T.J.; Benjamin, E.J.; Celermajer, D.; Charbonneau, F.; Creager, M.A.; Deanfield, J.; Drexler, H.; Gerhard-Herman, M.; Herrington, D.; et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J. Am. Coll. Cardiol. 2002, 39, 257–265. [Google Scholar] [CrossRef]
- Thijssen, D.H.; Black, M.A.; Pyke, K.E.; Padilla, J.; Atkinson, G.; Harris, R.A.; Parker, B.; Widlansky, M.E.; Tschakovsky, M.E.; Green, D.J. Assessment of flow-mediated dilation in humans: A methodological and physiological guideline. Am. J. Physiol.-Heart Circ. Physiol. 2011, 300, H2–H12. [Google Scholar] [CrossRef]
- Bassett, D.R.; Howley, E.T.; Thompson, D.L.; King, G.A.; Strath, S.J.; McLaughlin, J.E.; Parr, B.B. Validity of inspiratory and expiratory methods of measuring gas exchange with a computerized system. J. Appl. Physiol. (1985) 2001, 91, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Sedgeman, D.; Dalleck, L.; Clark, I.E.; Jamnick, N.; Pettitt, R.W. Analysis of square-wave bouts to verify VO2max. Int. J. Sports Med. 2013, 34, 1058–1062. [Google Scholar] [CrossRef] [PubMed]
- Poole, D.C.; Jones, A.M. Measurement of the maximum oxygen uptake VO2max: VO2peak is no longer acceptable. J. Appl. Physiol. (1985) 2017, 122, 997–1002. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, B.J.; McMahon, N.; Thornhill, K.L.; Baughman, B.R.; Mahoney, J.M.; Pattison, K.L.; Freeberg, K.A.; Botts, R.T. Supra-Versus Submaximal Cycle Ergometer Verification of VO2max in Males and Females. Sports 2020, 8, 163. [Google Scholar] [CrossRef] [PubMed]
- Gemignani, V.; Faita, F.; Ghiadoni, L.; Poggianti, E.; Demi, M. A system for real-time measurement of the brachial artery diameter in B-mode ultrasound images. IEEE Trans. Med. Imaging 2007, 26, 393–404. [Google Scholar] [CrossRef] [PubMed]
- Ghiadoni, L.; Faita, F.; Salvetti, M.; Cordiano, C.; Biggi, A.; Puato, M.; Di Monaco, A.; De Siati, L.; Volpe, M.; Ambrosio, G.; et al. Assessment of flow-mediated dilation reproducibility: A nationwide multicenter study. J. Hypertens. 2012, 30, 1399–1405. [Google Scholar] [CrossRef] [PubMed]
- Tucker, W.J.; Sawyer, B.J.; Jarrett, C.L.; Bhammar, D.M.; Gaesser, G.A. Physiological Responses to High-Intensity Interval Exercise Differing in Interval Duration. J. Strength Cond. Res. 2015, 29, 3326–3335. [Google Scholar] [CrossRef] [PubMed]
- Green, D.J.; O’Driscoll, G.; Joyner, M.J.; Cable, N.T. Exercise and cardiovascular risk reduction: Time to update the rationale for exercise? J. Appl. Physiol. (1985) 2008, 105, 766–768. [Google Scholar] [CrossRef] [PubMed]
- Tinken, T.M.; Thijssen, D.H.; Hopkins, N.; Black, M.A.; Dawson, E.A.; Minson, C.T.; Newcomer, S.C.; Laughlin, M.H.; Cable, N.T.; Green, D.J. Impact of shear rate modulation on vascular function in humans. Hypertension 2009, 54, 278–285. [Google Scholar] [CrossRef]
- Delp, M.D.; Laughlin, M.H. Regulation of skeletal muscle perfusion during exercise. Acta Physiol. Scand. 1998, 162, 411–419. [Google Scholar] [CrossRef]
- Just, T.P.; Cooper, I.R.; DeLorey, D.S. Sympathetic Vasoconstriction in Skeletal Muscle: Adaptations to Exercise Training. Exerc. Sport Sci. Rev. 2016, 44, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Dawson, E.A.; Green, D.J.; Cable, N.T.; Thijssen, D.H. Effects of acute exercise on flow-mediated dilatation in healthy humans. J. Appl. Physiol. (1985) 2013, 115, 1589–1598. [Google Scholar] [CrossRef] [PubMed]
- Currie, K.D.; McKelvie, R.S.; Macdonald, M.J. Flow-mediated dilation is acutely improved after high-intensity interval exercise. Med. Sci. Sports Exerc. 2012, 44, 2057–2064. [Google Scholar] [CrossRef] [PubMed]
- Bailey, T.G.; Perissiou, M.; Windsor, M.; Russell, F.; Golledge, J.; Green, D.J.; Askew, C.D. Cardiorespiratory fitness modulates the acute flow-mediated dilation response following high-intensity but not moderate-intensity exercise in elderly men. J. Appl. Physiol. (1985) 2017, 122, 1238–1248. [Google Scholar] [CrossRef] [PubMed]
- Hwang, I.C.; Kim, K.H.; Choi, W.S.; Kim, H.J.; Im, M.S.; Kim, Y.J.; Kim, S.H.; Kim, M.A.; Sohn, D.W.; Zo, J.H. Impact of acute exercise on brachial artery flow-mediated dilatation in young healthy people. Cardiovasc. Ultrasound 2012, 10, 39. [Google Scholar] [CrossRef] [PubMed]
- Rognmo, O.; Bjørnstad, T.H.; Kahrs, C.; Tjønna, A.E.; Bye, A.; Haram, P.M.; Stølen, T.; Slørdahl, S.A.; Wisløff, U. Endothelial function in highly endurance-trained men: Effects of acute exercise. J. Strength Cond. Res. 2008, 22, 535–542. [Google Scholar] [CrossRef]
- Gori, T.; Grotti, S.; Dragoni, S.; Lisi, M.; Di Stolfo, G.; Sonnati, S.; Fineschi, M.; Parker, J.D. Assessment of vascular function: Flow-mediated constriction complements the information of flow-mediated dilatation. Heart 2010, 96, 141–147. [Google Scholar] [CrossRef]


| Mean ± SD (n = 16) | |
|---|---|
| Age (yr) | 22.5 ± 3.2 |
| Height (cm) | 176.95 ± 8.64 |
| Weight (kg) | 77.78 ± 9.18 |
| BMI (kg/m2) | 25.5 ± 3.0 |
| VO2max (mL/kg/min) | 43.6 ± 6.2 |
| MOD (n = 15) | HIIE (n = 15) | p Value # | F Statistic | Effect Size (Partial eta2) | |
|---|---|---|---|---|---|
| Diameter (mm) | 4.30 ± 0.42 | 4.22 ± 0.33 | 0.34 | 0.91 | 0.012 |
| Anterograde Blood Flow (mL/min) | 191.3 ± 80.3 | 153.9 ± 67.5 | 0.03 * | 4.89 | 0.039 |
| Retrograde Blood Flow (mL/min) | −48.7 ± 21.3 | −63.9 ± 23.3 | <0.01 * | 9.01 | 0.027 |
| Anterograde Blood Velocity (cm/s) | 21.7 ± 8.1 | 18.0 ± 6.1 | 0.02 * | 5.27 | 0.065 |
| Retrograde Blood Velocity (cm/s) | −5.5 ± 2.0 | −7.8 ± 2.8 | <0.01 * | 15.58 | 0.170 |
| Anterograde Shear Rate (s−1) | 203.5 ± 78.1 | 170.8 ± 55.5 | 0.04 * | 4.44 | 0.055 |
| Retrograde Shear Rate (s−1) | −51.5 ± 19.8 | −73.8 ± 28.4 | <0.01 * | 16.54 | 0.179 |
| HIIE On | HIIE Off | MOD | Post Hoc p-Values | ||||
|---|---|---|---|---|---|---|---|
| Main Effect p-Values #, F Statistic, Partial eta2 | On vs. Off | On vs. MOD | Off vs. MOD | ||||
| Diameter (mm) | 4.22 ± 0.38 | 4.22 ± 0.37 | 4.30 ± 0.42 | 0.72, 0.45, 0.010 | 1.00 | 1.00 | 1.00 |
| Anterograde Blood Flow (mL/min) | 142.5 ± 73.7 | 164.8 ± 81.7 | 191.3 ± 80.3 | 0.04 *, 2.89, 0.059 | 0.81 | 0.04 * | 0.48 |
| Retrograde Blood Flow (mL/min) | −77.5 ± 29.6 | −49.6 ± 21.9 | −48.7 ± 21.3 | <0.01 *, 10.93, 0.192 | <0.01 * | <0.01 * | 1.00 |
| Anterograde Blood Velocity (cm/s) | 16.4 ± 6.5 | 19.2 ± 7.8 | 21.7 ± 8.1 | 0.01 *, 3.71, 0.075 | 0.46 | 0.01 * | 0.46 |
| Retrograde Blood Velocity (cm/s) | −9.22 ± 3.2 | −6.0 ± 2.7 | −5.5 ± 2.0 | <0.01 *, 13.94, 0.233 | <0.01 * | <0.01 * | 1.00 |
| Anterograde Shear Rate (s−1) | 154.8 ± 56.1 | 181.7 ± 71.5 | 203.5 ± 78.1 | 0.02 *, 3.55, 0.072 | 0.41 | 0.02 * | 0.58 |
| Retrograde Shear Rate (s−1) | −88.4 ± 31.3 | −57.8 ± 27.7 | −51.5 ± 19.8 | <0.01 *, 13.45, 0.226 | <0.01 * | <0.01 * | 0.92 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baughman, B.R.; Sawyer, B.J. Comparison of Blood Flow Characteristics in Young Healthy Males between High-Intensity Interval and Moderate-Intensity Continuous Exercise. Physiologia 2024, 4, 253-265. https://doi.org/10.3390/physiologia4030015
Baughman BR, Sawyer BJ. Comparison of Blood Flow Characteristics in Young Healthy Males between High-Intensity Interval and Moderate-Intensity Continuous Exercise. Physiologia. 2024; 4(3):253-265. https://doi.org/10.3390/physiologia4030015
Chicago/Turabian StyleBaughman, Brett R., and Brandon J. Sawyer. 2024. "Comparison of Blood Flow Characteristics in Young Healthy Males between High-Intensity Interval and Moderate-Intensity Continuous Exercise" Physiologia 4, no. 3: 253-265. https://doi.org/10.3390/physiologia4030015
APA StyleBaughman, B. R., & Sawyer, B. J. (2024). Comparison of Blood Flow Characteristics in Young Healthy Males between High-Intensity Interval and Moderate-Intensity Continuous Exercise. Physiologia, 4(3), 253-265. https://doi.org/10.3390/physiologia4030015








