Abstract
(1) Background: Periodontal instrumentation with dental curettes is associated with discomfort, fatigue, and musculoskeletal diseases. The goal of this study was to compare comfort, fatigue, and muscle work using three different curettes. (2) Methods: Eight hygienists each scaled three typodonts using the three different curettes. Curette A was a prototype with a novel adaptive design, Curette B had a conventional stainless-steel design, and Curette C featured a conventional silicon-covered handle. Time-based work in four muscles, comfort, fatigue, tactile feedback, grip and blade position, and pinch and grasp strength were recorded. Statistical analysis was performed using a General Linear Model (GLIM) and Tukey’s post hoc test. The level of significance was set at p < 0.05. (3) Results: Comfort, correct grasp, fingertip placement, and blade-to-tooth adaptation were significantly better with Curette A (p < 0.05). While pinch and grasp strength were significantly reduced post-instrumentation for Curettes B and C (p < 0.05), they remained unchanged for Curette A. Curette A required significantly less total muscle work and work in individual muscles, resulting in significantly less post-instrumentation fatigue than for Curettes B and C, but similar levels of tactile feedback (p < 0.05). (4) Conclusions: The ergonomic performance of a prototype adaptive periodontal curette was significantly better than that of two conventional instruments with rigid handle designs.
1. Introduction
The need to remove hard and soft deposits from the teeth has been recognized for many centuries [1]. In the mid-eighteenth century, Pierre Fauchard, who is often called the “father of modern dentistry”, described dental calculus and the need to remove it to maintain oral health. The design and materials used in dental instruments from that era are surprisingly similar to those in use today, despite considerable progress in our understanding of the mechanics, functionalities, and ergonomics of dental instrumentation. Because periodontal curettes are used for many hours daily by hygienists, requiring high-force, precise, and repetitive movements over long periods of time, their functionality and ergonomics stand out as being especially important in ensuring the health of patients and the clinicians who use them. The introduction of ultrasonic scalers has provided some respite; however, they do not replace all of the functions of hand instruments [2].
In dental clinicians, the ergonomic hazards caused by strained posture and prolonged repetitive movements can induce musculoskeletal disorders (MSDs). These are reported to occur in 54–93% of dental professionals and involve the spine, shoulder, and hand-wrist tract [3,4]. Extensive research has shown that, in the U.S., dental hygienists have the highest prevalence of any profession of instrumentation-related conditions such as carpal tunnel syndrome (CTS) [5], musculoskeletal diseases (MSDs) [6,7], and upper extremity disorders [5,8,9,10,11,12,13]. Within any 12-month period, 64–96% of hygienists experience symptoms of MSDs, and almost 50% of hygienists report symptoms of carpal tunnel syndrome (CTS) [14]. Dentists also suffer the consequences of prolonged and repetitive instrumentation, with up to two-thirds of all dental clinicians reporting related musculoskeletal pain [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. Indeed, after several years in clinical practice, most hygienists are unable to work full-time due to the consequences of work-related MSDs, which adversely affect clinical effectiveness, productivity, and work satisfaction [12,16,22]. Similarly, nearly one-third of dentists are forced to retire early because of work-related MSDs [22]. The consequences of this situation are personal and financial. One study estimated MSD-related poor sleep quality and a high level of stress in up to 48.1% of dental clinicians, a prevalence of frequent pain ranging from 6.4–46.5%, and reduced work ability in 33% of clinicians. Poor sleep, a high amount of stress, and multi-site pain were associated with a decreased ability to work [33]. In another study, investigators estimated an annual income loss of $131 million due to MSDs in the dental profession [34].
With the availability of increasingly diverse dental instrument materials and ever more sophisticated non-invasive tools for the real-time mapping of positioning, movement, and muscle work, new approaches to instrument design and construction are being evaluated. Novel image analysis techniques, quantitative positioning approaches, video tracking, and force and pressure sensors that can be mounted on the fingers, hands, or the instrument itself are all being explored. For example, studies on the role of the handle diameter and surface material on specific ergonomic properties of dental curettes have determined that somewhat larger diameter, lighter instruments, with resin- or silicone-covered, warmer, and softer instrument handles can be beneficial [35,36,37,38,39,40,41]. However, given the prevalence and severity of instrumentation-related MSDs in dental clinicians, more extensive, groundbreaking concepts to improve instrument design need to be developed and researched. The parameters that are currently used to assess ergonomic impact include measurements of muscle work [35,38,42,43], body posture, and movement [35,44,45], as well as pinch and grasp strength [37,46,47]. Better non-invasive tools for mapping the effects of each variable that may impact the development of MSDs also need to be developed and validated.
The goal of this in vivo study was to compare muscle work, comfort, fatigue, tactile feedback, grip, and blade position as well as pinch and grasp strength associated with performing a standardized scaling task using three periodontal curettes with different handle designs and materials. This study addresses gaps in our knowledge with regard to the actual muscle work performed in specific muscles during a set instrumentation task, the effects of the handle design on the clinician’s grip, grasp, instrumentation technique, and blade positioning, and the clinician’s semi-quantitative self-assessment of comfort and fatigue related to instrumentation.
2. Materials and Methods
All testing was performed by dental hygienists using standard typodont models. After a review by the University of California, Irvine’s IRB, this protocol was granted exempt status, as only de-identified data were collected and used in this study.
2.1. Testers
Eight right-handed hygienists, who are all experienced periodontal instrumentation instructors at local Schools of Dental Hygiene (University of Southern California, West Coast University, Cypress College, Cerritos College, San Joaquin Valley College, and Concorde College Schools of Dental Hygiene) participated in this study. Individuals with any injuries or disorders of their fingers, hands, or wrists within 6 months of this research and those with any symptoms or diagnosis of upper-extremity MSDs were excluded from the study.
2.2. Protocol
In order to ensure that the scaling task was identical for each test arm, artificial biofilm (Occlude Green Marking Spray, Pascal International, Bellevue, WA, USA) and calculus (Dental Calculus Set, Kilgore International Inc., Coldwater, MI, USA) were applied supra- and sub-gingivally to 32 artificial typodont teeth by the same researcher in a standardized fashion. Because artificial calculus increases in hardness over time, the biofilm and calculus were applied sequentially 18 h before each study arm. Once the artificial calculus had hardened, the teeth were mounted in a typodont model, which was then attached to a manikin (Kilgore International Inc., Coldwater, MI, USA). Before the beginning of clinical testing, each manikin was fixed onto a clinical dental chair. Next, testers were asked to adjust their chair, working positions, and typodont angle to their preferred configuration. The hygienists were allowed to change their seating position and adjust the typodont position as needed throughout the study. Whenever an adjustment of this kind was made, it was noted, so that its resultant disruptions in the sEMG trace could be identified. Hygienists were instructed to complete periodontal instrumentation as if they were working on a live patient, with the goal of removing all the simulated plaque and calculus deposits completely without damaging the underlying teeth or simulated soft tissues. The total study duration was approximately 60–90 min.
Each hygienist tested all 3 of the universal curettes (Barnhart 5/6), with the sequence of use randomized using the research randomizer software (randomizer.org, accessed on 14 August 2023). Research Randomizer is a free resource for researchers and students which generates random numbers or randomly assigns participants to experimental groups. Each curette was sharpened by the same experienced dental hygiene instructor each time before it was used. Testers were shown a 1-min instructional video on the use of the adaptive curette; then they were given 5 min to accustom themselves to the instruments before beginning instrumentation.
Hygienists worked sequentially on 3 typodont models, scaling one model with each type of curette. The total scaling duration was 8 min for each typodont, with a 20 min rest period between each of the 3 study arms. The duration of the rest period between each study arm was validated in prior studies [48], ensuring that all evaluation parameters had returned to baseline before the next study arm began. Testers spent 1 min scaling each typodont segment, following the same routine for all 3 curettes: (1) lower anterior sextant facial surfaces, (2) lower anterior sextant lingual surfaces, (3) upper anterior sextant facial surfaces, (4) upper anterior lingual surfaces, (5) lower right sextant buccal surfaces, (6) lower left sextant buccal surfaces, (7) upper right buccal surfaces, and (8) upper right sextant lingual surfaces.
2.3. Instruments
The characteristics of the 3 universal curettes (Barnhart 5/6) with stainless-steel tips that were used in this study are presented in Table 1, and representative photos of the curettes during testing are shown in Figure 1. A brief description of each instrument tested in this study is provided below:

Table 1.
Overview of instruments tested in this study, showing almost identical handle lengths, instrument lengths, weights, and blade materials for all curettes.
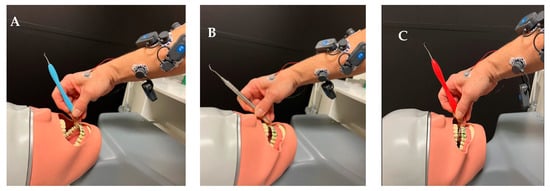
Figure 1.
Dental curettes tested in this study: (A) prototype adaptive curette; (B) conventional stainless-steel curette; (C) conventional curette featuring a silicone-covered rigid handle.
Curette A: a prototype (5/6 Barnhart) whose novel handle design features a flexible, universally adjustable core, which allows the instrument to adapt to the curvature of the hand and fingers. A silicone overlay of the handle provided a cushioned, thermally insulated grip.
Curette B: a conventional stainless-steel curette whose parameters align closely with some of the most widely used curettes (5/6 Barnhart Curette Stainless Steel, Sterling®, Menlo Park, Gauteng, South Africa).
Curette C: a conventional curette featuring a cushioned, thermally insulated silicone-covered rigid handle (LM DuraGradeMAX, LM Dental, FI-21600 Parainen, Finland)
2.4. Video Image Analysis: Grasp and Positioning
Testers’ dominant hands were filmed throughout instrumentation to permit ensuing evaluation of instrument grasp, fingertip placement, and blade-to-tooth angulation, as well as forearm and wrist positions. Using these video recordings, one pre-standardized dental hygienist with more than 20 years of instrumentation expertise (CW) evaluated the following variables: Video Image Analysis: Grasp and Positioning. Ideally, the scorer should have been blinded with regard to the handle design, but this was not possible as they needed to view the entire hand during the assessment, which meant that they were able to see which curette was being used during each evaluation.
- Clinicians’ grasp
- Finger pad positioning, including thumb, index, and middle finger placement on the instrument handle and functional shank: Correct/Incorrect.
- Maintaining an ergonomically relaxed, C- or V-shaped convex configuration of the index finger and thumb, using a “knuckles up” position to prevent joint hyperextension: Yes/No.
- Fingertip blanching, indicative of an excessively tight grasp: Yes/No.
- Blade-to-tooth adaptation: 60–80-degree angle: Correct/Incorrect.
- Instrument activation: Avoidance of finger flexing to initiate working strokes: Correct/Incorrect.
2.5. VAS Surveys and Open-Ended Comments
VAS surveys using a hard-copy scale of 0–10 were recorded immediately at the end of each study arm. Visual VAS scales with a range of 0–10 are commonly used for semi-quantitative assessment of non-quantifiable data. One survey evaluated tester fatigue, the second documented user comfort in wrist, fingers, and palm, with 0 being no fatigue or discomfort and 10 being extreme fatigue or discomfort, and the third recorded testers’ evaluation of the quality of tactile feedback from each instrument. Clinicians were also asked to provide open-ended comments regarding the 3 instruments and the 2 handle designs. Finally, participants were asked to indicate which instrument they preferred and why.
2.6. Dynamometry
Standard dynamometers (Jamar, J.A. Preston Corp., Clifton, NJ, USA) were used to measure pinch and grasp strength before and after each study arm (Figure 2). Each measurement was repeated three times, and the tester was blinded during the measurement.

Figure 2.
(A) Pinch; (B) Grasp; (C) Strength Dynamometers and Electrode Placement.
2.7. Surface Electromyography (sEMG)
Real-time, continuous surface EMG (sEMG) measurements were recorded using surface EMG electrodes (FREEEMG, ©BTS Engineering, Quincy, MA, USA) from 4 muscles that are specifically used for gripping and manipulating dental instruments [5,8,35,37,38,43,45,46,49]: Abductor Pollicis Brevis (APB), First Dorsal Interosseous (FDI), Flexor Pollicis Longus (FPL), and Extensor Digitorum Communis (EDC). The electric action potential signals were transmitted wirelessly to a Dell laptop via a USB-port dongle that connected with proprietary FREEEMG software from BTS Engineering on the laptop computer (FREEEMG, ©BTS Engineering, Quincy, MA, USA). sEMG mapping was conducted using a standardized protocol that was repeated for each testing sequence in each hygienist. First, live muscle function tests were performed to guide and fine-tune the placement of each electrode to an optimal position on each muscle (Figure 2) [50]. Next, a commonly used approach that permits subsequent normalization of test data was implemented by asking the testers to perform 15 s of maximum voluntary isometric contractions (MVC) for each muscle [51], and this trace was then considered 100% activity for that muscle [52,53,54,55].
Next, testers executed the prescribed scaling regimen. Surface EMG (sEMG) signals from all 4 muscles were recorded throughout instrumentation. After the data collection was completed, raw sEMG signals were rectified and filtered using a second-order Butterworth filter with a 10 Hz high-pass cutoff frequency using the proprietary FREEEMG software from BTS Engineering on the laptop computer (FREEEMG, ©BTS Engineering, Quincy, MA, USA). Finally, total muscle activity for each curette was calculated from the integrated EMG curve, which measures the total area under the curve (total workload) over the entire period of instrumentation.
Testers could not be blinded because of the very different appearance and functionality of Curettes A and B vs. Curette C, but all data evaluation was performed by a blinded, pre-standardized investigator (CW for instrumentation techniques and tactile feedback, PWS for sEMG, fatigue, and comfort).
2.8. Statistical Analysis
Standard SPSS 19 statistics software (IBM®, Armonk, NY, USA) was used to perform data analysis by means of a General Linear Model (GLIM) with pairwise tests for differences between instruments, followed by Tukey’s post hoc test. The level of significance was set at p < 0.05.
3. Results
The eight hygienists who were enrolled in this study as curette testers were all female and ranged in age from 24–68 years (mean age 36.1 years, median age 35). All testers completed the study in full compliance with the protocol.
3.1. Video Analysis of Curette Grasp and Adaptation (Table 2 and Table 3)
Testers using Curette A performed significantly better than using Curette B in all categories (p < 0.05), with less finger flexing to initiate a stroke, hyperflexion of the thumb and index finger, and separation of the middle and index finger during instrumentation (Table 2). Curette C performed similarly better (p < 0.05) than Curette B during instrumentation, except that it was not superior in the “hyperflexion category”.


Table 2.
Effect of curette design on clinician’s grasp of the instrument.
Table 2.
Effect of curette design on clinician’s grasp of the instrument.
| Mean % (S.D.) of 8 Scaling Locations in Which Correct Grasp Position was Achieved for Each Curette | |||
|---|---|---|---|
| Criterion | Curette A | Curette B | Curette C |
| Index finger and thumb pads remained opposed | 100 (15) | 80 (12) | 100 (10) |
| Correct middle finger placement | 100 (18) | 80 (14) | 100 (15) |
| Hyperextension of index finger or thumb avoided | 60 (9) | 40 (5) | 40 (5) |
| Correct ring finger position | 100 (10) | 80 (8) | 100 (10) |
Significantly better (p < 0.05) blade positioning—with the terminal shank generally parallel to the long axis of the tooth—was achieved using Curette A vs. Curettes B and C. Moreover, clinicians were able to adapt the blade optimally to the tooth surface with a correct angle of 70° twice as often using Curette A vs. Curettes B and C (Table 3).


Table 3.
Evaluation of curette blade position during instrumentation.
Table 3.
Evaluation of curette blade position during instrumentation.
| Mean (S.D.) % of 8 Locations in Which Correct Blade Position was Achieved | |||
|---|---|---|---|
| Criterion | Curette A | Curette B | Curette C |
| Terminal shank parallel to long axis of tooth | 60 (8) | 40 (5) | 40 (5) |
| Blade maintained at a 60–80-degree angle to tooth | 80 (10) | 40 (5) | 40 (5) |
3.2. Comfort, Fatigue, and Tactile Feedback (Figure 3, Table 4)
Adaptive Curette A performed significantly better than Curette B (p < 0.05) in all categories, with hygienists reporting better comfort in the hand, wrist, and fingers, as well as less overall fatigue when using the prototype adaptive Curette A vs. the rigid stainless-steel Curette C. Curette A was rated as significantly more comfortable (p < 0.05) than Curette C for the fingers and the palm. Curette C performed significantly better (p < 0.05) than Curette B with regard to comfort in the fingers. All clinicians reported no notable differences in tactile sensitivity between curettes (p > 0.05).
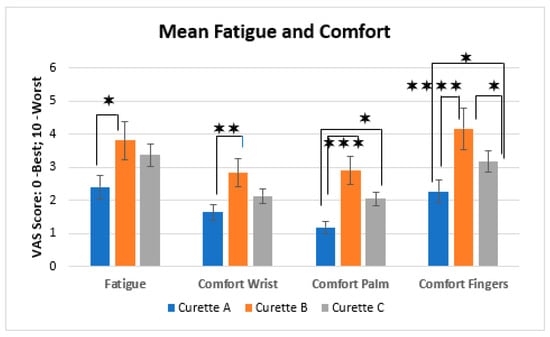

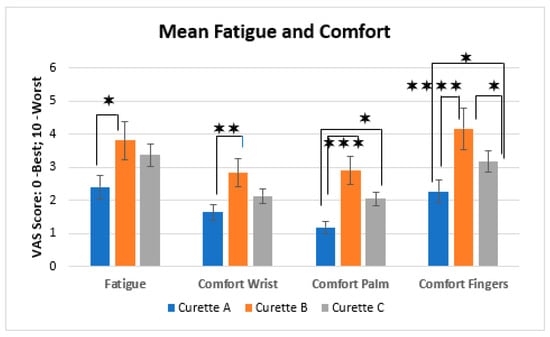
Figure 3.
Mean comfort and fatigue scores (S.D.) for each curette. Lines indicate statistically significant differences (p < 0.05), with **** indicating p < 0.0001, *** indicating p < 0.0005, ** indicating p < 0.01, and * indicating p < 0.05.

Table 4.
Statistical analysis of the data.
Table 4.
Statistical analysis of the data.
| Mean Diff. | 95% C.I. | p−Value | |
|---|---|---|---|
| APB Work A v B | −19.11 | −20.61 to −17.60 | <0.0001 |
| APB Work A v C | −4.108 | −5.617 to −2.600 | <0.0001 |
| APB Work B v C | 15 | 13.49 to 16.51 | <0.0001 |
| FDI Work A v B | −10.42 | −12.35 to −8.491 | <0.0001 |
| FDI Work A v C | −5.49 | −7.419 to −3.561 | <0.0001 |
| FDI Work B v C | 4.93 | 3.001 to 6.859 | <0.0001 |
| FPL Work A v B | −0.9183 | −1.380 to −0.4568 | <0.0001 |
| FPL Work A v C | −0.9183 | −1.380 to −0.4568 | <0.0001 |
| FPL Work B v C | 0 | −0.4615 to 0.4615 | >0.9999 |
| EDC Work A v B | −0.2908 | −0.9643 to 0.3826 | 0.5454 |
| EDC Work A v C | −1.798 | −2.472 to −1.125 | <0.0001 |
| EDC Work B v C | −1.508 | −2.181 to −0.8341 | <0.0001 |
| ALL MS Work A v B | −30.74 | −34.82 to −26.65 | <0.0001 |
| ALL MS Work A v C | −12.32 | −16.40 to −8.233 | <0.0001 |
| ALL MS Work B v C | 18.42 | 14.34 to 22.50 | <0.0001 |
| Comfort Wrist A v B | −1.25 | −2.197 to −0.3029 | 0.0075 |
| Comfort Wrist A v C | −0.8333 | −1.780 to 0.1138 | 0.0935 |
| Comfort Wrist B v C | 0.4167 | −0.5305 to 1.364 | 0.5333 |
| Comfort Palm A v B | −1.583 | −2.398 to −0.7685 | 0.0001 |
| Comfort Palm A v C | −0.9167 | −1.731 to −0.1018 | 0.0247 |
| Comfort Palm B v C | 0.6667 | −0.1482 to 1.481 | 0.1262 |
| Comfort Fingers A v B | −1.917 | −2.897 to −0.9366 | <0.0001 |
| Comfort Fingers A v C | −0.9167 | −1.897 to 0.06335 | 0.0705 |
| Comfort Fingers B v C | 1 | 0.01998 to 1.980 | 0.0447 |
| ∆Pinch Strength A v B | −59.98 | −81.64 to −38.33 | <0.0001 |
| ∆Pinch Strength A v C | −29.09 | −50.75 to −7.435 | 0.0065 |
| ∆Pinch Strength B v C | 30.89 | 9.232 to 52.55 | 0.0038 |
| ∆Grasp Strength A v B | −74.37 | −98.52 to −50.22 | <0.0001 |
| ∆Grasp Strength A v C | −56.63 | −80.78 to −32.48 | <0.0001 |
| ∆Grasp Strength B v C | 17.73 | −6.418 to 41.88 | 0.0185 |
| Fatigue A v B | −1.167 | −2.142 to −0.1918 | 0.0161 |
| Fatigue Palm A v C | −0.75 | −1.725 to 0.2248 | 0.1581 |
| Fatigue Palm B v C | 0.4167 | −0.5582 to 1.392 | 0.5520 |
3.3. Pinch and Grasp Strengths (Figure 4, Table 4)
Pre-scaling pinch and grasp strengths did not differ significantly between the three instrument types (p > 0.05). Pinch strength was significantly reduced after instrumentation for Curette B (p < 0.05) but not for Curettes A and C. Grasp strength was significantly reduced for Curettes B and C (p < 0.05) but not for Curette A.
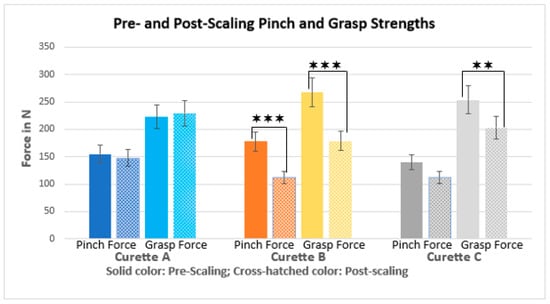
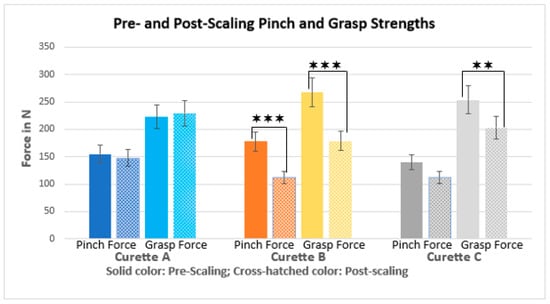
Figure 4.
Mean pre- and post-scaling pinch and grasp strength (S.D.) for each curette. Lines indicate statistically significant differences (p < 0.05), with *** indicating p < 0.0005, and ** indicating p < 0.01.
3.4. Surface EMG Data (Figure 5, Table 4)
Testers performed significantly (p < 0.05) less total work in all muscles combined and in each individual muscle when using Curette A vs. Curettes B and C, except in the EDC. In this muscle, the total work did not differ significantly between Curettes A and B, but it was significantly greater for Curette C. Moreover, testers using Curette C performed significantly (p < 0.05) less work than using Curette B in APB, FDI, and all muscles combined.
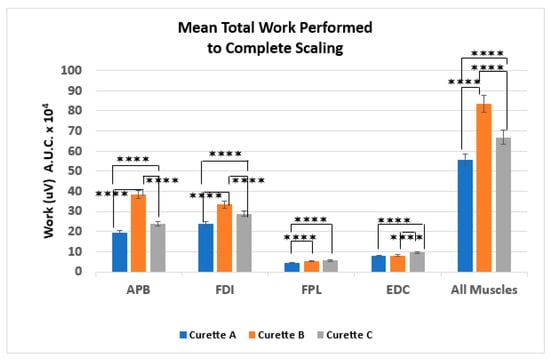
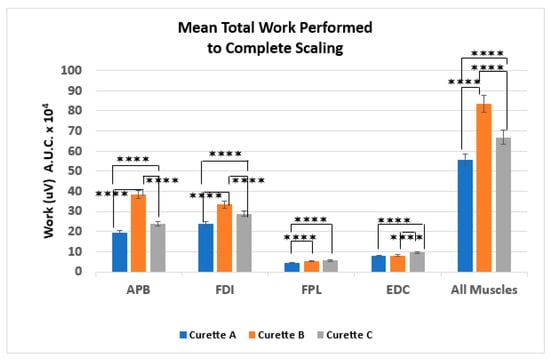
Figure 5.
Mean total work (S.D.) performed, by muscle, to complete scaling. APB—Abductor Pollicis Brevis; FDI—First Dorsal Interosseous; FPL—Flexor Pollicis Longus; EDC—Extensor Digitorum Communis (EDC). Lines indicate statistically significant differences (p < 0.05), with **** indicating p < 0.0001.
3.5. Tester Requests and Comments
After watching the instructional video on the use of adaptive Curette A, one hygienist requested an additional 5 min before the study began to accustom herself to Curette A. In their comments, testers stated that it was easier to reach areas of the mouth that are difficult to access using conventional rigid design. Seven of the eight testers stated that they did not have to grip the adaptive instrument as tightly as the conventional curettes during instrumentation. One of these testers commented that it would take some time to become used to the new design, despite it feeling more comfortable. All testers agreed that the benefits were immediately notable with the adaptive curette in the premolar and anterior zones. Three of the eight testers did not feel the need to adapt the curette when working on the molars and preferred to use it straight. The actual comments are cited in Table 5.

Table 5.
Testers’ free comments.
4. Discussion
The goal of this study was to investigate the muscle work, fatigue, and comfort related to a standardized scaling by three different curettes of a full set of teeth mounted in a dental typodont model. While many studies have been published on ergonomic hand tool design, with variables including features to improve pressure distribution by spreading instrumentation weight and forces over larger surface areas and additional anatomical structures beyond the fingers and thumb [50,56,57,58,59,60,61] and increasing the area of contact between the hand and fingers and the tool handle [6,56,57,58,59,60,61], far fewer studies have specifically targeted dental instrument design. Typically, the variables investigated related to dental instrument design have been limited to the weight, diameter, and handle materials or surface covering [35,36,37,38,39,40,41]. A recent paper, for the first time, reported on the performance of a periodontal curette with an adaptive handle design vs. a standard stainless-steel curette with regard to muscle work, fatigue, comfort, and user acceptance [48]. This second paper continues this conversation by first evaluating the ergonomic performance of a newer—though still rigid—curette with a silicone-covered handle vs. that of a curette with a conventional stainless-steel design. This comparison serves to examine the level of ergonomic improvement afforded by the newer, fatter silicone handles vs. the conventional metal grips. Additionally, this second study evaluates the ergonomic performance of a prototype adaptive (adjustabale) curette featuring a silicone-covered handle, comparing it with that of a conventional curette with a rigid silicone-covered handle. Because these two curettes feature almost exactly the same dimensions, weight, shape, diameter, and handle covering material, this second study for the first time allows an evaluation of the effect of the adaptive component alone, by using instruments with comparable handle covering material, diameter, shape, and weight.
Previous studies evaluating the ergonomics of hand tools typically included neurophysiological measurements of work in the specific muscles that are directly involved in the activity under investigation, as well as dynamometer force measurements and more subjective measures such as semi-quantitative VAS markers of fatigue or comfort. These studies found that both objective and subjective measurements are needed for meaningful design evaluation [56,62,63]. In this study, there was excellent overall agreement between the various evaluation tools that were used. Using VAS scales, hygienists predominantly reported better comfort and less overall fatigue associated with the prototype adaptive Curette A vs. the rigid Curettes B and C. Moreover, Curette C, which features a silicone-covered, larger-diameter handle than Curette B, performed better than Curette B in all evaluations of comfort and fatigue, although the difference achieved significance only with regard to comfort in the fingers. Corresponding sEMG data showed considerable congruence with the semi-quantitative VAS data and the hygienist’s comments: testers performed significantly less work in all muscles combined and in most individual muscles using Curette A than using Curettes B and C. Indeed, testers’ better VAS ratings for clinical comfort and fatigue using Curette C vs. Curette B were mirrored in the sEMG measurements, showing reduced work in all muscles combined and in APB and FDI. These results are in agreement with those of previous studies linking non-metal instrument handle coverings and larger handle diameters such as those of Curettes A and C with more favorable ergonomic performance [6,38,42,64,65,66]. Moreover, they echo the findings of a recent study, which reported the better ergonomic performance of the prototype adaptive instrument vs. a narrower diameter, rigid, conventional stainless-steel instrument [48]. That initial study only compared the ergonomic performance of the larger diameter, silicone-overlaid adaptive curette with that of a narrower stainless-steel tool, raising the question of to what extent the prototype’s better performance should be attributed to its diameter, shape, and material and/or the novel adaptive design. In order to address these potential variables, the current study used instruments with almost or completely identical curette weights, lengths, handle lengths, and blades. The curette diameter at the pen grip was almost identical for the two silicon-overlaid instruments, but the diameter of the stainless-steel instrument was more than 3 mm narrower, conforming with the usual parameters of stainless-steel curettes.
The finding that grasp strength after instrumentation was reduced significantly for Curettes B and C but not for Curette A seems reasonable given the smaller amount of muscle work used during instrumentation with Curette A. A similar trend, although not always at a significant level, was observed for the post-instrumentation grip strength.
While this study confirmed the findings of previous studies, it goes beyond their scope by introducing a novel prototype instrument that replaces the conventional rigid design with an adaptive handle design and also incorporating the known parameters for optimal ergonomic performance in dental hand instruments. Moreover, the adaptive prototype also incorporates some design features that have been shown to improve the ergonomic performance of other hand tools. For example, maximizing the area of contact between a tool and the hand and fingers supports an efficient transfer of forces between the operator and the instrument [6,50,56]. Furthermore, distributing instrumentation forces over a larger surface area is functionally and ergonomically advantageous [50,56,67]. Both of these design features are incorporated into Curette A, whose adaptive design allows the instrument to adapt more closely and over a larger surface area of the fingers and the hand than is possible with rigid linear instruments. Additionally, by spreading instrumentation weight and forces over a wider area of the index finger and the back of the hand, the adaptive feature reduces loading per unit of area, lowering the stress on the fingers and the hand during instrumentation. These features most likely contributed to the less work per time and reduced total work required to complete the scaling task as well as the decreased fatigue and improved comfort reported to be associated with the use of Curette A.
In summary, a novel adaptive design for dental curettes, which integrates state-of-the-art knowledge from a wide range of disciplines, may improve the ergonomic and clinical performance of this instrument. Additional, more extensive clinical studies with expanded investigational scope are under way. With greater sample sizes and study durations, they will further elucidate the effect of the adaptive handle design on instrumentation efficacy and speed as well as hand, wrist, and body positioning during instrumentation. Future investigations will also include comparisons with ultrasonic devices. Moreover, the potential of the adaptive design as a teaching tool to support correct instrumentation habits needs to be explored.
5. Practical Implication and Conclusions
Potential benefits of a novel adaptive handle design for dental hand instruments may include improved comfort, less muscle work, and reduced fatigue related to periodontal scaling. Extensive studies are now underway to solidify these initial findings and to develop a better understanding of novel design features to support musculoskeletal health in dental clinicians and others engaging in repetitive work with hand tools.
Author Contributions
Conceptualization, B.E.D. and P.W.-S.; Formal analysis, K.O. and A.A.H.; Investigation, C.W., K.L. and P.W.-S.; Methodology, C.W., B.E.D., K.O., A.A.H. and P.W.-S.; Project administration, P.W.-S.; Resources, P.W.-S.; Software, P.W.-S.; Supervision, C.W. and P.W.-S.; Validation, A.A.H. and P.W.-S.; Visualization, P.W.-S.; Writing—original draft, K.O. and P.W.-S.; Writing—review and editing, C.W., B.E.D., K.O. and A.A.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
After a review by the University of California, Irvine’s IRB, this protocol was granted exempt status, as only de-identified data were collected and used in this study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request due to restrictions. The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- McCall, J.O. The Historical Background of Periodontology. The Evolution of the Scaler and Its Influence on the Development of Periodontia. J. Periodontol. 1939, 10, 69–81. [Google Scholar] [CrossRef]
- Sabatini, S.; Maiorani, C.; Bassignani, J.; Cotellessa, S.; Di Trani, G.; Fulgenzi, E.; Iacono, R.; Mercogliano, I.; Butera, A. Effectiveness of Ultrasonic and Manual Instrumentation in Nonsurgical Periodontal Therapy: Are Additional Therapies More Effective? A Systematic Review. Appl. Sci. 2024, 14, 1950. [Google Scholar] [CrossRef]
- De Sio, S.; Traversini, V.; Rinaldo, F.; Colasanti, V.; Buomprisco, G.; Perri, R.; Mormone, F.; La Torre, G.; Guerra, F. Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: An umbrella review. PeerJ 2018, 6, e4154. [Google Scholar] [CrossRef] [PubMed]
- Saccucci, M.; Zumbo, G.; Mercuri, P.; Pranno, N.; Sotero, S.; Zara, F.; Vozza, I. Musculoskeletal disorders related to dental hygienist profession. Int. J. Dent. Hyg. 2022, 20, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Leigh, J.P.; Miller, T.R. Occupational illnesses within two national data sets. Int. J. Occup. Environ. Health 1998, 4, 99–113. [Google Scholar] [CrossRef] [PubMed]
- Suedbeck, J.R.; Tolle, S.L.; McCombs, G.; Walker, M.L.; Russell, D. Effects of Instrument Handle Design on Dental Hygienists’ Forearm Muscle Activity during Scaling. J. Dent. Hyg. 2017, 91, 47–54. [Google Scholar] [PubMed]
- Humann, P.; Rowe, D.J. Relationship of Musculoskeletal Disorder Pain to Patterns of Clinical Care in California Dental Hygienists. J. Dent. Hyg. 2015, 89, 305–312. [Google Scholar] [PubMed]
- Macdonald, G.; Robertson, M.M.; Erickson, J.A. Carpal tunnel syndrome among California dental hygienists. Dent. Hyg. 1988, 62, 322–327. [Google Scholar]
- Liss, G.M.; Jesin, E.; Kusiak, R.A.; White, P. Musculoskeletal problems among Ontario dental hygienists. Am. J. Ind. Med. 1995, 28, 521–540. [Google Scholar] [CrossRef] [PubMed]
- Lalumandier, J.A.; McPhee, S.D.; Riddle, S.; Shulman, J.D.; Daigle, W.W. Carpal tunnel syndrome: Effect on Army dental personnel. Mil. Med. 2000, 165, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Lalumandier, J.A.; McPhee, S.D. Prevalence and risk factors of hand problems and carpal tunnel syndrome among dental hygienists. J. Dent. Hyg. 2001, 75, 130–134. [Google Scholar] [PubMed]
- Osborn, J.B.; Newal, K.J.; Rudney, J.D.; Stoltenberg, J.L. Carpal tunnel syndrome among Minnesota dental hygienists. J. Dent. Hyg. 1990, 64, 79–85. [Google Scholar] [PubMed]
- Anton, D.; Rosecrance, J.; Merlino, L.; Cook, T. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am. J. Ind. Med. 2002, 42, 248–257. [Google Scholar] [CrossRef]
- Marshall, E.D.; Duncombe, L.M.; Robinson, R.Q.; Kilbreath, S.L. Musculoskeletal symptoms in New South Wales dentists. Aust. Dent. J. 1997, 42, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Milerad, E.; Ekenvall, L. Symptoms of the neck and upper extremities in dentists. Scand. J. Work Environ. Health 1990, 16, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Osborn, J.B.; Newal, K.J.; Rudney, J.D.; Stoltenberg, J.L. Musculoskeletal pain among Minnesota dental hygienists. J. Dent. Hyg. 1990, 64, 132–138. [Google Scholar] [PubMed]
- Rundcrantz, B.L. Pain and discomfort in the musculoskeletal system among dentists. Swed. Dent. J. 1991, 76, 1–102. [Google Scholar] [CrossRef]
- Oberg, T.; Oberg, U. Musculoskeletal complaints in dental hygiene: A survey study from a Swedish county. J. Dent. Hyg. 1993, 67, 257–261. [Google Scholar] [PubMed]
- Corks, I. Occupational health hazards in dentistry: Musculoskeletal disorders. Ont. Dent. 1997, 74, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Fish, D.R.; Morris-Allen, D.M. Musculoskeletal disorders in dentists. NY State Dent. J. 1998, 64, 44–48. [Google Scholar]
- Finsen, L.; Christensen, H.; Bakke, M. Musculoskeletal disorders among dentists and variation in dental work. Appl. Ergon. 1998, 29, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Akesson, I.; Johnsson, B.; Rylander, L.; Moritz, U.; Skerfving, S. Musculoskeletal disorders among female dental personnel: Clinical examination and a 5-year follow-up study of symptoms. Int. Arch. Occup. Environ. Health 1999, 72, 395–403. [Google Scholar] [CrossRef]
- Akesson, I.; Schutz, A.; Horstmann, V.; Skerfving, S.; Moritz, U. Musculoskeletal symptoms among dental personnel; Lack of association with mercury and selenium status, overweight and smoking. Swed. Dental. J. 2000, 24, 23–38. [Google Scholar]
- Alexopoulos, E.C.; Stathi, I.; Charizani, F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet. Disord. 2004, 5, 16. [Google Scholar] [CrossRef] [PubMed]
- Auguston, T.E.; Morken, T. Musculoskeletal problems among dental health personnel. A survey of the public dental health services in Hordaland. Tdsskr. Nor. Laegeforen. 1996, 116, 2776–2780. [Google Scholar]
- Chowanadisai, S.; Kukiattrakoon, B.; Yapong, B.; Kedjarune, U.; A Leggat, P. Occupational health problems of dentists in southern Thailand. Int. Dent. J. 2000, 50, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Lehto, T.U.; Helenius, H.Y.; Alaranta, H.T. Musculoskeletal symptoms of dentists assessed by a multidisciplinary approach. Community. Dent. Oral Epidemiol. 1991, 19, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Ratzon, N.Z.; Yaros, T.; Mizlik, A.; Kanner, T. Musculoskeletal symptoms among dentists in relation to work posture. Work 2000, 15, 153–158. [Google Scholar] [PubMed]
- Rundcrantz, B.; Johnsson, B.; Moritz, U. Cervical pain and discomfort among dentists. Epidemiological, clinical and therapeutic aspects. Swed. Dent. J. 1990, 14, 71–80. [Google Scholar] [PubMed]
- Rundcrantz, B.; Johnsson, B.; Moritz, U. Occupational cervico-brachial disorders among dentists: Analysis of ergonomics and locomotor functions. Swed. Dent. J. 1991, 15, 105–115. [Google Scholar] [PubMed]
- Shugars, D.A.; Miller, D.; Williams, D.; Fishburne, C.; Strickland, D. Musculoskeletal pain among general dentists. Gen. Dent. 1987, 35, 272–276. [Google Scholar] [PubMed]
- Kumar, M.; Pai, K.M.; Vineetha, R. Occupation-related musculoskeletal disorders among dental professionals. Med. Pharm. Rep. 2020, 93, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Marklund, S.; Mienna, C.S.; Wahlström, J.; Englund, E.; Wiesinger, B. Work ability and productivity among dentists: Associations with musculoskeletal pain, stress, and sleep. Int. Arch. Occup. Environ. Health 2020, 93, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Voruganti, K. Practice Dentistry Pain-free: Evidence-based Strategies to Prevent Pain and Extend Your Career. Br. Dent. J. 2009, 206, 181. [Google Scholar] [CrossRef][Green Version]
- Åkesson, I.; Balogh, I.; Hansson, G.Å. Physical workload in neck, shoulders and wrists/hands in dental hygienists during a work-day. Appl. Ergon. 2012, 43, 803–811. [Google Scholar] [CrossRef]
- Åkesson, I.; Hansson, G.A.; Balogh, I.; Moritz, U.; Skerfving, S. Quantifying work load in neck, shoulders and wrists in female dentists. Int. Arch. Occup. Environ. Health 1997, 69, 461–474. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Barr, A.; Loomer, P.; Rempel, D. The effects of finger rest positions on hand muscle load and pinch force in simulated dental hygiene work. J. Dent. Educ. 2005, 69, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Loomer, P.; Barr, A.; Barr, A.; LaRoche, C.; Young, E.; Rempel, D. The effect of tool handle shape on hand muscle load and pinch force in a simulated dental scaling task. Appl. Ergon. 2007, 38, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Jonker, D.; Rolander, B.; Balogh, I. Relation between perceived and measured workload obtained by long-term inclinometry among dentists. Appl. Ergon. 2009, 40, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Finsen, L. Biomechanical aspects of occupational neck postures during dental work. Int. J. Ind. Ergon. 1999, 23, 397–406. [Google Scholar] [CrossRef]
- Hagberg, M. Exposure variables in ergonomic epidemiology. Am. J. Ind. Med. 1992, 21, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Barr, A.; Loomer, P.; LaRoche, C.; Young, E.; Rempel, D. The effects of periodontal instrument handle design on hand muscle load and pinch force. J. Am. Dent. Assoc. 2006, 137, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- McCombs, G.; Russell, D.M. Comparison of Corded and Cordless Handpieces on Forearm Muscle Activity, Procedure Time and Ease of Use during Simulated Tooth Polishing. J. Dent. Hyg. 2014, 88, 386–393. [Google Scholar] [PubMed]
- Delfa, N.L.; Grondin, D.E.; Cox, J.; Potvin, J.R.; Howarth, S.J. The biomechanical demands of manual scaling on the shoulders & neck of dental hygienists. Ergonomics 2016, 60, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Enders, L.R.; Seo, N.J. Phalanx force magnitude and trajectory deviation increased during power grip with an increased coefficient of friction at the hand-object interface. J. Biomech. 2011, 44, 1447–1453. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, E.M. Instruments and Principles for Instrumentation. In Clinical Practice of Dental Hygienist, 8th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1999; pp. 99–111. [Google Scholar]
- Zappa, U.; Röthlisberger, J.P.; Simona, C.; Case, D. In vivo scaling and root planning forces in molars. J. Periodontol. 1993, 64, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.; Wink, C.; Dolan, B.; Osann, K.; Habib, A.A.; Gehrig, J.; Wilder-Smith, P. A Novel Ergonomic Curette Design Reduces Dental Prophylaxis-Induced Muscle Work and Fatigue. Dent. J. 2023, 11, 272. [Google Scholar] [CrossRef] [PubMed]
- Gehrig, J.S.; Sroda, R.; Saccuzzo, D. Ergonomic Risk Factors Associated with Periodontal Instrumentation. In Fundamentals of Periodontal Instrumentation & Advanced Root Instrumentation, 8th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2017; pp. 3–37. [Google Scholar]
- Das, D. Ergonomic evaluation, design and testing of hand tools. In Assessment of the Ergonomic Quality of Hand-Held Tools and Computer Input Devices, 1st ed.; Strasser, H., Ed.; IOS Press: Lancaster, UK, 2007; pp. 23–39. [Google Scholar]
- Smith, C.A.; Sommerich, C.M.; Mirka, G.A.; George, M.C. An investigation of ergonomic interventions in dental hygiene work. Appl. Ergon. 2002, 33, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Jarvik, J.G.; Yuen, E.; Kliot, M. Diagnosis of carpal tunnel syndrome: Electrodiagnostic and MR imaging evaluation. Neuroimag. Clin. N. Am. 2004, 14, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Burden, A.; Bartlett, R. Normalisation of EMG amplitude: An evaluation and comparison of old and new methods. Med. Eng. Phys. 1999, 21, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Bolga, L.A.; Uhl, T.L. Reliability of electromyographic normalization methods for evaluating the HIP musculature. J. Electromyogr. Kinesiol. 2007, 17, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Netto, K.J.; Burnett, A.F. Reliability of normalization methods for EMG analysis of neck muscles. Work 2006, 26, 123–130. [Google Scholar] [PubMed]
- Dianat, I.; Nedaei, M.; Nezami, M. The effects of tool handle shape on hand performance, usability and discomfort using masons’ trowels. Int. J. Ind. Ergon. 2015, 45, 13–20. [Google Scholar] [CrossRef]
- Aldien, Y.; Welcome, D.; Rakheja, S.; Dong, R.; Boileau, P.-E. Contact pressure distribution at hand–handle interface: Role of hand forces and handle size. Int. J. Ind. Ergon. 2005, 35, 267–286. [Google Scholar] [CrossRef]
- Fellows, G.L.; Freivalds, A. Ergonomics evaluation of a foam rubber grip for tool handles. Appl. Ergon. 1991, 22, 225–230. [Google Scholar] [CrossRef] [PubMed]
- A Freivalds. Tool evaluation and design. In Occupational Ergonomics: Theory and Applications, 2nd ed.; Bhattacharya, A., McGlothlin, J.D., Eds.; Marcel Dekker Inc.: New York, NY, USA, 1996; pp. 303–327. [Google Scholar]
- Harih, G.; Dolšak, B. Comparison of subjective comfort ratings between anatomically shaped and cylindrical handles. Appl. Ergon. 2014, 45, 943–954. [Google Scholar] [CrossRef] [PubMed]
- Harih, G.; Dolšak, B. Tool-handle design based on a digital human hand model. Int. J. Ind. Ergon. 2013, 43, 288–295. [Google Scholar] [CrossRef]
- Strasser, H.; Wang, B.; Hoffmann, A. Electromyographic and subjective evaluation of hand tools: The example of masons’ trowels. Int. J. Ind. Ergon. 1996, 18, 91–106. [Google Scholar] [CrossRef]
- Kuijt-Evers, L.; Bosch, T.; Huysmans, M.A. Association between objective and subjective measurements of comfort and discomfort in hand tools. Appl. Ergon. 2007, 38, 643–654. [Google Scholar] [CrossRef] [PubMed]
- Simmer-Beck, M.; Branson, B.G. An evidence-based review of ergonomic features of dental hygiene instruments. Work 2010, 35, 477–485. [Google Scholar] [CrossRef]
- Nevala, N. Evaluation of Ergonomics and Efficacy of Instruments in Dentistry. Ergon. Open J. 2013, 6, 6–12. [Google Scholar] [CrossRef][Green Version]
- Rempel, D.; Lee, D.L.; Dawson, K.; Loomer, P. The effects of periodontal curette handle weight and diameter on arm pain: A four-month randomized controlled trial. J. Am. Dent. Assoc. 2012, 143, 1105–1113. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Cai, D. Hand tool handle design based on hand measurements. MATEC Web Conf. 2016, 119, 01044. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).