Evaluation of Social-Cognitive Determinants of Patients’ Hand Hygiene Decisions and the Role of Mental Health in a Cross-Sectional and a Longitudinal Study of German Patients
Abstract
1. Introduction
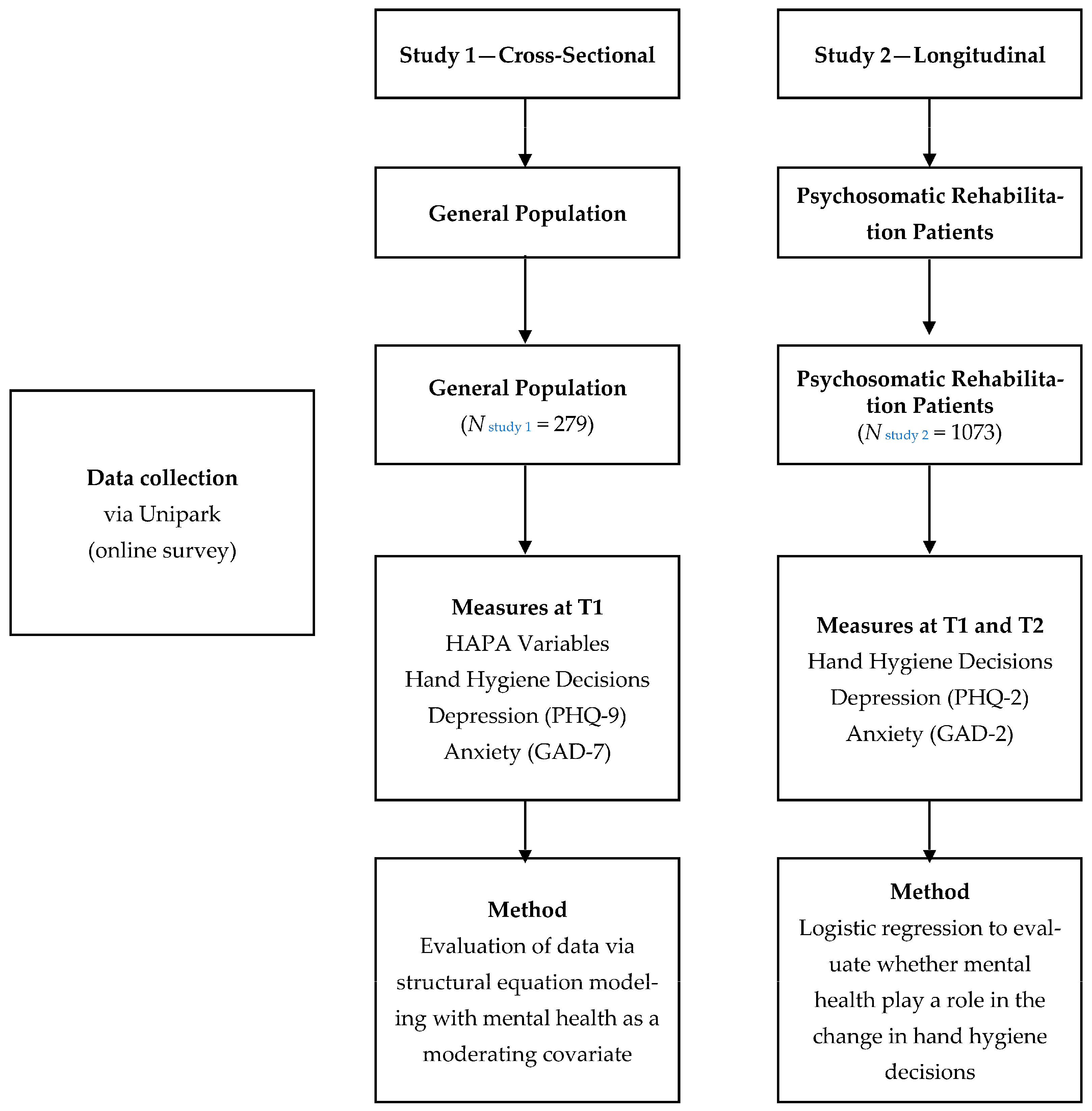
2. Materials and Methods
2.1. Study 1: Cross-Sectional Study
2.1.1. Procedure and Participants
2.1.2. Measures
Socio-Demographic Information
Hand Hygiene Decisions and HAPA Constructs
Mental Health Status
2.1.3. Data Analysis
2.1.4. Missing Data
2.2. Study 2: Longitudinal Study
2.2.1. Procedure and Participants: Longitudinal Study
2.2.2. Measures
Changes in Hand Hygiene Decisions
Mental Health Symptoms
2.2.3. Data Analysis
3. Results
3.1. Study 1
3.1.1. Scale Internal Consistency and Correlations between Constructs
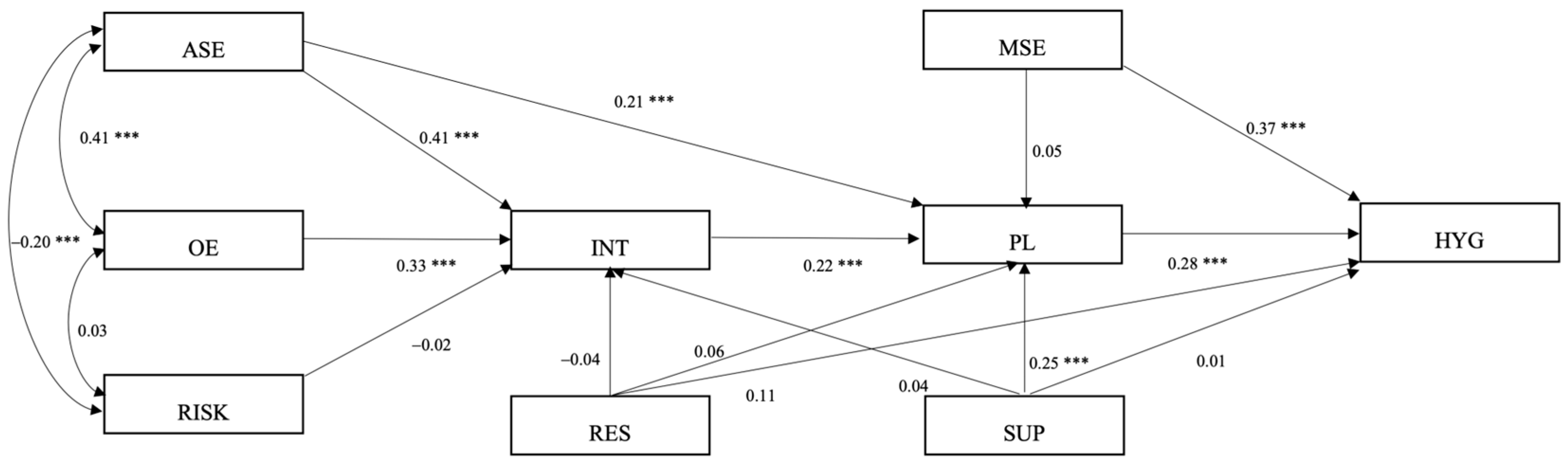
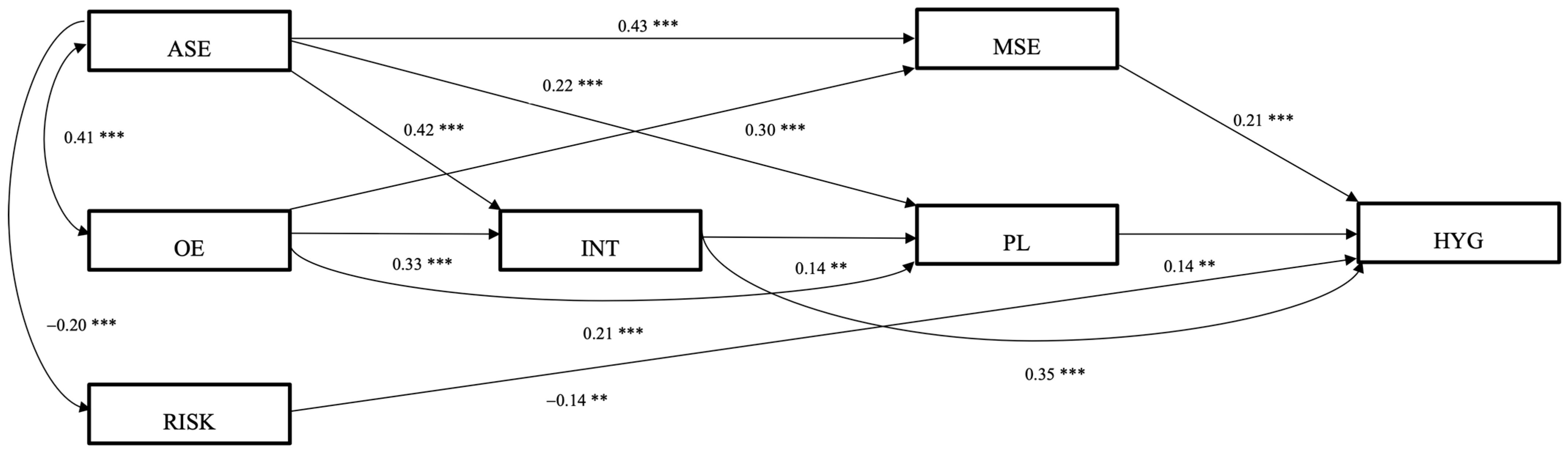
3.1.2. Structural Equation Modeling
3.1.3. Latent Mean Differences across Mental Health Status
3.2. Study 2
Changes in Compliance and Its Predictors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Difference between Participants from the Three Measurement Waves
Appendix B. Differences in Variables with Regard to Time of Hospital Visit
References
- Gaube, S.; Fischer, P.; Lermer, E. Hand(y) Hygiene Insights: Applying Three Theoretical Models to Investigate Hospital Patients’ and Visitors’ Hand Hygiene Behavior. PLoS ONE 2021, 16, e0245543. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahman, M. Personality Traits, Risk Perception, and Protective Behaviors of Arab Residents of Qatar during the COVID-19 Pandemic. Int. J. Ment. Health Addict. 2022, 20, 237–248. [Google Scholar] [CrossRef]
- Sickbert-Bennett, E.E.; DiBiase, L.M.; Willis, T.M.S.; Wolak, E.S.; Weber, D.J.; Rutala, W.A. Reduction of Healthcare-Associated Infections by Exceeding High Compliance with Hand Hygiene Practices. Emerg. Infect. Dis. 2016, 22, 1628–1630. [Google Scholar] [CrossRef] [PubMed]
- Stilo, A.; Troiano, G.; Melcarne, L.; Gioffrè, M.E.; Nante, N.; Messina, G.; Laganà, P. Hand Washing in Operating Room: A Procedural Comparison. Epidemiol. Biostat. Public Health 2016, 13, e12075. [Google Scholar] [CrossRef] [PubMed]
- Juneau, C.-E.; Pueyo, T.; Bell, M.; Gee, G.; Collazzo, P.; Potvin, L. Lessons from Past Pandemics: A Systematic Review of Evidence-Based, Cost-Effective Interventions to Suppress COVID-19. Syst. Rev. 2022, 11, 90. [Google Scholar] [CrossRef]
- Lotfinejad, N.; Peters, A.; Pittet, D. Hand Hygiene and the Novel Coronavirus Pandemic: The Role of Healthcare Workers. J. Hosp. Infect. 2020, 105, 776–777. [Google Scholar] [CrossRef] [PubMed]
- Bellissimo-Rodrigues, F.; Pires, D.; Zingg, W.; Pittet, D. Role of Parents in the Promotion of Hand Hygiene in the Paediatric Setting: A Systematic Literature Review. J. Hosp. Infect. 2016, 93, 159–163. [Google Scholar] [CrossRef]
- Sande-Meijide, M.; Lorenzo-González, M.; Mori-Gamarra, F.; Cortés-Gago, I.; González-Vázquez, A.; Moure-Rodríguez, L.; Herranz-Urbasos, M. Perceptions and Attitudes of Patients and Health Care Workers toward Patient Empowerment in Promoting Hand Hygiene. Am. J. Infect. Control 2019, 47, 45–50. [Google Scholar] [CrossRef]
- Scheithauer, S.; Lemmen, S.W. How Can Compliance with Hand Hygiene Be Improved in Specialized Areas of a University Hospital? J. Hosp. Infect. 2013, 83 (Suppl. S1), S17–S22. [Google Scholar] [CrossRef]
- Jabbari, P.; Taraghikhah, N.; Jabbari, F.; Ebrahimi, S.; Rezaei, N. Adherence of the General Public to Self-Protection Guidelines During the COVID-19 Pandemic. Disaster Med. Public Health Prep. 2022, 16, 871–874. [Google Scholar] [CrossRef]
- Schwarzer, R.; Luszczynska, A. How to Overcome Health-Compromising Behaviors: The Health Action Process Approach. Eur. Psychol. 2008, 13, 141–151. [Google Scholar] [CrossRef]
- Kwasnicka, D.; Dombrowski, S.U.; White, M.; Sniehotta, F. Theoretical Explanations for Maintenance of Behaviour Change: A Systematic Review of Behaviour Theories. Health Psychol. Rev. 2016, 10, 277–296. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, K.; Smith, S.R.; Keech, J.J.; Moyers, S.A.; Hagger, M.S. Application of the Health Action Process Approach to Social Distancing Behavior During COVID-19. Appl. Psychol. Health Well-Being 2020, 12, 1244–1269. [Google Scholar] [CrossRef] [PubMed]
- Sheeran, P.; Klein, W.M.P.; Rothman, A.J. Health Behavior Change: Moving from Observation to Intervention. Annu. Rev. Psychol. 2017, 68, 573–600. [Google Scholar] [CrossRef]
- Hashemzadeh, M.; Rahimi, A.; Zare-Farashbandi, F.; Alavi-Naeini, A.M.; Daei, A. Transtheoretical Model of Health Behavioral Change: A Systematic Review. Iran. J. Nurs. Midwifery Res. 2019, 24, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Lippke, S.; Luszczynska, A. Mechanisms of Health Behavior Change in Persons with Chronic Illness or Disability: The Health Action Process Approach (HAPA). Rehabil. Psychol. 2011, 56, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Lao, C.K.; Li, X.; Zhao, N.; Gou, M.; Zhou, G. Using the Health Action Process Approach to Predict Facemask Use and Hand Washing in the Early Stages of the COVID-19 Pandemic in China. Curr. Psychol. 2023, 42, 6484–6493. [Google Scholar] [CrossRef]
- Liang, W.; Duan, Y.; Li, F.; Rhodes, R.E.; Wang, X.; Peiris, D.L.I.H.K.; Zhou, L.; Shang, B.; Yang, Y.; Baker, J.S.; et al. Psychosocial Determinants of Hand Hygiene, Facemask Wearing, and Physical Distancing During the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Ann. Behav. Med. Publ. Soc. Behav. Med. 2022, 56, 1174–1187. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet Lond. Engl. 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Lee, S.A. Coronavirus Anxiety Scale: A Brief Mental Health Screener for COVID-19 Related Anxiety. Death Stud. 2020, 44, 393–401. [Google Scholar] [CrossRef]
- Cawcutt, K.A.; Starlin, R.; Rupp, M.E. Fighting Fear in Healthcare Workers during the COVID-19 Pandemic. Infect. Control Hosp. Epidemiol. 2020, 41, 1192–1193. [Google Scholar] [CrossRef] [PubMed]
- Ejeh, F.E.; Owoicho, S.; Saleh, A.S.; Madukaji, L.; Okon, K.O. Factors Associated with Preventive Behaviors, Anxiety among Healthcare Workers and Response Preparedness against COVID-19 Outbreak: A One Health Approach. Clin. Epidemiol. Glob. Health 2021, 10, 100671. [Google Scholar] [CrossRef]
- Denollet, J.; Pedersen, S.S.; Daemen, J.; de Jaegere, P.; Serruys, P.W.; van Domburg, R.T. Reduced Positive Affect (Anhedonia) Predicts Major Clinical Events Following Implantation of Coronary-Artery Stents. J. Intern. Med. 2008, 263, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Kessing, D.; Pelle, A.J.; Kupper, N.; Szabó, B.M.; Denollet, J. Positive Affect, Anhedonia, and Compliance with Self-Care in Patients with Chronic Heart Failure. J. Psychosom. Res. 2014, 77, 296–301. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Leventhal, A.M. Relations Between Anhedonia and Physical Activity. Am. J. Health Behav. 2012, 36, 860–872. [Google Scholar] [CrossRef] [PubMed]
- Beeckman, M.; De Paepe, A.; Van Alboom, M.; Maes, S.; Wauters, A.; Baert, F.; Kissi, A.; Veirman, E.; Van Ryckeghem, D.M.L.; Poppe, L. Adherence to the Physical Distancing Measures during the COVID-19 Pandemic: A HAPA-Based Perspective. Appl. Psychol. Health Well-Being 2020, 12, 1224–1243. [Google Scholar] [CrossRef] [PubMed]
- Farholm, A.; Sørensen, M. Motivation for Physical Activity and Exercise in Severe Mental Illness: A Systematic Review of Cross-Sectional Studies. Int. J. Ment. Health Nurs. 2016, 25, 116–126. [Google Scholar] [CrossRef]
- Krämer, L.V.; Helmes, A.W.; Seelig, H.; Fuchs, R.; Bengel, J. Correlates of Reduced Exercise Behaviour in Depression: The Role of Motivational and Volitional Deficits. Psychol. Health 2014, 29, 1206–1225. [Google Scholar] [CrossRef]
- Lhakhang, P.; Lippke, S.; Knoll, N.; Schwarzer, R. Evaluating Brief Motivational and Self-Regulatory Hand Hygiene Interventions: A Cross-over Longitudinal Design. BMC Public Health 2015, 15, 79. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Gholami, M.; Schwarzer, R. Brief Scales for the Multilingual Assessment of HAPA Variables. Available online: https://www.psyc.de/hapascales.pdf (accessed on 10 January 2024).
- Caudroit, J.; Stephan, Y.; Le Scanff, C. Social Cognitive Determinants of Physical Activity among Retired Older Individuals: An Application of the Health Action Process Approach. Br. J. Health Psychol. 2011, 16, 404–417. [Google Scholar] [CrossRef]
- Chiu, C.-Y.; Lynch, R.T.; Chan, F.; Berven, N.L. The Health Action Process Approach as a Motivational Model for Physical Activity Self-Management for People with Multiple Sclerosis: A Path Analysis. Rehabil. Psychol. 2011, 56, 171–181. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 7th ed.; Always learning; Pearson: New York, NY, USA, 2019; ISBN 978-0-13-479054-1. [Google Scholar]
- Hoyle, R.H.; Gottfredson, N.C. Structural Equation Modeling with Latent Variables. In APA Handbook of Research Methods in Psychology: Research Designs: Quantitative, Qualitative, Neuropsychological, and Biological, 2nd ed.; APA Handbooks in Psychology®; American Psychological Association: Washington, DC, USA, 2023; Volume 2, pp. 459–490. ISBN 978-1-4338-4133-0. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The Patient Health Questionnaire-2: Validity of a Two-Item Depression Screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef]
- Löwe, B.; Kroenke, K.; Gräfe, K. Detecting and Monitoring Depression with a Two-Item Questionnaire (PHQ-2). J. Psychosom. Res. 2005, 58, 163–171. [Google Scholar] [CrossRef]
- Löwe, B.; Wahl, I.; Rose, M.; Spitzer, C.; Glaesmer, H.; Wingenfeld, K.; Schneider, A.; Brähler, E. A 4-Item Measure of Depression and Anxiety: Validation and Standardization of the Patient Health Questionnaire-4 (PHQ-4) in the General Population. J. Affect. Disord. 2010, 122, 86–95. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Monahan, P.O.; Löwe, B. Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Barrett, P. Structural Equation Modelling: Adjudging Model Fit. Personal. Individ. Differ. 2007, 42, 815–824. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Yuan, K.-H.; Bentler, P.M. On Chi-Square Difference and z Tests in Mean and Covariance Structure Analysis When the Base Model Is Misspecified. Educ. Psychol. Meas. 2004, 64, 737–757. [Google Scholar] [CrossRef]
- Browne, M.W.; Cudeck, R. Alternative Ways of Assessing Model Fit. Sociol. Methods Res. 1992, 21, 230–258. [Google Scholar] [CrossRef]
- Reyes Fernández, B.; Knoll, N.; Hamilton, K.; Schwarzer, R. Social-Cognitive Antecedents of Hand Washing: Action Control Bridges the Planning-Behaviour Gap. Psychol. Health 2016, 31, 993–1004. [Google Scholar] [CrossRef] [PubMed]
- Shi, D.; Maydeu-Olivares, A.; Rosseel, Y. Assessing Fit in Ordinal Factor Analysis Models: SRMR vs. RMSEA. Struct. Equ. Model. Multidiscip. J. 2020, 27, 1–15. [Google Scholar] [CrossRef]
- Kenny, D.A.; Kaniskan, B.; McCoach, D.B. The Performance of RMSEA in Models with Small Degrees of Freedom. Sociol. Methods Res. 2015, 44, 486–507. [Google Scholar] [CrossRef]
- von Lengerke, T.; Ebadi, E.; Schock, B.; Krauth, C.; Lange, K.; Stahmeyer, J.T.; Chaberny, I.F. Impact of Psychologically Tailored Hand Hygiene Interventions on Nosocomial Infections with Multidrug-Resistant Organisms: Results of the Cluster-Randomized Controlled Trial PSYGIENE. Antimicrob. Resist. Infect. Control 2019, 8, 56. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Schuz, B.; Ziegelmann, J.P.; Lippke, S.; Luszczynska, A.; Scholz, U. Adoption and Maintenance of Four Health Behaviors: Theory-Guided Longitudinal Studies on Dental Flossing, Seat Belt Use, Dietary Behavior, and Physical Activity. Ann. Behav. Med. Publ. Soc. Behav. Med. 2007, 33, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.-Q.; Zhang, R.; Schwarzer, R.; Hagger, M.S. A Meta-Analysis of the Health Action Process Approach. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2019, 38, 623–637. [Google Scholar] [CrossRef] [PubMed]
- Dahmen, A.; Keller, F.; Kötting, L.; Derksen, C.; Lippke, S. Angst Vor Dem Coronavirus, Absicht Zum Befolgen Der AHA-Regeln Und Risikowahrnehmung Bezüglich Arztbesuchen: Querschnittsstudie Mit Psychisch Vorerkrankten Menschen. Gesundheitswesen Bundesverb. Arzte Offentlichen Gesundheitsdienstes Ger. 2021, 83, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Lippke, S.; Keller, F.M.; Derksen, C.; Kötting, L.; Dahmen, A. Hygiene Behaviors and SARS-CoV-2-Preventive Behaviors in the Face of the COVID-19 Pandemic: Self-Reported Compliance and Associations with Fear, SARS-CoV-2 Risk, and Mental Health in a General Population vs. a Psychosomatic Patients Sample in Germany. Hygiene 2022, 2, 28–43. [Google Scholar] [CrossRef]
- Guzek, D.; Skolmowska, D.; Głąbska, D. Analysis of Gender-Dependent Personal Protective Behaviors in a National Sample: Polish Adolescents’ COVID-19 Experience (PLACE-19) Study. Int. J. Environ. Res. Public Health 2020, 17, 5770. [Google Scholar] [CrossRef]
- Hobbs, M.A.; Robinson, S.; Neyens, D.M.; Steed, C. Visitor Characteristics and Alcohol-Based Hand Sanitizer Dispenser Locations at the Hospital Entrance: Effect on Visitor Use Rates. Am. J. Infect. Control 2016, 44, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Gaube, S.; Tsivrikos, D.; Dollinger, D.; Lermer, E. How a Smiley Protects Health: A Pilot Intervention to Improve Hand Hygiene in Hospitals by Activating Injunctive Norms through Emoticons. PLoS ONE 2018, 13, e0197465. [Google Scholar] [CrossRef] [PubMed]
| α | M | SD | ASE | OE | RISK | INT | MSE | PL | RES | SUP | HYG | DEP | ANX | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASE | 0.87 | 19.13 | 4.28 | - | ||||||||||
| OE | 0.83 | 24.61 | 3.83 | 0.41 ** | - | |||||||||
| RISK | - 1 | 3.16 | 1.33 | −0.20 ** | 0.03 | - | ||||||||
| INT | 0.68 | 10.04 | 1.87 | 0.55 ** | 0.50 ** | −0.08 | - | |||||||
| MSE | 0.91 | 19.58 | 3.99 | 0.56 ** | 0.48 ** | −0.08 | 0.55 ** | - | ||||||
| PL | 0.86 | 12.43 | 5.34 | 0.40 ** | 0.38 ** | −0.14 ** | 0.40 ** | 0.28 * | - | |||||
| RES | 0.81 | 20.28 | 5.03 | 0.27 ** | 0.34 ** | 0.03 | 0.21 ** | 0.26 ** | 0.16 ** | - | ||||
| SUP | 0.92 | 5.82 | 3.15 | 0.27 ** | 0.30 ** | 0.05 | 0.24 * | 0.06 | 0.33 ** | 0.44 ** | - | |||
| HYG | 0.87 | 48.12 | 7.98 | 0.39 ** | 0.32 ** | −0.20 ** | 0.52 ** | 0.44 ** | 0.36 ** | 0.22 ** | 0.12 * | - | ||
| DEP | 0.86 | 5.89 | 4.75 | −0.08 | −0.03 | −0.04 | 0.01 | −0.03 | 0.01 | −0.12 | −0.07 | −0.07 | - | |
| ANX | 0.85 | 4.70 | 3.82 | −0.08 | −0.03 | −0.08 | 0.03 | −0.10 | 0.01 | −0.05 | −0.10 | −0.01 | −0.48 ** | - |
| Indices | Unrestricted Model | Semi-Restricted Model | Fully Restricted Mode |
|---|---|---|---|
| χ2—Test of model fit | 40.49 | 51.77 | 63.15 |
| df | 16 | 12 | 27 |
| χ2 | p < 0.01 | p < 0.01 | p < 0.05 |
| CFI | 0.94 | 0.94 | 0.95 |
| TLI | 0.85 | 0.92 | 0.95 |
| Model 1 Delta TLI | – | −0.07 | −0.09 |
| RMSEA (90% CI) | 0.08 | 0.06 | 0.04 |
| Indices | Unrestricted Model | Semi-Restricted Model | Fully Restricted Model |
|---|---|---|---|
| χ2—Test of model fit | 29.75 | 40.63 | 63.80 |
| df | 16 | 12 | 27 |
| χ2 | p = 0.020 | p = 0.062 | p = 0.013 |
| CFI | 0.97 | 0.97 | 0.97 |
| TLI | 0.92 | 0.95 | 0.95 |
| Model 1 Delta TLI | - | −0.03 | −0.03 |
| RMSEA (90% CI) | 0.06 | 0.04 | 0.04 |
| ASE | OE | RISK | INT | MSE | PL | HYG | |
|---|---|---|---|---|---|---|---|
| With symptoms of depression in comparison to the reference group without depressive symptoms | |||||||
| Mean estimate (ME) | −0.194 | −0.090 | −0.137 | 0.049 | −0.239 | 0.050 | 0.016 |
| Standard error (SE) | 0.163 | 0.126 | 0.238 | 0.154 | 0.150 | 0.282 | 0.018 |
| Critical ratio (CR) | −1.252 | −0.715 | −0.576 | 0.320 | −1.159 | 0.177 | 0.907 |
| p | 0.233 | 0.475 | 0.565 | 0.749 | 0.110 | 0.859 | 0.365 |
| With symptoms of anxiety in comparison to the reference group without symptoms of anxiety | |||||||
| Mean estimate (ME) | −0.227 | −0.102 | −0.310 | 0.068 | −0.072 | 0.127 | −0.043 |
| Standard error (SE) | 0.212 | 0.136 | 0.242 | 0.176 | 0.168 | 0.294 | 0.029 |
| Critical ratio (CR) | −1.073 | −0.752 | −1.280 | 0.384 | −0.429 | 0.433 | −1.466 |
| p | 0.283 | 0.452 | 0.201 | 0.701 | 0.668 | 0.665 | 0.143 |
| Time 2 (after Rehabilitation) | ||||
|---|---|---|---|---|
| Non-Compliance | Compliance | Total | ||
| Time 1 | Non-compliance | 25 (45.46) | 30 (54.54) | 55 (100) |
| Compliance | 47 (4.69) | 956 (95.31) | 1003 (100) | |
| Predictors | Wald | OR | 95% CIOR | p-Value | Remaining in Baseline | Change in Compliance | ||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | |||||
| Change in compliance: remaining non-compliant (0) versus progression (1) | ||||||||
| Depression | 1.03 | 1.36 | 0.75–2.48 | 0.31 | 2.79 | 1.14 | 3.27 | 1.89 |
| Anxiety | 0.32 | 0.84 | 0.45–1.57 | 0.58 | 2.84 | 1.25 | 3.10 | 1.69 |
| Change in compliance: remaining compliant (0) versus regression (1) | ||||||||
| Depression | 1.14 | 1.15 | 0.89–1.48 | 0.29 | 3.45 | 1.66 | 3.83 | 1.61 |
| Anxiety | 0.05 | 0.97 | 0.75–1.26 | 0.84 | 3.61 | 1.67 | 3.82 | 1.35 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keller, F.M.; Dahmen, A.; Kötting, L.; Derksen, C.; Lippke, S. Evaluation of Social-Cognitive Determinants of Patients’ Hand Hygiene Decisions and the Role of Mental Health in a Cross-Sectional and a Longitudinal Study of German Patients. Hygiene 2024, 4, 76-92. https://doi.org/10.3390/hygiene4010005
Keller FM, Dahmen A, Kötting L, Derksen C, Lippke S. Evaluation of Social-Cognitive Determinants of Patients’ Hand Hygiene Decisions and the Role of Mental Health in a Cross-Sectional and a Longitudinal Study of German Patients. Hygiene. 2024; 4(1):76-92. https://doi.org/10.3390/hygiene4010005
Chicago/Turabian StyleKeller, Franziska Maria, Alina Dahmen, Lukas Kötting, Christina Derksen, and Sonia Lippke. 2024. "Evaluation of Social-Cognitive Determinants of Patients’ Hand Hygiene Decisions and the Role of Mental Health in a Cross-Sectional and a Longitudinal Study of German Patients" Hygiene 4, no. 1: 76-92. https://doi.org/10.3390/hygiene4010005
APA StyleKeller, F. M., Dahmen, A., Kötting, L., Derksen, C., & Lippke, S. (2024). Evaluation of Social-Cognitive Determinants of Patients’ Hand Hygiene Decisions and the Role of Mental Health in a Cross-Sectional and a Longitudinal Study of German Patients. Hygiene, 4(1), 76-92. https://doi.org/10.3390/hygiene4010005







