Independent Living for Older Adults with Cognitive Impairment: A Narrative Review of Stakeholder Perceptions and Experiences with Assistive and Socially Assistive Robots
Abstract
1. Introduction
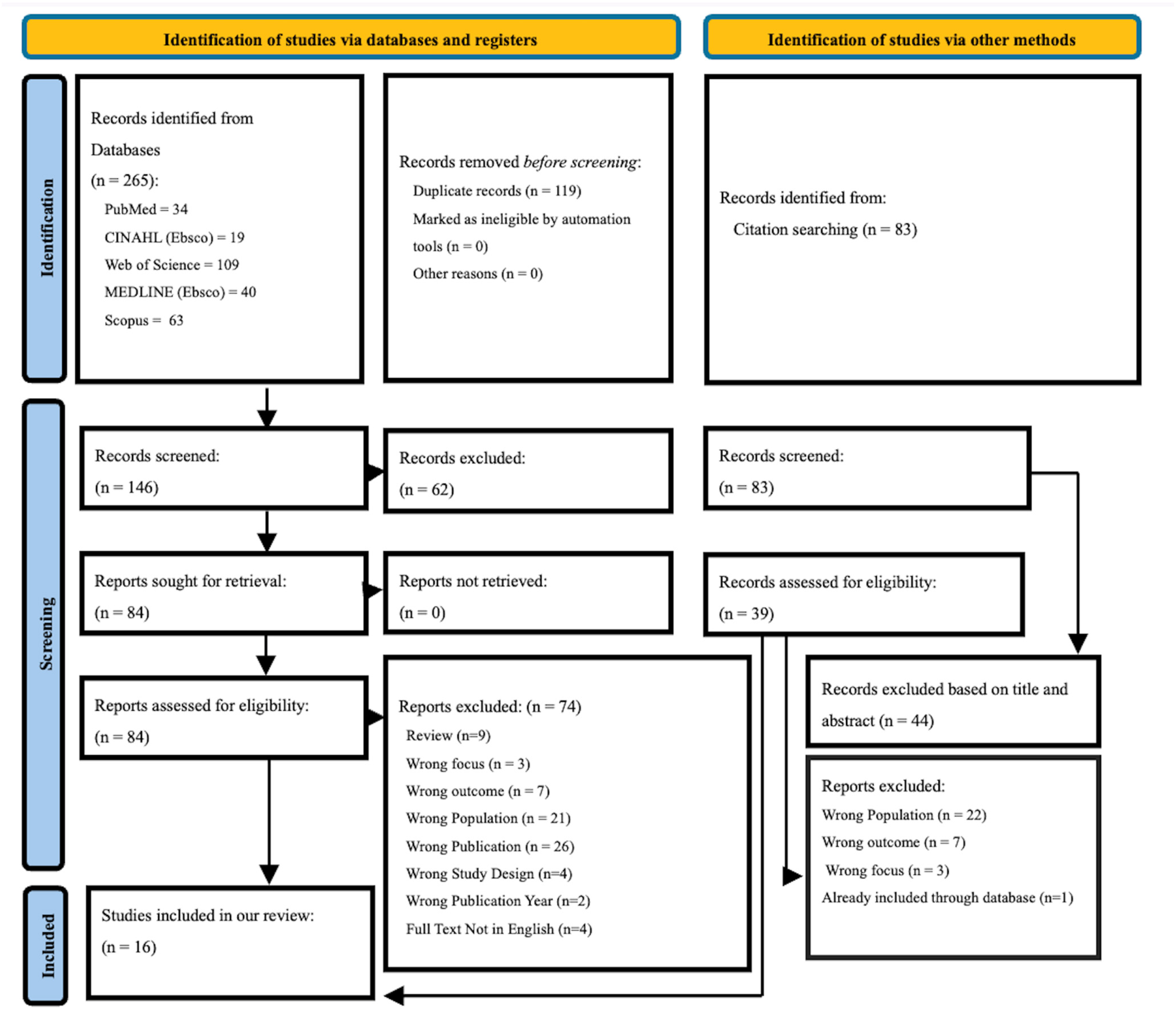
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Study Selection
2.3. Data Extraction
2.4. Data Synthesis
3. Results
3.1. Qualitative Findings
3.1.1. Domain 1: User Perceptions and Experiences
Theme 1: Perceived Usefulness and Benefits
Theme 2: Acceptance and Satisfaction
Theme 3: Emotional Connection
Theme 4: Control and Autonomy
3.1.2. Domain 2: Barriers to Adoption
Theme 1: Ethical Concerns and Emotional Disconnect
Theme 2: Technical Fears and Usability Challenges
Theme 3: Design and Functionality Limitations
Theme 4: Caregivers and Care Receiver Misalignment
Theme 5: Cost Concerns
3.1.3. Domain 3: Suggestions for Improving Robots for Independent Living
Theme 1: Personalization and Adaptation
Theme 2: Enhancing Robot Features
Theme 3: Advanced Functionalities
3.2. Quantitative Findings
3.2.1. Measure 1: Usability and Usefulness
3.2.2. Measure 2: Acceptance and Satisfaction
3.2.3. Measure 3: Human–Robot Interaction
3.2.4. Measure 4: Preferences
3.2.5. Measure 5: Barriers
4. Discussion
4.1. What Drives Robots’ Acceptance in Dementia Care?
4.2. Emotional Bonding vs. Functional Utility
4.3. Tensions Between Safety, Surveillance, and Autonomy
4.4. Ethical Concerns and Design Implications
4.5. Limitations
4.6. Gaps in the Literature and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADRD | Alzheimer’s disease and related dementias |
| PICo | Population, Phenomenon of Interest, Context |
| MCI | Mild cognitive impairment |
| AI | Artificial intelligence |
References
- World Health Organization. Dementia Facts Sheet. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 5 September 2025).
- Alzheimer’s Association. 2024 Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement. 2024, 20, 3708–3821. [Google Scholar] [CrossRef] [PubMed]
- Portacolone, E.; Halpern, J.; Luxenberg, J.; Harrison, K.L.; Covinsky, K.E. Ethical Issues Raised by the Introduction of Artificial Companions to Older Adults with Cognitive Impairment: A Call for Interdisciplinary Collaborations. J. Alzheimer’s Dis. 2020, 76, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Rahemi, Z.; Williams, C.L.; Tappen, R.M.; Engstrom, G.A. Health-Related Decisions for Serious Illness Among Ethnically Diverse Older Adults. ANS Adv. Nurs. Sci. 2018, 41, 84–97. [Google Scholar] [CrossRef] [PubMed]
- Rahemi, Z.; Parker, V. Does Culture Matter? Young and Middle-Aged Iranian-American Adults’ Perspectives Regarding End-of-Life Care Planning. Am. J. Hosp. Palliat. Care 2022, 39, 555–561. [Google Scholar] [CrossRef]
- Dratsiou, I.; Varella, A.; Romanopoulou, E.; Villacañas, O.; Cooper, S.; Isaris, P.; Serras, M.; Unzueta, L.; Silva, T.; Zurkuhlen, A.; et al. Assistive Technologies for Supporting the Wellbeing of Older Adults. Technologies 2022, 10, 8. [Google Scholar] [CrossRef]
- Bedaf, S.; Draper, H.; Gelderblom, G.-J.; Sorell, T.; de Witte, L. Can a Service Robot Which Supports Independent Living of Older People Disobey a Command? The Views of Older People, Informal Carers and Professional Caregivers on the Acceptability of Robots. Int. J. Soc. Robot. 2016, 8, 409–420. [Google Scholar] [CrossRef]
- Ghimire, B.; Parekh, M.; Behlow, H.; Sabet, M.; Bhattacharya, S.; Sapkota, N.; Chauhan, P.S.; Misra, A.; Rao, A.M. An Electrochemical Oscillator for Harvesting near Room Temperature Waste Heat. J. Mater. Chem. A 2025, 13, 6560–6572. [Google Scholar] [CrossRef]
- Sapkota, N.; Sabet, M.; Parekh, M.; Chen, N.; Basel, J.; Koehler, K.C.; Ding, Y.; Rao, A.M. Commercial Cellulosic Paper-Based Solid Electrolyte for High-Temperature Lithium–Sulfur Batteries. ACS Appl. Mater. Interfaces 2025, 17, 1234–1243. [Google Scholar] [CrossRef]
- Chen, N.; Sabet, M.; Sapkota, N.; Parekh, M.; Chiluwal, S.; Koehler, K.; Clemons, C.M.; Ding, Y.; Rao, A.M.; Pilla, S. Bioderived Silicon Nano-Quills: Synthesis, Structure and Performance in Lithium-Ion Battery Anodes. Green Chem. 2024, 26, 4691–4702. [Google Scholar] [CrossRef]
- Hsieh, C.-J.; Li, P.-S.; Wang, C.-H.; Lin, S.-L.; Hsu, T.-C.; Tsai, C.-M.T. Socially Assistive Robots for People Living with Dementia in Long-Term Facilities: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Gerontology 2023, 69, 1027–1042. [Google Scholar] [CrossRef]
- Sawik, B.; Tobis, S.; Baum, E.; Suwalska, A.; Kropińska, S.; Stachnik, K.; Pérez-Bernabeu, E.; Cildoz, M.; Agustin, A.; Wieczorowska-Tobis, K. Robots for Elderly Care: Review, Multi-Criteria Optimization Model and Qualitative Case Study. Healthcare 2023, 11, 1286. [Google Scholar] [CrossRef]
- Zsiga, K.; Edelmayer, G.; Rumeau, P.; Péter, O.; Tóth, A.; Fazekas, G. Home Care Robot for Socially Supporting the Elderly: Focus Group Studies in Three European Countries to Screen User Attitudes and Requirements. Int. J. Rehabil. Res. 2013, 36, 375–378. [Google Scholar] [CrossRef]
- Engelhart, K. What Robots Can—And Can’t—Do for the Old and Lonely. Available online: https://www.newyorker.com/magazine/2021/05/31/what-robots-can-and-cant-do-for-the-old-and-lonely (accessed on 28 April 2025).
- Higgins, M.; Brewer, L. Promoting the Benefits of Cognitive Stimulation Amongst Older Patients: A Brief Survey and Quality Improvement Project. Age Ageing 2022, 51, afac218.311. [Google Scholar] [CrossRef]
- Sirizi, D.; Sabet, M.; Yahyaeian, A.A.; Bacsu, J.-D.R.; Smith, M.L.; Rahemi, Z. Evaluating Human-Robot Interactions to Support Healthy Aging-in-Place. J. Appl. Gerontol. 2024, 44, 7334648241301485. [Google Scholar] [CrossRef]
- Sutton, A.; Clowes, M.; Preston, L.; Booth, A. Meeting the Review Family: Exploring Review Types and Associated Information Retrieval Requirements. Health Inf. Libr. J. 2019, 36, 202–222. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, M.-S.; Jahanshahlou, F.; Akbarzadeh, M.A.; Zarei, M.; Vaez-Gharamaleki, Y. Formulating Research Questions for Evidence-Based Studies. J. Med. Surg. Public Health 2024, 2, 100046. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic Review or Scoping Review? Guidance for Authors When Choosing between a Systematic or Scoping Review Approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Veritas Health Innovation Covidence Systematic Review Software 2024. Available online: www.covidence.org (accessed on 11 July 2025).
- Arthanat, S.; Begum, M. Effectiveness and Adoption of a Smart Home-Based Social Assistive Robot for Care of Individuals with Alzheimer’s Disease; University of New Hampshire: Durham, NH, USA, 2020. [Google Scholar]
- Dosso, J.A.; Bandari, E.; Malhotra, A.; Guerra, G.K.; Hoey, J.; Michaud, F.; Prescott, T.J.; Robillard, J.M. User Perspectives on Emotionally Aligned Social Robots for Older Adults and Persons Living with Dementia. J. Rehabil. Assist. Technol. Eng. 2022, 9, 20556683221108364. [Google Scholar] [CrossRef]
- Harris-Gersten, M.L.; Davagnino, J.M.; Alcorn, E.R.; Hastings, S.N. Usability and Acceptability of Social Robot Pets Among Community-Dwelling Veterans Living With Dementia and Their Caregivers. Am. J. Alzheimer’s Dis. Other Dement. 2023, 38, 15333175231200973. [Google Scholar] [CrossRef]
- Shin, M.H.; McLaren, J.; Ramsey, A.; Sullivan, J.L.; Moo, L. Improving a Mobile Telepresence Robot for People With Alzheimer Disease and Related Dementias: Semistructured Interviews With Stakeholders. JMIR Aging 2022, 5, e32322. [Google Scholar] [CrossRef]
- Turner, N.R.; Berridge, C. How I Want Technology Used in My Care: Learning from Documented Choices of People Living with Dementia Using a Dyadic Decision Making Tool. Inform. Health Soc. Care 2023, 48, 387–401. [Google Scholar] [CrossRef]
- Van Assche, M.; Petrovic, M.; Cambier, D.; Calders, P.; Van Gelder, P.; Van De Velde, D. The Perspectives of Older Adults with Mild Cognitive Impairment and Their Caregivers on the Use of Socially Assistive Robots in Healthcare: Exploring Factors That Influence Attitude in a Pre-Implementation Stage. Disabil. Rehabil. Assist. Technol. 2022, 19, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Van Assche, M.; Petrovic, M.; Cambier, D.; Calders, P.; Van Gelder, P.; Werner, F.; Van De Velde, D. Socially Assistive Robots in Aged Care: Expectations of Older Adults with MCI in Assisted Living Facilities and Their Caregivers. Int. J. Soc. Robot. 2024, 16, 687–698. [Google Scholar] [CrossRef]
- Van Orden, K.A.; Bower, E.; Beckler, T.; Rowe, J.; Gillespie, S. The Use of Robotic Pets with Older Adults during the COVID-19 Pandemic. Clin. Gerontol. 2022, 45, 189–194. [Google Scholar] [CrossRef]
- Chen, L.Y.; Sumioka, H.; Ke, L.J.; Shiomi, M.; Chen, L. Effects of Teleoperated Humanoid Robot Application in Older Adults with Neurocognitive Disorders in Taiwan: A Report of Three Cases. Aging Med. Healthc. 2020, 11, 67–71. [Google Scholar] [CrossRef]
- Coşar, S.; Fernandez-Carmona, M.; Agrigoroaie, R.; Pages, J.; Ferland, F.; Zhao, F.; Yue, S.; Bellotto, N.; Tapus, A. ENRICHME: Perception and Interaction of an Assistive Robot for the Elderly at Home. Int. J. Soc. Robot. 2020, 12, 779–805. [Google Scholar] [CrossRef]
- Raghunath, N.; Pereyda, C.; Frow, J.; Cook, D.; Schmitter-Edgecombe, M. A Robot Activity Support (RAS) System for Persons with Memory Impairment: Comparing Older and Younger Adults’ Perceptions of the System. Gerontechnology 2020, 19, 1–11. [Google Scholar] [CrossRef]
- Yuan, F.; Anderson, J.G.; Wyatt, T.H.; Lopez, R.P.; Crane, M.; Montgomery, A.; Zhao, X. Assessing the Acceptability of a Humanoid Robot for Alzheimer’s Disease and Related Dementia Care Using an Online Survey. Int. J. Soc. Robot. 2022, 14, 1223–1237. [Google Scholar] [CrossRef]
- Law, M.; Sutherland, C.; Ahn, H.S.; MacDonald, B.A.; Peri, K.; Johanson, D.L.; Vajsakovic, D.-S.; Kerse, N.; Broadbent, E. Developing Assistive Robots for People with Mild Cognitive Impairment and Mild Dementia: A Qualitative Study with Older Adults and Experts in Aged Care. BMJ Open 2019, 9, e031937. [Google Scholar] [CrossRef]
- Cruz-Sandoval, D.; Favela, J. Incorporating Conversational Strategies in a Social Robot to Interact with People with Dementia. Dement. Geriatr. Cogn. Disord. 2019, 47, 140–148. [Google Scholar] [CrossRef]
- Noyes, J.; Booth, A.; Moore, G.; Flemming, K.; Tunçalp, Ö.; Shakibazadeh, E. Synthesising Quantitative and Qualitative Evidence to Inform Guidelines on Complex Interventions: Clarifying the Purposes, Designs and Outlining Some Methods. BMJ Glob. Health 2019, 4, e000893. [Google Scholar] [CrossRef]
- Bevilacqua, R.; Felici, E.; Cavallo, F.; Amabili, G.; Maranesi, E. Designing Acceptable Robots for Assisting Older Adults: A Pilot Study on the Willingness to Interact. Int. J. Environ. Res. Public. Health 2021, 18, 10686. [Google Scholar] [CrossRef]
- Rebola, C.; Malle, B. A Longitudinal Study of Older Adults’ Acceptance of Robot Companions and Their Effects on Well-Being. Innov. Aging 2021, 5, 40–41. [Google Scholar] [CrossRef]
- Bayles, M.A.; Lee, J.; Kadylak, T.; Rogers, W.A. Understanding Older Adults’ Initial Perceptions of Robot Appearance and Function: Implications for Acceptance. Gerontechnology 2023, 22, 1–7. [Google Scholar] [CrossRef]
- MIT Media Lab. Co-Design of Social Robots with Older Adults. Available online: https://www.media.mit.edu/projects/co-design-of-social-robots-with-older-adults/overview/ (accessed on 28 April 2025).
- Wu, Y.-H.; Cristancho-Lacroix, V.; Fassert, C.; Faucounau, V.; de Rotrou, J.; Rigaud, A.-S. The Attitudes and Perceptions of Older Adults With Mild Cognitive Impairment Toward an Assistive Robot. J. Appl. Gerontol. 2016, 35, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Lim, J. Effects of a Cognitive-Based Intervention Program Using Social Robot PIO on Cognitive Function, Depression, Loneliness, and Quality of Life of Older Adults Living Alone. Front. Public Health 2023, 11, 1097485. [Google Scholar] [CrossRef]
- Robinson, H.; MacDonald, B.; Broadbent, E. The Role of Healthcare Robots for Older People at Home: A Review. Int. J. Soc. Robot. 2014, 6, 575–591. [Google Scholar] [CrossRef]
- Wada, K.; Shibata, T. Living With Seal Robots—Its Sociopsychological and Physiological Influences on the Elderly at a Care House. IEEE Trans. Robot. 2007, 23, 972–980. [Google Scholar] [CrossRef]
- Goher, K.M.; Mansouri, N.; Fadlallah, S.O. Assessment of Personal Care and Medical Robots from Older Adults’ Perspective. Robot. Biomim. 2017, 4, 5. [Google Scholar] [CrossRef]
- Hung, L.; Liu, C.; Woldum, E.; Au-Yeung, A.; Berndt, A.; Wallsworth, C.; Horne, N.; Gregorio, M.; Mann, J.; Chaudhury, H. The Benefits of and Barriers to Using a Social Robot PARO in Care Settings: A Scoping Review. BMC Geriatr. 2019, 19, 232. [Google Scholar] [CrossRef]
- Pirhonen, J.; Melkas, H.; Laitinen, A.; Pekkarinen, S. Could Robots Strengthen the Sense of Autonomy of Older People Residing in Assisted Living Facilities?—A Future-Oriented Study. Ethics Inf. Technol. 2020, 22, 151–162. [Google Scholar] [CrossRef]
| Authors, Year | Country | Method | Framework | Robot Type and Function | Purpose | Participants | Data Collection and Analysis | Key Findings/Themes |
|---|---|---|---|---|---|---|---|---|
| Arthanat and Begum (2020) [21] | U.S. | Qualitative Design | UTAUT, technology acceptance |
| Beta-test a novel SAR with ADRD caregivers and gather perspectives on home integration. |
|
|
|
| Dosso et al. (2022) [22] | Canada | Mixed-Methods Design (Survey + Open-Ended Questions) | TAM, Almere model, ACT |
| Understand emotional alignment and attitudes of (1) healthy older adults, (2) older adults with dementia, (3) care partners, in response to pet-like robots. | n = 206 participants
|
|
|
| Harris-Gersten et al. (2023) [23] | U.S. | Mixed-Methods Design | NIH stage model for behavioral interventions |
| Assess the usability and acceptability of robot pets among veterans with dementia and caregivers. |
|
|
|
| Portacolone et al. (2020) [3] | U.S. | Case Study (Qualitative) | Biomedical ethics (respect, beneficence, non-maleficence, justice) |
| Describe ethical issues in a specific case using a pet-avatar robot and suggest improvements for ethical application. |
|
|
|
| Sawik et al. (2023) [12] | Poland | Qualitative | Person-centered care |
| Explore robotic support for older adults with MCI. |
|
|
|
| Shin et al. (2022) [24] | U.S. | Qualitative Design | TAM (perceived usefulness, ease of use) |
| Assess applications to support the independence of individuals with MCI or ADRD and gather stakeholder opinions. |
|
|
|
| Turner and Berridge (2023) [25] | U.S. | Mixed-Methods (Convergent Design) | H-TAM |
| Examine the technology choices of people with mild AD and fit with the H-TAM framework. |
|
|
|
| Van Assche et al. (2022) [26] | Belgium | Qualitative Design | COREQ |
| Explore attitudes of older adults and caregivers toward SARs in assisted living. |
|
|
|
| Van Assche et al. (2024) [27] | Belgium | Qualitative Design | COREQ |
| Explore needs and preferences regarding SARs in assisted living. |
|
|
|
| Van Orden et al. (2022) [28] | U.S. | Qualitative Design | None specified |
| Inform implementation of robotic pet programs in real-world dementia care. |
|
|
|
| Chen et al. (2020) [29] | Taiwan | Case Study (Mixed Methods) | None specified |
| Explore participant experience, NPS impacts, uncanny valley response, and influencing factors. |
|
|
|
| Coşar et al. (2020) [30] | UK, Greece, Poland | Qualitative | None specified |
| Evaluate user interaction and experience with ENRICHME. |
|
|
|
| Raghunath et al. (2020) [31] | U.S. | Mixed Methods | None specified |
| Compare perceptions of RAS between younger and older adults. |
|
|
|
| Yuan et al. (2022) [32] | U.S. | Mixed Methods | Almere model |
| Assess attitudes toward Pepper for ADRD care and identify user needs. |
|
|
|
| Law et al. (2019) [33] | New Zealand | Qualitative Design | None specified |
| Evaluate the usefulness of daily care functions shown via the robot. |
|
|
|
| Cruz-Sandoval and Favela (2019) [34] | Mexico | Quantitative Methods | None specified |
| Assess effectiveness of conversation strategies to enhance PwD communication. |
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sirizi, D.; Sabet, M.; Hummel, K.; Bacsu, J.-D.R.; Longo, A.; Rahemi, Z. Independent Living for Older Adults with Cognitive Impairment: A Narrative Review of Stakeholder Perceptions and Experiences with Assistive and Socially Assistive Robots. J. Ageing Longev. 2025, 5, 34. https://doi.org/10.3390/jal5030034
Sirizi D, Sabet M, Hummel K, Bacsu J-DR, Longo A, Rahemi Z. Independent Living for Older Adults with Cognitive Impairment: A Narrative Review of Stakeholder Perceptions and Experiences with Assistive and Socially Assistive Robots. Journal of Ageing and Longevity. 2025; 5(3):34. https://doi.org/10.3390/jal5030034
Chicago/Turabian StyleSirizi, Delaram, Morteza Sabet, Katelyn Hummel, Juanita-Dawne R. Bacsu, Ava Longo, and Zahra Rahemi. 2025. "Independent Living for Older Adults with Cognitive Impairment: A Narrative Review of Stakeholder Perceptions and Experiences with Assistive and Socially Assistive Robots" Journal of Ageing and Longevity 5, no. 3: 34. https://doi.org/10.3390/jal5030034
APA StyleSirizi, D., Sabet, M., Hummel, K., Bacsu, J.-D. R., Longo, A., & Rahemi, Z. (2025). Independent Living for Older Adults with Cognitive Impairment: A Narrative Review of Stakeholder Perceptions and Experiences with Assistive and Socially Assistive Robots. Journal of Ageing and Longevity, 5(3), 34. https://doi.org/10.3390/jal5030034






