The Usability of Hip Protectors: A Mixed-Method Study from the Perspectives of Singapore Nursing Home Care Staff
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
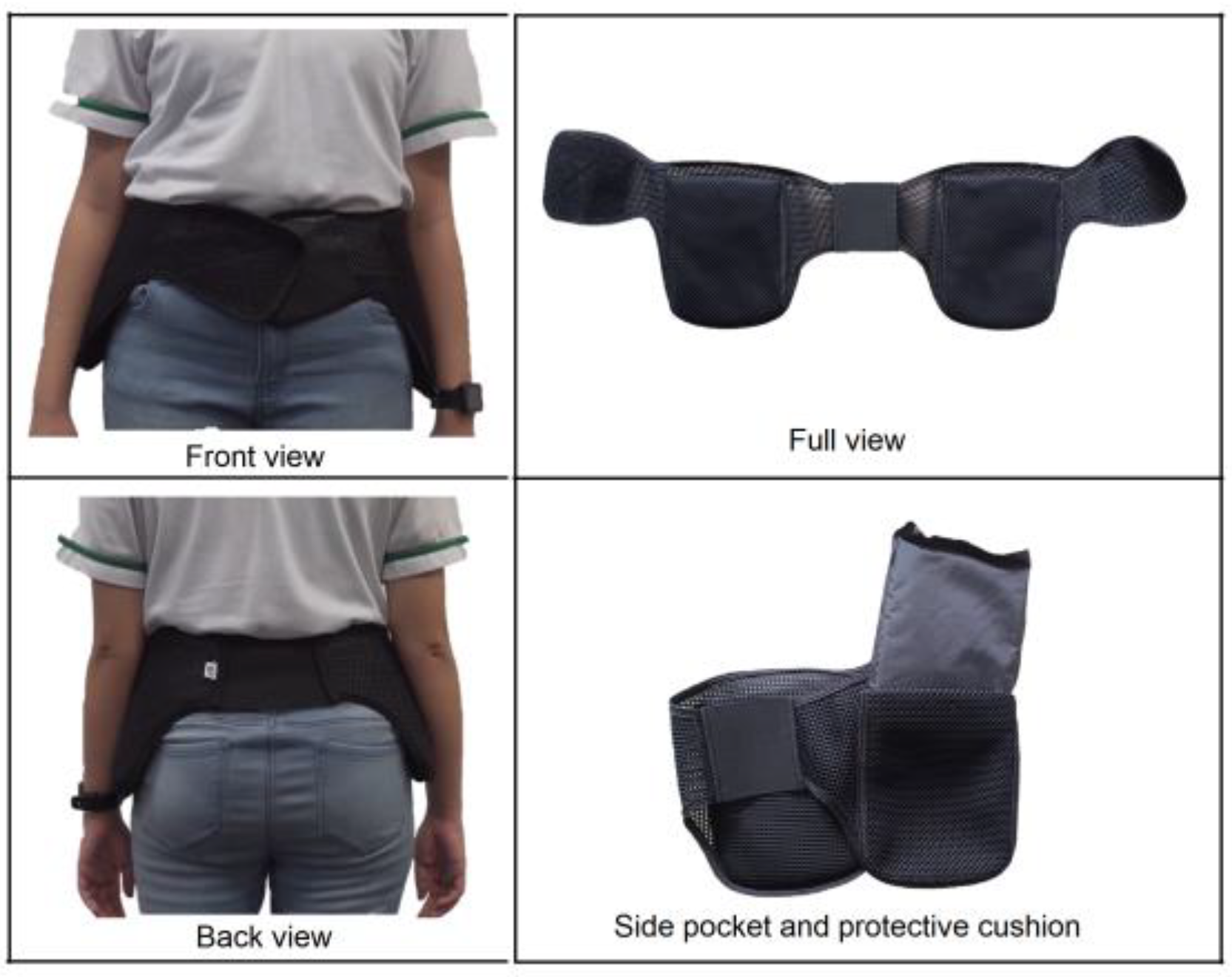
2.3. Hip Protector Trial
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. Quantitative Findings
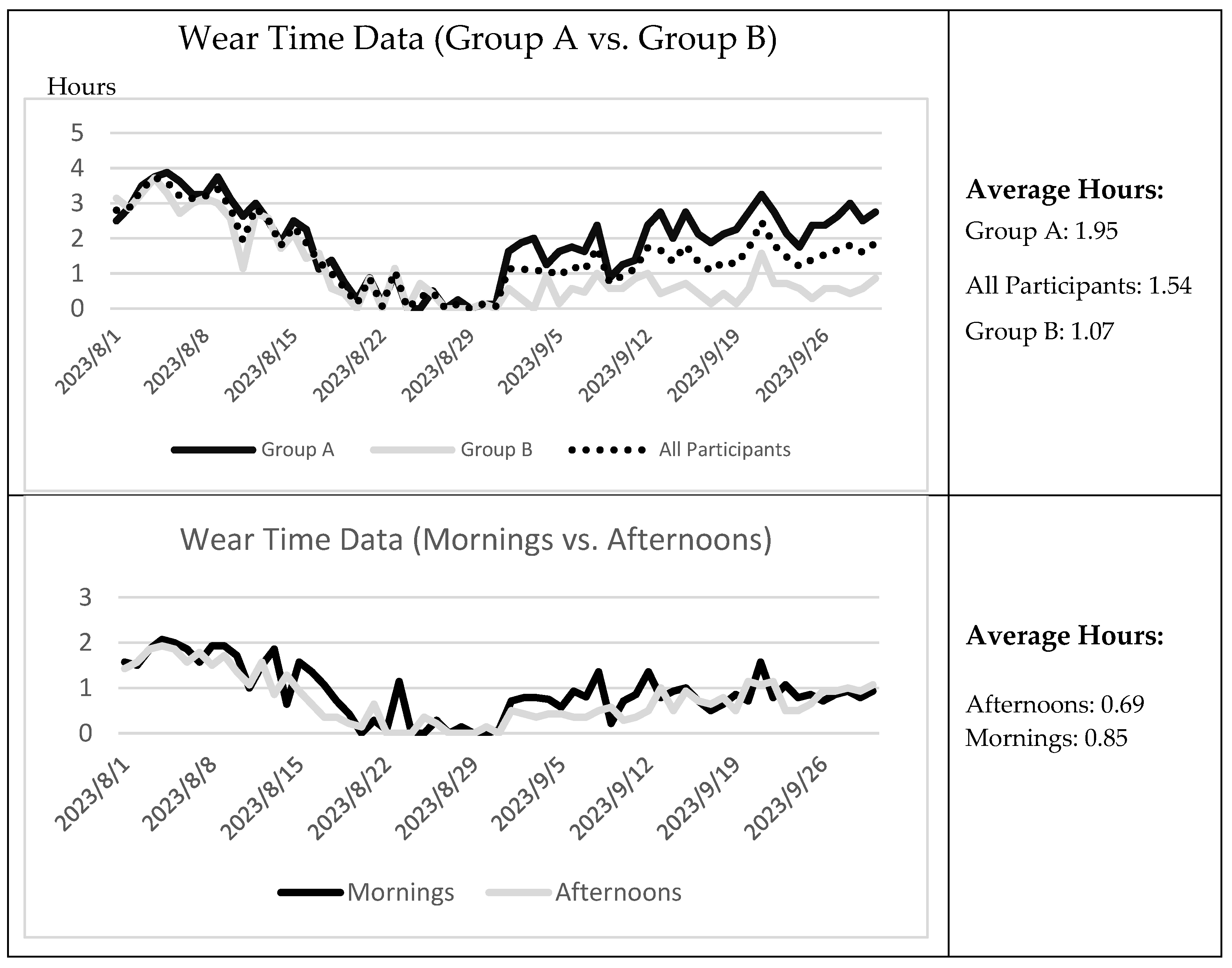
Wear Time Trends
3.2. Qualitative Findings
3.2.1. Learnability
- facilitators affecting the users’ learnability;
I appreciate the video. Because there’s visual feedback … our care staff translated [to] Chinese and … Malay. So, everybody understood. (S3)
Even though I don’t understand Chinese, [and] even residents who don’t understand anything, by seeing the demonstration, they will understand. (S5)
I can …[help] him wear [it] because I can talk to him … But other staff he [does] not follow … he will just throw everywhere, he shouts and make noise. (S8)
Since … S10 came back from hospital leave … the wearing has become more … we need staff to remind the elderly to always wear it. (S1)
- barriers affecting users’ learnability.
He tends not to wear the … [hip] protector… because … he always … goes toilet … because of incontinence (S7)
I think this training must be continued because they are very forgetful. (S4)
I was teaching them … how to wear. I tried to explain it to those who can only understand Chinese …, but my Chinese [is] not so good (S6)
I gave him (S2) the list of the elders … I am hoping that all the elders should be given [the hip protector], but I don’t know why he (S2) never gave [it] to “R6”. (S1)
3.2.2. Efficiency
- facilitators affecting the efficiency of the use of the hip protector;
… with the hip protector, they were still able to do their everyday activities within the household. So, it didn’t hinder anything. (S3)
I like the easy-to-use part of it, so the Velcro [is] easy to adjust if there is a mistake you just open [it] up (S3)
…If they trust you, they believe in you, then they will wear. (S1)
Reminders of wearing the hip protector were implemented and she’s really very strict with the elders … when S9 is there a full day, you can see the number of hours is increased. (S1)
I think compliance improves when someone is designated and focused specifically on the implementation of the hip protector in the ward. (S3)
she goes in the morning … But I can only put her once a day to remind her because she has other work to do (S1)
We can sustain them for 2 h in the morning, and 2 h in the afternoon. (S1)
One hour for the whole day … And then … [for] the following week, there was 2 h …[then] 4 h. About 2–3 h difference (S3)
When he (R10) goes to the toilet … he’s wearing the hip protector … it’s been a part of his routine (S7)
R14 is very particular … “Everybody has why I don’t have?” Ah is like that “I must have” (S4)
The easiest ones are the dementia elderly, they don’t realise, they don’t understand. When S9 says “wear it”, they will wear it. (S1)
- barriers affecting the efficiency of the use of the hip protector.
Even like the colour… black colour inside, brown colour outside … they wear “upside down”. (S2)
Some elders …like R10, feel itchy … maybe can consider changing the material so the material is more comfortable for them (S6)
Very hot … they feel uncomfortable (S4)
They will wear it only in the morning. After lunch they remove it, and they will not wear it in the afternoon again. (S1)
Those that were compliant there are several others now find rashes, and itchiness. (S3)
R9 … was complaining of abdominal discomfort then apparently after 30 min, he dislodged his IDC. (S7)
People like R8 don’t want to wear it. R15 also don’t want to wear … most of the time, they say, “I’m in the wheelchair I don’t need to walk, I don’t do it at all.” (S4)
Like R6 right, sometimes he (gets) aggressive … If they are not in a good mood … they will throw everything. (S8)
3.2.3. Satisfaction
- facilitators affecting the care staff’s satisfaction;
I think … client R10’s confidence level is there, [confidence] increased because of the hip protector. (S7)
I said, “If you don’t want it, you can give it to other people”. “No”, he said “I will keep it” … He said it belonged to him. He will not give it to other people. (S8)
If I compare that to the one that you were telling me, the one that needs to be worn underneath, then I prefer this. (S3)
It is comfortable the way they walk. It’s not really uneasy or it’s not really unsafe. That is my reason of maybe recommending it in a nursing home in the future. (S1)
- barriers affecting the care staff’s satisfaction.
We’re not very confident the reason is because these elders have co-morbidities, [and] pre-existing conditions. So they need constant supervision (S7)
I think this has nothing to do with the equipment. It’s just how we do our SOPs, how we supervise, and how we take care of the elderly. (S3)
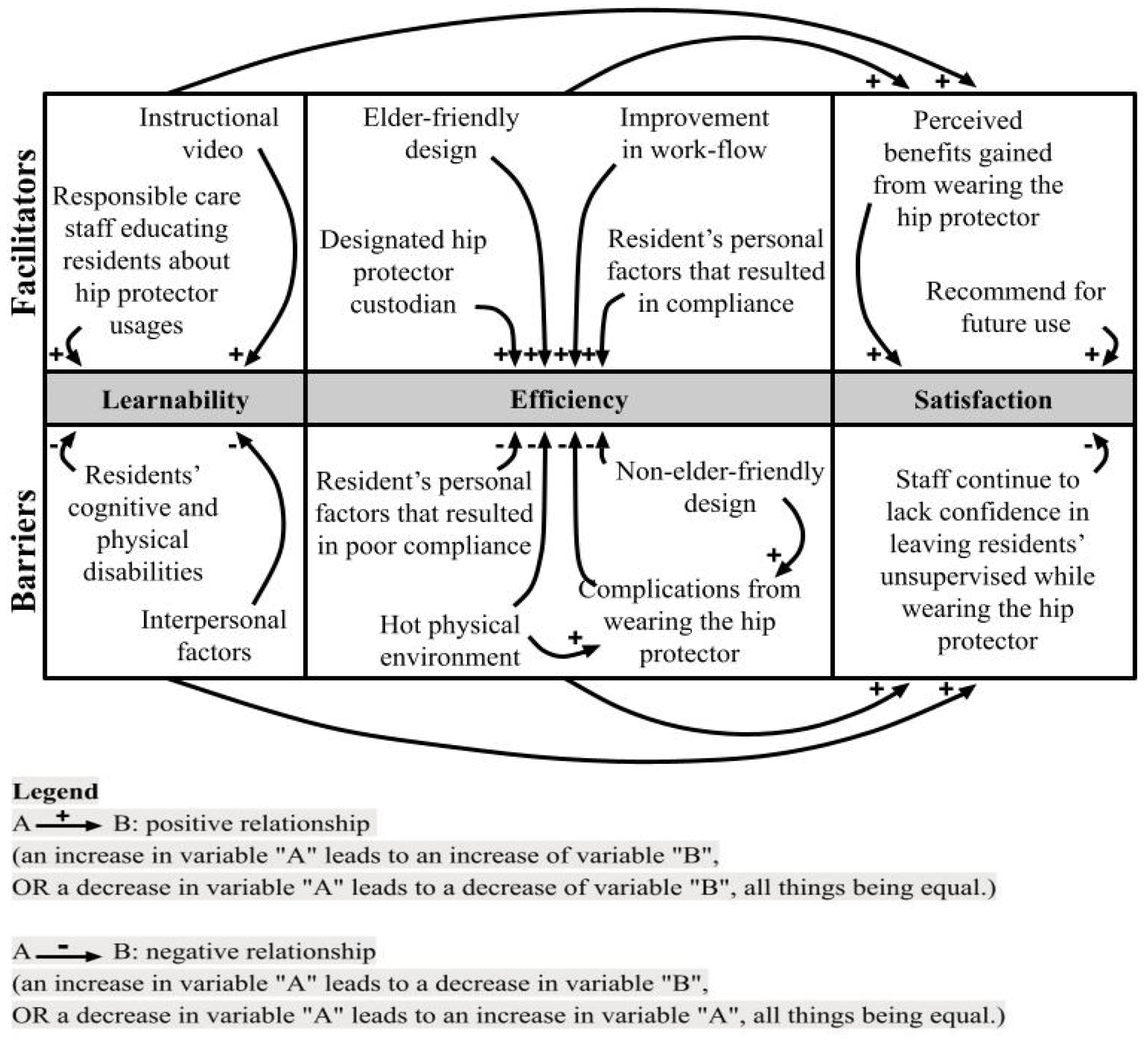
3.2.4. Relationship Between Themes
3.2.5. Relationship Between Quantitative and Qualitative Data
4. Discussion
4.1. Learnability
4.2. Efficiency
4.3. Satisfaction
4.4. Limitations of the Study
4.5. Implications for Practice and Future Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization [WHO]. WHO Global Report on Falls Prevention in Older Age; WHO: Geneva, Switzerland, 2008; Available online: https://iris.who.int/bitstream/handle/10665/43811/9789241563536_eng.pdf?sequence=1 (accessed on 1 December 2023).
- Montero-Odasso, M.; Van Der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef] [PubMed]
- Tyrovolas, S.; Koyanagi, A.; Lara, E.; Ivan Santini, Z.; Haro, J.M. Mild cognitive impairment is associated with falls among older adults: Findings from the Irish Longitudinal Study on Ageing (TILDA). Exp. Gerontol. 2016, 75, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Rau, C.S.; Lin, T.S.; Wu, S.C.; Yang, J.C.S.; Hsu, S.Y.; Cho, T.Y.; Hsieh, C.H. Geriatric hospitalizations in fall-related injuries. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 63. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Pei, J.; Ma, Y.; Cui, Y.; Guo, J.; Wei, Y.; Han, L. Cognitive frailty as a predictor of future falls in older adults: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2023, 24, 38–47. [Google Scholar] [CrossRef]
- Yong, E.L.; Ganesan, G.; Kramer, M.S.; Logan, S.; Lau, T.C.; Cauley, J.A.; Tan, K.B. Hip fractures in Singapore: Ethnic differences and temporal trends in the new millennium. Osteoporos. Int. 2019, 30, 879–886. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Josephson, K.R. The epidemiology of falls and syncope. Clin. Geriatr. Med. 2002, 18, 141–158. [Google Scholar] [CrossRef] [PubMed]
- Yap, P.; Au, S.; Ang, Y.H.; Kwan, K.Y.; Ng, S.C.; Ee, C. Who are the residents of a Nursing Home in Singapore? Singap. Med. J. 2003, 44, 65–73. Available online: https://pubmed.ncbi.nlm.nih.gov/14503779/ (accessed on 1 November 2023).
- Romli, M.H.; Tan, M.P.; Mackenzie, L.; Lovarini, M.; Suttanon, P.; Clemson, L. Falls amongst older people in Southeast Asia: A scoping review. Public Health 2017, 145, 96–112. [Google Scholar] [CrossRef]
- Takatou, K.; Shinomiya, N. Cloud-based fall Detection System with Passive RFID Sensor Tags and Supervised Learning. In Proceedings of the 2021 IEEE 10th Global Conference on Consumer Electronics (GCCE), Kyoto, Japan, 12–15 October 2021; pp. 153–156. [Google Scholar] [CrossRef]
- Hewitt, J.; Goodall, S.; Clemson, L.; Henwood, T.; Refshauge, K. Progressive resistance and balance training for falls prevention in long-term residential aged care: A cluster randomized trial of the Sunbeam Program. J. Am. Med. Dir. Assoc. 2018, 19, 361–369. [Google Scholar] [CrossRef]
- Pepera, G.; Krinta, K.; Mpea, C.; Antoniou, V.; Peristeropoulos, A.; Dimitriadis, Z. Randomized controlled trial of group exercise intervention for fall risk factors reduction in nursing home residents. Can. J. Aging 2023, 42, 328–336. [Google Scholar] [CrossRef]
- Chen, H.; Wang, S.; Tan, W.; Luo, J. STM32-based Anti-fall Smart Vest System for the Elderly. In Proceedings of the 2022 IEEE 6th Information Technology and Mechatronics Engineering Conference (ITOEC), Chongqing, China, 4–6 March 2022; Volume 6. [Google Scholar] [CrossRef]
- Santesso, N.; Carrasco-Labra, A.; Brignardello-Petersen, R.; Santesso, N. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst. Rev. 2014, 2014, CD001255. [Google Scholar] [CrossRef] [PubMed]
- Cameron, I.D.; Murray, G.R.; Gillespie, L.D.; Robertson, M.C.; Hill, K.D.; Cumming, R.G.; Kerse, N. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst. Rev. 2010, 2010, CD005465. [Google Scholar] [CrossRef]
- Parker, M.J.; Gillespie, W.J.; Gillespie, L.D. Effectiveness of hip protectors for preventing hip fractures in elderly people: Systematic review. BMJ 2006, 332, 571–573. [Google Scholar] [CrossRef]
- Sawka, A.M.; Boulos, P.; Beattie, K.; Thabane, L.; Papaioannou, A.; Gafni, A.; Cranney, A.; Zytaruk, N.; Hanley, D.A.; Adachi, J.D. Do hip protectors decrease the risk of hip fracture in institutional and community-dwelling elderly? A systematic review and meta-analysis of randomized controlled trials. Osteoporos. Int. 2005, 16, 1461–1474. [Google Scholar] [CrossRef]
- van Schoor, N.M.; Deville, W.L.; Bouter, L.M.; Lips, P.T.A.M.; Lips, P. Acceptance and compliance with external hip protectors: A systematic review of the literature. Osteoporos. Int. 2002, 13, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Health Promotion Board. Falls Prevention Among Older Adults Living in The Community; Health Promotion Board: Singapore, 2015. Available online: https://www.hpb.gov.sg/docs/default-source/pdf/cpg_falls_preventionb274.pdf (accessed on 2 October 2023).
- Wang, P.; Yap, P.; Koh, G.; Chong, J.A.; Davies, L.J.; Dalakoti, M.; Fong, N.P.; Tiong, W.W.; Luo, N. Quality of life and related factors of nursing home residents in Singapore. Health Qual. Life Outcomes 2016, 14, 112. [Google Scholar] [CrossRef]
- Hornboek, K. Current practice in measuring usability: Challenges to usability studies and research. Int. J. Hum.-Comput. Stud. 2006, 64, 79–102. [Google Scholar] [CrossRef]
- Lewis, J.R. Usability: Lessons Learned … and Yet to Be Learned. Int. J. Hum.-Comput. Interact. 2014, 30, 663–684. [Google Scholar] [CrossRef]
- Creswell, J.W.; Fetters, M.D.; Ivankova, N.V. Designing a mixed methods study in primary care. Ann. Fam. Med. 2004, 2, 7–12. [Google Scholar] [CrossRef]
- Deandrea, S.; Bravi, F.; Turati, F.; Lucenteforte, E.; La Vecchia, C.; Negri, E. Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2013, 56, 407–415. [Google Scholar] [CrossRef]
- Sahadevan, S.; Tan, N.J.L.; Tan, T.; Tan, S. Cognitive testing of elderly Chinese people in Singapore: Influence of education and age on normative scores. Age Ageing 1997, 26, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; SAGE Publications Ltd.: London, UK, 2013; Available online: https://uk.sagepub.com/en-gb/eur/successful-qualitative-research/book233059 (accessed on 1 November 2023).
- Nemeth, B.; van der Kaaij, M.; Nelissen, R.; van Wijnen, J.-K.; Drost, K.; Blauw, G.J. Prevention of hip fractures in older adults residing in long-term care facilities with a hip airbag: A retrospective pilot study. BMC Geriatr. 2022, 22, 547. [Google Scholar] [CrossRef]
- Post, E.; Komisar, V.; Sims-Gould, J.; Korall, A.; Feldman, F.; Robinovitch, S. Development of a stick-on hip protector: A multiple methods study to improve hip protector design for older adults in the acute care environment. J. Rehabil. Assist. Technol. Eng. 2019, 6, 2055668319877314. [Google Scholar] [CrossRef]
- Morgan, D.L. The Focus Group Guidebook; Sage Publications: Thousand Oaks, CA, USA, 1998; pp. 9–15. Available online: https://sk.sagepub.com/books/the-focus-group-guidebook (accessed on 5 October 2023).
- Morgan, D.; Fellows, C.; Guevara, H. Emergent methods to focus group research. In Handbook for Emergent Methods; Hesse-Biber, S.N., Leavy, P., Eds.; The Guilford Press: New York, NY, USA, 2008; pp. 189–206. Available online: https://books.google.com.sg/books?id=ZimnUvfmE-0C&lpg=PR1&ots=XnRmxaEs2D&dq=Handbook%20for%20Emergent%20Methods&lr&pg=PP1#v=onepage&q=Handbook%20for%20Emergent%20Methods&f=false (accessed on 1 September 2023).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Meyer, G.; Warnke, A.; Bender, R.; Mühlhauser, I. Effect on hip fractures of increased use of hip protectors in nursing homes: Cluster randomised controlled trial. Br. Med. J. 2003, 326, 76. [Google Scholar] [CrossRef]
- Ren, Y.; Guo, A.; Xu, Z.; Wang, T.; Wu, R.; Yang, W. Age-related functional brain connectivity during audio–visual hand-held tool recognition. Brain Behav. 2020, 10, e01759. [Google Scholar] [CrossRef]
- O’Halloran, P.D.; Cran, G.W.; Beringer, T.R.O.; Kernohan, G.; Orr, J.; Dunlop, L.; Murray, L.J. Factors affecting adherence to use of hip protectors amongst residents of nursing homes—A correlation study. Int. J. Nurs. Stud. 2007, 44, 672–686. [Google Scholar] [CrossRef] [PubMed]
- Son, G.-R.; Therrien, B.; Whall, A. Implicit Memory and Familiarity Among Elders with Dementia. J. Nurs. Scholarsh. 2002, 34, 263–267. [Google Scholar] [CrossRef]
- Korall, A.M.; Feldman, F.; Scott, V.J.; Wasdell, M.; Gillan, R.; Ross, D.; Thompson-Franson, T.; Leung, P.; Lin, L. Facilitators of and barriers to hip protector acceptance and adherence in long-term care facilities: A systematic review. J. Am. Med. Dir. Assoc. 2015, 16, 185–193. [Google Scholar] [CrossRef]
- Guerdoux, E.; Dressaire, D.; Martin, S.; Adam, S.; Brouillet, D. Habit and Recollection in Healthy Aging, Mild Cognitive Impairment, and Alzheimer’s Disease. Neuropsychology 2012, 26, 517–533. [Google Scholar] [CrossRef]
- Ang, Y.H.; Au, S.Y.; Yap, L.K.; Ee, C.H. Functional decline of the elderly in a nursing home. Singap. Med. J. 2006, 47, 219–224. Available online: http://www.smj.org.sg/sites/default/files/4703/4703a6.pdf (accessed on 1 November 2023).
- Hubacher, M.; Wettstein, A. Acceptance of hip protectors for hip fracture prevention in nursing homes. Osteoporos. Int. 2001, 12, 794–799. [Google Scholar] [CrossRef] [PubMed]
- Lally, P.; van Jaarsveld, C.H.M.; Potts, H.W.W.; Wardle, J. How are habits formed: Modelling habit formation in the real world. Eur. J. Soc. Psychol. 2010, 40, 998–1010. [Google Scholar] [CrossRef]
- Love, W.E.; Nedorost, S.T. Fabric preferences of atopic dermatitis patients. Dermatitis 2009, 20, 29–33. Available online: https://pubmed.ncbi.nlm.nih.gov/19321117/ (accessed on 1 November 2023). [CrossRef]

| Group A (n = 8) | Group B (n = 7) | p | |
|---|---|---|---|
| Age, mean (±SD) | 81.4 (±10.9) | 77.0 (±9.1) | 0.256 |
| Gender (Male), n (%) | 8 (100%) | 7 (100%) | 1.000 |
| Ethnicity (Chinese), n (%) | 8 (100%) | 5 (71.4%) | 0.398 |
| Ethnicity (Malay), n (%) | 0 (0%) | 2 (28.6%) | 0.571 |
| Have ≥2 chronic health conditions, n (%) | 8 (100%) | 7 (100%) | 1.000 |
| AMT, mean (±SD) | 3.9 (±3.0) | 8.6 (±2.0) | 0.0001 |
| TUG, mean (±SD) | 26.0 s (±16.2 s) | 14.9 s (±21.3 s) | 0.341 |
| MBI, mean (±SD) | 80.9 (±19.2) | 72.7 (±15.3) | 0.383 |
| History of falls in the past 6 months, n (%) | 3 (37.55%) | 0 (0%) | 0.040 |
| Independent walking, n (%) | 7 (87.5%) | 3 (42.9%) | 0.264 |
| Wheelchair bound, n (%) | 1 (12.5%) | 4 (57.1%) | 0.398 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, T.; Lim, Y.V.; Wee, L.S.X.; Tan, Y.J.S.; Xue, A.L. The Usability of Hip Protectors: A Mixed-Method Study from the Perspectives of Singapore Nursing Home Care Staff. J. Ageing Longev. 2024, 4, 359-372. https://doi.org/10.3390/jal4040026
Xu T, Lim YV, Wee LSX, Tan YJS, Xue AL. The Usability of Hip Protectors: A Mixed-Method Study from the Perspectives of Singapore Nursing Home Care Staff. Journal of Ageing and Longevity. 2024; 4(4):359-372. https://doi.org/10.3390/jal4040026
Chicago/Turabian StyleXu, Tianma, Yu Venedict Lim, Lynn Shi Xuan Wee, Yong Jean Shina Tan, and Agnes Lishan Xue. 2024. "The Usability of Hip Protectors: A Mixed-Method Study from the Perspectives of Singapore Nursing Home Care Staff" Journal of Ageing and Longevity 4, no. 4: 359-372. https://doi.org/10.3390/jal4040026
APA StyleXu, T., Lim, Y. V., Wee, L. S. X., Tan, Y. J. S., & Xue, A. L. (2024). The Usability of Hip Protectors: A Mixed-Method Study from the Perspectives of Singapore Nursing Home Care Staff. Journal of Ageing and Longevity, 4(4), 359-372. https://doi.org/10.3390/jal4040026







