Abstract
The global population has been gradually aging over the past few decades, with a growing proportion of people aged 65 years or older. Simultaneously, the medical profession has shifted towards promoting the concept of “positive” gerontology, emphasizing healthy aging. In this context, we investigated the trends in pathological specimen submissions from patients aged 85 or older over ten years at a single center. We observed a nearly two-fold increase in submissions during 2015–2019 compared to 2010–2014, out of proportion to the change in the fraction of older adults in the population, suggesting a changing attitude towards medical care in these older patients. Dermatologic samples were the main driver of growth, followed by gastrointestinal and urinary tract samples. However, other samples, like breast and lung, did not significantly increase. Although further research is needed to understand the implications of increasing invasive procedures in the oldest old, a noteworthy trend has emerged towards increased and more active healthcare for this population. Healthcare providers and administrators should be prepared for a continued rise in invasive interventions in this age group.
1. Introduction
Over the past few decades, the world’s population has gradually grown older, due to a combination of longer lifespans and declining fertility rates. The share of the global population aged 65 years or older has grown from 6% in 1990 to 10% in 2022, and is projected to continue to increase to 16% in 2050 [1]. At the same time, the medical profession has seen a change in attitude towards the aging process. Conservative literature that viewed aging as primarily characterized by cognitive and physical decline has been supplanted by a new wave of publications promoting the concept of successful, healthy, and productive aging (a development which has been termed “positive” gerontology) [2]. This increasing emphasis on health in old age, coupled with the development of minimally invasive procedures for treating conditions that once required major surgery, are resulting in increased surgical interventions among the older population [3,4,5]. However, increasing age is still associated with increasing procedure-related morbidity and mortality, and uncertainty remains in many cases regarding the balance of the risk and benefit of various medical interventions in this age group [6,7,8].
While debates regarding the risks and benefits of invasive procedures in older patients continue, it is of interest to examine what effect the increase in the number of elderly patients and the changing attitude towards this population is having in the real world. This effect is expected to be reflected in, among others, the number and type of samples submitted for pathological examination from elderly patients. We therefore studied samples submitted for pathological analysis from patients aged 85 years and older over a period of 10 years in a single center, delineating time trends across multiple medical disciplines in this older age group.
2. Materials and Methods
This was a single-center retrospective study carried out at the pathology institute of the Hadassah Medical Center (Jerusalem, Israel). Patient and pathology data retrieval from electronic medical records was approved by the local institutional review board. All samples (including biopsies and cytological and surgical specimens) of patients aged 85 or older between the years 2010 and 2019 were included.
Sample anonymization was done prior to data analysis by an independent pathology institute employee. All statistical analyses were performed using R software version 3.6.3 and GraphPad Prism version 9.5.1. Samples were classified as benign or malignant and by tissue origin (e.g., lung, gastrointestinal tract, breast, etc.). Linear regression was used to examine the relationship between the year and the number of pathological specimens submitted. Analysis of covariance (ANCOVA) was used to compare time trends between groups. Student’s t-test was used to compare the number of pathological specimens submitted during the first 5 years (2010–2014) of the examined period to the number of specimens submitted during the last 5 years (2015–2019), in total and in prespecified subgroups, with adjustment for multiple comparisons according to the Benjamini–Hochberg false discovery rate (FDR) procedure [9].
3. Results
From 2010 to 2019, 3797 specimens were obtained from patients aged over 85 years. After excluding samples from patients with a documented age over 110 (due to a likely typing error), 3549 tissue samples from 1446 patients were included in the study. The median age of the patients was 89 years (range, 85–99). A total of 52.9% (n = 1877) of samples were obtained from female patients and 47.1% (n = 1672) from male patients.
When compared to the years 2010–2014, the average annual number of tissue samples obtained from patients over 85 years old between the years 2015 and 2019 increased nearly two-fold, from 253 (±51) to 457 (±131) (Table 1), compared to an increase of only approximately 25%—from 24,542 (±1007) per year to 30,199 (±3174)—in the general number of samples (Figure 1A).

Table 1.
Pathology samples from patients over 85 years of age: 2010–2014 vs. 2015–2019, by diagnosis (malignant vs. benign), procedure type (surgical vs. biopsy), and tissue of origin; p-value = false discovery rate-adjusted p-values; avg. = average; yr. = year; SD = standard deviation.
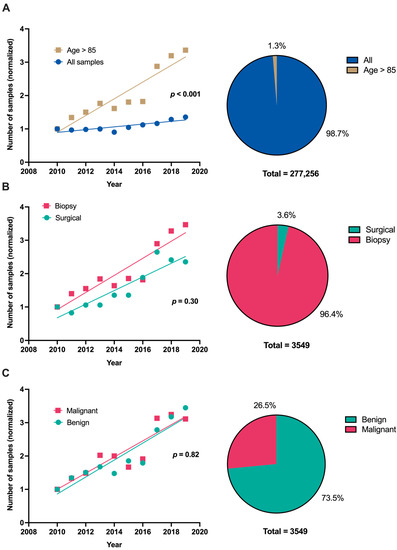
Figure 1.
(A). Number of pathological samples per year, normalized to the number of samples in the year 2010, from all patients and from patients >85 years of age, highlighting the disproportionate increase in the older age group (left); fraction of samples derived from patients above and below 85 years of age across the entire 10-year period (right). (B). Number of pathological samples per year, normalized to the number of samples in the year 2010, derived from biopsies or surgical procedures in patients >85 years of age, showing a similar trend for both sample types (left); proportion of samples derived from surgical resections and biopsies across the entire 10-year period (right). (C). Number of pathological samples per year, normalized to the number of samples in the year 2010, resulting in malignant or benign diagnoses in patients >85 years of age, showing aligned yearly trends (left); proportion of samples resulting in malignant and benign diagnoses across the entire 10-year period (right).
Of all the samples from older people, 7.7% (±1.5%) were surgical resections. This percentage remained stable over the study period, with a proportionate increase in both surgical and biopsy samples (Table 1 and Figure 1B). Of the 3549 samples collected, 26.7% (±2.5%) resulted in malignant diagnoses. The proportion of malignant and benign diagnoses also remained stable over the study period, despite the substantial increase in total sample volume (Table 1 and Figure 1C).
Of the categories with 50 or more samples, four showed a statistically significant increase in the number of submitted specimens (Figure 2A)—skin, upper gastrointestinal (GI) tract, lower GI tract, and prostate. The remaining categories (bone marrow, breast, lung, head and neck, soft tissue, and urinary tract) also showed an increasing trend, which did not reach statistical significance.
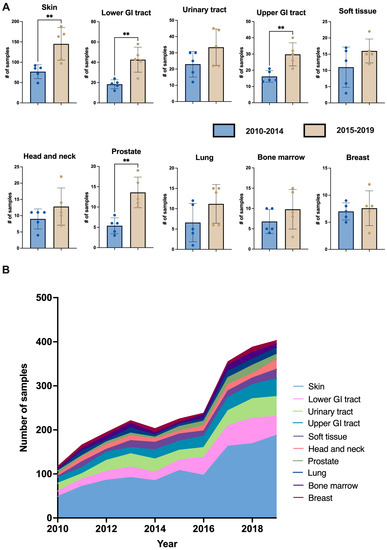
Figure 2.
(A). Number of pathological samples per year from patients over 85 years of age in the years 2010–2014 vs. 2015–2019, according to tissue of origin. (B). Number of pathological samples per year from patients over 85 years of age according to tissue of origin, showing the relative contribution of each type of sample to the overall rising trend. ** p < 0.01.
The samples from the upper GI tract were nearly all derived from endoscopic rather than surgical procedures (227/230, 99%), and rarely resulted in malignant diagnoses (17/230, 7%). The lower GI tract samples were in comparison more commonly the result of surgical resections (67/305, 22%) and more commonly resulted in malignant diagnoses (72/305, 24%).
Skin samples were the most frequently collected specimens, accounting for 31.1% (±1.8%) of all tissue samples. This percentage remained relatively stable over the study period (ranging from 28% to 34.4%; Figure 2B). Nearly half (43.5 ± 5.3%) of skin samples resulted in a diagnosis of non-melanoma skin cancer (squamous or basal cell carcinomas), with an approximately equal proportion of squamous and basal cell carcinomas (an average of 53.1 ± 5.7% squamous cell carcinomas). Correspondingly, non-melanoma skin cancer was the most common malignant diagnosis, accounting for 52.1% (±4.9%) of all malignant diagnoses, followed by urological malignancies (14.2 ± 2.4%), colorectal cancers (11.7 ± 6.0%), melanoma (7.4 ± 3.0%), hematological malignancies (7.0 ± 3.2%), breast (3.8 ± 2.7%), and lung (2.7 ± 1.5%).
4. Discussion
In this study we examined the trends in the provision of health care, and specifically medical interventions, among the oldest old through the lens of samples submitted for pathological analysis. In the 10 years from 2010 to 2019, the annual number of pathology specimens from patients aged 85 and above nearly doubled, outpacing the comparatively small 25% increase in the general number of pathological samples submitted annually during this same period. This disparity cannot be attributed solely to the aging of the Israeli population, as the proportion of older adults in the country has remained nearly constant from 1995 to 2020, with only a marginal 1% increase [10], nor to changes in national cancer screening guidelines, which align with those of the United States and recommend screening up to age 74 [11,12]. Therefore, the observed trend suggests a genuine shift in attitude towards medical care in older patients, with interventions once avoided and diagnostic and therapeutic procedures once reserved for younger patients now becoming part of the standard of care for this older age group. This change in approach could be driven by medical practitioners or may reflect the improved health status of today’s oldest old when compared to previous generations [13,14].
It is important to note the discrepancy between the proportion of male and female patients in our study to that of the known gender distribution in this age group. There were slightly more pathological specimens obtained from male patients than from female patients, even though women comprise a substantially larger proportion (approximately 60%) of the population above 85 years of age [10,15]. This is in line with previously published data concerning gender bias and may reflect women’s lower priority in the household as well as an unintentional discrimination in health practitioners’ willingness to perform procedures in women in this age group [16].
Nearly a third of the pathological samples were of dermatologic origin, with almost half of these resulting in a malignant diagnosis. The proportion of squamous to basal cell carcinomas was nearly equal, in contrast to the predominance of basal cell carcinomas in younger age groups [17] but consistent with previously reported data from older patients [18]. Regardless, data regarding treatment of these conditions in older age is limited [19], and the rapid growth in their incidence necessitates age-specific research to optimize care in this demographic.
It is notable that while a marked increase was seen in samples originating from the gastrointestinal and urinary tracts, other types of samples obtained through invasive procedures, most notably breast and lung specimens, did not display a significant increase. Indeed, when comparing the proportion of breast, lung, and prostate malignancies in our study to previous reports of cancer incidence in adults over 85 years of age, it was surprisingly low. Instead, melanoma, colorectal, and bladder cancers occupied a larger than expected proportion. This finding may be consistent with a greater reluctance within some medical professions to perform invasive diagnostic and therapeutic procedures in this age group. The reasons behind this heterogeneity in attitudes remain unclear.
More interventions do not necessarily equal better healthcare, especially with older age. While physicians may be tempted to assume that the benefits of certain interventions in younger patients apply to older patients as well, this is not always the case. For example, sentinel lymph node biopsy in women undergoing breast cancer surgery is of proven benefit in younger patients but has no effect on survival in women over 70 years of age [20]. As noted above, the rate of complications in nearly all invasive procedures rises with increasing age. In addition, the impact of diagnostic procedures on subsequent treatment, especially with malignant diagnoses, is in many cases modest in older patients, likely due to the more limited treatment options in this group. This is true even in the case of diagnostic procedures with a relatively low rate of complications, including renal biopsies performed in the evaluation of kidney failure [21,22,23,24,25], image-guided biopsies for suspected malignant disease [26,27], and gastrointestinal endoscopy [28,29], in which studies have shown only slightly higher rates of complications in older compared to younger patients. The increasing number of invasive interventions in older patients will warrant further studies to assess which patient characteristics are associated with a more favorable benefit to risk ratio for each type of procedure.
As our study is confined to pathological reports, we cannot make definitive conclusions about the therapeutic potential of the diagnoses, or the complications associated with the tests. In fact, an increase in pathological specimens may lead to more worries and overdiagnosis, particularly among the oldest old. Further research is needed to explore the clinical implications of our findings and to determine which type of procedures truly reflect an improvement in healthcare outcomes for this age group. It is also worth noting that our data, obtained from a single but sizeable medical center, may not reflect broader trends in other settings.
5. Conclusions
In summary, our analysis of the pathological specimens from patients over 85 years of age shows a disproportionate increase in this demographic over the years 2010 to 2019. This increase is not due to changes in the proportion of this age group in the general population or the general growth in the number of annual samples. Our findings thus point to a significant trend towards increased and more comprehensive healthcare for the elderly. Importantly, our findings also highlight areas in which this trend does not hold true such as breast- and lung-related procedures. Additionally, the number of samples from women was relatively low compared to their proportion in the population. While caution in breast- and lung-related procedures in the oldest old may reflect good clinical practice, gender bias cannot be justified and warrants active intervention.
Author Contributions
Conceptualization, T.K.H. and N.P.; methodology, N.P.; data curation, T.K.H., A.H. and N.P.; writing—original draft preparation, T.K.H.; writing—review and editing, T.K.H., A.H. and N.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the Hadassah Hebrew University Medical Center (protocol code 0638-19-HMO, approved 5 March 2019).
Informed Consent Statement
Patient consent was waived due to patient anonymization.
Data Availability Statement
Data will be made available upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Population Prospects—Population Division—United Nations. Available online: https://population.un.org/wpp/ (accessed on 31 August 2021).
- Johnson, K.J.; Mutchler, J.E. The Emergence of a Positive Gerontology: From Disengagement to Social Involvement. Gerontologist 2014, 54, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Oksuzyan, A.; Jeune, B.; Juel, K.; Vaupel, J.W.; Christensen, K. Changes in Hospitalisation and Surgical Procedures among the Oldest-Old: A Follow-up Study of the Entire Danish 1895 and 1905 Cohorts from Ages 85 to 99 Years. Age Ageing 2013, 42, 476–481. [Google Scholar] [CrossRef][Green Version]
- Mandawat, A.; Mandawat, A.; Mandawat, M.K.; Tinetti, M.E. Hospitalization Rates and In-Hospital Mortality among Centenarians. Arch. Intern. Med. 2012, 172, 1179–1180. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Deng, C.; Mitchell, S.; Paine, S.-J.; Kerse, N. Retrospective Analysis of the 13-Year Trend in Acute and Elective Surgery for Patients Aged 60 Years and over at Auckland City Hospital, New Zealand. J. Epidemiol. Community Health 2020, 74, 42–47. [Google Scholar] [CrossRef]
- Berlet, M.; Weber, M.-C.; Neumann, P.-A.; Friess, H.; Reim, D. Gastrectomy for Cancer beyond Life Expectancy. A Comprehensive Analysis of Oncological Gastric Surgery in Germany between 2008 and 2018. Front. Oncol. 2022, 12, 1032443. [Google Scholar] [CrossRef]
- Turri, G.; Caliskan, G.; Conti, C.; Martinelli, L.; De Giulio, E.; Ruzzenente, A.; Guglielmi, A.; Verlato, G.; Pedrazzani, C. Impact of Age and Comorbidities on Short- and Long-Term Outcomes of Patients Undergoing Surgery for Colorectal Cancer. Front. Oncol. 2022, 12, 959650. [Google Scholar] [CrossRef]
- Gajdos, C.; Kile, D.; Hawn, M.T.; Finlayson, E.; Henderson, W.G.; Robinson, T.N. Advancing Age and 30-Day Adverse Outcomes Following Non-Emergent General Surgical Operations. J. Am. Geriatr. Soc. 2013, 61, 1608–1614. [Google Scholar] [CrossRef] [PubMed]
- Haynes, W. Benjamini–Hochberg Method. In Encyclopedia of Systems Biology; Dubitzky, W., Wolkenhauer, O., Cho, K.-H., Yokota, H., Eds.; Springer: New York, NY, USA, 2013; p. 78. ISBN 978-1-4419-9863-7. [Google Scholar]
- International Senior Citizen’s Day 2020: Selected Data on Various Topics Regarding Israeli Senior Citizens Aged 65 and Over. Available online: https://www.cbs.gov.il/en/mediarelease/Pages/2020/International-Day-of-Senior-Citizens-Day-2020.aspx (accessed on 30 July 2023).
- Shaukat, A.; Kahi, C.J.; Burke, C.A.; Rabeneck, L.; Sauer, B.G.; Rex, D.K. ACG Clinical Guidelines: Colorectal Cancer Screening 2021. Am. J. Gastroenterol. 2021, 116, 458–479. [Google Scholar] [CrossRef]
- Siu, A.L. U.S. Preventive Services Task Force Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann. Intern. Med. 2016, 164, 279–296. [Google Scholar] [CrossRef]
- Engberg, H.; Christensen, K.; Andersen-Ranberg, K.; Jeune, B. Cohort Changes in Cognitive Function among Danish Centenarians. A Comparative Study of 2 Birth Cohorts Born in 1895 and 1905. Dement. Geriatr. Cogn. Disord. 2008, 26, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Engberg, H.; Christensen, K.; Andersen-Ranberg, K.; Vaupel, J.W.; Jeune, B. Improving Activities of Daily Living in Danish Centenarians--but Only in Women: A Comparative Study of Two Birth Cohorts Born in 1895 and 1905. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 1186–1192. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roberts, A.W.; Ogunwole, S.U.; Blakeslee, L.; Rabe, M.A. The Population 65 Years and Older in the United States: 2016; US Census Bureau: Suitland, MD, USA, 2016.
- Mondal, B.; Dubey, J.D. Gender Discrimination in Health-Care Expenditure: An Analysis across the Age-Groups with Special Focus on the Elderly. Soc. Sci. Med. 2020, 258, 113089. [Google Scholar] [CrossRef] [PubMed]
- Muzic, J.G.; Schmitt, A.R.; Wright, A.C.; Alniemi, D.T.; Zubair, A.S.; Olazagasti Lourido, J.M.; Sosa Seda, I.M.; Weaver, A.L.; Baum, C.L. Incidence and Trends of Basal Cell Carcinoma and Cutaneous Squamous Cell Carcinoma: A Population-Based Study in Olmsted County, Minnesota, 2000–2010. Mayo Clin. Proc. 2017, 92, 890–898. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.H.; Chen, K.H.; Tseng, M.P.; Sun, C.C. Pattern of Skin Diseases in a Geriatric Patient Group in Taiwan: A 7-Year Survey from the Outpatient Clinic of a University Medical Center. Dermatology 2001, 203, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Lubeek, S.F.K.; van Vugt, L.J.; Aben, K.K.H.; van de Kerkhof, P.C.M.; Gerritsen, M.-J.P. The Epidemiology and Clinicopathological Features of Basal Cell Carcinoma in Patients 80 Years and Older: A Systematic Review. JAMA Dermatol. 2017, 153, 71–78. [Google Scholar] [CrossRef]
- Minami, C.A.; Bryan, A.F.; Freedman, R.A.; Revette, A.C.; Schonberg, M.A.; King, T.A.; Mittendorf, E.A. Assessment of Oncologists’ Perspectives on Omission of Sentinel Lymph Node Biopsy in Women 70 Years and Older with Early-Stage Hormone Receptor–Positive Breast Cancer. JAMA Netw. Open 2022, 5, e2228524. [Google Scholar] [CrossRef]
- Bomback, A.S.; Herlitz, L.C.; Markowitz, G.S. Renal Biopsy in the Elderly and Very Elderly: Useful or Not? Adv. Chronic Kidney Dis. 2012, 19, 61–67. [Google Scholar] [CrossRef]
- Moutzouris, D.-A.; Herlitz, L.; Appel, G.B.; Markowitz, G.S.; Freudenthal, B.; Radhakrishnan, J.; D’Agati, V.D. Renal Biopsy in the Very Elderly. Clin. J. Am. Soc. Nephrol. 2009, 4, 1073–1082. [Google Scholar] [CrossRef]
- Verde, E.; Quiroga, B.; Rivera, F.; López-Gómez, J.M. Renal Biopsy in Very Elderly Patients: Data from the Spanish Registry of Glomerulonephritis. Am. J. Nephrol. 2012, 35, 230–237. [Google Scholar] [CrossRef]
- Nair, R.; Bell, J.M.; Walker, P.D. Renal Biopsy in Patients Aged 80 Years and Older. Am. J. Kidney Dis. 2004, 44, 618–626. [Google Scholar] [CrossRef]
- Gupta, P.; Rana, D.S. Importance of Renal Biopsy in Patients Aged 60 Years and Older: Experience from a Tertiary Care Hospital. Saudi J. Kidney Dis. Transpl. 2018, 29, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Welch, B.T.; Welch, T.J.; Maus, T.P. Percutaneous Image-Guided Biopsy in an Elderly Population. J. Vasc. Interv. Radiol. 2010, 21, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.S.; Kanthapillai, P. Transthoracic Needle Biopsy for Suspected Thoracic Malignancy in Elderly Patients Using CT Guidance. Clin. Radiol. 1998, 53, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Lobo, B.; Casellas, F.; de Torres, I.; Chicharro, L.; Malagelada, J.R. Usefulness of Jejunal Biopsy in the Study of Intestinal Malabsorption in the Elderly. Rev. Esp. Enferm. Dig. 2004, 96, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Lin, O.S. Performing Colonoscopy in Elderly and Very Elderly Patients: Risks, Costs and Benefits. World J. Gastrointest. Endosc. 2014, 6, 220–226. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).