To Be Biased or Not to Be: A Play for G-Protein Coupled Receptors
Abstract
1. Introduction to G Protein-Coupled Receptors (GPCRs)
2. GPCR Signaling
3. GPCR Bias and Types of Biased Signaling
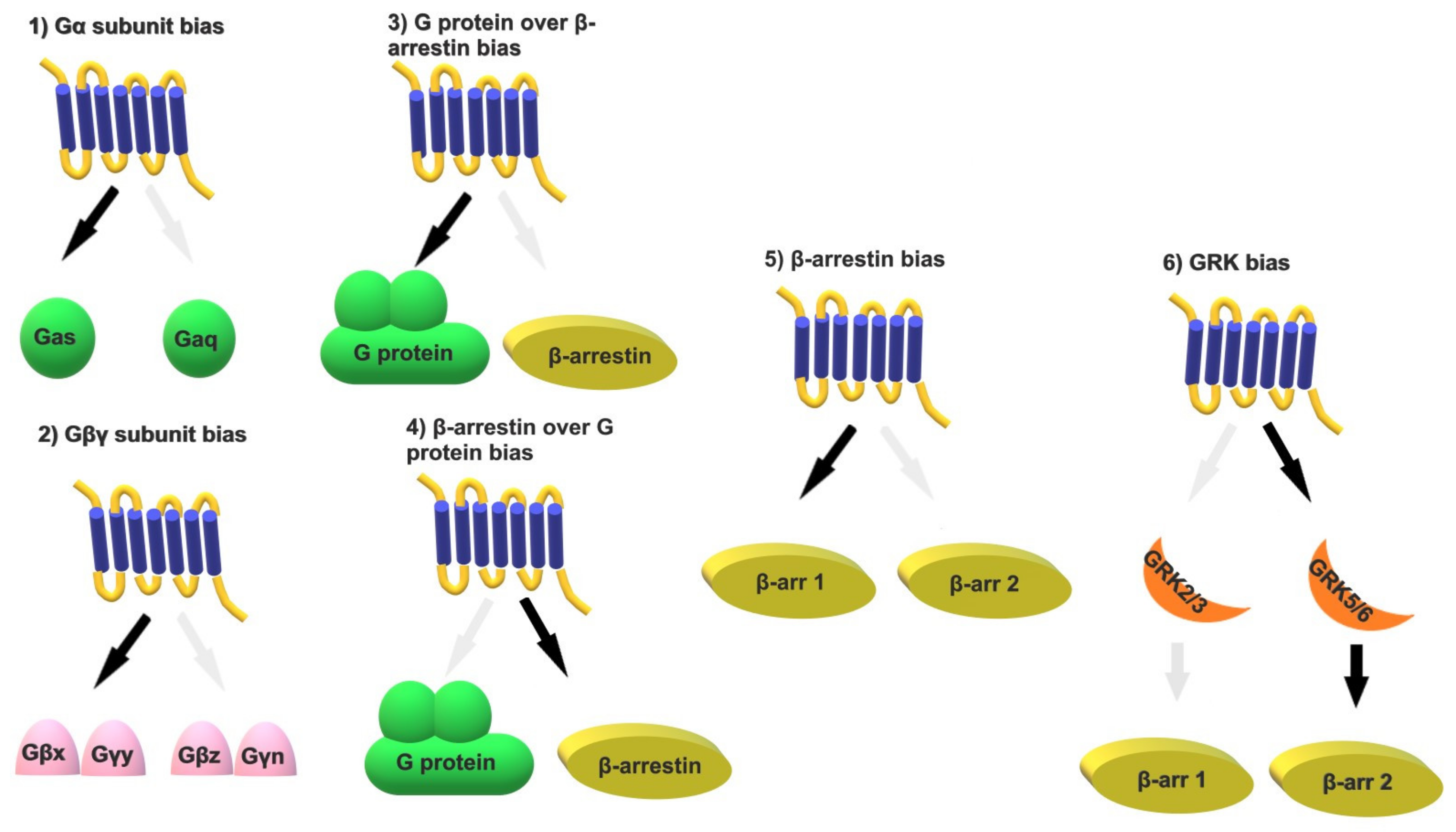
- (1)
- Gα subunit bias: A GPCR can link to more than one of the 16 Gα subunits, each of which has its own effectors and signaling molecules. One can therefore envision numerous possibilities for each receptor. An example is the protease-activated receptor 1 (PAR1). Thrombin activation of PAR1 signals through Gαq, Gα12/13, and β-arrestin 2, while the coagulation protease–activated protein C (aPC) signals through Gα12/13 and β-arrestin 2, but not Gαq [58].
- (2)
- Gβγ subunit bias: The 5 Gβ and 12 Gγ subunits form 60 possible dimer combinations that differ in their subcellular translocation and downstream signaling kinetics and efficacy [59]. A recent study supports the notion that all β-arrestin effects mediated by GRK2/3 are Gβγ-dependent, while the β-arrestin effects mediated by GRK5/6 are independent of G proteins [60]. Certain Gβγ combinations specifically affect ion channel function, and tissue-specific expression of Gβ and Gγ subunits suggests that particular subunit combinations may correspond to distinct functions in specific tissues and organs [61].
- (3)
- G protein over β-arrestin bias: G protein bias over β-arrestin has been observed with numerous endogenous or exogenous ligands, as exemplified in the following sections.
- (4)
- β-arrestin over G protein bias: The conformational patterns of the complex between the ligand, the receptor, and the β-arrestin dictate the effectors to which arrestin will bind and how it will regulate G protein signaling [62]. Examples are discussed in the following sections.
- (5)
- β-arrestin bias: By selectively silencing each β-arrestin, it has been demonstrated that β-arrestins 1 and 2 have differential affinity for different GPCRs and activate different downstream mediators [41,63]. One example is the angiotensin II type 1 receptor (AT1 R), which interacts with both β-arrestins 1 and 2. Each β-arrestin stabilizes different AT1 R conformations with distinct agonist-binding affinities, suggesting that it may be possible to design AT1R-biased agonists that selectively recruit β-arrestin 1 or 2 [64]. However, the functional consequence of such an approach remains unclear.
- (6)
- GRK bias: It is known that several phosphate groups must be attached to the receptor to promote β-arrestin recruitment. Variability in receptor–ligand conformations leads to the selective recruitment of specific GRKs, resulting in distinct phosphorylation patterns, known as phosphorylation “barcodes”, and unique downstream signaling pathways [35,36,65]. Recent studies on the AT1R have shown that upon binding of angiotensin II, the recruitment of β-arrestin depends on both GRK2/3 and GRK5/6; upon binding of the β-arrestin-biased ligand TRV027, recruitment of β-arrestin depends solely on GRK5/6 [66]. GRK-specific phosphorylation “barcodes” can differentially recruit β-arrestin 1 and β-arrestin 2, activating distinct β-arrestin-mediated signaling pathways [67]. Other than acting as intermediates between G proteins and β-arrestins, GRKs may also mediate GPCR-independent signaling. This notion is supported by a recent study describing the development of GRK2-biased β2 adrenergic receptor partial agonists that increase glucose tolerance in preclinical models of diabetes and obesity, without significant cardiovascular effects [68].
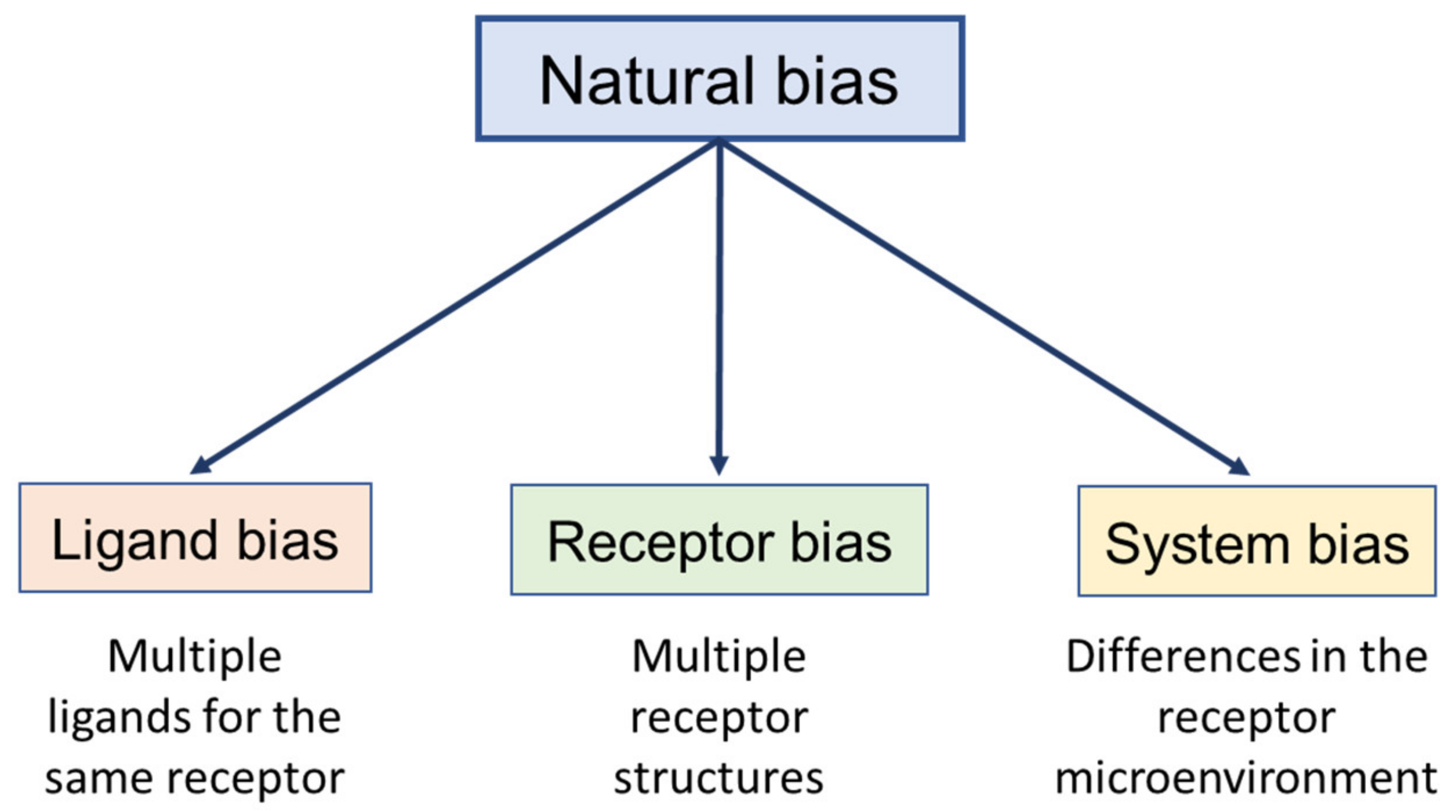
3.1. Natural (Intrinsic or Physiological) Bias
3.2. Synthetic Ligand Bias
3.3. Receptor Bias
| Mechanism | Bias | Receptor(s) | Potential Implication | Ligand(s) | Refs. |
|---|---|---|---|---|---|
| Receptor mutations/SNPs | β-arrestin over G protein | FSHR (A189V) | Sub/infertility (men/women) | Unknown | [81] |
| V2R (R137H) | Familial nephrogenic diabetes insipidus | Unknown | [149,150] | ||
| CaS (several) | Bartter syndrome type V, familial hypocalciuric hypercalcemia, and autosomal dominant hypercalcemia | Unknown | [151,152,153] | ||
| GLP1R (T149M) | Disturbed glucose metabolism | Allosteric modulator | [154,155] | ||
| MC3R (several) | Obesity | Unknown | [156] | ||
| G protein over β-arrestin | CaS (several) | Bartter syndrome type V, familial hypocalciuric hypercalcemia, and autosomal dominant hypercalcemia | Unknown | [151,152,153] | |
| MC3R (several) | Obesity | Unknown | [156] | ||
| Receptor di/oligomerization | Gs over Gi | A1/A2A receptor heterodimer | Inhibition of A1 signaling | High adenosine concentrations | [158] |
| β-arrestin over G protein | μ-opioid/δ-opioid receptor heterodimer | Morphine tolerance | Prolonged morphine treatment, CYM51010 | [160,161] | |
| G protein over β-arrestin | PAF receptor di/oligomers | Decreased agonist-induced internalization | PAF | [162] | |
| β-arrestin over G protein | ACKR3/CXCR4 | Inhibition of CXCL12-induced chemotaxis of lymphocytes, platelet activation, and thrombus formation Enhancement of colorectal tumorigenesis | CXCL12 dimers | [164,165] |
3.4. System Bias
| Reason | Bias | Location | Receptor | Ligand(s)/Effect | Refs. |
|---|---|---|---|---|---|
| Receptor density | β-arrestin over G protein | Cell membrane | D2 dopamine receptor | Aripiprazole at high receptor levels Brexpiprazole at low receptor levels Cariprazine at all receptor levels | [175] |
| G protein over β-arrestin | Cell membrane | D2 dopamine receptor | Aripiprazole at low receptor levels Brexpiprazole at high receptor levels | [175] | |
| Subcellular receptor localization | Unknown | Golgi | β-adrenergic receptor in cardiac myocytes | Cell-permeable metoprolol to prevent cardiac hypertrophy | [176] |
| β-arrestin over G protein | 5-HT2A receptors in cortical neurons | Lipophilic psychedelic substances promote neuroplasticity | [178] | ||
| G protein over β-arrestin | δ-opioid receptor | Distinct effectors and signaling responses | [183] | ||
| Unknown | Endosomes | NK1R in spinal neurons | Cell-permeable antagonists as effective analgesics | [177] | |
| CXCR3 | Biased signaling depending on the chemokine | [181,182] | |||
| Mitochondrial membrane | CB1 receptor in the hippocampus | Related to cannabinoid-induced amnesia | [180] | ||
| Nuclear membrane/nucleus | Neural mGluR5 | Cell-permeable antagonists for greater analgesia | [179] | ||
| G protein expression levels | ↑ Gαolf | Striatum | D1 dopamine receptor | Tavapadon in Parkinson’s | [173] |
| ↑ Gαs | Prefrontal cortex | D1 dopamine receptor | Tavapadon, but does not affect cognitive function | [173] | |
| β-arrestin expression levels | ↑ β-arrestin 2 | Prefrontal cortex | β-arrestin 2-biased D2 receptor ligands | Agonistic activity | [170,171,172] |
| ↓ β-arrestin 2 | Striatum | β-arrestin 2-biased D2 receptor ligands | Antagonistic activity | [170,171,172] |
4. Limitations Associated with Ligand Bias Investigation
5. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 5-HT2A | 5-hydroxytryptamine 2A |
| AC | Adenylyl cyclase |
| ACKRs | Atypical chemokine receptors |
| AP2 | Adaptive protein 2 |
| aPC | Activated protein C |
| AR | Adrenergic receptor |
| AT1R | Angiotensin II type 1 receptor |
| BRET | Bioluminescence resonance energy transfer |
| CaS | Calcium sensing |
| CB1 | Cannabinoid 1 |
| CCR | CC chemokine receptor |
| CNS | Central nervous system |
| CXCR | CXC chemokine receptor |
| EGFR | Epidermal growth factor receptor |
| ERK | Extracellular signal-regulated kinase |
| FRET | Fluorescence resonance energy transfer |
| FSHR | Follicle-stimulating hormone receptor |
| GalR2 | Galanin receptor 2 |
| GLP1 | Glucagon-like peptide 1 |
| GPCRs | G protein-coupled receptors |
| GRKs | GPCR kinases |
| HCA3 | Hydroxycarboxylic acid receptor 3 |
| LSD | Lysergic acid diethylamide |
| MC4R | Melanocortin−4 receptor |
| NK1R | Neurokinin 1 receptor |
| NTSR1 | Neurotensin receptor 1 |
| PAF | Platelet activation factor |
| PAR1 | Protease-activated receptor 1 |
| SNP | Single-nucleotide polymorphism |
| V2R | Vasopressin receptor 2 |
References
- Alexander, S.P.H.; Christopoulos, A.; Davenport, A.P.; Kelly, E.; Mathie, A.A.; Peters, J.A.; Veale, E.L.; Armstrong, J.F.; Faccenda, E.; Harding, S.D.; et al. The Concise Guide to PHARMACOLOGY 2023/24: G protein-coupled receptors. Br. J. Pharmacol. 2023, 180, S23–S144. [Google Scholar] [CrossRef] [PubMed]
- Slosky, L.M.; Caron, M.G.; Barak, L.S. Biased Allosteric Modulators: New Frontiers in GPCR Drug Discovery. Trends Pharmacol. Sci. 2021, 42, 283–299. [Google Scholar] [CrossRef] [PubMed]
- Schoneberg, T.; Liebscher, I. Mutations in G Protein-Coupled Receptors: Mechanisms, Pathophysiology and Potential Therapeutic Approaches. Pharmacol. Rev. 2021, 73, 89–119. [Google Scholar] [CrossRef] [PubMed]
- Boutin, J.A.; Legros, C. The five dimensions of receptor pharmacology exemplified by melatonin receptors: An opinion. Pharmacol. Res. Perspect. 2020, 8, e00556. [Google Scholar] [CrossRef]
- Shimada, I.; Ueda, T.; Kofuku, Y.; Eddy, M.T.; Wuthrich, K. GPCR drug discovery: Integrating solution NMR data with crystal and cryo-EM structures. Nat. Rev. Drug Discov. 2019, 18, 59–82. [Google Scholar] [CrossRef]
- Odoemelam, C.S.; Percival, B.; Wallis, H.; Chang, M.W.; Ahmad, Z.; Scholey, D.; Burton, E.; Williams, I.H.; Kamerlin, C.L.; Wilson, P.B. G-Protein coupled receptors: Structure and function in drug discovery. RSC Adv. 2020, 10, 36337–36348. [Google Scholar] [CrossRef]
- Di Pizio, A.; Levit, A.; Slutzki, M.; Behrens, M.; Karaman, R.; Niv, M.Y. Comparing Class A GPCRs to bitter taste receptors: Structural motifs, ligand interactions and agonist-to-antagonist ratios. Methods Cell Biol. 2016, 132, 401–427. [Google Scholar] [CrossRef]
- Xu, C.; Wang, Y.; Ni, H.; Yao, M.; Cheng, L.; Lin, X. The role of orphan G protein-coupled receptors in pain. Heliyon 2024, 10, e28818. [Google Scholar] [CrossRef]
- Singh, A.; Shadangi, S.; Rana, S. G-protein coupled receptors in neuroinflammation, neuropharmacology, and therapeutics. Biochem. Pharmacol. 2025, 242, 117301. [Google Scholar] [CrossRef]
- Crilly, S.E.; Puthenveedu, M.A. Compartmentalized GPCR Signaling from Intracellular Membranes. J. Membr. Biol. 2021, 254, 259–271. [Google Scholar] [CrossRef]
- Bradley, S.J.; Tobin, A.B. Design of Next-Generation G Protein-Coupled Receptor Drugs: Linking Novel Pharmacology and In Vivo Animal Models. Annu. Rev. Pharmacol. Toxicol. 2016, 56, 535–559. [Google Scholar] [CrossRef]
- Wacker, D.; Stevens, R.C.; Roth, B.L. How Ligands Illuminate GPCR Molecular Pharmacology. Cell 2017, 170, 414–427. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Martin, B.; Brenneman, R.; Luttrell, L.M.; Maudsley, S. Allosteric modulators of G protein-coupled receptors: Future therapeutics for complex physiological disorders. J. Pharmacol. Exp. Ther. 2009, 331, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, M.F.; Tampé, R. Ligand-independent receptor clustering modulates transmembrane signaling: A new paradigm. Trends Biochem. Sci. 2023, 48, 156–171. [Google Scholar] [CrossRef] [PubMed]
- Marti-Solano, M.; Crilly, S.E.; Malinverni, D.; Munk, C.; Harris, M.; Pearce, A.; Quon, T.; Mackenzie, A.E.; Wang, X.; Peng, J.; et al. Combinatorial expression of GPCR isoforms affects signalling and drug responses. Nature 2020, 587, 650–656, Correction in Nature 2020, 588, E24. [Google Scholar] [CrossRef]
- Nagi, K.; Onaran, H.O. Biased agonism at G protein-coupled receptors. Cell. Signal. 2021, 83, 109981. [Google Scholar] [CrossRef]
- Sriram, K.; Insel, P.A. G Protein-Coupled Receptors as Targets for Approved Drugs: How Many Targets and How Many Drugs? Mol. Pharmacol. 2018, 93, 251–258. [Google Scholar] [CrossRef]
- Mohammad Nezhady, M.A.; Rivera, J.C.; Chemtob, S. Location Bias as Emerging Paradigm in GPCR Biology and Drug Discovery. iScience 2020, 23, 101643. [Google Scholar] [CrossRef]
- Yang, H.; Wang, Y.; Liu, W.; He, T.; Liao, J.; Qian, Z.; Zhao, J.; Cong, Z.; Sun, D.; Liu, Z.; et al. Genome-wide pan-GPCR cell libraries accelerate drug discovery. Acta Pharm. Sin. B 2024, 14, 4296–4311. [Google Scholar] [CrossRef]
- Campbell, A.P.; Smrcka, A.V. Targeting G protein-coupled receptor signalling by blocking G proteins. Nat. Rev. Drug Discov. 2018, 17, 789–803. [Google Scholar] [CrossRef]
- Wang, J.; Gareri, C.; Rockman, H.A. G-Protein-Coupled Receptors in Heart Disease. Circ. Res. 2018, 123, 716–735, Correction in Circ. Res. 2018, 123, e34. [Google Scholar] [CrossRef]
- Calebiro, D.; Miljus, T.; O’Brien, S. Endomembrane GPCR signaling: 15 years on, the quest continues. Trends Biochem. Sci. 2025, 50, 46–60. [Google Scholar] [CrossRef] [PubMed]
- Lorenzen, E.; Ceraudo, E.; Berchiche, Y.A.; Rico, C.A.; Fürstenberg, A.; Sakmar, T.P.; Huber, T. G protein subtype-specific signaling bias in a series of CCR5 chemokine analogs. Sci. Signal. 2018, 11, eaao6152. [Google Scholar] [CrossRef] [PubMed]
- Littmann, T.; Buschauer, A.; Bernhardt, G. Split luciferase-based assay for simultaneous analyses of the ligand concentration- and time-dependent recruitment of β-arrestin2. Anal. Biochem. 2019, 573, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Suno, R. Exploring Diverse Signaling Mechanisms of G Protein-Coupled Receptors through Structural Biology. J. Biochem. 2024, 175, 357–365. [Google Scholar] [CrossRef]
- Horioka, M.; Ceraudo, E.; Lorenzen, E.; Sakmar, T.P.; Huber, T. Purinergic Receptors Crosstalk with CCR5 to Amplify Ca2+ Signaling. Cell Mol. Neurobiol. 2021, 41, 1085–1101. [Google Scholar] [CrossRef]
- Liu, S.; Anderson, P.J.; Rajagopal, S.; Lefkowitz, R.J.; Rockman, H.A. G Protein-Coupled Receptors: A Century of Research and Discovery. Circ. Res. 2024, 135, 174–197. [Google Scholar] [CrossRef]
- Raehal, K.M.; Bohn, L.M. β-arrestins: Regulatory role and therapeutic potential in opioid and cannabinoid receptor-mediated analgesia. Handb. Exp. Pharmacol. 2014, 219, 427–443. [Google Scholar] [CrossRef]
- Caron, M.G.; Barak, L.S. A Brief History of the β-Arrestins. Methods Mol. Biol. 2019, 1957, 3–8. [Google Scholar] [CrossRef]
- Vilardaga, J.P.; Jean-Alphonse, F.G.; Gardella, T.J. Endosomal generation of cAMP in GPCR signaling. Nat. Chem. Biol. 2014, 10, 700–706. [Google Scholar] [CrossRef]
- Kahsai, A.W.; Shah, K.S.; Shim, P.J.; Lee, M.A.; Shreiber, B.N.; Schwalb, A.M.; Zhang, X.; Kwon, H.Y.; Huang, L.Y.; Soderblom, E.J.; et al. Signal transduction at GPCRs: Allosteric activation of the ERK MAPK by β-arrestin. Proc. Natl. Acad. Sci. USA 2023, 120, e2303794120. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Tesmer, J.J.G. G protein-coupled receptor interactions with arrestins and GPCR kinases: The unresolved issue of signal bias. J. Biol. Chem. 2022, 298, 102279. [Google Scholar] [CrossRef] [PubMed]
- Maharana, J.; Sarma, P.; Yadav, M.K.; Saha, S.; Singh, V.; Saha, S.; Chami, M.; Banerjee, R.; Shukla, A.K. Structural snapshots uncover a key phosphorylation motif in GPCRs driving β-arrestin activation. Mol. Cell 2023, 83, 2091–2107.e7. [Google Scholar] [CrossRef]
- Perry-Hauser, N.A.; Asher, W.B.; Hauge Pedersen, M.; Javitch, J.A. Assays for detecting arrestin interaction with GPCRs. Methods Cell Biol. 2021, 166, 43–65. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi-Agnihotri, H.; Chaturvedi, M.; Baidya, M.; Stepniewski, T.M.; Pandey, S.; Maharana, J.; Srivastava, A.; Caengprasath, N.; Hanyaloglu, A.C.; Selent, J.; et al. Distinct phosphorylation sites in a prototypical GPCR differently orchestrate β-arrestin interaction, trafficking, and signaling. Sci. Adv. 2020, 6, eabb8368. [Google Scholar] [CrossRef]
- Kaya, A.I.; Perry, N.A.; Gurevich, V.V.; Iverson, T.M. Phosphorylation barcode-dependent signal bias of the dopamine D1 receptor. Proc. Natl. Acad. Sci. USA 2020, 117, 14139–14149. [Google Scholar] [CrossRef]
- Madhu, M.K.; Debroy, A.; Murarka, R.K. Molecular Insights into Phosphorylation-Induced Allosteric Conformational Changes in a β2-Adrenergic Receptor. J. Phys. Chem. B 2022, 126, 1917–1932. [Google Scholar] [CrossRef]
- Heo, E.H.; Abrol, R. Thermodynamic role of receptor phosphorylation barcode in cannabinoid receptor desensitization. Biochem. Biophys. Res. Commun. 2025, 743, 151100. [Google Scholar] [CrossRef]
- Gurevich, E.V.; Tesmer, J.J.; Mushegian, A.; Gurevich, V.V. G protein-coupled receptor kinases: More than just kinases and not only for GPCRs. Pharmacol. Ther. 2012, 133, 40–69. [Google Scholar] [CrossRef]
- Li, L.; Homan, K.T.; Vishnivetskiy, S.A.; Manglik, A.; Tesmer, J.J.; Gurevich, V.V.; Gurevich, E.V. G Protein-coupled Receptor Kinases of the GRK4 Protein Subfamily Phosphorylate Inactive G Protein-coupled Receptors (GPCRs). J. Biol. Chem. 2015, 290, 10775–10790. [Google Scholar] [CrossRef]
- Kee, T.R.; Khan, S.A.; Neidhart, M.B.; Masters, B.M.; Zhao, V.K.; Kim, Y.K.; McGill Percy, K.C.; Woo, J.A. The multifaceted functions of β-arrestins and their therapeutic potential in neurodegenerative diseases. Exp. Mol. Med. 2024, 56, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Moo, E.V.; van Senten, J.R.; Brauner-Osborne, H.; Moller, T.C. Arrestin-Dependent and -Independent Internalization of G Protein-Coupled Receptors: Methods, Mechanisms, and Implications on Cell Signaling. Mol. Pharmacol. 2021, 99, 242–255. [Google Scholar] [CrossRef] [PubMed]
- Gurevich, V.V.; Chen, Q.; Gurevich, E.V. Arrestins: Introducing Signaling Bias Into Multifunctional Proteins. Prog. Mol. Biol. Transl. Sci. 2018, 160, 47–61. [Google Scholar] [CrossRef] [PubMed]
- Gesty-Palmer, D.; Luttrell, L.M. Refining efficacy: Exploiting functional selectivity for drug discovery. Adv. Pharmacol. 2011, 62, 79–107. [Google Scholar] [CrossRef]
- Nogueras-Ortiz, C.; Yudowski, G.A. The Multiple Waves of Cannabinoid 1 Receptor Signaling. Mol. Pharmacol. 2016, 90, 620–626. [Google Scholar] [CrossRef]
- Roth, B.L.; Chuang, D.M. Multiple mechanisms of serotonergic signal transduction. Life Sci. 1987, 41, 1051–1064. [Google Scholar] [CrossRef]
- Kenakin, T. Agonist-receptor efficacy. II. Agonist trafficking of receptor signals. Trends Pharmacol. Sci. 1995, 16, 232–238. [Google Scholar] [CrossRef]
- Luttrell, L.M. Minireview: More than just a hammer: Ligand “bias” and pharmaceutical discovery. Mol. Endocrinol. 2014, 28, 281–294. [Google Scholar] [CrossRef]
- Guven, B.; Onay-Besikci, A. Past and present of beta arrestins: A new perspective on insulin secretion and effect. Eur. J. Pharmacol. 2023, 956, 175952. [Google Scholar] [CrossRef]
- Chen, A.; Su, C.; Zhang, Z.; Zhang, H. Cryo-EM Structures and AlphaFold3 Models of Histamine Receptors Reveal Diverse Ligand Binding and G Protein Bias. Pharmaceuticals 2025, 18, 292. [Google Scholar] [CrossRef]
- Hilger, D. The role of structural dynamics in GPCR-mediated signaling. FEBS J. 2021, 288, 2461–2489. [Google Scholar] [CrossRef] [PubMed]
- Wright, S.C.; Bouvier, M. Illuminating the complexity of GPCR pathway selectivity-advances in biosensor development. Curr. Opin. Struct. Biol. 2021, 69, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Olsen, R.H.J.; English, J.G. Advancements in G protein-coupled receptor biosensors to study GPCR-G protein coupling. Br. J. Pharmacol. 2023, 180, 1433–1443. [Google Scholar] [CrossRef] [PubMed]
- Eiger, D.S.; Hicks, C.; Gardner, J.; Pham, U.; Rajagopal, S. Location bias: A “Hidden Variable” in GPCR pharmacology. Bioessays 2023, 45, e2300123. [Google Scholar] [CrossRef]
- Grundmann, M.; Kostenis, E. Temporal Bias: Time-Encoded Dynamic GPCR Signaling. Trends Pharmacol. Sci. 2017, 38, 1110–1124. [Google Scholar] [CrossRef]
- Kayser, C.; Melkes, B.; Derieux, C.; Bock, A. Spatiotemporal GPCR signaling illuminated by genetically encoded fluorescent biosensors. Curr. Opin. Pharmacol. 2023, 71, 102384. [Google Scholar] [CrossRef]
- Morales, P.; Scharf, M.M.; Bermudez, M.; Egyed, A.; Franco, R.; Hansen, O.K.; Jagerovic, N.; Jakubik, J.; Keseru, G.M.; Kiss, D.J.; et al. Progress on the development of Class A GPCR-biased ligands. Br. J. Pharmacol. 2025, 182, 3249–3300. [Google Scholar] [CrossRef]
- Künze, G.; Isermann, B. Targeting biased signaling by PAR1: Function and molecular mechanism of parmodulins. Blood 2023, 141, 2675–2684. [Google Scholar] [CrossRef]
- Masuho, I.; Skamangas, N.K.; Muntean, B.S.; Martemyanov, K.A. Diversity of the Gβγ complexes defines spatial and temporal bias of GPCR signaling. Cell Syst. 2021, 12, 324–337.e5. [Google Scholar] [CrossRef]
- Matthees, E.S.F.; Filor, J.C.; Jaiswal, N.; Reichel, M.; Youssef, N.; D’Uonnolo, G.; Szpakowska, M.; Drube, J.; König, G.M.; Kostenis, E.; et al. GRK specificity and Gβγ dependency determines the potential of a GPCR for arrestin-biased agonism. Commun. Biol. 2024, 7, 802. [Google Scholar] [CrossRef]
- Tennakoon, M.; Senarath, K.; Kankanamge, D.; Ratnayake, K.; Wijayaratna, D.; Olupothage, K.; Ubeysinghe, S.; Martins-Cannavino, K.; Hebert, T.E.; Karunarathne, A. Subtype-dependent regulation of Gβγ signalling. Cell. Signal. 2021, 82, 109947. [Google Scholar] [CrossRef] [PubMed]
- Wootten, D.; Christopoulos, A.; Marti-Solano, M.; Babu, M.M.; Sexton, P.M. Mechanisms of signalling and biased agonism in G protein-coupled receptors. Nat. Rev. Mol. Cell Biol. 2018, 19, 638–653. [Google Scholar] [CrossRef] [PubMed]
- Oakley, R.H.; Laporte, S.A.; Holt, J.A.; Caron, M.G.; Barak, L.S. Differential affinities of visual arrestin, beta arrestin1, and beta arrestin2 for G protein-coupled receptors delineate two major classes of receptors. J. Biol. Chem. 2000, 275, 17201–17210. [Google Scholar] [CrossRef]
- Sanni, S.J.; Hansen, J.T.; Bonde, M.M.; Speerschneider, T.; Christensen, G.L.; Munk, S.; Gammeltoft, S.; Hansen, J.L. β-Arrestin 1 and 2 stabilize the angiotensin II type I receptor in distinct high-affinity conformations. Br. J. Pharmacol. 2010, 161, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Gurevich, V.V.; Gurevich, E.V. Biased GPCR signaling: Possible mechanisms and inherent limitations. Pharmacol. Ther. 2020, 211, 107540, Correction in Pharmacol. Ther. 2020, 213, 107615. [Google Scholar] [CrossRef]
- Kawakami, K.; Yanagawa, M.; Hiratsuka, S.; Yoshida, M.; Ono, Y.; Hiroshima, M.; Ueda, M.; Aoki, J.; Sako, Y.; Inoue, A. Heterotrimeric Gq proteins act as a switch for GRK5/6 selectivity underlying β-arrestin transducer bias. Nat. Commun. 2022, 13, 487. [Google Scholar] [CrossRef]
- Chen, Q.; Schafer, C.T.; Mukherjee, S.; Wang, K.; Gustavsson, M.; Fuller, J.R.; Tepper, K.; Lamme, T.D.; Aydin, Y.; Agrawal, P.; et al. Effect of phosphorylation barcodes on arrestin binding to a chemokine receptor. Nature 2025, 643, 280–287. [Google Scholar] [CrossRef]
- Motso, A.; Pelcman, B.; Kalinovich, A.; Kahlous, N.A.; Bokhari, M.H.; Dehvari, N.; Halleskog, C.; Waara, E.; de Jong, J.; Cheesman, E.; et al. GRK-biased adrenergic agonists for the treatment of type 2 diabetes and obesity. Cell 2025, 188, 5142–5156.e23. [Google Scholar] [CrossRef]
- Kenakin, T. Biased Receptor Signaling in Drug Discovery. Pharmacol. Rev. 2019, 71, 267–315. [Google Scholar] [CrossRef]
- Gomes, I.; Sierra, S.; Lueptow, L.; Gupta, A.; Gouty, S.; Margolis, E.B.; Cox, B.M.; Devi, L.A. Biased signaling by endogenous opioid peptides. Proc. Natl. Acad. Sci. USA 2020, 117, 11820–11828. [Google Scholar] [CrossRef]
- LaVigne, J.; Keresztes, A.; Chiem, D.; Streicher, J.M. The endomorphin-1/2 and dynorphin-B peptides display biased agonism at the mu opioid receptor. Pharmacol. Rep. 2020, 72, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Thompson, G.L.; Lane, J.R.; Coudrat, T.; Sexton, P.M.; Christopoulos, A.; Canals, M. Biased Agonism of Endogenous Opioid Peptides at the μ-Opioid Receptor. Mol. Pharmacol. 2015, 88, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Shao, Z.; Shen, Q.; Yao, B.; Mao, C.; Chen, L.N.; Zhang, H.; Shen, D.D.; Zhang, C.; Li, W.; Du, X.; et al. Identification and mechanism of G protein-biased ligands for chemokine receptor CCR1. Nat. Chem. Biol. 2022, 18, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Liu, Y.; Zaidi, S.A.; Xu, L.; Zhan, Y.; Chen, A.; Guo, J.; Huang, X.P.; Roth, B.L.; Katritch, V.; et al. Structural insights into angiotensin receptor signaling modulation by balanced and biased agonists. EMBO J. 2023, 42, e112940. [Google Scholar] [CrossRef]
- Szakadáti, G.; Tóth, A.D.; Oláh, I.; Erdélyi, L.S.; Balla, T.; Várnai, P.; Hunyady, L.; Balla, A. Investigation of the fate of type I angiotensin receptor after biased activation. Mol. Pharmacol. 2015, 87, 972–981. [Google Scholar] [CrossRef]
- Galandrin, S.; Denis, C.; Boularan, C.; Marie, J.; M’Kadmi, C.; Pilette, C.; Dubroca, C.; Nicaise, Y.; Seguelas, M.H.; N’Guyen, D.; et al. Cardioprotective Angiotensin-(1-7) Peptide Acts as a Natural-Biased Ligand at the Angiotensin II Type 1 Receptor. Hypertension 2016, 68, 1365–1374. [Google Scholar] [CrossRef]
- Reyes-Alcaraz, A.; Lee, Y.N.; Yun, S.; Hwang, J.I.; Seong, J.Y. Conformational signatures in β-arrestin2 reveal natural biased agonism at a G-protein-coupled receptor. Commun. Biol. 2018, 1, 128. [Google Scholar] [CrossRef]
- Thomsen, A.R.; Hvidtfeldt, M.; Brauner-Osborne, H. Biased agonism of the calcium-sensing receptor. Cell Calcium 2012, 51, 107–116. [Google Scholar] [CrossRef]
- Peters, A.; Rabe, P.; Liebing, A.D.; Krumbholz, P.; Nordström, A.; Jäger, E.; Kraft, R.; Stäubert, C. Hydroxycarboxylic acid receptor 3 and GPR84—Two metabolite-sensing G protein-coupled receptors with opposing functions in innate immune cells. Pharmacol. Res. 2022, 176, 106047. [Google Scholar] [CrossRef]
- Peters, A.; Rabe, P.; Krumbholz, P.; Kalwa, H.; Kraft, R.; Schöneberg, T.; Stäubert, C. Natural biased signaling of hydroxycarboxylic acid receptor 3 and G protein-coupled receptor 84. Cell Commun. Signal. 2020, 18, 31. [Google Scholar] [CrossRef]
- Landomiel, F.; De Pascali, F.; Raynaud, P.; Jean-Alphonse, F.; Yvinec, R.; Pellissier, L.P.; Bozon, V.; Bruneau, G.; Crepieux, P.; Poupon, A.; et al. Biased Signaling and Allosteric Modulation at the FSHR. Front. Endocrinol. 2019, 10, 148. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Metcalf, M.; Bunnett, N.W. Biased signaling of protease-activated receptors. Front. Endocrinol. 2014, 5, 67, Correction in Front. Endocrinol. 2015, 5, 228. [Google Scholar] [CrossRef] [PubMed]
- Hodavance, S.Y.; Gareri, C.; Torok, R.D.; Rockman, H.A. G Protein-coupled Receptor Biased Agonism. J. Cardiovasc. Pharmacol. 2016, 67, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Laprairie, R.B.; Bagher, A.M.; Denovan-Wright, E.M. Cannabinoid receptor ligand bias: Implications in the central nervous system. Curr. Opin. Pharmacol. 2017, 32, 32–43. [Google Scholar] [CrossRef]
- Smith, J.S.; Lefkowitz, R.J.; Rajagopal, S. Biased signalling: From simple switches to allosteric microprocessors. Nat. Rev. Drug Discov. 2018, 17, 243–260. [Google Scholar] [CrossRef]
- Bologna, Z.; Teoh, J.P.; Bayoumi, A.S.; Tang, Y.; Kim, I.M. Biased G Protein-Coupled Receptor Signaling: New Player in Modulating Physiology and Pathology. Biomol. Ther. (Seoul) 2017, 25, 12–25. [Google Scholar] [CrossRef]
- Raehal, K.M.; Walker, J.K.; Bohn, L.M. Morphine side effects in β-arrestin 2 knockout mice. J. Pharmacol. Exp. Ther. 2005, 314, 1195–1201. [Google Scholar] [CrossRef]
- Chen, X.T.; Pitis, P.; Liu, G.; Yuan, C.; Gotchev, D.; Cowan, C.L.; Rominger, D.H.; Koblish, M.; Dewire, S.M.; Crombie, A.L.; et al. Structure-activity relationships and discovery of a G protein biased mu opioid receptor ligand, [(3-methoxythiophen-2-yl)methyl](2-[(9R)-9-(pyridin-2-yl)-6-oxaspiro-[4.5]decan-9-yl]ethyl)amine (TRV130), for the treatment of acute severe pain. J. Med. Chem. 2013, 56, 8019–8031. [Google Scholar] [CrossRef]
- Soergel, D.G.; Subach, R.A.; Sadler, B.; Connell, J.; Marion, A.S.; Cowan, C.L.; Violin, J.D.; Lark, M.W. First clinical experience with TRV130: Pharmacokinetics and pharmacodynamics in healthy volunteers. J. Clin. Pharmacol. 2014, 54, 351–357. [Google Scholar] [CrossRef]
- Soergel, D.G.; Subach, R.A.; Burnham, N.; Lark, M.W.; James, I.E.; Sadler, B.M.; Skobieranda, F.; Violin, J.D.; Webster, L.R. Biased agonism of the μ-opioid receptor by TRV130 increases analgesia and reduces on-target adverse effects versus morphine: A randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Pain 2014, 155, 1829–1835. [Google Scholar] [CrossRef]
- Viscusi, E.R.; Webster, L.; Kuss, M.; Daniels, S.; Bolognese, J.A.; Zuckerman, S.; Soergel, D.G.; Subach, R.A.; Cook, E.; Skobieranda, F. A randomized, phase 2 study investigating TRV130, a biased ligand of the μ-opioid receptor, for the intravenous treatment of acute pain. Pain 2016, 157, 264–272. [Google Scholar] [CrossRef]
- Singla, N.K.; Skobieranda, F.; Soergel, D.G.; Salamea, M.; Burt, D.A.; Demitrack, M.A.; Viscusi, E.R. APOLLO-2: A Randomized, Placebo and Active-Controlled Phase III Study Investigating Oliceridine (TRV130), a G Protein-Biased Ligand at the μ-Opioid Receptor, for Management of Moderate to Severe Acute Pain Following Abdominoplasty. Pain Pract. 2019, 19, 715–731. [Google Scholar] [CrossRef] [PubMed]
- Viscusi, E.R.; Skobieranda, F.; Soergel, D.G.; Cook, E.; Burt, D.A.; Singla, N. APOLLO-1: A randomized placebo and active-controlled phase III study investigating oliceridine (TRV130), a G protein-biased ligand at the μ-opioid receptor, for management of moderate-to-severe acute pain following bunionectomy. J. Pain Res. 2019, 12, 927–943. [Google Scholar] [CrossRef] [PubMed]
- Che, T.; Dwivedi-Agnihotri, H.; Shukla, A.K.; Roth, B.L. Biased ligands at opioid receptors: Current status and future directions. Sci. Signal. 2021, 14, eaav0320. [Google Scholar] [CrossRef] [PubMed]
- Kliewer, A.; Schmiedel, F.; Sianati, S.; Bailey, A.; Bateman, J.T.; Levitt, E.S.; Williams, J.T.; Christie, M.J.; Schulz, S. Phosphorylation-deficient G-protein-biased μ-opioid receptors improve analgesia and diminish tolerance but worsen opioid side effects. Nat. Commun. 2019, 10, 367. [Google Scholar] [CrossRef]
- Kliewer, A.; Gillis, A.; Hill, R.; Schmiedel, F.; Bailey, C.; Kelly, E.; Henderson, G.; Christie, M.J.; Schulz, S. Morphine-induced respiratory depression is independent of β-arrestin2 signalling. Br. J. Pharmacol. 2020, 177, 2923–2931. [Google Scholar] [CrossRef]
- Gillis, A.; Gondin, A.B.; Kliewer, A.; Sanchez, J.; Lim, H.D.; Alamein, C.; Manandhar, P.; Santiago, M.; Fritzwanker, S.; Schmiedel, F.; et al. Low intrinsic efficacy for G protein activation can explain the improved side effect profiles of new opioid agonists. Sci. Signal. 2020, 13, eaaz3140. [Google Scholar] [CrossRef]
- van de Wetering, R.; Alder, A.F.; Biggerstaff, A.; Sellen, K.; Luo, D.; Crowley, R.S.; Prisinzano, T.E.; Kivell, B.M. Role of β-Arrestin 2 in the antinociceptive and side effect profile of morphine and the novel mu opioid receptor agonists, kurkinorin and kurkinol. Neuropsychopharmacology 2025, 50, 1777–1786. [Google Scholar] [CrossRef]
- Stahl, E.L.; Bohn, L.M. Low Intrinsic Efficacy Alone Cannot Explain the Improved Side Effect Profiles of New Opioid Agonists. Biochemistry 2022, 61, 1923–1935. [Google Scholar] [CrossRef]
- Conibear, A.E.; Asghar, J.; Hill, R.; Henderson, G.; Borbely, E.; Tekus, V.; Helyes, Z.; Palandri, J.; Bailey, C.; Starke, I.; et al. A Novel G Protein-Biased Agonist at the δ Opioid Receptor with Analgesic Efficacy in Models of Chronic Pain. J. Pharmacol. Exp. Ther. 2020, 372, 224–236. [Google Scholar] [CrossRef]
- PharmNovo: Positive Final Phase I Results. Available online: https://www.pharmnovo.com/post/positive-final-phase-i-results (accessed on 19 November 2025).
- PharmNovo: CTA Approval for PN6047. Available online: https://www.pharmnovo.com/post/cta-approval-for-pn6047 (accessed on 19 November 2025).
- Fossler, M.J.; Schmith, V.; Greene, S.A.; Lohmer, L.; Kramer, M.S.; Arscott, K.; James, I.E.; Demitrack, M.A. A Phase I, Randomized, Single-Blind, Placebo-Controlled, Single Ascending Dose Study of the Safety, Tolerability, and Pharmacokinetics of Subcutaneous and Oral TRV250, a G Protein-Selective Delta Receptor Agonist, in Healthy Subjects. CNS Drugs 2020, 34, 853–865. [Google Scholar] [CrossRef] [PubMed]
- Bertels, Z.; Witkowski, W.D.; Asif, S.; Siegersma, K.; van Rijn, R.M.; Pradhan, A.A. A non-convulsant delta-opioid receptor agonist, KNT-127, reduces cortical spreading depression and nitroglycerin-induced allodynia. Headache 2021, 61, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.Y.; Zhang, H.; Shen, Q.; Cai, C.; Ding, Y.; Shen, D.D.; Guo, J.; Qin, J.; Dong, Y.; Zhang, Y.; et al. Snapshot of the cannabinoid receptor 1-arrestin complex unravels the biased signaling mechanism. Cell 2023, 186, 5784–5797.e17. [Google Scholar] [CrossRef] [PubMed]
- Ford, B.M.; Franks, L.N.; Tai, S.; Fantegrossi, W.E.; Stahl, E.L.; Berquist, M.D.; Cabanlong, C.V.; Wilson, C.D.; Penthala, N.R.; Crooks, P.A.; et al. Characterization of structurally novel G protein biased CB1 agonists: Implications for drug development. Pharmacol. Res. 2017, 125, 161–177. [Google Scholar] [CrossRef] [PubMed]
- Gray, D.L.; Allen, J.A.; Mente, S.; O’Connor, R.E.; DeMarco, G.J.; Efremov, I.; Tierney, P.; Volfson, D.; Davoren, J.; Guilmette, E.; et al. Impaired β-arrestin recruitment and reduced desensitization by non-catechol agonists of the D1 dopamine receptor. Nat. Commun. 2018, 9, 674. [Google Scholar] [CrossRef]
- Martini, M.L.; Ray, C.; Yu, X.; Liu, J.; Pogorelov, V.M.; Wetsel, W.C.; Huang, X.P.; McCorvy, J.D.; Caron, M.G.; Jin, J. Designing Functionally Selective Noncatechol Dopamine D1 Receptor Agonists with Potent In Vivo Antiparkinsonian Activity. ACS Chem. Neurosci. 2019, 10, 4160–4182. [Google Scholar] [CrossRef]
- Teng, X.; Chen, S.; Nie, Y.; Xiao, P.; Yu, X.; Shao, Z.; Zheng, S. Ligand recognition and biased agonism of the D1 dopamine receptor. Nat. Commun. 2022, 13, 3186. [Google Scholar] [CrossRef]
- Kaye, A.D.; Ford, B.M.; Abbott, B.M.; Broocks, K.M.; Novacic, S.; Shekoohi, S. Emerging Clinical Role of Tavapadon, a Novel Dopamine Partial Agonist, in the Treatment of Parkinson’s Disease. Diseases 2025, 13, 290. [Google Scholar] [CrossRef]
- Jastrzębski, M.K.; Wójcik, P.; Grudzińska, A.; Andreozzi, G.; Vetrò, T.; Asim, A.; Mudgal, A.; Czapiński, J.; Wróbel, T.M.; Bartuzi, D.; et al. Biased signaling via serotonin 5-HT2A receptor: From structural aspects to in vitro and in vivo pharmacology. Acta Pharm. Sin. B 2025, 15, 4438–4455. [Google Scholar] [CrossRef]
- Muneta-Arrate, I.; Miranda-Azpiazu, P.; Horrillo, I.; Diez-Alarcia, R.; Meana, J.J. Ligand bias and inverse agonism on 5-HT2A receptor-mediated modulation of G protein activity in post-mortem human brain. Br. J. Pharmacol. 2025, 182, 3320–3335. [Google Scholar] [CrossRef]
- Pieri, L.; Keller, H.H.; Burkard, W.; Da Prada, M. Effects of lisuride and LSD on cerebral monoamine systems and hallucinosis. Nature 1978, 272, 278–280. [Google Scholar] [CrossRef] [PubMed]
- Wallach, J.; Cao, A.B.; Calkins, M.M.; Heim, A.J.; Lanham, J.K.; Bonniwell, E.M.; Hennessey, J.J.; Bock, H.A.; Anderson, E.I.; Sherwood, A.M.; et al. Identification of 5-HT2A receptor signaling pathways associated with psychedelic potential. Nat. Commun. 2023, 14, 8221. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Che, T.; Panova, O.; DiBerto, J.F.; Lyu, J.; Krumm, B.E.; Wacker, D.; Robertson, M.J.; Seven, A.B.; Nichols, D.E.; et al. Structure of a Hallucinogen-Activated Gq-Coupled 5-HT2A Serotonin Receptor. Cell 2020, 182, 1574–1588.e19. [Google Scholar] [CrossRef] [PubMed]
- Cao, D.; Yu, J.; Wang, H.; Luo, Z.; Liu, X.; He, L.; Qi, J.; Fan, L.; Tang, L.; Chen, Z.; et al. Structure-based discovery of nonhallucinogenic psychedelic analogs. Science 2022, 375, 403–411. [Google Scholar] [CrossRef]
- Vollenweider, F.X.; Vollenweider-Scherpenhuyzen, M.F.; Babler, A.; Vogel, H.; Hell, D. Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. Neuroreport 1998, 9, 3897–3902. [Google Scholar] [CrossRef]
- Ippolito, A.; Vasudevan, S.; Hurley, S.; Gilmour, G.; Westhorpe, F.; Churchill, G.; Sharp, T. Evidence that 5-HT2A receptor signalling efficacy and not biased agonism differentiates serotonergic psychedelic from non-psychedelic drugs. Br. J. Pharmacol. 2025. [Google Scholar] [CrossRef]
- Mathieu, N.M.; Nakagawa, P.; Grobe, J.L.; Sigmund, C.D. Insights into the Role of Angiotensin-II AT1 Receptor-Dependent β-Arrestin Signaling in Cardiovascular Disease. Hypertension 2024, 81, 6–16. [Google Scholar] [CrossRef]
- Zanaty, M.; Seara, F.A.C.; Nakagawa, P.; Deng, G.; Mathieu, N.M.; Balapattabi, K.; Karnik, S.S.; Grobe, J.L.; Sigmund, C.D. β-Arrestin-Biased Agonist Targeting the Brain AT1R (Angiotensin II Type 1 Receptor) Increases Aversion to Saline and Lowers Blood Pressure in Deoxycorticosterone Acetate-Salt Hypertension. Hypertension 2021, 77, 420–431. [Google Scholar] [CrossRef]
- Kashihara, T.; Kawagishi, H.; Nakada, T.; Numaga-Tomita, T.; Kadota, S.; Wolf, E.E.; Du, C.K.; Shiba, Y.; Morimoto, S.; Yamada, M. β-Arrestin-Biased AT1 Agonist TRV027 Causes a Neonatal-Specific Sustained Positive Inotropic Effect Without Increasing Heart Rate. JACC Basic Transl. Sci. 2020, 5, 1057–1069. [Google Scholar] [CrossRef]
- Soergel, D.G.; Subach, R.A.; Cowan, C.L.; Violin, J.D.; Lark, M.W. First clinical experience with TRV027: Pharmacokinetics and pharmacodynamics in healthy volunteers. J. Clin. Pharmacol. 2013, 53, 892–899. [Google Scholar] [CrossRef]
- Pang, P.S.; Butler, J.; Collins, S.P.; Cotter, G.; Davison, B.A.; Ezekowitz, J.A.; Filippatos, G.; Levy, P.D.; Metra, M.; Ponikowski, P.; et al. Biased ligand of the angiotensin II type 1 receptor in patients with acute heart failure: A randomized, double-blind, placebo-controlled, phase IIB, dose ranging trial (BLAST-AHF). Eur. Heart J. 2017, 38, 2364–2373. [Google Scholar] [CrossRef] [PubMed]
- Noto, N.M.; Restrepo, Y.M.; Pang, H.W.; Stoyell-Conti, F.; West, C.A.; Speth, R.C. Comparative evaluation of biased agonists Sarcosine1, d-Alanine8—Angiotensin (Ang) II (SD Ang II) and Sarcosine1, Isoleucine8—Ang II (SI Ang II) and their radioiodinated congeners binding to rat liver membrane AT1 receptors. Pharmacol. Res. Perspect. 2023, 11, e01053. [Google Scholar] [CrossRef] [PubMed]
- Ippolito, M.; Benovic, J.L. Biased agonism at β-adrenergic receptors. Cell. Signal. 2021, 80, 109905. [Google Scholar] [CrossRef] [PubMed]
- Tokmakova, A.; Kim, D.; Goddard, W.A., 3rd; Liggett, S.B. Biased β-Agonists Favoring Gs over β-Arrestin for Individualized Treatment of Obstructive Lung Disease. J. Pers. Med. 2022, 12, 331. [Google Scholar] [CrossRef]
- Gimenez, L.E.; Baameur, F.; Vayttaden, S.J.; Clark, R.B. Salmeterol Efficacy and Bias in the Activation and Kinase-Mediated Desensitization of β2-Adrenergic Receptors. Mol. Pharmacol. 2015, 87, 954–964. [Google Scholar] [CrossRef]
- Casiraghi, M.; Wang, H.; Brennan, P.C.; Habrian, C.; Hübner, H.; Schmidt, M.F.; Maul, L.; Pani, B.; Bahriz, S.; Xu, B.; et al. Structure and dynamics determine G protein coupling specificity at a class A GPCR. Sci. Adv. 2025, 11, eadq3971, Erratum in Sci. Adv. 2025, 11, eadz4217. [Google Scholar] [CrossRef]
- Lymperopoulos, A.; Wertz, S.L.; Pollard, C.M.; Desimine, V.L.; Maning, J.; McCrink, K.A. Not all arrestins are created equal: Therapeutic implications of the functional diversity of the β-arrestins in the heart. World J. Cardiol. 2019, 11, 47–56. [Google Scholar] [CrossRef]
- Wisler, J.W.; DeWire, S.M.; Whalen, E.J.; Violin, J.D.; Drake, M.T.; Ahn, S.; Shenoy, S.K.; Lefkowitz, R.J. A unique mechanism of β-blocker action: Carvedilol stimulates β-arrestin signaling. Proc. Natl. Acad. Sci. USA 2007, 104, 16657–16662. [Google Scholar] [CrossRef]
- Münzel, T.; Gori, T. Nebivolol: The somewhat-different beta-adrenergic receptor blocker. J. Am. Coll. Cardiol. 2009, 54, 1491–1499. [Google Scholar] [CrossRef]
- Liu, X.; Ma, L.; Li, H.H.; Huang, B.; Li, Y.X.; Tao, Y.Z.; Ma, L. β-Arrestin-biased signaling mediates memory reconsolidation. Proc. Natl. Acad. Sci. USA 2015, 112, 4483–4488. [Google Scholar] [CrossRef]
- Yi, B.; Jahangir, A.; Evans, A.K.; Briggs, D.; Ravina, K.; Ernest, J.; Farimani, A.B.; Sun, W.; Rajadas, J.; Green, M.; et al. Discovery of novel brain permeable and G protein-biased beta-1 adrenergic receptor partial agonists for the treatment of neurocognitive disorders. PLoS ONE 2017, 12, e0180319. [Google Scholar] [CrossRef]
- Shen, J.; Peddada, T.N.; Komolov, K.E.; De Pascali, F.; Garces, A.M.; Wang, H.; Lerch, M.T.; Benovic, J.L.; Xu, J.; Kobilka, B.K. A biased allosteric modulator functions as a molecular glue to induce β2AR dimerization. bioRxiv 2025. [Google Scholar] [CrossRef]
- Ippolito, M.; De Pascali, F.; Hopfinger, N.; Komolov, K.E.; Laurinavichyute, D.; Reddy, P.A.N.; Sakkal, L.A.; Rajkowski, K.Z.; Nayak, A.P.; Lee, J.; et al. Identification of a β-arrestin-biased negative allosteric modulator for the β2-adrenergic receptor. Proc. Natl. Acad. Sci. USA 2023, 120, e2302668120. [Google Scholar] [CrossRef] [PubMed]
- Slosky, L.M.; Bai, Y.; Toth, K.; Ray, C.; Rochelle, L.K.; Badea, A.; Chandrasekhar, R.; Pogorelov, V.M.; Abraham, D.M.; Atluri, N.; et al. β-Arrestin-Biased Allosteric Modulator of NTSR1 Selectively Attenuates Addictive Behaviors. Cell 2020, 181, 1364–1379. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Chen, O.; Zhou, Y.; Bang, S.; Chandra, S.; Li, Y.; Chen, G.; Xie, R.G.; He, W.; Xu, J.; et al. Arrestin-biased allosteric modulator of neurotensin receptor 1 alleviates acute and chronic pain. Cell 2025, 188, 4332–4349.e21. [Google Scholar] [CrossRef]
- Moore, M.N.; Person, K.L.; Robleto, V.L.; Alwin, A.R.; Krusemark, C.L.; Foster, N.; Ray, C.; Inoue, A.; Jackson, M.R.; Sheedlo, M.J.; et al. Designing allosteric modulators to change GPCR G protein subtype selectivity. Nature 2025. [Google Scholar] [CrossRef]
- Hedderich, J.B.; Persechino, M.; Becker, K.; Heydenreich, F.M.; Gutermuth, T.; Bouvier, M.; Bunemann, M.; Kolb, P. The pocketome of G-protein-coupled receptors reveals previously untargeted allosteric sites. Nat. Commun. 2022, 13, 2567. [Google Scholar] [CrossRef]
- Conde-Frieboes, K.; Thøgersen, H.; Lau, J.F.; Sensfuss, U.; Hansen, T.K.; Christensen, L.; Spetzler, J.; Olsen, H.B.; Nilsson, C.; Raun, K.; et al. Identification and in vivo and in vitro characterization of long acting and melanocortin 4 receptor (MC4-R) selective α-melanocyte-stimulating hormone (α-MSH) analogues. J. Med. Chem. 2012, 55, 1969–1977. [Google Scholar] [CrossRef]
- Royalty, J.E.; Konradsen, G.; Eskerod, O.; Wulff, B.S.; Hansen, B.S. Investigation of safety, tolerability, pharmacokinetics, and pharmacodynamics of single and multiple doses of a long-acting α-MSH analog in healthy overweight and obese subjects. J. Clin. Pharmacol. 2014, 54, 394–404. [Google Scholar] [CrossRef]
- Yang, L.K.; Hou, Z.S.; Tao, Y.X. Biased signaling in naturally occurring mutations of G protein-coupled receptors associated with diverse human diseases. Biochim. Biophys. Acta Mol. Basis Dis. 2021, 1867, 165973. [Google Scholar] [CrossRef]
- Rajagopal, S.; Kim, J.; Ahn, S.; Craig, S.; Lam, C.M.; Gerard, N.P.; Gerard, C.; Lefkowitz, R.J. β-arrestin- but not G protein-mediated signaling by the “decoy” receptor CXCR7. Proc. Natl. Acad. Sci. USA 2010, 107, 628–632. [Google Scholar] [CrossRef]
- Szpakowska, M.; Nevins, A.M.; Meyrath, M.; Rhainds, D.; D’Huys, T.; Guité-Vinet, F.; Dupuis, N.; Gauthier, P.A.; Counson, M.; Kleist, A.; et al. Different contributions of chemokine N-terminal features attest to a different ligand binding mode and a bias towards activation of ACKR3/CXCR7 compared with CXCR4 and CXCR3. Br. J. Pharmacol. 2018, 175, 1419–1438. [Google Scholar] [CrossRef]
- Kalatskaya, I.; Berchiche, Y.A.; Gravel, S.; Limberg, B.J.; Rosenbaum, J.S.; Heveker, N. AMD3100 is a CXCR7 ligand with allosteric agonist properties. Mol. Pharmacol. 2009, 75, 1240–1247. [Google Scholar] [CrossRef] [PubMed]
- Gutjahr, J.C.; Crawford, K.S.; Jensen, D.R.; Naik, P.; Peterson, F.C.; Samson, G.P.B.; Legler, D.F.; Duchene, J.; Veldkamp, C.T.; Rot, A.; et al. The dimeric form of CXCL12 binds to atypical chemokine receptor 1. Sci. Signal. 2021, 14, eabc9012. [Google Scholar] [CrossRef]
- Veldkamp, C.T.; Seibert, C.; Peterson, F.C.; De la Cruz, N.B.; Haugner, J.C., 3rd; Basnet, H.; Sakmar, T.P.; Volkman, B.F. Structural basis of CXCR4 sulfotyrosine recognition by the chemokine SDF-1/CXCL12. Sci. Signal. 2008, 1, ra4. [Google Scholar] [CrossRef] [PubMed]
- Drury, L.J.; Ziarek, J.J.; Gravel, S.; Veldkamp, C.T.; Takekoshi, T.; Hwang, S.T.; Heveker, N.; Volkman, B.F.; Dwinell, M.B. Monomeric and dimeric CXCL12 inhibit metastasis through distinct CXCR4 interactions and signaling pathways. Proc. Natl. Acad. Sci. USA 2011, 108, 17655–17660. [Google Scholar] [CrossRef] [PubMed]
- Jean-Alphonse, F.; Perkovska, S.; Frantz, M.C.; Durroux, T.; Méjean, C.; Morin, D.; Loison, S.; Bonnet, D.; Hibert, M.; Mouillac, B.; et al. Biased agonist pharmacochaperones of the AVP V2 receptor may treat congenital nephrogenic diabetes insipidus. J. Am. Soc. Nephrol. 2009, 20, 2190–2203. [Google Scholar] [CrossRef]
- Mendre, C.; Mouillac, B. Misfolding of vasopressin receptors: Biased agonist pharmacochaperones as potential therapeutics. Adv. Protein Chem. Struct. Biol. 2019, 118, 249–272. [Google Scholar] [CrossRef]
- Leach, K.; Wen, A.; Davey, A.E.; Sexton, P.M.; Conigrave, A.D.; Christopoulos, A. Identification of molecular phenotypes and biased signaling induced by naturally occurring mutations of the human calcium-sensing receptor. Endocrinology 2012, 153, 4304–4316. [Google Scholar] [CrossRef]
- Watanabe, S.; Fukumoto, S.; Chang, H.; Takeuchi, Y.; Hasegawa, Y.; Okazaki, R.; Chikatsu, N.; Fujita, T. Association between activating mutations of calcium-sensing receptor and Bartter’s syndrome. Lancet 2002, 360, 692–694. [Google Scholar] [CrossRef]
- Hendy, G.N.; D’Souza-Li, L.; Yang, B.; Canaff, L.; Cole, D.E. Mutations of the calcium-sensing receptor (CASR) in familial hypocalciuric hypercalcemia, neonatal severe hyperparathyroidism, and autosomal dominant hypocalcemia. Hum. Mutat. 2000, 16, 281–296. [Google Scholar] [CrossRef]
- Koole, C.; Wootten, D.; Simms, J.; Valant, C.; Miller, L.J.; Christopoulos, A.; Sexton, P.M. Polymorphism and ligand dependent changes in human glucagon-like peptide-1 receptor (GLP-1R) function: Allosteric rescue of loss of function mutation. Mol. Pharmacol. 2011, 80, 486–497, Erratum in Mol. Pharmacol. 2012, 82, P142. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Ji, R.L.; Tao, Y.X. Naturally occurring mutations in G protein-coupled receptors associated with obesity and type 2 diabetes mellitus. Pharmacol. Ther. 2022, 234, 108044. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Huang, H.; Tao, Y.X. Biased signaling in naturally occurring mutations in human melanocortin-3 receptor gene. Int. J. Biol. Sci. 2015, 11, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Lotta, L.A.; Mokrosiński, J.; Mendes de Oliveira, E.; Li, C.; Sharp, S.J.; Luan, J.; Brouwers, B.; Ayinampudi, V.; Bowker, N.; Kerrison, N.; et al. Human Gain-of-Function MC4R Variants Show Signaling Bias and Protect against Obesity. Cell 2019, 177, 597–607.e9. [Google Scholar] [CrossRef]
- Franco, R.; Rivas-Santisteban, R.; Reyes-Resina, I.; Navarro, G. The Old and New Visions of Biased Agonism Through the Prism of Adenosine Receptor Signaling and Receptor/Receptor and Receptor/Protein Interactions. Front. Pharmacol. 2020, 11, 628601. [Google Scholar] [CrossRef]
- Ciruela, F.; Casadó, V.; Rodrigues, R.J.; Luján, R.; Burgueño, J.; Canals, M.; Borycz, J.; Rebola, N.; Goldberg, S.R.; Mallol, J.; et al. Presynaptic control of striatal glutamatergic neurotransmission by adenosine A1-A2A receptor heteromers. J. Neurosci. 2006, 26, 2080–2087. [Google Scholar] [CrossRef]
- Rozenfeld, R.; Devi, L.A. Receptor heterodimerization leads to a switch in signaling: Beta-arrestin2-mediated ERK activation by mu-delta opioid receptor heterodimers. FASEB J. 2007, 21, 2455–2465. [Google Scholar] [CrossRef]
- Gomes, I.; Fujita, W.; Gupta, A.; Saldanha, S.A.; Negri, A.; Pinello, C.E.; Eberhart, C.; Roberts, E.; Filizola, M.; Hodder, P.; et al. Identification of a μ-δ opioid receptor heteromer-biased agonist with antinociceptive activity. Proc. Natl. Acad. Sci. USA 2013, 110, 12072–12077, Correction in Proc. Natl. Acad. Sci. USA 2013, 110, 17160. [Google Scholar] [CrossRef]
- Liu, J.; Tang, H.; Xu, C.; Zhou, S.; Zhu, X.; Li, Y.; Prezeau, L.; Xu, T.; Pin, J.P.; Rondard, P.; et al. Biased signaling due to oligomerization of the G protein-coupled platelet-activating factor receptor. Nat. Commun. 2022, 13, 6365. [Google Scholar] [CrossRef]
- Levoye, A.; Balabanian, K.; Baleux, F.; Bachelerie, F.; Lagane, B. CXCR7 heterodimerizes with CXCR4 and regulates CXCL12-mediated G protein signaling. Blood 2009, 113, 6085–6093. [Google Scholar] [CrossRef]
- Dicenta-Baunach, V.; Laspa, Z.; Schaale, D.; Sigle, M.; Bayrak, A.; Castor, T.; Pillaiyar, T.; Laufer, S.; Gawaz, M.P.; Rohlfing, A.K. ACKR3 agonism induces heterodimerization with chemokine receptor CXCR4 and attenuates platelet function. Eur. J. Clin. Invest. 2025, 55, e14327. [Google Scholar] [CrossRef]
- Song, Z.Y.; Wang, F.; Cui, S.X.; Gao, Z.H.; Qu, X.J. CXCR7/CXCR4 heterodimer-induced histone demethylation: A new mechanism of colorectal tumorigenesis. Oncogene 2019, 38, 1560–1575. [Google Scholar] [CrossRef]
- Kubatova, N.; Schmidt, T.; Wang, Q.; Clore, G.M. Dimerization propensity of the β1-adrenergic receptor in lipid nanodiscs probed by DEER and single-molecule spectroscopies. Proc. Natl. Acad. Sci. USA 2025, 122, e2519609122. [Google Scholar] [CrossRef] [PubMed]
- Masuho, I.; Ostrovskaya, O.; Kramer, G.M.; Jones, C.D.; Xie, K.; Martemyanov, K.A. Distinct profiles of functional discrimination among G proteins determine the actions of G protein-coupled receptors. Sci. Signal. 2015, 8, ra123. [Google Scholar] [CrossRef] [PubMed]
- Kenakin, T. Is the Quest for Signaling Bias Worth the Effort? Mol. Pharmacol. 2018, 93, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Schattauer, S.S.; Kuhar, J.R.; Song, A.; Chavkin, C. Nalfurafine is a G-protein biased agonist having significantly greater bias at the human than rodent form of the kappa opioid receptor. Cell. Signal. 2017, 32, 59–65. [Google Scholar] [CrossRef]
- Urs, N.M.; Peterson, S.M.; Caron, M.G. New Concepts in Dopamine D2 Receptor Biased Signaling and Implications for Schizophrenia Therapy. Biol. Psychiatry 2017, 81, 78–85. [Google Scholar] [CrossRef]
- Urs, N.M.; Gee, S.M.; Pack, T.F.; McCorvy, J.D.; Evron, T.; Snyder, J.C.; Yang, X.; Rodriguiz, R.M.; Borrelli, E.; Wetsel, W.C.; et al. Distinct cortical and striatal actions of a β-arrestin-biased dopamine D2 receptor ligand reveal unique antipsychotic-like properties. Proc. Natl. Acad. Sci. USA 2016, 113, E8178–E8186. [Google Scholar] [CrossRef]
- Park, S.M.; Chen, M.; Schmerberg, C.M.; Dulman, R.S.; Rodriguiz, R.M.; Caron, M.G.; Jin, J.; Wetsel, W.C. Effects of β-Arrestin-Biased Dopamine D2 Receptor Ligands on Schizophrenia-Like Behavior in Hypoglutamatergic Mice. Neuropsychopharmacology 2016, 41, 704–715. [Google Scholar] [CrossRef]
- Nguyen, A.M.; Semeano, A.; Quach, V.; Inoue, A.; Nichols, D.E.; Yano, H. Characterization of Gαs and Gαolf activation by catechol and non-catechol dopamine D1 receptor agonists. iScience 2025, 28, 112345. [Google Scholar] [CrossRef] [PubMed]
- Onfroy, L.; Galandrin, S.; Pontier, S.M.; Seguelas, M.H.; N’Guyen, D.; Sénard, J.M.; Galés, C. G protein stoichiometry dictates biased agonism through distinct receptor-G protein partitioning. Sci. Rep. 2017, 7, 7885. [Google Scholar] [CrossRef] [PubMed]
- Ferraiolo, M.; Ponthot, R.; Atik, H.; Koener, B.; Hanson, J.; Hermans, E. Receptor density influences the recruitment bias of aripiprazole and brexpiprazole at the dopamine D2L receptor. Fundam. Clin. Pharmacol. 2022, 36, 976–984. [Google Scholar] [CrossRef] [PubMed]
- Nash, C.A.; Wei, W.; Irannejad, R.; Smrcka, A.V. Golgi localized β1-adrenergic receptors stimulate Golgi PI4P hydrolysis by PLCepsilon to regulate cardiac hypertrophy. eLife 2019, 8, e48167. [Google Scholar] [CrossRef]
- Jensen, D.D.; Lieu, T.; Halls, M.L.; Veldhuis, N.A.; Imlach, W.L.; Mai, Q.N.; Poole, D.P.; Quach, T.; Aurelio, L.; Conner, J.; et al. Neurokinin 1 receptor signaling in endosomes mediates sustained nociception and is a viable therapeutic target for prolonged pain relief. Sci. Transl. Med. 2017, 9, eaal3447. [Google Scholar] [CrossRef]
- Vargas, M.V.; Dunlap, L.E.; Dong, C.; Carter, S.J.; Tombari, R.J.; Jami, S.A.; Cameron, L.P.; Patel, S.D.; Hennessey, J.J.; Saeger, H.N.; et al. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Science 2023, 379, 700–706. [Google Scholar] [CrossRef]
- Vincent, K.; Cornea, V.M.; Jong, Y.I.; Laferriere, A.; Kumar, N.; Mickeviciute, A.; Fung, J.S.T.; Bandegi, P.; Ribeiro-da-Silva, A.; O’Malley, K.L.; et al. Intracellular mGluR5 plays a critical role in neuropathic pain. Nat. Commun. 2016, 7, 10604. [Google Scholar] [CrossRef]
- Hebert-Chatelain, E.; Desprez, T.; Serrat, R.; Bellocchio, L.; Soria-Gomez, E.; Busquets-Garcia, A.; Pagano Zottola, A.C.; Delamarre, A.; Cannich, A.; Vincent, P.; et al. A cannabinoid link between mitochondria and memory. Nature 2016, 539, 555–559. [Google Scholar] [CrossRef]
- Eiger, D.S.; Boldizsar, N.; Honeycutt, C.C.; Gardner, J.; Kirchner, S.; Hicks, C.; Choi, I.; Pham, U.; Zheng, K.; Warman, A.; et al. Location bias contributes to functionally selective responses of biased CXCR3 agonists. Nat. Commun. 2022, 13, 5846. [Google Scholar] [CrossRef]
- Gardner, J.; Eiger, D.S.; Hicks, C.; Choi, I.; Pham, U.; Chundi, A.; Namjoshi, O.; Rajagopal, S. GPCR kinases differentially modulate biased signaling downstream of CXCR3 depending on their subcellular localization. Sci. Signal. 2024, 17, eadd9139. [Google Scholar] [CrossRef]
- Crilly, S.E.; Ko, W.; Weinberg, Z.Y.; Puthenveedu, M.A. Conformational specificity of opioid receptors is determined by subcellular location irrespective of agonist. eLife 2021, 10, e67478. [Google Scholar] [CrossRef]
- Kim, D.; Tokmakova, A.; Woo, J.A.; An, S.S.; Goddard, W.A., 3rd; Liggett, S.B. Selective Signal Capture from Multidimensional GPCR Outputs with Biased Agonists: Progress Towards Novel Drug Development. Mol. Diagn. Ther. 2022, 26, 383–396. [Google Scholar] [CrossRef]
- Chidiac, P. RGS proteins destroy spare receptors: Effects of GPCR-interacting proteins and signal deamplification on measurements of GPCR agonist potency. Methods 2016, 92, 87–93. [Google Scholar] [CrossRef]
- Li, A.; Liu, S.; Huang, R.; Ahn, S.; Lefkowitz, R.J. Loss of biased signaling at a G protein-coupled receptor in overexpressed systems. PLoS ONE 2023, 18, e0283477. [Google Scholar] [CrossRef]
- Alvarez-Curto, E.; Inoue, A.; Jenkins, L.; Raihan, S.Z.; Prihandoko, R.; Tobin, A.B.; Milligan, G. Targeted Elimination of G Proteins and Arrestins Defines Their Specific Contributions to Both Intensity and Duration of G Protein-coupled Receptor Signaling. J. Biol. Chem. 2016, 291, 27147–27159. [Google Scholar] [CrossRef] [PubMed]
- Kolb, P.; Kenakin, T.; Alexander, S.P.H.; Bermudez, M.; Bohn, L.M.; Breinholt, C.S.; Bouvier, M.; Hill, S.J.; Kostenis, E.; Martemyanov, K.A.; et al. Community guidelines for GPCR ligand bias: IUPHAR review 32. Br. J. Pharmacol. 2022, 179, 3651–3674. [Google Scholar] [CrossRef] [PubMed]
- Pineyro, G.; Nagi, K. Signaling diversity of mu- and delta- opioid receptor ligands: Re-evaluating the benefits of β-arrestin/G protein signaling bias. Cell. Signal. 2021, 80, 109906. [Google Scholar] [CrossRef] [PubMed]
- Hashem, S.; Dougha, A.; Tufféry, P. Ligand-Induced Biased Activation of GPCRs: Recent Advances and New Directions from In Silico Approaches. Molecules 2025, 30, 1047. [Google Scholar] [CrossRef]
| Site of Interaction with the Receptor | Bias | Receptor | Ligand(s) | Potential Therapeutic Indication | Refs. |
|---|---|---|---|---|---|
| Extracellular | β-arrestin over G protein | 5-HT2A | HCH-7113 | Anti-depressive, non-hallucinogenic | [116] |
| AT1R | TRV027 | Anti-hypertensive | [120] | ||
| β1AR, β2AR | Carvedilol, nebivolol | Cardioprotection | [125,129,130] | ||
| Carvedilol, alprenolol | Memory-related disorders | [132] | |||
| G protein over β-arrestin | μ opioid | Oliceridine, | Analgesia | [88] | |
| δ opioid | PN6047, TRV250, KNT-127 | Analgesia (neuropathic pain, migraine) | [100,103,104] | ||
| CB1R | Indole quinulidinones | Analgesia | [106] | ||
| D1 | Tavapadon and other noncatechol agonists | Parkinson’s disease | [110] | ||
| β1AR | STD-101-D1 | Cognitive disorders | [133] | ||
| β2AR | Salmeterol | Bronchodilation with decreased tolerance | [125,127] | ||
| G protein bias | 5-HT2A | Pimavanserin | Parkinson’s disease psychosis | [111,112] | |
| Ketanserin | Hypertension | [111,112,117] | |||
| MC4R | MC4-NN2-0453 | Obesity with fewer cardiovascular implications | [140,141] | ||
| GRK bias | β2AR | Modified BRL-37344 analogs | Type 2 diabetes and obesity | [68] | |
| Transmembrane | G protein over β-arrestin through receptor di/oligomerization | β2AR | AP-7-168 | Sustained bronchodilation | [134,135] |
| Intracellular | β-arrestin over G protein | NTSR1 | SBI-553, SBI-810 | Peripheral and central neuropathic pain | [136,137] |
| G protein | NTSR1 | Modified SBI-553 analogs | None yet | [138] |
| Status/Phase | Drug/Ligand | Receptor | Bias | Therapeutic Indication | References |
|---|---|---|---|---|---|
| Approved | Oliceridine (TRV130) | μ-opioid | G protein over β-arrestin | Short-term management of moderate-to-severe acute pain | [90,91,92,93] |
| Pimavanserin | 5-HT2A | Gαi/o over Gαq/11 | Parkinson’s disease psychosis | [111,112] | |
| Ketanserin | 5-HT2A | Gαq/11 over Gαi/o Gαq/11 over β-arrestin | Hypertension | [111,112,117] | |
| Carvedilol | β1AR, β2AR | β-arrestin over G protein | Hypertension, heart failure | [125,129,130] | |
| Nebivolol | β1AR | β-arrestin over G protein | Hypertension, heart failure | [125] | |
| Salmeterol | β2AR | Gαs over β-arrestin | Asthma | [125] | |
| Phase III | Tavapadon | D1 | G protein over β-arrestin | Parkinson’s disease | [110] |
| Phase IIa | TRV250 | δ-opioid | G protein over β-arrestin | Acute migraine | [103] |
| Phase I | PN6047 | δ-opioid | G protein over β-arrestin | Neuropathic pain | [101] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liolitsas, N.G.; Pantazaka, E.; Papadimitriou, E. To Be Biased or Not to Be: A Play for G-Protein Coupled Receptors. Int. J. Transl. Med. 2025, 5, 56. https://doi.org/10.3390/ijtm5040056
Liolitsas NG, Pantazaka E, Papadimitriou E. To Be Biased or Not to Be: A Play for G-Protein Coupled Receptors. International Journal of Translational Medicine. 2025; 5(4):56. https://doi.org/10.3390/ijtm5040056
Chicago/Turabian StyleLiolitsas, Nikitas G., Evangelia Pantazaka, and Evangelia Papadimitriou. 2025. "To Be Biased or Not to Be: A Play for G-Protein Coupled Receptors" International Journal of Translational Medicine 5, no. 4: 56. https://doi.org/10.3390/ijtm5040056
APA StyleLiolitsas, N. G., Pantazaka, E., & Papadimitriou, E. (2025). To Be Biased or Not to Be: A Play for G-Protein Coupled Receptors. International Journal of Translational Medicine, 5(4), 56. https://doi.org/10.3390/ijtm5040056






