2. Case Report
An 81-year-old Caucasian male was admitted to the Emergency Department following a syncopal episode at home, accompanied by acute pain in the right iliac fossa. Two weeks prior, he had been discharged after treatment for multifocal pneumonia caused by multidrug-resistant Klebsiella pneumoniae, along with severe thrombocytopenia. His antibiotic regimen included Ceftazidime/Avibactam for 10 days. Additionally, he had a history of hospitalization for COVID-19 eight months earlier, which was complicated by hydropneumothorax and pulmonary embolism.
The patient’s medical history included atrial fibrillation, managed with oral anticoagulation (Apixaban), hypertension, and non-insulin-dependent diabetes mellitus. Upon admission, the patient was conscious but pallid, with his vital signs indicating an arterial blood pressure of 110/70 mmHg, heart rate of 162 bpm, and oxygen saturation of 90%. Laboratory tests revealed neutrophilic leukocytosis (WBC 33.80/μL), elevated partial thromboplastin time (PTT 49 s), INR 1.8, and decreased hemoglobin (7.6 g/dL), with a normal platelet count (292,000 µL).
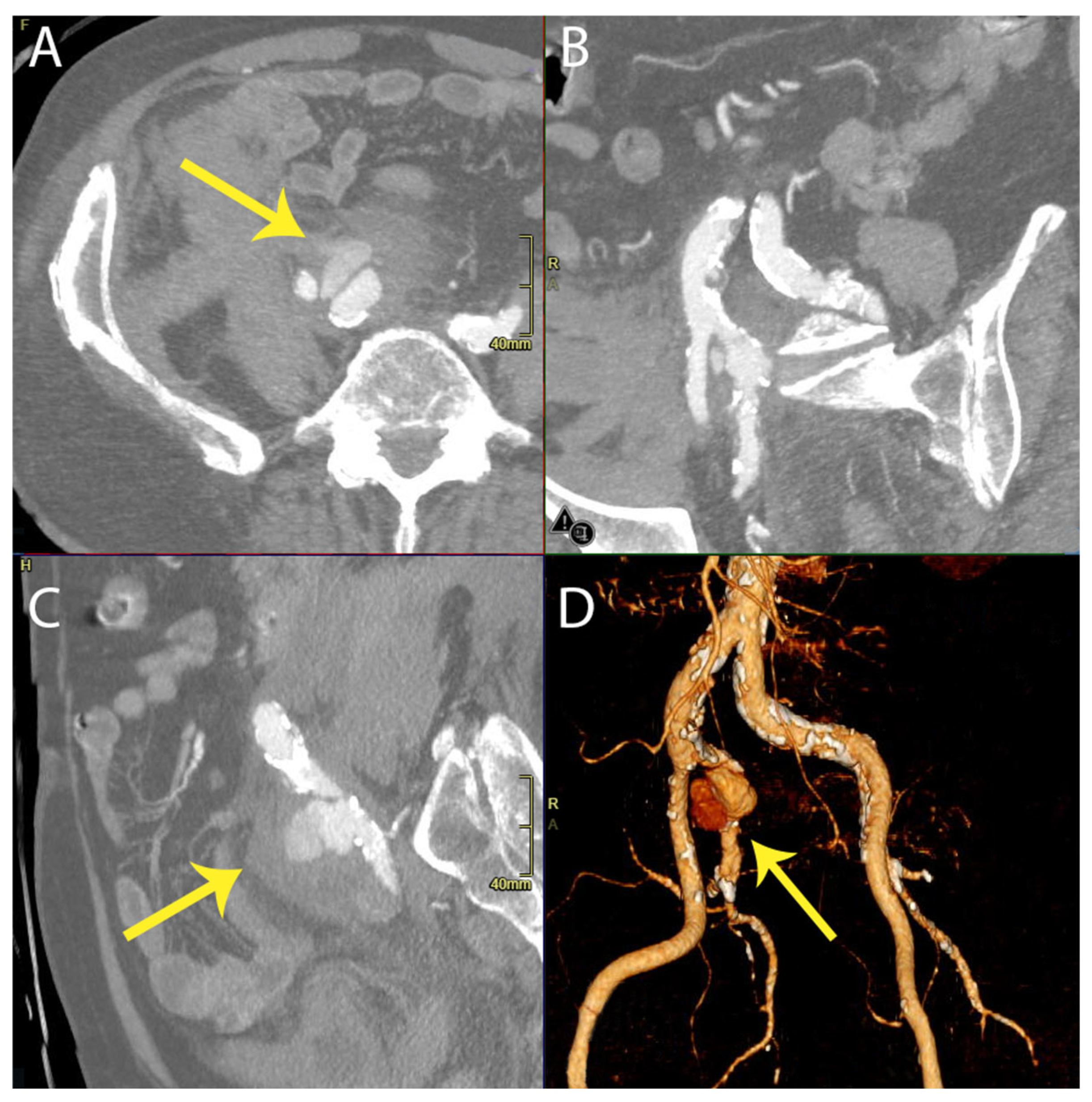
An intravenous contrast-enhanced abdominal CT scan demonstrated an “aneurysmatic dilatation of the right iliac bifurcation”, predominantly affecting the IIA, with a diameter of 4 cm and evidence of extraluminal extravasation of the contrast media, indicative of a rupture. Additionally, blood effusion was noted in the perianeurysmal space, perihepatic area, right paracolic gutter, and pelvic cavity. The patient was promptly taken to the operating theatre, where permissive hypotension and hypovolemia were employed. See
Figure 1.
Under local anesthesia, percutaneous left femoral access was obtained using ultrasound guidance. Following aortic catheter crossing, an 8 Fr Flexor (Cook) sheath was inserted into the right IIA. Diagnostic angiography confirmed a free rupture of the middle portion of the artery. Intraoperative evaluation revealed a focal plaque rupture as the source of the hemorrhage.
A 7 mm × 10 cm Viabahn (Gore) stent graft was deployed distally, with proximal extension to the origin of the IIA using an additional 9 mm × 57 mm BeGraft (Bentley) stent. Control angiography confirmed technical success, with no leaks from the iliac branches. Femoral access was subsequently closed using a 6 Fr Perclose Proglide device.
The patient remained hemodynamically stable during the perioperative period and was transferred to a normal ward shortly after surgery. Blood cultures taken postoperatively identified carbapenem-resistant Klebsiella pneumoniae, leading to the initiation of immediate antibiotic therapy with Colistin for 20 days. Following two consecutive negative blood cultures, treatment was discontinued. However, urine cultures revealed Staphylococcus aureus and the persistence of Klebsiella pneumoniae, necessitating additional treatment with Ceftazidime/Avibactam and Vancomycin for 7 and 14 days, respectively.
Given the history of bacteremia, the possibility of a PET-CT scan was discussed within the multidisciplinary team. However, due to the patient’s clinical stability and normalization of inflammatory markers, PET-CT was deferred unless clinical or biochemical signs of infection emerged.
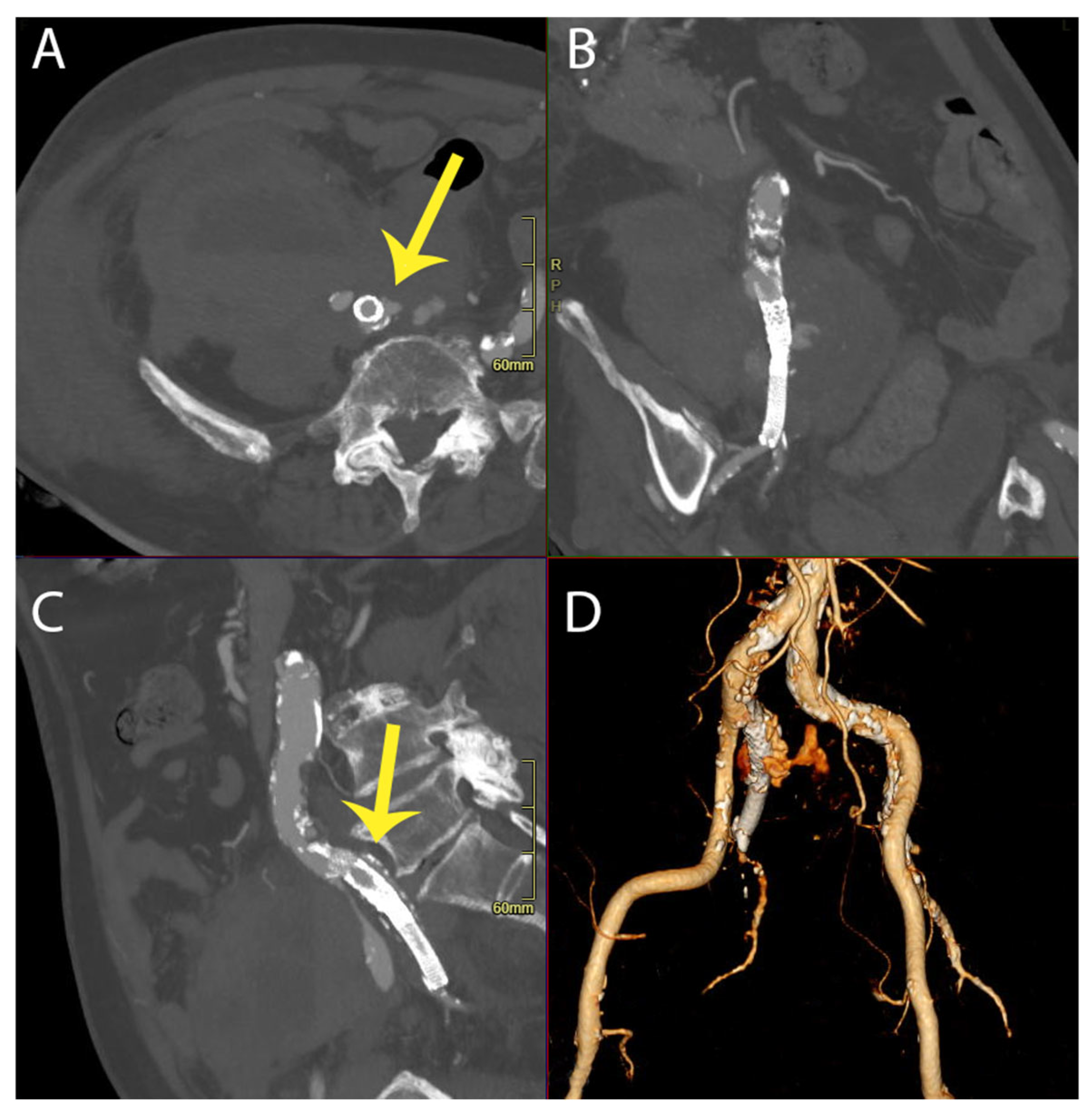
On the 30th postoperative day, the patient experienced a leakage from their rupture site that was a type Ia Endoleak (
Figure 2), requiring an additional endovascular procedure to embolize the IIA and reline the common iliac and external iliac artery with an endograft.
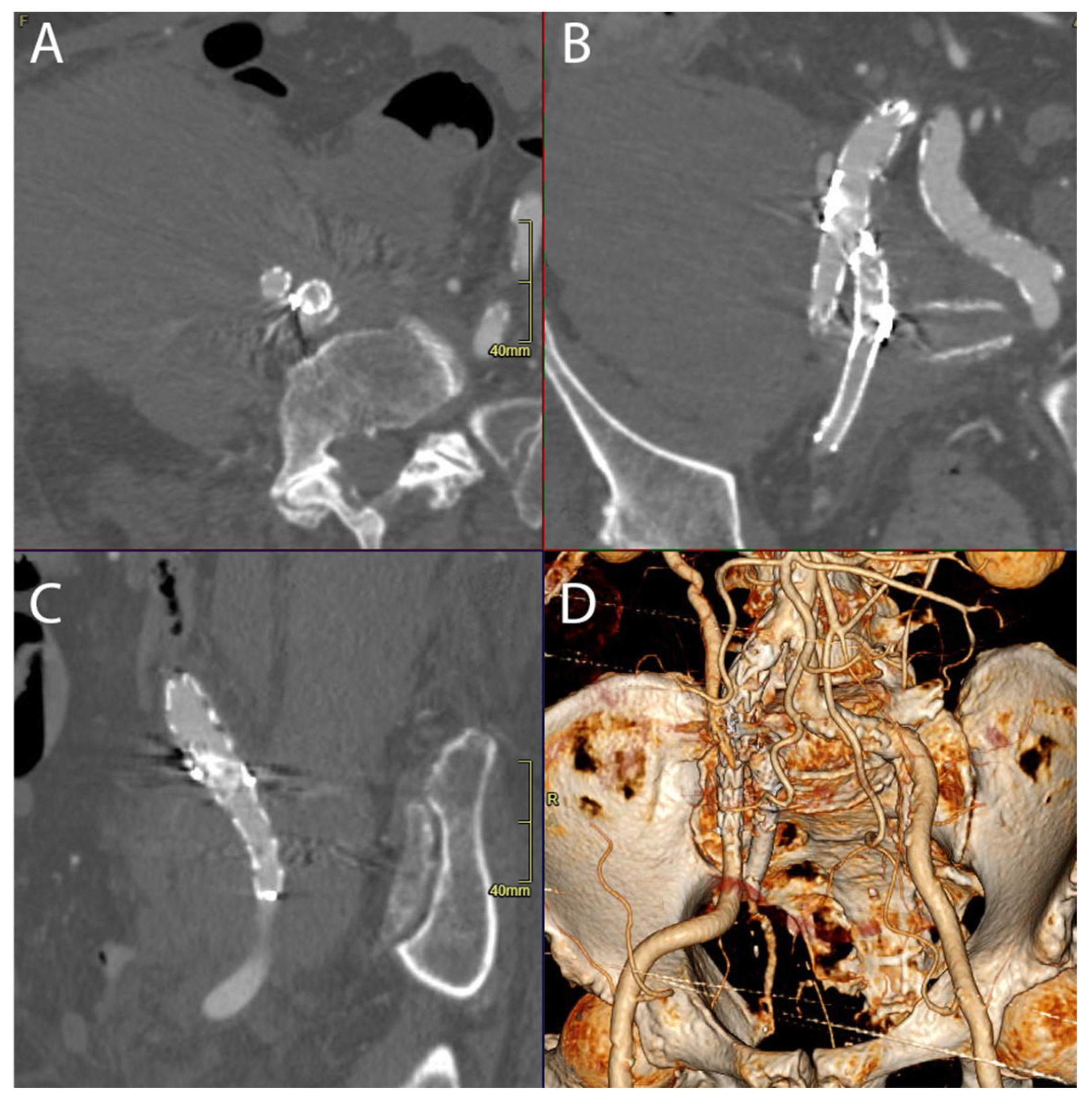
This intervention successfully managed the recurrent rupture, and the patient achieved clinical stability, leading to their discharge on the 35th postoperative day. Se
Figure 3.
3. Discussion
The intraoperative discovery of plaque rupture as the source of the hemorrhage suggests a mechanical cause of the spontaneous rupture. However, given the patient’s recent severe infection with Klebsiella pneumoniae and its known association with vascular complications, an infectious etiology is the more probable contributor to vascular instability. While the patient had underlying atherosclerotic vascular disease, the abrupt nature of the rupture, in the absence of a significant pre-existing aneurysm, strongly suggests that infection-induced arterial wall weakening played a primary role.
Open surgical repair, including arterial ligation or bypass reconstruction, remains the definitive option for managing ruptured iliac aneurysms, especially in the presence of infection. However, in this case, the infectious etiology was not initially confirmed, as the diagnosis of bacteremia was only established after the results of the hemoculture samples. Given this uncertainty, along with the patient’s significant frailty and multiple comorbidities, an extensive open procedure was considered too high-risk. Less invasive strategies were evaluated, including coiling, but the anatomical configuration and the presence of an active rupture site made achieving complete exclusion challenging with coiling alone. Ultimately, an endovascular approach with stent grafting was chosen, ensuring rapid hemorrhage control while preserving vessel patency. This strategy balanced the need for urgent intervention with the patient’s overall clinical condition, minimizing surgical trauma while effectively managing the rupture.
The cause of the endoleak or secondary rupture may be attributed to incomplete apposition of the stent graft to the vessel wall, likely due to the undersizing of the initial graft in relation to the dynamically changing vessel diameter post-rupture or arterial wall degeneration due to the infection. The sizing during the emergency procedure was based on available preoperative imaging, which may not have accurately reflected the post-rupture anatomy. The subsequent intervention aimed to address this by extending the landing zone and utilizing additional graft material for better sealing.
The presence of carbapenem-resistant Klebsiella pneumoniae bacteremia posed an additional challenge in the management of this patient. Research indicates that Klebsiella infections, while rare in vascular graft infections, have been reported [
5,
6]. Although the initial endovascular procedure was justified by the patient’s hemodynamic instability and comorbidities, an open surgical approach with proximal ligation was considered after the endoleak. However, given the patient’s frailty, the risk of extensive open surgery was deemed higher than that of a secondary endovascular repair, despite the addition of more synthetic material.
Endovascular aneurysm repair for aortoiliac aneurysms is a well-established and standardized technique for both elective and emergency abdominal aortic aneurysm repairs, with continual advancements being made in its techniques and innovative approaches [
7]. However, there is no consensus on treatment strategies for isolated IIAA or IIA ruptures, as anatomical challenges and lesion topography significantly influence the choice between open (ligation, interposition, bypass) and endovascular approaches (endografting, coil embolization, plug, glue) [
8].
Two decades ago, graft placement directly into the IIA was considered impractical, with internal iliac aneurysms typically excluded through stenting of the external and common iliac arteries. Stenting was seen as analogous to proximal ligation, while coiling was viewed as equivalent to distal ligation [
4]. In the modern era, endovascular approaches provide minimally invasive techniques, reducing the impact of life-threatening hemorrhages and their associated complications.
In our case, the presence of IIAA rupture, as indicated by preoperative CT angiography, led to the decision to proceed with an endovascular approach, considering the patient’s fragility. This strategy aimed to fully cover the IIA with an endograft. A review of previous CT scans from one month prior to the rupture event revealed no evidence of aneurysms; instead, only atherosclerosis of both iliac arteries and some ectasia of the right common iliac artery (with a maximum diameter of 18 × 20 mm) were noted, with the IIA measuring 13–15 mm in the portion that was most ectatic. See
Figure 4.
The history of pneumonia with multidrug-resistant Klebsiella pneumoniae prompted blood culture testing, which returned positive for carbapenem-resistant Klebsiella pneumoniae, in accordance with the MAGIC criteria. The patient exhibited a gradual decrease in inflammatory markers, with two subsequent blood cultures returning negative after 10 and 20 days of antibiotic therapy.
Following the second intervention, the patient initially showed clinical stability, and he was discharged to a rehabilitation clinic. However, during an attempt to obtain long-term follow-up data, we were informed by the family that the patient had passed away due to causes unrelated to the vascular intervention. While further clinical details are unavailable, this underscores the frailty of such patients and the importance of individualized treatment strategies.
While we cannot definitively rule out the influence of Klebsiella pneumoniae infection as a cause of the spontaneous IIA rupture, no cases have been documented in the literature linking this pathogen to such events or to spontaneous ruptures occurring without congenital or degenerative pathology. However, infectious pseudoaneurysms due to Klebsiella pneumoniae have been reported in the literature, predominantly affecting the femoral and tibioperoneal arteries. Wang et al. described a case of a pseudoaneurysm of the right common femoral artery associated with a K. pneumoniae infection, which was successfully treated with a stent graft and long-term antibiotic therapy [
6]. Similarly, Ninomiya et al. reported a case of a tibioperoneal trunk pseudoaneurysm caused by hypermucoviscous K. pneumoniae, which ruptured into an abscess cavity and was effectively treated with endovascular coil embolization [
9]. Khairunnisa et al. described a rapidly progressing pseudoaneurysm of the right common femoral artery in the context of K. pneumoniae infection, resulting in fatal rupture before definitive surgical intervention [
10]. These cases illustrate the potential for Klebsiella pneumoniae to cause vascular compromise, particularly in the presence of systemic infection and bacteremia.
Cai et al. described a case of donor-derived CRKP infection in one patient following liver transplantation and two patients following renal transplantation (involving one liver and two kidneys from the same donor). All three patients presented with sudden abdominal pain and hemorrhage shortly after transplantation. Graft artery rupture, attributed to corrosion caused by the CRKP infection, was confirmed through computed tomography, blood culture, laparotomy, and pulsed-field gel electrophoresis [
11].
One report described a case of spontaneous internal iliac artery rupture in a pregnant patient, though the exact cause remained undetermined. The mortality rate associated with internal iliac rupture in non-pregnant women ranges from 50% to 100%, often due to delayed diagnosis and subsequent hemodynamic complications [
3].
Therefore, acute abdominal pain, especially with a sudden drop in hemoglobin, should prompt immediate investigation. Recent infections affecting the pulmonary, gastrointestinal, or urinary tracts may be considered potential risk factors for vascular compromise. Additionally, prior vascular surgeries, particularly aortoiliac bypasses, could elevate the risk of complications, including aortoenteric fistula formation. Timely CT imaging is crucial for accurate diagnosis and successful intervention in such cases.
Importantly, individual anatomical variations may not always be conducive to the implantation of intravascular devices such as iliac branch devices, given the limitations specified in their instructions for use (IFU). Our findings suggest that a more extensive landing zone in the initial repair may have prevented recurrence.