Common Variable Immunodeficiency and Selective IgA Deficiency: Focus on Autoimmune Manifestations and Their Pathogenesis
Abstract
1. Introduction
2. CVID
2.1. Epidemiology
2.2. Genetics
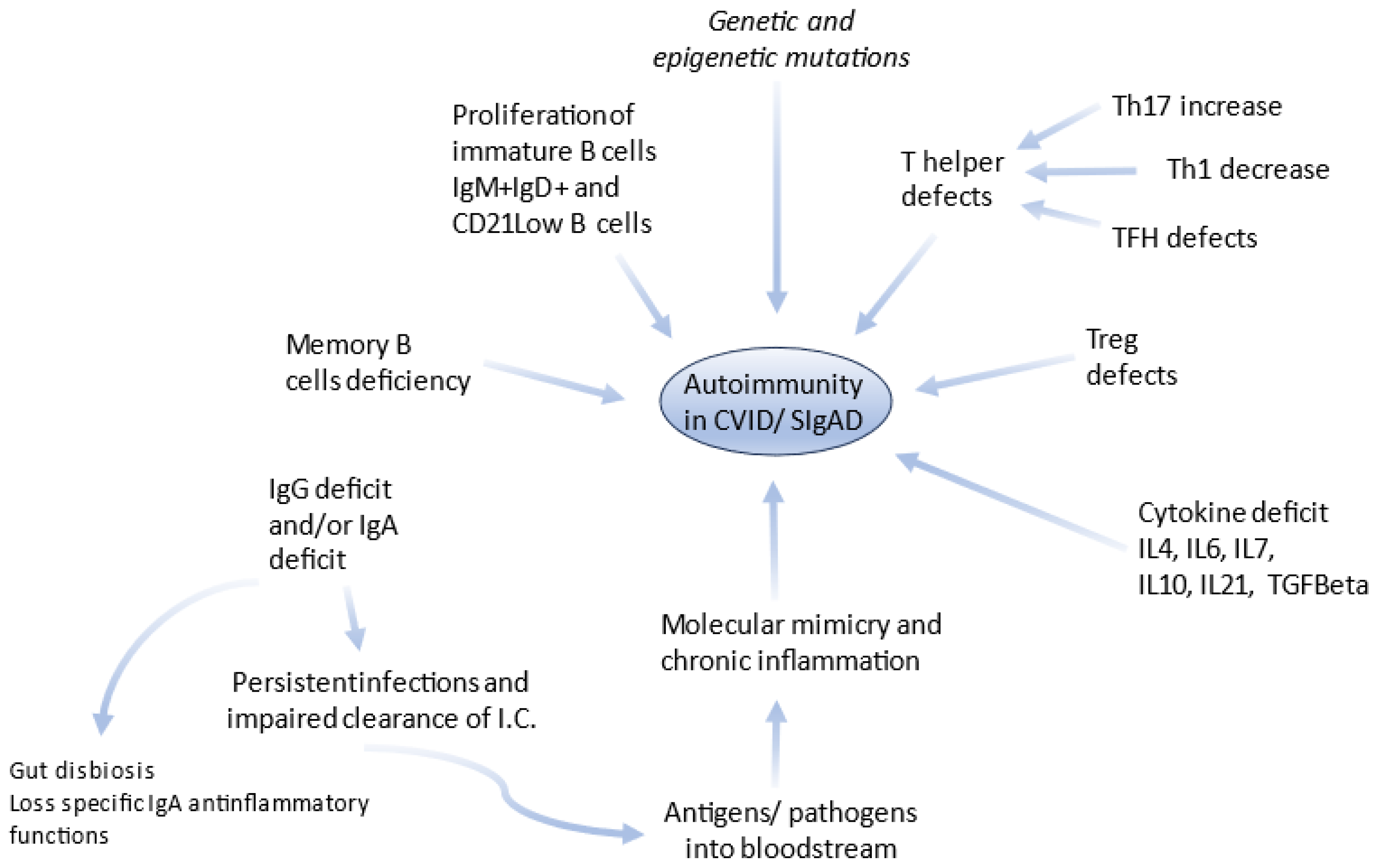
2.3. Pathogenetic Notes on CVID and Associated Autoimmunity
2.4. Clinical Manifestations
3. Selective IgA Deficiency
3.1. Epidemiology
3.2. Genetics
3.3. Pathogenetic Notes on SIgAD and Associated Autoimmunity
3.4. Clinical Phenotypes
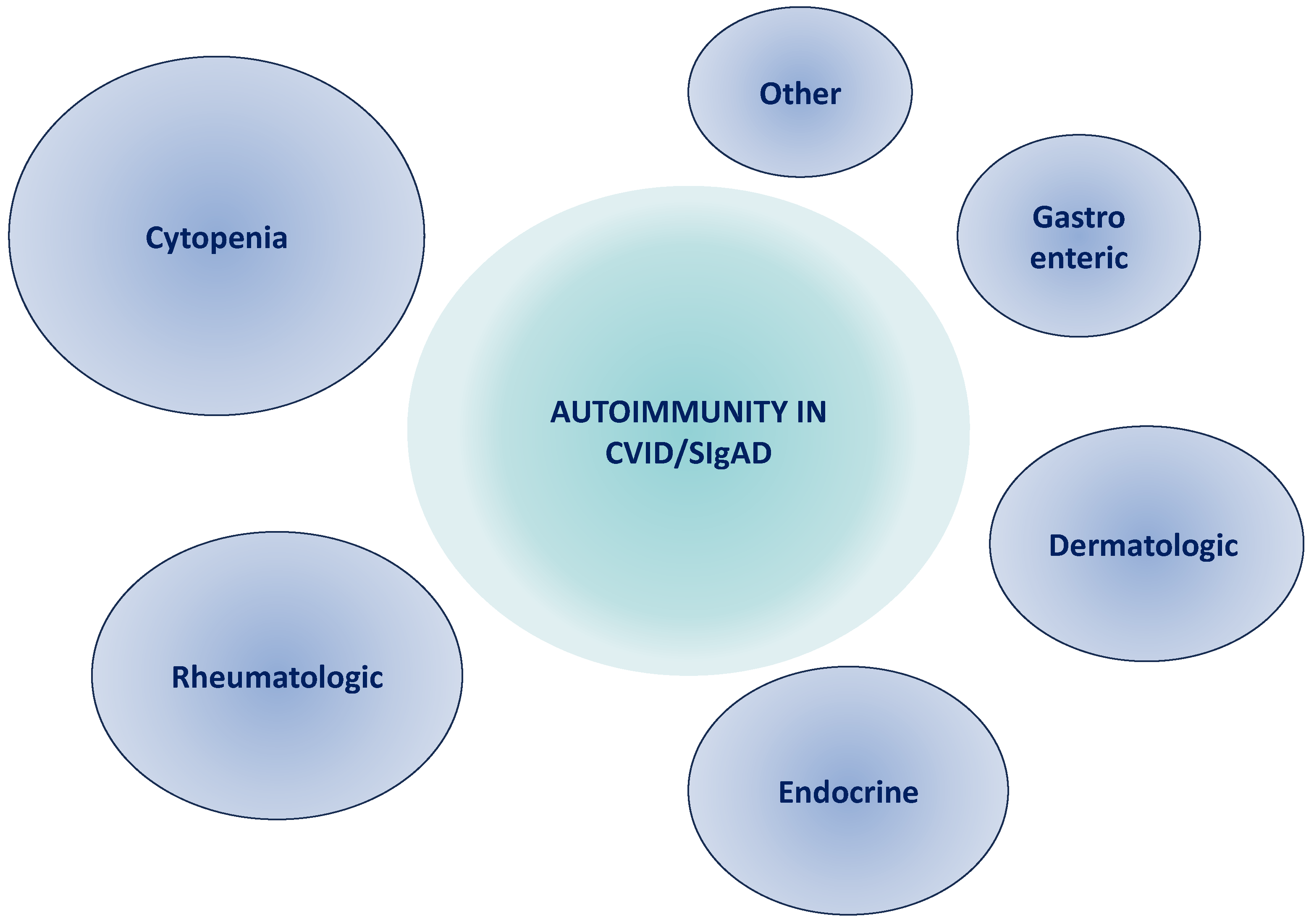
4. Autoimmune Manifestations in CVID and SIgAD
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Fischer, A.; Provot, J.; Jais, J.-P.; Alcais, A.; Mahlaoui, N.; Members of the CEREDIH French PID Study Group. Autoimmune and Inflammatory Manifestations Occur Frequently in Patients with Primary Immunodeficiencies. J. Allergy Clin. Immunol. 2017, 140, 1388–1393.e8. [Google Scholar] [CrossRef]
- Walter, J.E.; Ayala, I.A.; Milojevic, D. Autoimmunity as a Continuum in Primary Immunodeficiency. Curr. Opin. Pediatr. 2019, 31, 851–862. [Google Scholar] [CrossRef] [PubMed]
- Gavrilova, T. Primary Immunodeficiency with Severe Multi-Organ Immune Dysregulation. Case Rep. Immunol. 2019, 2019, 8746249. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, F.-S.; Gershwin, M.E. Human Autoimmune Diseases: A Comprehensive Update. J. Intern. Med. 2015, 278, 369–395. [Google Scholar] [CrossRef] [PubMed]
- Ray, D.; Yung, R. Immune Senescence, Epigenetics and Autoimmunity. Clin. Immunol. 2018, 196, 59–63. [Google Scholar] [CrossRef]
- Samuels, H.; Malov, M.; Saha Detroja, T.; Ben Zaken, K.; Bloch, N.; Gal-Tanamy, M.; Avni, O.; Polis, B.; Samson, A.O. Autoimmune Disease Classification Based on PubMed Text Mining. J. Clin. Med. 2022, 11, 4345. [Google Scholar] [CrossRef]
- Tuano, K.S.; Seth, N.; Chinen, J. Secondary Immunodeficiencies: An Overview. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2021, 127, 617–626. [Google Scholar] [CrossRef]
- Avery, R.K.; Pasternack, M.S. Approach to Adult Patients with Recurrent Infections. Cleve. Clin. J. Med. 1997, 64, 249–257. [Google Scholar] [CrossRef]
- Gathmann, B.; Grimbacher, B.; Beauté, J.; Dudoit, Y.; Mahlaoui, N.; Fischer, A.; Knerr, V.; Kindle, G.; ESID Registry Working Party. The European Internet-Based Patient and Research Database for Primary Immunodeficiencies: Results 2006–2008. Clin. Exp. Immunol. 2009, 157 (Suppl. S1), 3–11. [Google Scholar] [CrossRef]
- Miller, F.W. The Increasing Prevalence of Autoimmunity and Autoimmune Diseases: An Urgent Call to Action for Improved Understanding, Diagnosis, Treatment, and Prevention. Curr. Opin. Immunol. 2023, 80, 102266. [Google Scholar] [CrossRef]
- Tangye, S.G.; Al-Herz, W.; Bousfiha, A.; Cunningham-Rundles, C.; Franco, J.L.; Holland, S.M.; Klein, C.; Morio, T.; Oksenhendler, E.; Picard, C.; et al. Human Inborn Errors of Immunity: 2022 Update on the Classification from the International Union of Immunological Societies Expert Committee. J. Clin. Immunol. 2022, 42, 1473–1507. [Google Scholar] [CrossRef] [PubMed]
- Pinto, M.V.; Neves, J.F. Precision Medicine: The Use of Tailored Therapy in Primary Immunodeficiencies. Front. Immunol. 2022, 13, 1029560. [Google Scholar] [CrossRef] [PubMed]
- Boyle, J.M.; Buckley, R.H. Population Prevalence of Diagnosed Primary Immunodeficiency Diseases in the United States. J. Clin. Immunol. 2007, 27, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Modell, V.; Orange, J.S.; Quinn, J.; Modell, F. Global Report on Primary Immunodeficiencies: 2018 Update from the Jeffrey Modell Centers Network on Disease Classification, Regional Trends, Treatment Modalities, and Physician Reported Outcomes. Immunol. Res. 2018, 66, 367–380. [Google Scholar] [CrossRef]
- Abolhassani, H.; Azizi, G.; Sharifi, L.; Yazdani, R.; Mohsenzadegan, M.; Delavari, S.; Sohani, M.; Shirmast, P.; Chavoshzadeh, Z.; Mahdaviani, S.A.; et al. Global Systematic Review of Primary Immunodeficiency Registries. Expert Rev. Clin. Immunol. 2020, 16, 717–732. [Google Scholar] [CrossRef]
- Agarwal, S.; Cunningham-Rundles, C. Autoimmunity in Common Variable Immunodeficiency. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2019, 123, 454–460. [Google Scholar] [CrossRef]
- Agarwal, S.; Cunningham-Rundles, C. Autoimmunity in Common Variable Immunodeficiency. Curr. Allergy Asthma Rep. 2009, 9, 347–352. [Google Scholar] [CrossRef]
- Etzioni, A. Immune Deficiency and Autoimmunity. Autoimmun. Rev. 2003, 2, 364–369. [Google Scholar] [CrossRef]
- Eldeniz, F.C.; Gul, Y.; Yorulmaz, A.; Guner, S.N.; Keles, S.; Reisli, I. Evaluation of the 10 Warning Signs in Primary and Secondary Immunodeficient Patients. Front. Immunol. 2022, 13, 900055. [Google Scholar] [CrossRef]
- Keles, S.; Artac, H.; Kara, R.; Gokturk, B.; Ozen, A.; Reisli, I. Transient Hypogammaglobulinemia and Unclassified Hypogammaglobulinemia: “Similarities and Differences. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2010, 21, 843–851. [Google Scholar] [CrossRef]
- Bellutti Enders, F.; Conti, F.; Candotti, F.; Angelini, F. Transient hypogammaglobulinemia of infancy. Rev. Med. Suisse 2017, 13, 739–742. [Google Scholar] [PubMed]
- Aghamohammadi, A.; Mohammadi, J.; Parvaneh, N.; Rezaei, N.; Moin, M.; Espanol, T.; Hammarstrom, L. Progression of Selective IgA Deficiency to Common Variable Immunodeficiency. Int. Arch. Allergy Immunol. 2008, 147, 87–92. [Google Scholar] [CrossRef]
- Aghamohammadi, A.; Cheraghi, T.; Gharagozlou, M.; Movahedi, M.; Rezaei, N.; Yeganeh, M.; Parvaneh, N.; Abolhassani, H.; Pourpak, Z.; Moin, M. IgA Deficiency: Correlation between Clinical and Immunological Phenotypes. J. Clin. Immunol. 2009, 29, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Vořechovský, I.; Zetterquist, H.; Paganelli, R.; Koskinen, S.; David, A.; Webster, B.; Björkander, J.; Smith, C.I.E.; Hammarström, L. Family and Linkage Study of Selective IgA Deficiency and Common Variable Immunodeficiency. Clin. Immunol. Immunopathol. 1995, 77, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Finck, A.; Van Der Meer, J.W.M.; Schäffer, A.A.; Pfannstiel, J.; Fieschi, C.; Plebani, A.; Webster, A.D.B.; Hammarström, L.; Grimbacher, B. Linkage of Autosomal-Dominant Common Variable Immunodeficiency to Chromosome 4q. Eur. J. Hum. Genet. 2006, 14, 867–875. [Google Scholar] [CrossRef]
- Bonilla, F.A.; Barlan, I.; Chapel, H.; Costa-Carvalho, B.T.; Cunningham-Rundles, C.; De La Morena, M.T.; Espinosa-Rosales, F.J.; Hammarström, L.; Nonoyama, S.; Quinti, I.; et al. International Consensus Document (ICON): Common Variable Immunodeficiency Disorders. J. Allergy Clin. Immunol. Pract. 2016, 4, 38–59. [Google Scholar] [CrossRef]
- Del Pino-Molina, L.; Rodríguez-Ubreva, J.; Torres Canizales, J.; Coronel-Díaz, M.; Kulis, M.; Martín-Subero, J.I.; Van Der Burg, M.; Ballestar, E.; López-Granados, E. Impaired CpG Demethylation in Common Variable Immunodeficiency Associates With B Cell Phenotype and Proliferation Rate. Front. Immunol. 2019, 10, 878. [Google Scholar] [CrossRef]
- Bisgin, A.; Sonmezler, O.; Boga, I.; Yilmaz, M. The Impact of Rare and Low-Frequency Genetic Variants in Common Variable Immunodeficiency (CVID). Sci. Rep. 2021, 11, 8308. [Google Scholar] [CrossRef]
- Singh, A.; Joshi, V.; Jindal, A.K.; Mathew, B.; Rawat, A. An Updated Review on Activated PI3 Kinase Delta Syndrome (APDS). Genes Dis. 2020, 7, 67–74. [Google Scholar] [CrossRef]
- Fekrvand, S.; Khanmohammadi, S.; Abolhassani, H.; Yazdani, R. B- and T-Cell Subset Abnormalities in Monogenic Common Variable Immunodeficiency. Front. Immunol. 2022, 13, 912826. [Google Scholar] [CrossRef]
- Salzer, U.; Bacchelli, C.; Buckridge, S.; Pan-Hammarström, Q.; Jennings, S.; Lougaris, V.; Bergbreiter, A.; Hagena, T.; Birmelin, J.; Plebani, A.; et al. Relevance of Biallelic versus Monoallelic TNFRSF13B Mutations in Distinguishing Disease-Causing from Risk-Increasing TNFRSF13B Variants in Antibody Deficiency Syndromes. Blood 2009, 113, 1967–1976. [Google Scholar] [CrossRef]
- Vincent, F.B.; Saulep-Easton, D.; Figgett, W.A.; Fairfax, K.A.; Mackay, F. The BAFF/APRIL System: Emerging Functions beyond B Cell Biology and Autoimmunity. Cytokine Growth Factor Rev. 2013, 24, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Knight, A.K.; Radigan, L.; Marron, T.; Langs, A.; Zhang, L.; Cunningham-Rundles, C. High Serum Levels of BAFF, APRIL, and TACI in Common Variable Immunodeficiency. Clin. Immunol. Orlando Fla 2007, 124, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Gardam, S.; Brink, R. Non-Canonical NF-κB Signaling Initiated by BAFF Influences B Cell Biology at Multiple Junctures. Front. Immunol. 2014, 4, 509. [Google Scholar] [CrossRef] [PubMed]
- Ou, X.; Xu, S.; Lam, K.-P. Deficiency in TNFRSF13B (TACI) Expands T-Follicular Helper and Germinal Center B Cells via Increased ICOS-Ligand Expression but Impairs Plasma Cell Survival. Proc. Natl. Acad. Sci. USA 2012, 109, 15401–15406. [Google Scholar] [CrossRef] [PubMed]
- Kakkas, I.; Tsinti, G.; Kalala, F.; Farmaki, E.; Kourakli, A.; Kapousouzi, A.; Dimou, M.; Kalaitzidou, V.; Sevdali, E.; Peristeri, A.-M.; et al. TACI Mutations in Primary Antibody Deficiencies: A Nationwide Study in Greece. Medicina 2021, 57, 827. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, J.; Zhang, Y.-M.; Zhang, X.-M.; Tao, J. Effect of TACI Signaling on Humoral Immunity and Autoimmune Diseases. J. Immunol. Res. 2015, 2015, 247426. [Google Scholar] [CrossRef]
- Smulski, C.R.; Eibel, H. BAFF and BAFF-Receptor in B Cell Selection and Survival. Front. Immunol. 2018, 9, 2285. [Google Scholar] [CrossRef]
- Conley, M.E.; Dobbs, A.K.; Farmer, D.M.; Kilic, S.; Paris, K.; Grigoriadou, S.; Coustan-Smith, E.; Howard, V.; Campana, D. Primary B Cell Immunodeficiencies: Comparisons and Contrasts. Annu. Rev. Immunol. 2009, 27, 199–227. [Google Scholar] [CrossRef]
- DeFranco, A.L. The Germinal Center Antibody Response in Health and Disease. F1000Research 2016, 5, 999. [Google Scholar] [CrossRef]
- Warnatz, K.; Denz, A.; Dräger, R.; Braun, M.; Groth, C.; Wolff-Vorbeck, G.; Eibel, H.; Schlesier, M.; Peter, H.H. Severe Deficiency of Switched Memory B Cells (CD27+IgM−IgD−) in Subgroups of Patients with Common Variable Immunodeficiency: A New Approach to Classify a Heterogeneous Disease. Blood 2002, 99, 1544–1551. [Google Scholar] [CrossRef] [PubMed]
- Azizi, G.; Abolhassani, H.; Kiaee, F.; Tavakolinia, N.; Rafiemanesh, H.; Yazdani, R.; Mahdaviani, S.; Mohammadikhajehdehi, S.; Tavakol, M.; Ziaee, V.; et al. Autoimmunity and Its Association with Regulatory T Cells and B Cell Subsets in Patients with Common Variable Immunodeficiency. Allergol. Immunopathol. 2018, 46, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Ramón, S.; Radigan, L.; Yu, J.E.; Bard, S.; Cunningham-Rundles, C. Memory B Cells in Common Variable Immunodeficiency: Clinical Associations and Sex Differences. Clin. Immunol. 2008, 128, 314–321. [Google Scholar] [CrossRef]
- Hillier, K.; Kumar, S.; Roy, P.G.; Allard-Chamard, H.; Das, J.; Farmer, J.; Pillai, S. Expanded Autoreactive Transitional B Cells in Monogenic Common Variable Immunodeficiency. Blood 2022, 140 (Suppl. S1), 5505–5507. [Google Scholar] [CrossRef]
- Friman, V.; Quinti, I.; Davydov, A.N.; Shugay, M.; Farroni, C.; Engström, E.; Pour Akaber, S.; Barresi, S.; Mohamed, A.; Pulvirenti, F.; et al. Defective Peripheral B Cell Selection in Common Variable Immune Deficiency Patients with Autoimmune Manifestations. Cell Rep. 2023, 42, 112446. [Google Scholar] [CrossRef]
- Reincke, M.E.; Payne, K.J.; Harder, I.; Strohmeier, V.; Voll, R.E.; Warnatz, K.; Keller, B. The Antigen Presenting Potential of CD21low B Cells. Front. Immunol. 2020, 11, 535784. [Google Scholar] [CrossRef] [PubMed]
- Rakhmanov, M.; Keller, B.; Gutenberger, S.; Foerster, C.; Hoenig, M.; Driessen, G.; Van Der Burg, M.; Van Dongen, J.J.; Wiech, E.; Visentini, M.; et al. Circulating CD21low B Cells in Common Variable Immunodeficiency Resemble Tissue Homing, Innate-like B Cells. Proc. Natl. Acad. Sci. USA 2009, 106, 13451–13456. [Google Scholar] [CrossRef]
- Boileau, J.; Mouillot, G.; Gérard, L.; Carmagnat, M.; Rabian, C.; Oksenhendler, E.; Pasquali, J.-L.; Korganow, A.-S. Autoimmunity in Common Variable Immunodeficiency: Correlation with Lymphocyte Phenotype in the French DEFI Study. J. Autoimmun. 2011, 36, 25–32. [Google Scholar] [CrossRef]
- Wehr, C.; Kivioja, T.; Schmitt, C.; Ferry, B.; Witte, T.; Eren, E.; Vlkova, M.; Hernandez, M.; Detkova, D.; Bos, P.R.; et al. The EUROclass Trial: Defining Subgroups in Common Variable Immunodeficiency. Blood 2008, 111, 77–85. [Google Scholar] [CrossRef]
- Warnatz, K.; Schlesier, M. Flowcytometric Phenotyping of Common Variable Immunodeficiency. Cytom. B Clin. Cytom. 2008, 74B, 261–271. [Google Scholar] [CrossRef]
- Van Der Burg, M.; Kalina, T.; Perez-Andres, M.; Vlkova, M.; Lopez-Granados, E.; Blanco, E.; Bonroy, C.; Sousa, A.E.; Kienzler, A.-K.; Wentink, M.; et al. The EuroFlow PID Orientation Tube for Flow Cytometric Diagnostic Screening of Primary Immunodeficiencies of the Lymphoid System. Front. Immunol. 2019, 10, 246. [Google Scholar] [CrossRef] [PubMed]
- Roskin, K.M.; Simchoni, N.; Liu, Y.; Lee, J.-Y.; Seo, K.; Hoh, R.A.; Pham, T.; Park, J.H.; Furman, D.; Dekker, C.L.; et al. IgH Sequences in Common Variable Immune Deficiency Reveal Altered B Cell Development and Selection. Sci. Transl. Med. 2015, 7, 302ra135. [Google Scholar] [CrossRef] [PubMed]
- Ghraichy, M.; Galson, J.D.; Kelly, D.F.; Trück, J. B-Cell Receptor Repertoire Sequencing in Patients with Primary Immunodeficiency: A Review. Immunology 2018, 153, 145–160. [Google Scholar] [CrossRef]
- Hargreaves, C.E.; Salatino, S.; Sasson, S.C.; Charlesworth, J.E.G.; Bateman, E.; Patel, A.M.; Anzilotti, C.; Broxholme, J.; Knight, J.C.; Patel, S.Y. Decreased ATM Function Causes Delayed DNA Repair and Apoptosis in Common Variable Immunodeficiency Disorders. J. Clin. Immunol. 2021, 41, 1315–1330. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, L.; Mirshafiey, A.; Rezaei, N.; Azizi, G.; Magaji Hamid, K.; Amirzargar, A.A.; Asgardoon, M.H.; Aghamohammadi, A. The Role of Toll-like Receptors in B-Cell Development and Immunopathogenesis of Common Variable Immunodeficiency. Expert Rev. Clin. Immunol. 2016, 12, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Wehr, C.; Houet, L.; Unger, S.; Kindle, G.; Goldacker, S.; Grimbacher, B.; Caballero Garcia de Oteyza, A.; Marks, R.; Pfeifer, D.; Nieters, A.; et al. Altered Spectrum of Lymphoid Neoplasms in a Single-Center Cohort of Common Variable Immunodeficiency with Immune Dysregulation. J. Clin. Immunol. 2021, 41, 1250–1265. [Google Scholar] [CrossRef]
- Azizi, G.; Rezaei, N.; Kiaee, F.; Tavakolinia, N.; Yazdani, R.; Mirshafiey, A.; Aghamohammadi, A. T-Cell Abnormalities in Common Variable Immunodeficiency. J. Investig. Allergol. Clin. Immunol. 2016, 26, 233–243. [Google Scholar] [CrossRef]
- Bateman, E.A.L.; Ayers, L.; Sadler, R.; Lucas, M.; Roberts, C.; Woods, A.; Packwood, K.; Burden, J.; Harrison, D.; Kaenzig, N.; et al. T Cell Phenotypes in Patients with Common Variable Immunodeficiency Disorders: Associations with Clinical Phenotypes in Comparison with Other Groups with Recurrent Infections. Clin. Exp. Immunol. 2012, 170, 202–211. [Google Scholar] [CrossRef]
- Chawla, S.; Barman, P.; Tyagi, R.; Jindal, A.K.; Sharma, S.; Rawat, A.; Singh, S. Autoimmune Cytopenias in Common Variable Immunodeficiency Are a Diagnostic and Therapeutic Conundrum: An Update. Front. Immunol. 2022, 13, 869466. [Google Scholar] [CrossRef]
- Mouillot, G.; Carmagnat, M.; Gérard, L.; Garnier, J.-L.; Fieschi, C.; Vince, N.; Karlin, L.; Viallard, J.-F.; Jaussaud, R.; Boileau, J.; et al. B-Cell and T-Cell Phenotypes in CVID Patients Correlate with the Clinical Phenotype of the Disease. J. Clin. Immunol. 2010, 30, 746–755. [Google Scholar] [CrossRef]
- Rossi, S.; Baronio, M.; Gazzurelli, L.; Tessarin, G.; Baresi, G.; Chiarini, M.; Moratto, D.; Badolato, R.; Plebani, A.; Lougaris, V. Lymphocyte Alterations in Patients with Common Variable Immunodeficiency (CVID) and Autoimmune Manifestations. Clin. Immunol. 2022, 241, 109077. [Google Scholar] [CrossRef] [PubMed]
- Berbers, R.-M.; Van Der Wal, M.M.; Van Montfrans, J.M.; Ellerbroek, P.M.; Dalm, V.A.S.H.; Van Hagen, P.M.; Leavis, H.L.; Van Wijk, F. Chronically Activated T-Cells Retain Their Inflammatory Properties in Common Variable Immunodeficiency. J. Clin. Immunol. 2021, 41, 1621–1632. [Google Scholar] [CrossRef] [PubMed]
- Le Saos-Patrinos, C.; Loizon, S.; Blanco, P.; Viallard, J.-F.; Duluc, D. Functions of Tfh Cells in Common Variable Immunodeficiency. Front. Immunol. 2020, 11, 6. [Google Scholar] [CrossRef]
- Barreto De Oliveira, A.K.; Alcala Neves, M.A.; Salmazi, K.C.; Miraglia, J.; Barros, M.T.; Kalil, J.; Kokron, C. Evaluation of TH17 Profile in Common Variable Immunodeficiency Patients with or without Autoimmunity. World Allergy Organ. J. 2015, 8, A236. [Google Scholar] [CrossRef]
- Ganjalikhani-Hakemi, M.; Yazdani, R.; Sherkat, R.; Homayouni, V.; Masjedi, M.; Hosseini, M. Evaluation of the T Helper 17 Cell Specific Genes and the Innate Lymphoid Cells Counts in the Peripheral Blood of Patients with the Common Variable Immunodeficiency. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2014, 19 (Suppl. S1), S30–S35. [Google Scholar]
- Marwaha, A.K.; Leung, N.J.; McMurchy, A.N.; Levings, M.K. TH17 Cells in Autoimmunity and Immunodeficiency: Protective or Pathogenic? Front. Immunol. 2012, 3, 129. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, R.R.; Silva, S.P.; Silva, S.L.; Melo, A.C.; Pedro, E.; Barbosa, M.P.; Pereira-Santos, M.C.; Victorino, R.M.M.; Sousa, A.E. Primary B-Cell Deficiencies Reveal a Link between Human IL-17-Producing CD4 T-Cell Homeostasis and B-Cell Differentiation. PLoS ONE 2011, 6, e22848. [Google Scholar] [CrossRef]
- McGinley, A.M.; Sutton, C.E.; Edwards, S.C.; Leane, C.M.; DeCourcey, J.; Teijeiro, A.; Hamilton, J.A.; Boon, L.; Djouder, N.; Mills, K.H.G. Interleukin-17A Serves a Priming Role in Autoimmunity by Recruiting IL-1β-Producing Myeloid Cells That Promote Pathogenic T Cells. Immunity 2020, 52, 342–356.e6. [Google Scholar] [CrossRef]
- Rajendiran, A.; Tenbrock, K. Regulatory T Cell Function in Autoimmune Disease. J. Transl. Autoimmun. 2021, 4, 100130. [Google Scholar] [CrossRef]
- Azizi, G.; Hafezi, N.; Mohammadi, H.; Yazdani, R.; Alinia, T.; Tavakol, M.; Aghamohammadi, A.; Mirshafiey, A. Abnormality of Regulatory T Cells in Common Variable Immunodeficiency. Cell. Immunol. 2017, 315, 11–17. [Google Scholar] [CrossRef]
- Gupta, S.; Demirdag, Y.; Gupta, A.A. Members of the Regulatory Lymphocyte Club in Common Variable Immunodeficiency. Front. Immunol. 2022, 13, 864307. [Google Scholar] [CrossRef]
- Bacchetta, R.; Barzaghi, F.; Roncarolo, M.-G. From IPEX Syndrome to FOXP3 Mutation: A Lesson on Immune Dysregulation: IPEX Syndrome and FOXP3. Ann. N. Y. Acad. Sci. 2018, 1417, 5–22. [Google Scholar] [CrossRef]
- Ramesh, M.; Hamm, D.; Simchoni, N.; Cunningham-Rundles, C. Clonal and Constricted T Cell Repertoire in Common Variable Immune Deficiency. Clin. Immunol. 2017, 178, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Farrington, M.; Grosmaire, L.S.; Nonoyama, S.; Fischer, S.H.; Hollenbaugh, D.; Ledbetter, J.A.; Noelle, R.J.; Aruffo, A.; Ochs, H.D. CD40 Ligand Expression Is Defective in a Subset of Patients with Common Variable Immunodeficiency. Proc. Natl. Acad. Sci. USA 1994, 91, 1099–1103. [Google Scholar] [CrossRef] [PubMed]
- Aspalter, R.M.; Eibl, M.M.; Wolf, H.M. Defective T-Cell Activation Caused by Impairment of the TNF Receptor 2 Costimulatory Pathway in Common Variable Immunodeficiency. J. Allergy Clin. Immunol. 2007, 120, 1193–1200. [Google Scholar] [CrossRef]
- Jørgensen, S.F.; Trøseid, M.; Kummen, M.; Anmarkrud, J.A.; Michelsen, A.E.; Osnes, L.T.; Holm, K.; Høivik, M.L.; Rashidi, A.; Dahl, C.P.; et al. Altered Gut Microbiota Profile in Common Variable Immunodeficiency Associates with Levels of Lipopolysaccharide and Markers of Systemic Immune Activation. Mucosal Immunol. 2016, 9, 1455–1465. [Google Scholar] [CrossRef] [PubMed]
- Fiedorová, K.; Radvanský, M.; Bosák, J.; Grombiříková, H.; Němcová, E.; Králíčková, P.; Černochová, M.; Kotásková, I.; Lexa, M.; Litzman, J.; et al. Bacterial but Not Fungal Gut Microbiota Alterations Are Associated With Common Variable Immunodeficiency (CVID) Phenotype. Front. Immunol. 2019, 10, 1914. [Google Scholar] [CrossRef]
- Varricchi, G.; Poto, R.; Ianiro, G.; Punziano, A.; Marone, G.; Gasbarrini, A.; Spadaro, G. Gut Microbiome and Common Variable Immunodeficiency: Few Certainties and Many Outstanding Questions. Front. Immunol. 2021, 12, 712915. [Google Scholar] [CrossRef]
- Rojas, M.; Restrepo-Jiménez, P.; Monsalve, D.M.; Pacheco, Y.; Acosta-Ampudia, Y.; Ramírez-Santana, C.; Leung, P.S.C.; Ansari, A.A.; Gershwin, M.E.; Anaya, J.-M. Molecular Mimicry and Autoimmunity. J. Autoimmun. 2018, 95, 100–123. [Google Scholar] [CrossRef]
- Ghimire, L.; Paudel, S.; Jin, L.; Jeyaseelan, S. The NLRP6 Inflammasome in Health and Disease. Mucosal Immunol. 2020, 13, 388–398. [Google Scholar] [CrossRef]
- Ho, H.; Cunningham-Rundles, C. Seeking Relevant Biomarkers in Common Variable Immunodeficiency. Front. Immunol. 2022, 13, 857050. [Google Scholar] [CrossRef] [PubMed]
- Long, A.; Kleiner, A.; Looney, R.J. Immune Dysregulation. J. Allergy Clin. Immunol. 2023, 151, 70–80. [Google Scholar] [CrossRef]
- Chapel, H.; Lucas, M.; Lee, M.; Bjorkander, J.; Webster, D.; Grimbacher, B.; Fieschi, C.; Thon, V.; Abedi, M.R.; Hammarstrom, L. Common Variable Immunodeficiency Disorders: Division into Distinct Clinical Phenotypes. Blood 2008, 112, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Yazdani, R.; Habibi, S.; Sharifi, L.; Azizi, G.; Abolhassani, H.; Olbrich, P.; Aghamohammadi, A. Common Variable Immunodeficiency: Epidemiology, Pathogenesis, Clinical Manifestations, Diagnosis, Classification, and Management. J. Investig. Allergol. Clin. Immunol. 2020, 30, 14–34. [Google Scholar] [CrossRef] [PubMed]
- Wehr, C.; Gennery, A.R.; Lindemans, C.; Schulz, A.; Hoenig, M.; Marks, R.; Recher, M.; Gruhn, B.; Holbro, A.; Heijnen, I.; et al. Multicenter Experience in Hematopoietic Stem Cell Transplantation for Serious Complications of Common Variable Immunodeficiency. J. Allergy Clin. Immunol. 2015, 135, 988–997.e6. [Google Scholar] [CrossRef]
- Lacombe, V.; Lozac’h, P.; Orvain, C.; Lavigne, C.; Miot, C.; Pellier, I.; Urbanski, G. Traitement du PTI et de l’AHAI au cours du DICV: Revue systématique de la littérature. Rev. Méd. Interne 2019, 40, 491–500. [Google Scholar] [CrossRef]
- Health Quality Ontario. Home-Based Subcutaneous Infusion of Immunoglobulin for Primary and Secondary Immunodeficiencies: A Health Technology Assessment. Ont. Health Technol. Assess. Ser. 2017, 17, 1–86. [Google Scholar]
- Cunningham-Rundles, C. How I Treat Common Variable Immune Deficiency. Blood 2010, 116, 7–15. [Google Scholar] [CrossRef]
- Abolhassani, H.; Sagvand, B.T.; Shokuhfar, T.; Mirminachi, B.; Rezaei, N.; Aghamohammadi, A. A Review on Guidelines for Management and Treatment of Common Variable Immunodeficiency. Expert Rev. Clin. Immunol. 2013, 9, 561–575. [Google Scholar] [CrossRef]
- Hernandez-Trujillo, V.P.; Scalchunes, C.; Cunningham-Rundles, C.; Ochs, H.D.; Bonilla, F.A.; Paris, K.; Yel, L.; Sullivan, K.E. Autoimmunity and Inflammation in X-Linked Agammaglobulinemia. J. Clin. Immunol. 2014, 34, 627–632. [Google Scholar] [CrossRef]
- Costagliola, G.; Cappelli, S.; Consolini, R. Autoimmunity in Primary Immunodeficiency Disorders: An Updated Review on Pathogenic and Clinical Implications. J. Clin. Med. 2021, 10, 4729. [Google Scholar] [CrossRef] [PubMed]
- Pikkarainen, S.; Martelius, T.; Ristimäki, A.; Siitonen, S.; Seppänen, M.R.J.; Färkkilä, M. A High Prevalence of Gastrointestinal Manifestations in Common Variable Immunodeficiency. Am. J. Gastroenterol. 2019, 114, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Andersen, I.; Jørgensen, S. Gut Inflammation in CVID: Causes and Consequences. Expert Rev. Clin. Immunol. 2022, 18, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Quirós, A.; Solís-Sánchez, P.; Garrote-Adrados, J.A.; Arranz-Sanz, E. Common Variable Immunodeficiency. Old Questions Are Getting Clearer. Allergol. Immunopathol. 2006, 34, 263–275. [Google Scholar] [CrossRef]
- Ho, H.; Cunningham-Rundles, C. Non-Infectious Complications of Common Variable Immunodeficiency: Updated Clinical Spectrum, Sequelae, and Insights to Pathogenesis. Front. Immunol. 2020, 11, 149. [Google Scholar] [CrossRef]
- Kaarbø, M.; Yang, M.; Hov, J.R.; Holm, K.; De Sousa, M.M.L.; Macpherson, M.E.; Reims, H.M.; Kran, A.-M.B.; Halvorsen, B.; Karlsen, T.H.; et al. Duodenal Inflammation in Common Variable Immunodeficiency Has Altered Transcriptional Response to Viruses. J. Allergy Clin. Immunol. 2023, 151, 767–777. [Google Scholar] [CrossRef]
- Jørgensen, S.F.; Reims, H.M.; Aukrust, P.; Lundin, K.E.A.; Fevang, B. CVID and Celiac Disease. Am. J. Gastroenterol. 2017, 112, 393. [Google Scholar] [CrossRef]
- Maccaferri, S.; Vitali, B.; Klinder, A.; Kolida, S.; Ndagijimana, M.; Laghi, L.; Calanni, F.; Brigidi, P.; Gibson, G.R.; Costabile, A. Rifaximin Modulates the Colonic Microbiota of Patients with Crohn’s Disease: An in Vitro Approach Using a Continuous Culture Colonic Model System. J. Antimicrob. Chemother. 2010, 65, 2556–2565. [Google Scholar] [CrossRef]
- Malamut, G.; Verkarre, V.; Suarez, F.; Viallard, J.-F.; Lascaux, A.-S.; Cosnes, J.; Bouhnik, Y.; Lambotte, O.; Béchade, D.; Ziol, M.; et al. The Enteropathy Associated with Common Variable Immunodeficiency: The Delineated Frontiers with Celiac Disease. Am. J. Gastroenterol. 2010, 105, 2262–2275. [Google Scholar] [CrossRef]
- Fuss, I.J.; Friend, J.; Yang, Z.; He, J.P.; Hooda, L.; Boyer, J.; Xi, L.; Raffeld, M.; Kleiner, D.E.; Heller, T.; et al. Nodular Regenerative Hyperplasia in Common Variable Immunodeficiency. J. Clin. Immunol. 2013, 33, 748–758. [Google Scholar] [CrossRef]
- Cabañero-Navalon, M.D.; Garcia-Bustos, V.; Nuñez-Beltran, M.; Císcar Fernández, P.; Mateu, L.; Solanich, X.; Carrillo-Linares, J.L.; Robles-Marhuenda, Á.; Puchades-Gimeno, F.; Pelaez Ballesta, A.; et al. Current Clinical Spectrum of Common Variable Immunodeficiency in Spain: The Multicentric Nationwide GTEM-SEMI-CVID Registry. Front. Immunol. 2022, 13, 1033666. [Google Scholar] [CrossRef] [PubMed]
- Gobert, D.; Bussel, J.B.; Cunningham-Rundles, C.; Galicier, L.; Dechartres, A.; Berezne, A.; Bonnotte, B.; DeRevel, T.; Auzary, C.; Jaussaud, R.; et al. Efficacy and Safety of Rituximab in Common Variable Immunodeficiency-Associated Immune Cytopenias: A Retrospective Multicentre Study on 33 Patients: Efficacy and Safety of Rituximab. Br. J. Haematol. 2011, 155, 498–508. [Google Scholar] [CrossRef] [PubMed]
- Judson, M.A. Granulomatous Sarcoidosis Mimics. Front. Med. 2021, 8, 680989. [Google Scholar] [CrossRef]
- Ardeniz, Ö.; Cunningham-Rundles, C. Granulomatous Disease in Common Variable Immunodeficiency. Clin. Immunol. 2009, 133, 198–207. [Google Scholar] [CrossRef]
- Hurst, J.R.; Warnatz, K. Interstitial Lung Disease in Primary Immunodeficiency: Towards a Brighter Future. Eur. Respir. J. 2020, 55, 2000089. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.; Cunningham-Rundles, C. Lymphoid Malignancy in Common Variable Immunodeficiency in a Single-center Cohort. Eur. J. Haematol. 2021, 107, 503–516. [Google Scholar] [CrossRef]
- Salavoura, K.; Kolialexi, A.; Tsangaris, G.; Mavrou, A. Development of Cancer in Patients with Primary Immunodeficiencies. Anticancer Res. 2008, 28, 1263–1269. [Google Scholar]
- Piquer Gibert, M.; Alsina, L.; Giner Muñoz, M.T.; Cruz Martínez, O.; Ruiz Echevarria, K.; Dominguez, O.; Plaza Martín, A.M.; Arostegui, J.I.; De Valles, G.; Juan Otero, M.; et al. Non-Hodgkin Lymphoma in Pediatric Patients with Common Variable Immunodeficiency. Eur. J. Pediatr. 2015, 174, 1069–1076. [Google Scholar] [CrossRef][Green Version]
- Abolhassani, H.; Wang, Y.; Hammarström, L.; Pan-Hammarström, Q. Hallmarks of Cancers: Primary Antibody Deficiency Versus Other Inborn Errors of Immunity. Front. Immunol. 2021, 12, 720025. [Google Scholar] [CrossRef]
- Pulvirenti, F.; Pecoraro, A.; Cinetto, F.; Milito, C.; Valente, M.; Santangeli, E.; Crescenzi, L.; Rizzo, F.; Tabolli, S.; Spadaro, G.; et al. Gastric Cancer Is the Leading Cause of Death in Italian Adult Patients With Common Variable Immunodeficiency. Front. Immunol. 2018, 9, 2546. [Google Scholar] [CrossRef]
- Luca, L.; Beuvon, C.; Puyade, M.; Roblot, P.; Martin, M. Selective IgA deficiency. Rev. Med. Interne 2021, 42, 764–771. [Google Scholar] [CrossRef] [PubMed]
- Ammann, A.J.; Hong, R. Selective IgA Deficiency and Autoimmunity. Clin. Exp. Immunol. 1970, 7, 833–838. [Google Scholar] [PubMed]
- Swain, S.; Selmi, C.; Gershwin, M.E.; Teuber, S.S. The Clinical Implications of Selective IgA Deficiency. J. Transl. Autoimmun. 2019, 2, 100025. [Google Scholar] [CrossRef] [PubMed]
- Walker, A.M.; Kemp, A.S.; Hill, D.J.; Shelton, M.J. Features of Transient Hypogammaglobulinaemia in Infants Screened for Immunological Abnormalities. Arch. Dis. Child. 1994, 70, 183–186. [Google Scholar] [CrossRef][Green Version]
- Carneiro-Sampaio, M.M.; Carbonare, S.B.; Rozentraub, R.B.; de Araújo, M.N.; Riberiro, M.A.; Porto, M.H. Frequency of Selective IgA Deficiency among Brazilian Blood Donors and Healthy Pregnant Women. Allergol. Immunopathol. 1989, 17, 213–216. [Google Scholar]
- Al-Attas, R.A.; Rahi, A.H. Primary Antibody Deficiency in Arabs: First Report from Eastern Saudi Arabia. J. Clin. Immunol. 1998, 18, 368–371. [Google Scholar] [CrossRef]
- Pan-Hammarström, Q.; Hammarström, L. Antibody Deficiency Diseases. Eur. J. Immunol. 2008, 38, 327–333. [Google Scholar] [CrossRef]
- Kanoh, T.; Mizumoto, T.; Yasuda, N.; Koya, M.; Ohno, Y.; Uchino, H.; Yoshimura, K.; Ohkubo, Y.; Yamaguchi, H. Selective IgA Deficiency in Japanese Blood Donors: Frequency and Statistical Analysis. Vox Sang. 1986, 50, 81–86. [Google Scholar] [CrossRef]
- Karaca, N.E.; Severcan, E.U.; Bilgin, B.G.; Azarsiz, E.; Akarcan, S.; Gunaydın, N.C.; Gulez, N.; Genel, F.; Aksu, G.; Kutukculer, N. Familial Inheritance and Screening of First-Degree Relatives in Common Variable Immunodeficiency and Immunoglobulin A Deficiency Patients. Int. J. Immunopathol. Pharmacol. 2018, 32, 2058738418779458. [Google Scholar] [CrossRef]
- Ulfarsson, J.; Gudmundsson, S.; Birgisdóttir, B.; Kjeld, J.M.; Jensson, O. Selective Serum IgA Deficiency in Icelanders. Frequency, Family Studies and Ig Levels. Acta Med. Scand. 1982, 211, 481–487. [Google Scholar] [CrossRef]
- Schäffer, A.A.; Pfannstiel, J.; Webster, A.D.B.; Plebani, A.; Hammarström, L.; Grimbacher, B. Analysis of Families with Common Variable Immunodeficiency (CVID) and IgA Deficiency Suggests Linkage of CVID to Chromosome 16q. Hum. Genet. 2006, 118, 725–729. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, J.; Ramanujam, R.; Jarefors, S.; Rezaei, N.; Aghamohammadi, A.; Gregersen, P.K.; Hammarström, L. IgA Deficiency and the MHC: Assessment of Relative Risk and Microheterogeneity within the HLA A1 B8, DR3 (8.1) Haplotype. J. Clin. Immunol. 2010, 30, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Cooper, G.S.; Stroehla, B.C. The Epidemiology of Autoimmune Diseases. Autoimmun. Rev. 2003, 2, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Hov, J.R.; Zhong, H.; Qin, B.; Anmarkrud, J.A.; Holm, K.; Franke, A.; Lie, B.A.; Karlsen, T.H. The Influence of the Autoimmunity-Associated Ancestral HLA Haplotype AH8.1 on the Human Gut Microbiota: A Cross-Sectional Study. PLoS ONE 2015, 10, e0133804. [Google Scholar] [CrossRef]
- Di Lorenzo, B.; Pacillo, L.; Milardi, G.; Jofra, T.; Di Cesare, S.; Gerosa, J.; Marzinotto, I.; Zapparoli, E.; Rivalta, B.; Cifaldi, C.; et al. Natural History of Type 1 Diabetes on an Immunodysregulatory Background with Genetic Alteration in B-Cell Activating Factor Receptor: A Case Report. Front. Immunol. 2022, 13, 952715. [Google Scholar] [CrossRef]
- Muñiz-Castrillo, S.; Vogrig, A.; Honnorat, J. Associations between HLA and Autoimmune Neurological Diseases with Autoantibodies. Autoimmun. Highlights 2020, 11, 2. [Google Scholar] [CrossRef]
- Vidan-Jeras, B. When Type 1 Diabetes Meets Celiac Disease. HLA 2018, 92, 64–66. [Google Scholar] [CrossRef]
- Medrano, L.M.; Dema, B.; López-Larios, A.; Maluenda, C.; Bodas, A.; López-Palacios, N.; Figueredo, M.Á.; Fernández-Arquero, M.; Núñez, C. HLA and Celiac Disease Susceptibility: New Genetic Factors Bring Open Questions about the HLA Influence and Gene-Dosage Effects. PLoS ONE 2012, 7, e48403. [Google Scholar] [CrossRef]
- Carneiro-Sampaio, M.; Liphaus, B.L.; Jesus, A.A.; Silva, C.A.A.; Oliveira, J.B.; Kiss, M.H. Understanding Systemic Lupus Erythematosus Physiopathology in the Light of Primary Immunodeficiencies. J. Clin. Immunol. 2008, 28, 34–41. [Google Scholar] [CrossRef]
- Kumar, V.; Jarzabek-Chorzelska, M.; Sulej, J.; Karnewska, K.; Farrell, T.; Jablonska, S. Celiac Disease and Immunoglobulin A Deficiency: How Effective Are the Serological Methods of Diagnosis? Clin. Vaccine Immunol. 2002, 9, 1295–1300. [Google Scholar] [CrossRef]
- Cuoco, L.; Certo, M.; Jorizzo, R.A.; De Vitis, I.; Tursi, A.; Papa, A.; De Marinis, L.; Fedeli, P.; Fedeli, G.; Gasbarrini, G. Prevalence and Early Diagnosis of Coeliac Disease in Autoimmune Thyroid Disorders. Ital. J. Gastroenterol. Hepatol. 1999, 31, 283–287. [Google Scholar] [PubMed]
- Morley, J.E. An Overview of Diabetes Mellitus in Older Persons. Clin. Geriatr. Med. 1999, 15, 211–224. [Google Scholar] [CrossRef] [PubMed]
- Castigli, E.; Scott, S.; Dedeoglu, F.; Bryce, P.; Jabara, H.; Bhan, A.K.; Mizoguchi, E.; Geha, R.S. Impaired IgA Class Switching in APRIL-Deficient Mice. Proc. Natl. Acad. Sci. USA 2004, 101, 3903–3908. [Google Scholar] [CrossRef] [PubMed]
- Hammarström, L.; Vorechovsky, I.; Webster, D. Selective IgA Deficiency (SIgAD) and Common Variable Immunodeficiency (CVID). Clin. Exp. Immunol. 2000, 120, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Yel, L. Selective IgA Deficiency. J. Clin. Immunol. 2010, 30, 10–16. [Google Scholar] [CrossRef]
- Borte, S.; Pan-Hammarström, Q.; Liu, C.; Sack, U.; Borte, M.; Wagner, U.; Graf, D.; Hammarström, L. Interleukin-21 Restores Immunoglobulin Production Ex Vivo in Patients with Common Variable Immunodeficiency and Selective IgA Deficiency. Blood 2009, 114, 4089–4098. [Google Scholar] [CrossRef]
- Cao, A.T.; Yao, S.; Gong, B.; Nurieva, R.I.; Elson, C.O.; Cong, Y. Interleukin (IL)-21 Promotes Intestinal IgA Response to Microbiota. Mucosal Immunol. 2015, 8, 1072–1082. [Google Scholar] [CrossRef]
- Grosserichter-Wagener, C.; Franco-Gallego, A.; Ahmadi, F.; Moncada-Vélez, M.; Dalm, V.A.; Rojas, J.L.; Orrego, J.C.; Correa Vargas, N.; Hammarström, L.; Schreurs, M.W.; et al. Defective Formation of IgA Memory B Cells, Th1 and Th17 Cells in Symptomatic Patients with Selective IgA Deficiency. Clin. Transl. Immunol. 2020, 9, e1130. [Google Scholar] [CrossRef]
- Russell, M.W. Biological Functions of IgA. In Mucosal Immune Defense: Immunoglobulin A; Kaetzel, C.S., Ed.; Springer: Boston, MA, USA, 2007; pp. 144–172. [Google Scholar] [CrossRef]
- Monteiro, R.C. Immunoglobulin A as an Anti-Inflammatory Agent: Anti-Inflammatory Properties of IgA. Clin. Exp. Immunol. 2014, 178, 108–110. [Google Scholar] [CrossRef]
- Catanzaro, J.R.; Strauss, J.D.; Bielecka, A.; Porto, A.F.; Lobo, F.M.; Urban, A.; Schofield, W.B.; Palm, N.W. IgA-Deficient Humans Exhibit Gut Microbiota Dysbiosis despite Secretion of Compensatory IgM. Sci. Rep. 2019, 9, 13574. [Google Scholar] [CrossRef]
- Takeuchi, T.; Ohno, H. IgA in Human Health and Diseases: Potential Regulator of Commensal Microbiota. Front. Immunol. 2022, 13, 1024330. [Google Scholar] [CrossRef]
- Bagheri, Y.; Moeini Shad, T.; Namazi, S.; Tofighi Zavareh, F.; Azizi, G.; Salami, F.; Sadani, S.; Hosseini, A.; Saeidi, M.; Pashangzadeh, S.; et al. B Cells and T Cells Abnormalities in Patients with Selective IgA Deficiency. Allergy Asthma Clin. Immunol. 2023, 19, 23. [Google Scholar] [CrossRef] [PubMed]
- Dardalhon, V.; Korn, T.; Kuchroo, V.K.; Anderson, A.C. Role of Th1 and Th17 Cells in Organ-Specific Autoimmunity. J. Autoimmun. 2008, 31, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Crane, I.J.; Forrester, J.V. Th1 and Th2 Lymphocytes in Autoimmune Disease. Crit. Rev. Immunol. 2005, 25, 75–102. [Google Scholar] [CrossRef] [PubMed]
- Allenspach, E.; Torgerson, T.R. Autoimmunity and Primary Immunodeficiency Disorders. J. Clin. Immunol. 2016, 36 (Suppl. S1), 57–67. [Google Scholar] [CrossRef] [PubMed]
- Soheili, H.; Abolhassani, H.; Arandi, N.; Khazaei, H.A.; Shahinpour, S.; Hirbod-Mobarakeh, A.; Rezaei, N.; Aghamohammadi, A. Evaluation of Natural Regulatory T Cells in Subjects with Selective IgA Deficiency: From Senior Idea to Novel Opportunities. Int. Arch. Allergy Immunol. 2013, 160, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Cunningham-Rundles, C. Physiology of IgA and IgA Deficiency. J. Clin. Immunol. 2001, 21, 303–309. [Google Scholar] [CrossRef]
- Mella, M.A.; Lavrinienko, A.; Akhi, R.; Hindström, R.; Nissinen, A.E.; Wang, C.; Kullaa, A.; Salo, T.; Auvinen, J.; Koskimäki, J.J.; et al. Compensatory IgM to the Rescue: Patients with Selective IgA Deficiency Have Increased Natural IgM Antibodies to MAA–LDL and No Changes in Oral Microbiota. ImmunoHorizons 2021, 5, 170–181. [Google Scholar] [CrossRef]
- Zhang, J.; Van Oostrom, D.; Li, J.; Savelkoul, H.F.J. Innate Mechanisms in Selective IgA Deficiency. Front. Immunol. 2021, 12, 649112. [Google Scholar] [CrossRef]
- Latiff, A.H.A.; Kerr, M.A. The Clinical Significance of Immunoglobulin A Deficiency. Ann. Clin. Biochem. Int. J. Lab. Med. 2007, 44, 131–139. [Google Scholar] [CrossRef]
- Demirdag, Y.Y.; Gupta, S. Update on Infections in Primary Antibody Deficiencies. Front. Immunol. 2021, 12, 634181. [Google Scholar] [CrossRef]
- Magen, E.; Waitman, D.-A.; Goldstein, N.; Schlesinger, M.; Dickstein, Y.; Kahan, N.R. Helicobacter Pylori Infection in Patients with Selective Immunoglobulin a Deficiency. Clin. Exp. Immunol. 2016, 184, 332–337. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koenen, M.H.; Bosma, M.; Roorda, U.A.; Wopereis, F.M.; Roos, A.; van der Vries, E.; Bogaert, D.; Sanders, E.A.; Boes, M.; Heidema, J.; et al. A Novel Method to Standardise Serum IgA Measurements Shows an Increased Prevalence of IgA Deficiency in Young Children with Recurrent Respiratory Tract Infections. Clin. Transl. Immunol. 2021, 10, e1344. [Google Scholar] [CrossRef] [PubMed]
- Padda, J.; Khalid, K.; Cooper, A.C.; Jean-Charles, G. Association Between Helicobacter Pylori and Gastric Carcinoma. Cureus 2021, 13, e15165. [Google Scholar] [CrossRef] [PubMed]
- Washington, K.; Stenzel, T.T.; Buckley, R.H.; Gottfried, M.R. Gastrointestinal Pathology in Patients with Common Variable Immunodeficiency and X-Linked Agammaglobulinemia. Am. J. Surg. Pathol. 1996, 20, 1240–1252. [Google Scholar] [CrossRef]
- Albuquerque, A. Nodular Lymphoid Hyperplasia in the Gastrointestinal Tract in Adult Patients: A Review. World J. Gastrointest. Endosc. 2014, 6, 534–540. [Google Scholar] [CrossRef]
- Lilic, D. IgA Deficiency: What We Should--or Should Not--Be Doing. J. Clin. Pathol. 2001, 54, 337–338. [Google Scholar] [CrossRef]
- Abrahamian, F.; Agrawal, S.; Gupta, S. Immunological and Clinical Profile of Adult Patients with Selective Immunoglobulin Subclass Deficiency: Response to Intravenous Immunoglobulin Therapy. Clin. Exp. Immunol. 2010, 159, 344–350. [Google Scholar] [CrossRef]
- Bohländer, F. A New Hope? Possibilities of Therapeutic IgA Antibodies in the Treatment of Inflammatory Lung Diseases. Front. Immunol. 2023, 14, 1127339. [Google Scholar] [CrossRef]
- Cinicola, B.L.; Pulvirenti, F.; Capponi, M.; Bonetti, M.; Brindisi, G.; Gori, A.; De Castro, G.; Anania, C.; Duse, M.; Zicari, A.M. Selective IgA Deficiency and Allergy: A Fresh Look to an Old Story. Medicina 2022, 58, 129. [Google Scholar] [CrossRef]
- Janzi, M.; Kull, I.; Sjöberg, R.; Wan, J.; Melén, E.; Bayat, N.; Ostblom, E.; Pan-Hammarström, Q.; Nilsson, P.; Hammarström, L. Selective IgA Deficiency in Early Life: Association to Infections and Allergic Diseases during Childhood. Clin. Immunol. 2009, 133, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Shahin, R.Y.; Ali, F.H.A.; Melek, N.A.N.; Elateef, I.A.A.; Attia, M.Y. Study of Selective Immunoglobulin A Deficiency among Egyptian Patients with Food Allergy. Cent. Eur. J. Immunol. 2020, 45, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Tuano, K.S.; Orange, J.S.; Sullivan, K.; Cunningham-Rundles, C.; Bonilla, F.A.; Davis, C.M. Food Allergy in Patients with Primary Immunodeficiency Diseases: Prevalence within the US Immunodeficiency Network (USIDNET). J. Allergy Clin. Immunol. 2015, 135, 273–275. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Moschese, V.; Chini, L.; Graziani, S.; Sgrulletti, M.; Gallo, V.; Di Matteo, G.; Ferrari, S.; Di Cesare, S.; Cirillo, E.; Pession, A.; et al. Follow-up and Outcome of Symptomatic Partial or Absolute IgA Deficiency in Children. Eur. J. Pediatr. 2019, 178, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Erkoçoğlu, M.; Metin, A.; Kaya, A.; Özcan, C.; Akan, A.; Civelek, E.; Çapanoğlu, M.; Giniş, T.; Kocabaş, C.N. Allergic and Autoimmune Disorders in Families with Selective IgA Deficiency. Turk. J. Med. Sci. 2017, 47, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Rachid, R.; Bonilla, F.A. The Role of Anti-IgA Antibodies in Causing Adverse Reactions to Gamma Globulin Infusion in Immunodeficient Patients: A Comprehensive Review of the Literature. J. Allergy Clin. Immunol. 2012, 129, 628–634. [Google Scholar] [CrossRef]
- Rachid, R.; Castells, M.; Cunningham-Rundles, C.; Bonilla, F.A. Association of Anti-IgA Antibodies with Adverse Reactions to γ-Globulin Infusion. J. Allergy Clin. Immunol. 2011, 128, 228–230.e1. [Google Scholar] [CrossRef]
- Mayor, P.C.; Eng, K.H.; Singel, K.L.; Abrams, S.I.; Odunsi, K.; Moysich, K.B.; Fuleihan, R.; Garabedian, E.; Lugar, P.; Ochs, H.D.; et al. Cancer in Primary Immunodeficiency Diseases: Cancer Incidence in the United States Immune Deficiency Network Registry. J. Allergy Clin. Immunol. 2018, 141, 1028–1035. [Google Scholar] [CrossRef]
- Ludvigsson, J.F.; Neovius, M.; Ye, W.; Hammarström, L. IgA Deficiency and Risk of Cancer: A Population-Based Matched Cohort Study. J. Clin. Immunol. 2015, 35, 182–188. [Google Scholar] [CrossRef]
- Mellemkjær, L.; Hammarström, L.; Andersen, V.; Yuen, J.; Heilmann, C.; Barington, T.; Björkander, J.; Olsen, J.H. Cancer Risk among Patients with IgA Deficiency or Common Variable Immunodeficiency and Their Relatives: A Combined Danish and Swedish Study. Clin. Exp. Immunol. 2002, 130, 495–500. [Google Scholar] [CrossRef]
- Satgé, D. A Tumor Profile in Primary Immune Deficiencies Challenges the Cancer Immune Surveillance Concept. Front. Immunol. 2018, 9, 1149. [Google Scholar] [CrossRef] [PubMed]
- Gernert, M.; Kiesel, M.; Fröhlich, M.; Renner, R.; Strunz, P.-P.; Portegys, J.; Tony, H.-P.; Schmalzing, M.; Schwaneck, E.C. High Prevalence of Genital Human Papillomavirus Infection in Patients With Primary Immunodeficiencies. Front. Immunol. 2021, 12, 789345. [Google Scholar] [CrossRef] [PubMed]
- Hewavisenti, R.V.; Arena, J.; Ahlenstiel, C.L.; Sasson, S.C. Human Papillomavirus in the Setting of Immunodeficiency: Pathogenesis and the Emergence of next-Generation Therapies to Reduce the High Associated Cancer Risk. Front. Immunol. 2023, 14, 1112513. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, F.S.; Zainaldain, H.; Rafiemanesh, H.; Jamee, M.; Hossein-Khannazer, N.; Hamedifar, H.; Sabzevari, A.; Yazdani, R.; Abolhassani, H.; Aghamohammadi, A.; et al. Autoimmunity in Common Variable Immunodeficiency: A Systematic Review and Meta-Analysis. Expert Rev. Clin. Immunol. 2020, 16, 1227–1235. [Google Scholar] [CrossRef] [PubMed]
- Odineal, D.D.; Gershwin, M.E. The Epidemiology and Clinical Manifestations of Autoimmunity in Selective IgA Deficiency. Clin. Rev. Allergy Immunol. 2020, 58, 107–133. [Google Scholar] [CrossRef]
- Conrad, N.; Misra, S.; Verbakel, J.Y.; Verbeke, G.; Molenberghs, G.; Taylor, P.N.; Mason, J.; Sattar, N.; McMurray, J.J.V.; McInnes, I.B.; et al. Incidence, Prevalence, and Co-Occurrence of Autoimmune Disorders over Time and by Age, Sex, and Socioeconomic Status: A Population-Based Cohort Study of 22 Million Individuals in the UK. Lancet 2023, 401, 1878–1890. [Google Scholar] [CrossRef]
- Sohn, E. Why Autoimmunity Is Most Common in Women. Nature 2021, 595, S51–S53. [Google Scholar] [CrossRef]
- Xiang, Z.; Yang, Y.; Chang, C.; Lu, Q. The Epigenetic Mechanism for Discordance of Autoimmunity in Monozygotic Twins. J. Autoimmun. 2017, 83, 43–50. [Google Scholar] [CrossRef]
- Bogdanos, D.P.; Smyk, D.S.; Rigopoulou, E.I.; Mytilinaiou, M.G.; Heneghan, M.A.; Selmi, C.; Eric Gershwin, M. Twin Studies in Autoimmune Disease: Genetics, Gender and Environment. J. Autoimmun. 2012, 38, J156–J169. [Google Scholar] [CrossRef]
- Barka, N.; Shen, G.Q.; Shoenfeld, Y.; Alosachie, I.J.; Gershwin, M.E.; Reyes, H.; Peter, J.B. Multireactive Pattern of Serum Autoantibodies in Asymptomatic Individuals with Immunoglobulin A Deficiency. Clin. Diagn. Lab. Immunol. 1995, 2, 469–472. [Google Scholar] [CrossRef]
- Delogu, L.G.; Deidda, S.; Delitala, G.; Manetti, R. Infectious Diseases and Autoimmunity. J. Infect. Dev. Ctries. 2011, 5, 679–687. [Google Scholar] [CrossRef] [PubMed]
- Turpin, D.; Furudoi, A.; Parrens, M.; Blanco, P.; Viallard, J.-F.; Duluc, D. Increase of Follicular Helper T Cells Skewed toward a Th1 Profile in CVID Patients with Non-Infectious Clinical Complications. Clin. Immunol. 2018, 197, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Abolhassani, H.; Gharib, B.; Shahinpour, S.; Masoom, S.N.; Havaei, A.; Mirminachi, B.; Arandi, N.; Torabi-Sagvand, B.; Khazaei, H.A.; Mohammadi, J.; et al. Autoimmunity in Patients with Selective IgA Deficiency. J. Investig. Allergol. Clin. Immunol. 2015, 25, 112–119. [Google Scholar] [PubMed]
- Resnick, E.S.; Moshier, E.L.; Godbold, J.H.; Cunningham-Rundles, C. Morbidity and Mortality in Common Variable Immune Deficiency over 4 Decades. Blood 2012, 119, 1650–1657. [Google Scholar] [CrossRef]
- Feuille, E.J.; Anooshiravani, N.; Sullivan, K.E.; Fuleihan, R.L.; Cunningham-Rundles, C. Autoimmune Cytopenias and Associated Conditions in CVID: A Report From the USIDNET Registry. J. Clin. Immunol. 2018, 38, 28–34. [Google Scholar] [CrossRef]
- Patuzzo, G.; Barbieri, A.; Tinazzi, E.; Veneri, D.; Argentino, G.; Moretta, F.; Puccetti, A.; Lunardi, C. Autoimmunity and Infection in Common Variable Immunodeficiency (CVID). Autoimmun. Rev. 2016, 15, 877–882. [Google Scholar] [CrossRef]
- Chen, Y.; Hu, J.; Chen, Y. Platelet Desialylation and TFH Cells–the Novel Pathway of Immune Thrombocytopenia. Exp. Hematol. Oncol. 2021, 10, 21. [Google Scholar] [CrossRef]
- Tinazzi, E.; Osti, N.; Beri, R.; Argentino, G.; Veneri, D.; Dima, F.; Bason, C.; Jadav, G.; Dolcino, M.; Puccetti, A.; et al. Pathogenesis of Immune Thrombocytopenia in Common Variable Immunodeficiency. Autoimmun. Rev. 2020, 19, 102616. [Google Scholar] [CrossRef]
- Gathmann, B.; Mahlaoui, N.; Gérard, L.; Oksenhendler, E.; Warnatz, K.; Schulze, I.; Kindle, G.; Kuijpers, T.W.; Van Beem, R.T.; Guzman, D.; et al. Clinical Picture and Treatment of 2212 Patients with Common Variable Immunodeficiency. J. Allergy Clin. Immunol. 2014, 134, 116–126.e11. [Google Scholar] [CrossRef]
- Maglione, P.J. Autoimmune and Lymphoproliferative Complications of Common Variable Immunodeficiency. Curr. Allergy Asthma Rep. 2016, 16, 19. [Google Scholar] [CrossRef]
- Quinti, I.; Soresina, A.; Spadaro, G.; Martino, S.; Donnanno, S.; Agostini, C.; Claudio, P.; Franco, D.; Maria Pesce, A.; Borghese, F.; et al. Long-Term Follow-Up and Outcome of a Large Cohort of Patients with Common Variable Immunodeficiency. J. Clin. Immunol. 2007, 27, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Ghorbani, M.; Fekrvand, S.; Shahkarami, S.; Yazdani, R.; Sohani, M.; Shaghaghi, M.; Hassanpour, G.; Mohammadi, J.; Negahdari, B.; Abolhassani, H.; et al. The Evaluation of Neutropenia in Common Variable Immune Deficiency Patients. Expert Rev. Clin. Immunol. 2019, 15, 1225–1233. [Google Scholar] [CrossRef] [PubMed]
- Malphettes, M.; Gérard, L.; Carmagnat, M.; Mouillot, G.; Vince, N.; Boutboul, D.; Bérezné, A.; Nove-Josserand, R.; Lemoing, V.; Tetu, L.; et al. Late-Onset Combined Immune Deficiency: A Subset of Common Variable Immunodeficiency with Severe T Cell Defect. Clin. Infect. Dis. 2009, 49, 1329–1338. [Google Scholar] [CrossRef] [PubMed]
- Somasundaram, N.; Meyer, O.; Scheibenbogen, C.; Hanitsch, L.G.; Stittrich, A.; Kölsch, U.; Wittke, K. Clinical and Immunological Characterisation of Patients with Common Variable Immunodeficiency Related Immune Thrombocytopenia. Clin. Exp. Med. 2023. [Google Scholar] [CrossRef]
- Almizraq, R.J.; Branch, D.R. Efficacy and Mechanism of Intravenous Immunoglobulin Treatment for Immune Thrombocytopenia in Adults. Ann. Blood 2021, 6, 2. [Google Scholar] [CrossRef]
- Hantaweepant, C.; Pairattanakorn, P.; Karaketklang, K.; Owattanapanich, W.; Chinthammitr, Y. Efficacy and Safety of Second-Line Treatment in Thai Patients with Primary Warm-Type Autoimmune Hemolytic Anemia. Hematology 2019, 24, 720–726. [Google Scholar] [CrossRef]
- Lopes, J.P.; Ho, H.; Cunningham-Rundles, C. Interstitial Lung Disease in Common Variable Immunodeficiency. Front. Immunol. 2021, 12, 605945. [Google Scholar] [CrossRef]
- Yazdani, R.; Abolhassani, H.; Asgardoon, M.; Shaghaghi, M.; Modaresi, M.; Azizi, G.; Aghamohammadi, A. Infectious and Noninfectious Pulmonary Complications in Patients With Primary Immunodeficiency Disorders. J. Investig. Allergol. Clin. Immunol. 2017, 27, 213–224. [Google Scholar] [CrossRef]
- Casal, A.; Riveiro, V.; Suárez-Antelo, J.; Ferreiro, L.; Rodríguez-Núñez, N.; Lama, A.; Toubes, M.E.; Valdés, L. Pulmonary Manifestations of Primary Humoral Deficiencies. Can. Respir. J. 2022, 2022, 7140919. [Google Scholar] [CrossRef]
- Larsen, B.T.; Smith, M.L.; Tazelaar, H.D.; Yi, E.S.; Ryu, J.H.; Churg, A. GLILD Revisited: Pulmonary Pathology of Common Variable and Selective IgA Immunodeficiency. Am. J. Surg. Pathol. 2020, 44, 1073–1081. [Google Scholar] [CrossRef]
- Boursiquot, J.-N.; Gérard, L.; Malphettes, M.; Fieschi, C.; Galicier, L.; Boutboul, D.; Borie, R.; Viallard, J.-F.; Soulas-Sprauel, P.; Berezne, A.; et al. Granulomatous Disease in CVID: Retrospective Analysis of Clinical Characteristics and Treatment Efficacy in a Cohort of 59 Patients. J. Clin. Immunol. 2013, 33, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Twomey, J.J.; Jordan, P.H.; Jarrold, T.; Trubowitz, S.; Ritz, N.D.; Conn, H.O. The Syndrome of Immunoglobulin Deficiency and Pernicious Anemia. Am. J. Med. 1969, 47, 340–350. [Google Scholar] [CrossRef] [PubMed]
- Motta-Raymundo, A.; Rosmaninho, P.; Santos, D.F.; Ferreira, R.D.; Silva, S.P.; Ferreira, C.; Sousa, A.E.; Silva, S.L. Contribution of Helicobacter Pylori to the Inflammatory Complications of Common Variable Immunodeficiency. Front. Immunol. 2022, 13, 834137. [Google Scholar] [CrossRef] [PubMed]
- Wroblewski, L.E.; Peek, R.M.; Wilson, K.T. Helicobacter Pylori and Gastric Cancer: Factors That Modulate Disease Risk. Clin. Microbiol. Rev. 2010, 23, 713–739. [Google Scholar] [CrossRef] [PubMed]
- Jacob, C.M.A.; Pastorino, A.C.; Fahl, K.; Carneiro-Sampaio, M.; Monteiro, R.C. Autoimmunity in IgA Deficiency: Revisiting the Role of IgA as a Silent Housekeeper. J. Clin. Immunol. 2008, 28, 56–61. [Google Scholar] [CrossRef]
- Rojas, O.-L.; Rojas-Villarraga, A.; Cruz-Tapias, P.; Sánchez, J.L.; Suárez-Escudero, J.-C.; Patarroyo, M.-A.; Anaya, J.-M. HLA Class II Polymorphism in Latin American Patients with Multiple Sclerosis. Autoimmun. Rev. 2010, 9, 407–413. [Google Scholar] [CrossRef]
- Umemura, T.; Katsuyama, Y.; Yoshizawa, K.; Kimura, T.; Joshita, S.; Komatsu, M.; Matsumoto, A.; Tanaka, E.; Ota, M. Human Leukocyte Antigen Class II Haplotypes Affect Clinical Characteristics and Progression of Type 1 Autoimmune Hepatitis in Japan. PLoS ONE 2014, 9, e100565. [Google Scholar] [CrossRef]
- Song, J.; Lleo, A.; Yang, G.X.; Zhang, W.; Bowlus, C.L.; Gershwin, M.E.; Leung, P.S.C. Common Variable Immunodeficiency and Liver Involvement. Clin. Rev. Allergy Immunol. 2018, 55, 340–351. [Google Scholar] [CrossRef]
- Ward, C.; Lucas, M.; Piris, J.; Collier, J.; Chapel, H. Abnormal Liver Function in Common Variable Immunodeficiency Disorders Due to Nodular Regenerative Hyperplasia. Clin. Exp. Immunol. 2008, 153, 331–337. [Google Scholar] [CrossRef]
- Myneedu, K.; Chavez, L.O.; Sussman, N.L.; Michael, M.; Padilla, A.; Zuckerman, M.J. Autoimmune Hepatitis in a Patient With Common Variable Immunodeficiency. ACG Case Rep. J. 2021, 8, e00547. [Google Scholar] [CrossRef]
- Queirós, P.D.O.; Sousa Martín, J.M. Autoimmune Hepatitis as a Complication of Common Variable Immunodeficiency. Rev. Esp. Enferm. Dig. 2018, 110, 212–213. [Google Scholar] [CrossRef] [PubMed]
- Lima, F.M.S.; Toledo-Barros, M.; Alves, V.A.F.; Duarte, M.I.S.; Takakura, C.; Bernardes-Silva, C.F.; Marinho, A.K.B.B.; Grecco, O.; Kalil, J.; Kokron, C.M. Liver Disease Accompanied by Enteropathy in Common Variable Immunodeficiency: Common Pathophysiological Mechanisms. Front. Immunol. 2022, 13, 933463. [Google Scholar] [CrossRef] [PubMed]
- James, S.P.; Jones, E.A.; Schafer, D.F.; Hoofnagle, J.H.; Varma, R.R.; Strober, W. Selective Immimoglobulin a Deficiency Associated with Primary Biliary Cirrhosis in a Family with Liver Disease. Gastroenterology 1986, 90, 283–288. [Google Scholar] [CrossRef]
- Boyer, J.L. Idiopathic Portal Hypertension: Comparison with the Portal Hypertension of Cirrhosis and Extrahepatic Portal Vein Obstruction. Ann. Intern. Med. 1967, 66, 41. [Google Scholar] [CrossRef] [PubMed]
- Schouten, J.N.; Verheij, J.; Seijo, S. Idiopathic Non-Cirrhotic Portal Hypertension: A Review. Orphanet J. Rare Dis. 2015, 10, 67. [Google Scholar] [CrossRef]
- Azar, A.; Aldaoud, N.; Hardenbergh, D.; Krimins, R.; Son, J.; Shiroky, J.; Timlin, H. Systemic Lupus Erythematosus and Common Variable Immunodeficiency. JCR J. Clin. Rheumatol. 2022, 28, e245–e248. [Google Scholar] [CrossRef]
- Sawada, T.; Fujimori, D.; Yamamoto, Y. Systemic Lupus Erythematosus and Immunodeficiency. Immunol. Med. 2019, 42, 1–9. [Google Scholar] [CrossRef]
- Dominguez-Villar, M.; Hafler, D.A. Regulatory T Cells in Autoimmune Disease. Nat. Immunol. 2018, 19, 665–673. [Google Scholar] [CrossRef]
- Sogkas, G.; Witte, T. The Link between Rheumatic Disorders and Inborn Errors of Immunity. eBioMedicine 2023, 90, 104501. [Google Scholar] [CrossRef]
- Pott, N.M.; Atschekzei, F.; Pott, C.C.; Ernst, D.; Witte, T.; Sogkas, G. Primary Antibody Deficiency-Associated Arthritis Shares Features with Spondyloarthritis and Enteropathic Arthritis. RMD Open 2022, 8, e002664. [Google Scholar] [CrossRef]
- Orozco, G.; Sanchez, E.; Collado, M.D.; Lopez-Nevot, M.A.; Paco, L.; Garcia, A.; Jimenez-Alonso, J.; Martin, J. Analysis of the Functional NFKB1 Promoter Polymorphism in Rheumatoid Arthritis and Systemic Lupus Erythematosus. Tissue Antigens 2005, 65, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Sabir, J.S.M.; El Omri, A.; Banaganapalli, B.; Al-Shaeri, M.A.; Alkenani, N.A.; Sabir, M.J.; Hajrah, N.H.; Zrelli, H.; Ciesla, L.; Nasser, K.K.; et al. Dissecting the Role of NF-Κb Protein Family and Its Regulators in Rheumatoid Arthritis Using Weighted Gene Co-Expression Network. Front. Genet. 2019, 10, 1163. [Google Scholar] [CrossRef] [PubMed]
- Perazzio, S.F.; Allenspach, E.J.; Eklund, K.K.; Varjosalo, M.; Shinohara, M.M.; Torgerson, T.R.; Seppänen, M.R.J. Behçet Disease (BD) and BD-like Clinical Phenotypes: NF-κB Pathway in Mucosal Ulcerating Diseases. Scand. J. Immunol. 2020, 92, e12973. [Google Scholar] [CrossRef] [PubMed]
- Lorenzini, T.; Fliegauf, M.; Klammer, N.; Frede, N.; Proietti, M.; Bulashevska, A.; Camacho-Ordonez, N.; Varjosalo, M.; Kinnunen, M.; De Vries, E.; et al. Characterization of the Clinical and Immunologic Phenotype and Management of 157 Individuals with 56 Distinct Heterozygous NFKB1 Mutations. J. Allergy Clin. Immunol. 2020, 146, 901–911. [Google Scholar] [CrossRef]
- Barnabei, L.; Laplantine, E.; Mbongo, W.; Rieux-Laucat, F.; Weil, R. NF-κB: At the Borders of Autoimmunity and Inflammation. Front. Immunol. 2021, 12, 716469. [Google Scholar] [CrossRef]
- Yong, P.F.K.; Aslam, L.; Karim, M.Y.; Khamashta, M.A. Management of Hypogammaglobulinaemia Occurring in Patients with Systemic Lupus Erythematosus. Rheumatology 2008, 47, 1400–1405. [Google Scholar] [CrossRef][Green Version]
- Mantovani, A.P.F.; Monclaro, M.P.; Skare, T.L. Prevalence of IgA Deficiency in Adult Systemic Lupus Erythematosus and the Study of the Association with Its Clinical and Autoantibody Profiles. Rev. Bras. Reumatol. 2010, 50, 273–282. [Google Scholar] [CrossRef]
- Fernández-Castro, M.; Mellor-Pita, S.; Citores, M.J.; Muñoz, P.; Tutor-Ureta, P.; Silva, L.; Vargas, J.A.; Yebra-Bango, M.; Andreu, J.L. Common Variable Immunodeficiency in Systemic Lupus Erythematosus. Semin. Arthritis Rheum. 2007, 36, 238–245. [Google Scholar] [CrossRef]
- Cassidy, J.T.; Kitson, R.K.; Selby, C.L. Selective IgA Deficiency in Children and Adults with Systemic Lupus Erythematosus. Lupus 2007, 16, 647–650. [Google Scholar] [CrossRef]
- Perazzio, S.F.; Granados, Á.; Salomão, R.; Silva, N.P.; Carneiro-Sampaio, M.; Andrade, L.E.C. High Frequency of Immunodeficiency-like States in Systemic Lupus Erythematosus: A Cross-Sectional Study in 300 Consecutive Patients. Rheumatology 2016, 55, 1647–1655. [Google Scholar] [CrossRef]
- Quartuccio, L.; De Marchi, G.; Longhino, S.; Manfrè, V.; Rizzo, M.T.; Gandolfo, S.; Tommasini, A.; De Vita, S.; Fox, R. Shared Pathogenetic Features Between Common Variable Immunodeficiency and Sjögren’s Syndrome: Clues for a Personalized Medicine. Front. Immunol. 2021, 12, 703780. [Google Scholar] [CrossRef] [PubMed]
- Farmer, J.R.; Ong, M.-S.; Barmettler, S.; Yonker, L.M.; Fuleihan, R.; Sullivan, K.E.; Cunningham-Rundles, C.; The USIDNET Consortium; Walter, J.E. Common Variable Immunodeficiency Non-Infectious Disease Endotypes Redefined Using Unbiased Network Clustering in Large Electronic Datasets. Front. Immunol. 2018, 8, 1740. [Google Scholar] [CrossRef] [PubMed]
- Boyarchuk, O.; Dobrovolska, L.; Svystunovych, H. Selective Immunoglobulin A Deficiency in Children with Diabetes Mellitus: Data from a Medical Center in Ukraine. PLoS ONE 2022, 17, e0277273. [Google Scholar] [CrossRef] [PubMed]
- Jamee, M.; Alaei, M.R.; Mesdaghi, M.; Noorian, S.; Moosavian, M.; Dolatshahi, E.; Taghavi Kojidi, H.; Chavoshzadeh, Z.; Fallahi, M.; Parviz, S.; et al. The Prevalence of Selective and Partial Immunoglobulin A Deficiency in Patients with Autoimmune Polyendocrinopathy. Immunol. Investig. 2022, 51, 778–786. [Google Scholar] [CrossRef] [PubMed]
- Coopmans, E.C.; Chunharojrith, P.; Neggers, S.J.C.M.M.; Van Der Ent, M.W.; Swagemakers, S.M.A.; Hollink, I.H.; Barendregt, B.H.; Van Der Spek, P.J.; Van Der Lely, A.-J.; Van Hagen, P.M.; et al. Endocrine Disorders Are Prominent Clinical Features in Patients With Primary Antibody Deficiencies. Front. Immunol. 2019, 10, 2079. [Google Scholar] [CrossRef]
- Heneghan, M.A.; McHugh, P.; Stevens, F.M.; McCarthy, C.F. Addison’s Disease and Selective IgA Deficiency in Two Coeliac Patients. Scand. J. Gastroenterol. 1997, 32, 509–511. [Google Scholar] [CrossRef]
- Ferreira, R.C.; Pan-Hammarström, Q.; Graham, R.R.; Gateva, V.; Fontán, G.; Lee, A.T.; Ortmann, W.; Urcelay, E.; Fernández-Arquero, M.; Núñez, C.; et al. Association of IFIH1 and Other Autoimmunity Risk Alleles with Selective IgA Deficiency. Nat. Genet. 2010, 42, 777–780. [Google Scholar] [CrossRef]
- Parackova, Z.; Klocperk, A.; Rataj, M.; Kayserova, J.; Zentsova, I.; Sumnik, Z.; Kolouskova, S.; Sklenarova, J.; Pruhova, S.; Obermannova, B.; et al. Alteration of B Cell Subsets and the Receptor for B Cell Activating Factor (BAFF) in Paediatric Patients with Type 1 Diabetes. Immunol. Lett. 2017, 189, 94–100. [Google Scholar] [CrossRef]
- Johnson, M.B.; De Franco, E.; Lango Allen, H.; Al Senani, A.; Elbarbary, N.; Siklar, Z.; Berberoglu, M.; Imane, Z.; Haghighi, A.; Razavi, Z.; et al. Recessively Inherited LRBA Mutations Cause Autoimmunity Presenting as Neonatal Diabetes. Diabetes 2017, 66, 2316–2322. [Google Scholar] [CrossRef]
- Charbonnier, L.-M.; Janssen, E.; Chou, J.; Ohsumi, T.K.; Keles, S.; Hsu, J.T.; Massaad, M.J.; Garcia-Lloret, M.; Hanna-Wakim, R.; Dbaibo, G.; et al. Regulatory T-Cell Deficiency and Immune Dysregulation, Polyendocrinopathy, Enteropathy, X-Linked–like Disorder Caused by Loss-of-Function Mutations in LRBA. J. Allergy Clin. Immunol. 2015, 135, 217–227.e9. [Google Scholar] [CrossRef]
- Fierabracci, A.; Belcastro, E.; Carbone, E.; Pagliarosi, O.; Palma, A.; Pacillo, L.; Giancotta, C.; Zangari, P.; Finocchi, A.; Cancrini, C.; et al. In Search for the Missing Link in APECED-like Conditions: Analysis of the AIRE Gene in a Series of 48 Patients. J. Clin. Med. 2022, 11, 3242. [Google Scholar] [CrossRef] [PubMed]
- Quentien, M.-H.; Delemer, B.; Papadimitriou, D.T.; Souchon, P.-F.; Jaussaud, R.; Pagnier, A.; Munzer, M.; Jullien, N.; Reynaud, R.; Galon-Faure, N.; et al. Deficit in Anterior Pituitary Function and Variable Immune Deficiency (DAVID) in Children Presenting with Adrenocorticotropin Deficiency and Severe Infections. J. Clin. Endocrinol. Metab. 2012, 97, E121–E128. [Google Scholar] [CrossRef] [PubMed]
- Poowuttikul, P.; McGrath, E.; Kamat, D. Deficit of Anterior Pituitary Function and Variable Immune Deficiency Syndrome: A Novel Mutation. Glob. Pediatr. Health 2017, 4, 2333794X16686870. [Google Scholar] [CrossRef] [PubMed]
| Clinical Phenotypes | Clinical Features |
|---|---|
| No complications: infections only | Recurrent/persistent respiratory/gastrointestinal infections |
| Autoimmune disease | Cytopenia, rheumatologic disease, endocrinopathy, dermatologic manifestations |
| Predominant enteropathy | Non-infectious diarrhea, celiac-like, IBD-like, atrophic gastritis, liver disease |
| Lymphocytic organ infiltration | Lymphocytic enteropathy, granulomas, splenomegaly, unexplained hepatomegaly, persistent lymphadenopathy, and/or lymphoid interstitial pneumonia |
| Lymphoid carcinoma | Non-Hodgkin lymphoma |
| Clinical Phenotypes | Clinical Features |
|---|---|
| Asymptomatic | None |
| Recurrent infections | Gastrointestinal/respiratory infections |
| Allergy | Asthma, rhinitis, urticaria, atopic dermatitis, food allergy, anaphylaxis induced by blood products |
| Autoimmunity | Cytopenia, endocrinopathies, rheumatologic/dermatologic manifestations, and enteropathies |
| Malignancy | Gastrointestinal carcinoma |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sircana, M.C.; Vidili, G.; Gidaro, A.; Delitala, A.P.; Filigheddu, F.; Castelli, R.; Manetti, R. Common Variable Immunodeficiency and Selective IgA Deficiency: Focus on Autoimmune Manifestations and Their Pathogenesis. Int. J. Transl. Med. 2023, 3, 432-460. https://doi.org/10.3390/ijtm3040031
Sircana MC, Vidili G, Gidaro A, Delitala AP, Filigheddu F, Castelli R, Manetti R. Common Variable Immunodeficiency and Selective IgA Deficiency: Focus on Autoimmune Manifestations and Their Pathogenesis. International Journal of Translational Medicine. 2023; 3(4):432-460. https://doi.org/10.3390/ijtm3040031
Chicago/Turabian StyleSircana, Marta Chiara, Gianpaolo Vidili, Antonio Gidaro, Alessandro Palmerio Delitala, Fabiana Filigheddu, Roberto Castelli, and Roberto Manetti. 2023. "Common Variable Immunodeficiency and Selective IgA Deficiency: Focus on Autoimmune Manifestations and Their Pathogenesis" International Journal of Translational Medicine 3, no. 4: 432-460. https://doi.org/10.3390/ijtm3040031
APA StyleSircana, M. C., Vidili, G., Gidaro, A., Delitala, A. P., Filigheddu, F., Castelli, R., & Manetti, R. (2023). Common Variable Immunodeficiency and Selective IgA Deficiency: Focus on Autoimmune Manifestations and Their Pathogenesis. International Journal of Translational Medicine, 3(4), 432-460. https://doi.org/10.3390/ijtm3040031










