Non-Clear Cell Renal Cell Carcinoma: Molecular Pathogenesis, Innovative Modeling, and Targeted Therapeutic Approaches
Abstract
1. Introduction
1.1. Non-Clear RCC
1.2. Papillary Renal Cell Carcinoma (pRCC)
1.3. Renal Chromophobe Cell Carcinomas and Oncocytomas
1.4. Collecting (Bellini) Duct Renal Cell Carcinoma
1.5. Renal Medullary Cell Carcinoma (RMC)
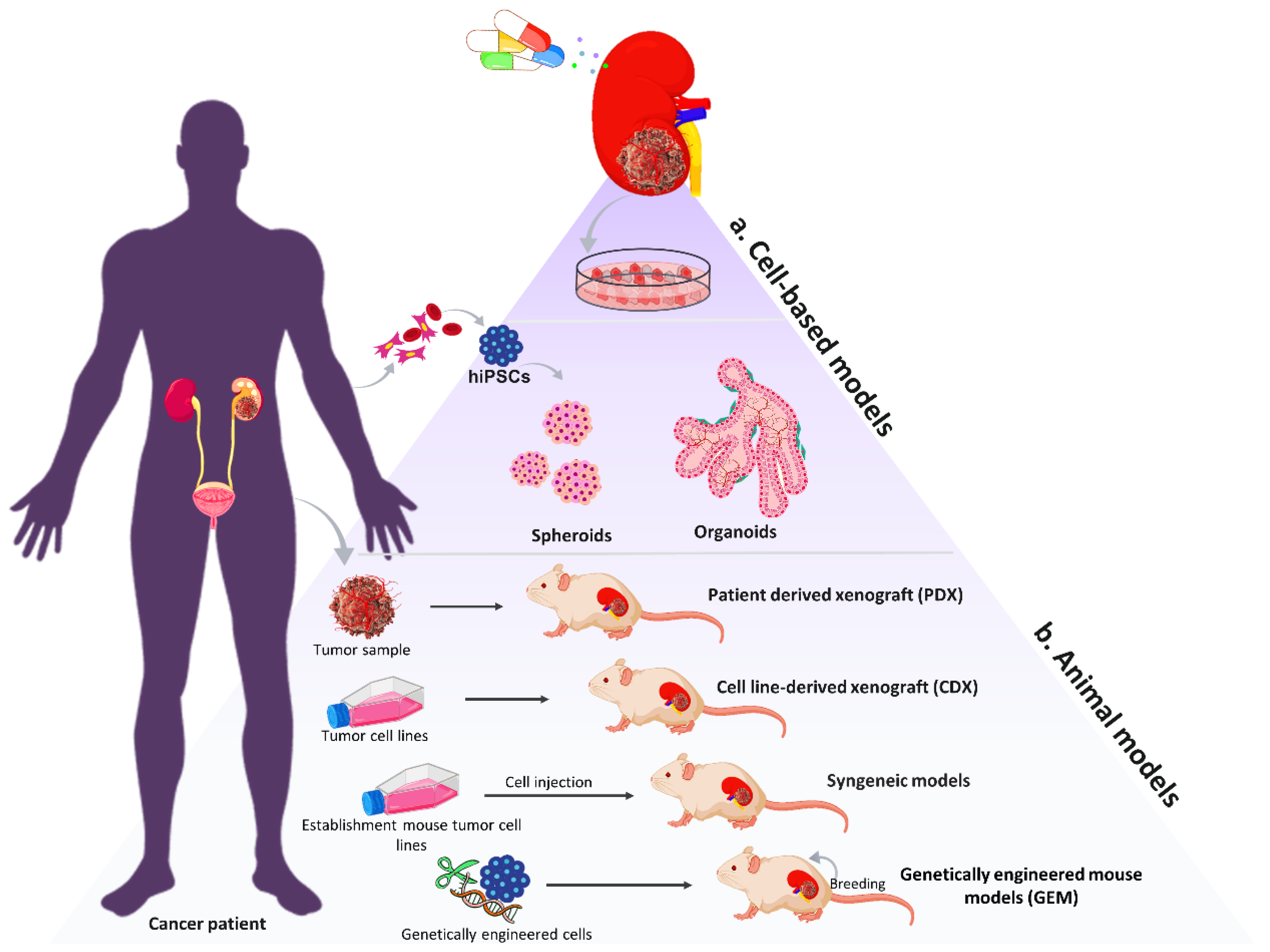
2. Main Therapeutic Approaches in Non-Clear Renal Cell Carcinoma (nccRCC)
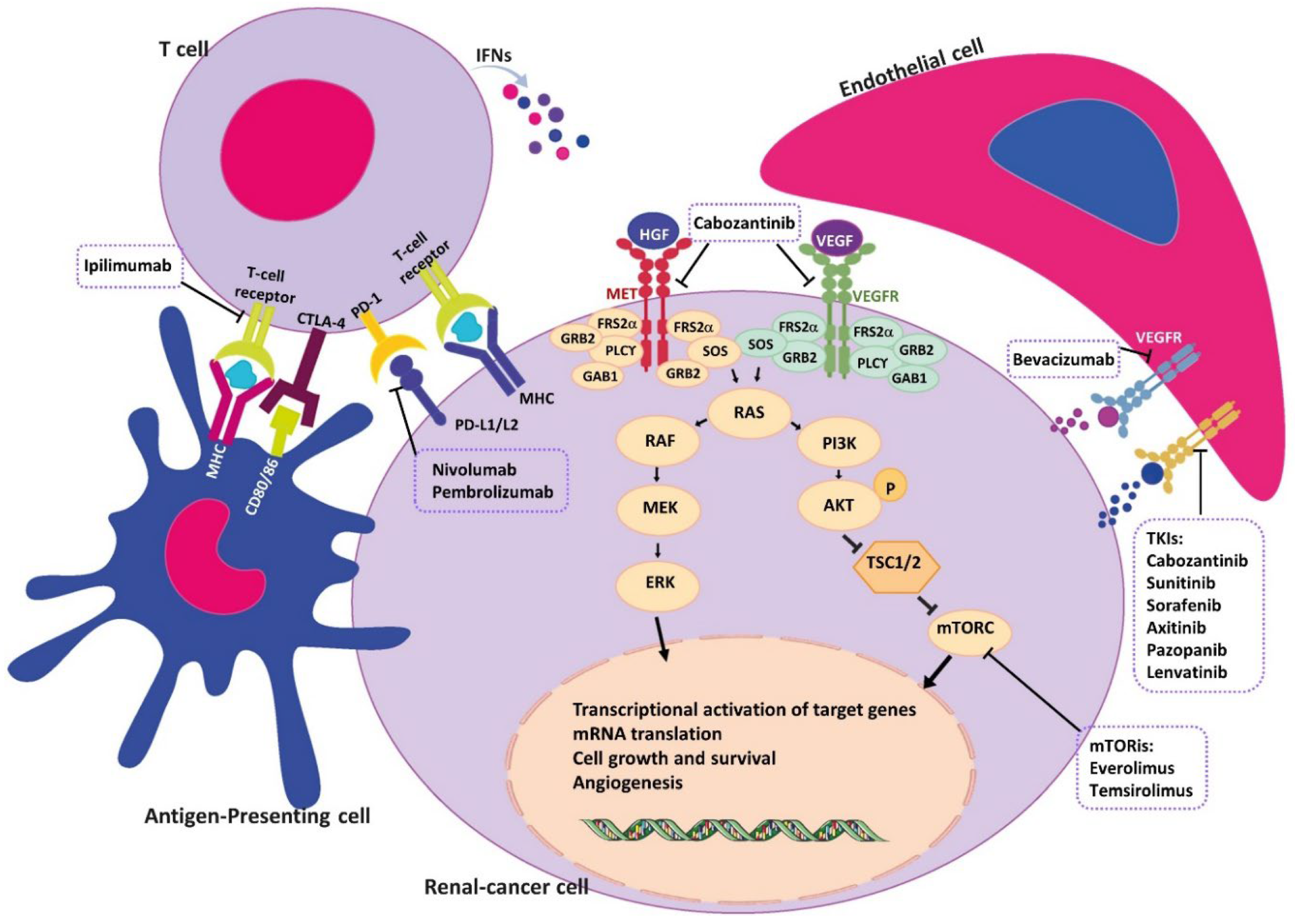
2.1. Tyrosine Kinase Inhibitors (TKIs)
2.2. Mammalian Target of Rapamycin Inhibitors (mTORis)
2.3. Immune Checkpoint Inhibitors (ICIs)
2.4. Chemotherapy
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Karumanchi, S.A.; Merchan, J.; Sukhatme, V.P. Renal cancer: Molecular mechanisms and newer therapeutic options. Curr. Opin. Nephrol. Hypertens. 2002, 11, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Brodziak, A.; Sobczuk, P.; Bartnik, E.; Fiedorowicz, M.; Porta, C.; Szczylik, C.; Czarnecka, A.M. Drug resistance in papillary RCC: From putative mechanisms to clinical practicalities. Nat. Rev. Urol. 2019, 16, 655–673. [Google Scholar] [CrossRef] [PubMed]
- Moch, H.; Cubilla, A.L.; Humphrey, P.A.; Reuter, V.E.; Ulbright, T.M. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part A: Renal, Penile, and Testicular Tumours. Eur. Urol. 2016, 70, 93–105. [Google Scholar] [CrossRef] [PubMed]
- Sircar, K.; Rao, P.; Jonasch, E.; Monzon, F.A.; Tamboli, P. Contemporary approach to diagnosis and classification of renal cell carcinoma with mixed histologic feature. Chin. J. Cancer 2013, 32, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Muglia, V.F.; Prando, A. Renal cell carcinoma: Histological classification and correlation with imaging findings. Radiol. Bras. 2015, 48, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Sepe, P.; Ottini, A.; Pircher, C.; Franza, A.; Claps, M.; Guadalupi, V.; Verzoni, E.; Procopio, G. Characteristics and treatment challenges of non-clear cell renal cell carcinoma. Cancers 2021, 13, 3807. [Google Scholar] [CrossRef]
- Pang, J.; Li, Z.; Lin, P.; Wang, X.; Chen, G.; Yan, H.; Li, S. The underlying molecular mechanism and potential drugs for treatment in papillary renal cell carcinoma: A study based on TCGA and Cmap datasets. Oncol. Rep. 2019, 41, 2089–2102. [Google Scholar] [CrossRef] [PubMed]
- Cancer Genome Atlas Research Network; Linehan, W.M.; Spellman, P.T.; Ricketts, C.J.; Creighton, C.J.; Fei, S.S.; Davis, C.; Wheeler, D.A.; Murray, B.A.; Schmidt, L.; et al. Comprehensive Molecular Characterization of Papillary Renal-Cell Carcinoma. N. Engl. J. Med. 2016, 374, 135–145. [Google Scholar] [CrossRef]
- Akhtar, M.; Al-Bozom, I.A.; Al Hussain, T. Papillary Renal Cell Carcinoma (PRCC): An Update. Adv. Anat. Pathol. 2019, 26, 124–132. [Google Scholar] [CrossRef]
- Linehan, W.M.; Schmidt, L.S.; Crooks, D.R.; Wei, D.; Srinivasan, R.; Lang, M.; Ricketts, C.J. The Metabolic Basis of Kidney Cancer. Cancer Discov. 2019, 9, 1006–1021. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, J.; Huang, Y. Characterization of Clinical Cases of Advanced Papillary Renal Cell Carcinoma via Comprehensive Genomic Profiling. Eur. Urol. 2018, 74, 398–399. [Google Scholar] [CrossRef] [PubMed]
- Ahrens, M.; Scheich, S.; Hartmann, A.; Bergmann, L. Non-Clear Cell Renal Cell Carcinoma—Pathology and Treatment Options. Oncol. Res. Treat. 2019, 42, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Shinojima, T.; Oya, M.; Takayanagi, A.; Mizuno, R.; Shimizu, N.; Murai, M. Renal cancer cells lacking hypoxia inducible factor (HIF)-1α expression maintain vascular endothelial growth factor expression through HIF-2α. Carcinogenesis 2007, 28, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Winer, A.G.; Chevinsky, M.; Jakubowski, C.; Chen, Y.-B.; Dong, Y.; Tickoo, S.K.; Reuter, V.E.; Russo, P.; Coleman, J.; et al. Analysis of renal cancer cell lines from two major resources enables genomics-guided cell line selection. Nat. Commun. 2017, 8, 15165. [Google Scholar] [CrossRef]
- Schmidt, L.; Junker, K.; Nakaigawa, N.; Kinjerski, T.; Weirich, G.; Miller, M.; Lubensky, I.; Neumann, H.P.; Brauch, H.; Decker, J.; et al. Novel mutations of the MET proto-oncogene in papillary renal carcinomas. Oncogene 1999, 18, 2343–2350. [Google Scholar] [CrossRef]
- Sakai, I.; Miyake, H.; Fujisawa, M. Acquired resistance to sunitinib in human renal cell carcinoma cells is mediated by constitutive activation of signal transduction pathways associated with tumour cell proliferation. BJU Int. 2013, 112, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Furge, K.A.; Chen, J.; Koeman, J.; Swiatek, P.; Dykema, K.; Lucin, K.; Kahnoski, R.; Yang, X.J.; Teh, B.T. Detection of DNA copy number changes and oncogenic signaling abnormalities from gene expression data reveals MYC activation in high-grade papillary renal cell carcinoma. Cancer Res. 2007, 67, 3171–3176. [Google Scholar] [CrossRef]
- Yang, Y.; Valera, V.A.; Padilla-Nash, H.M.; Sourbier, C.; Vocke, C.D.; Vira, M.A.; Abu-Asab, M.S.; Bratslavsky, G.; Tsokos, M.; Merino, M.J.; et al. UOK 262 cell line, fumarate hydratase deficient (FH-/FH-) hereditary leiomyomatosis renal cell carcinoma: In vitro and in vivo model of an aberrant energy metabolic pathway in human cancer. Cancer Genet. Cytogenet. 2010, 196, 45–55. [Google Scholar] [CrossRef]
- Yang, Y.; Valera, V.; Sourbier, C.; Vocke, C.D.; Wei, M.; Pike, L.; Huang, Y.; Merino, M.A.; Bratslavsky, G.; Wu, M.; et al. A novel fumarate hydratase-deficient HLRCC kidney cancer cell line, UOK268: A model of the Warburg effect in cancer. Cancer Genet. 2012, 205, 377–390. [Google Scholar] [CrossRef]
- Looyenga, B.D.; Furge, K.A.; Dykema, K.J.; Koeman, J.; Swiatek, P.J.; Giordano, T.J.; West, A.B.; Resau, J.H.; Teh, B.T.; MacKeigan, J.P. Chromosomal amplification of leucine-rich repeat kinase-2 (LRRK2) is required for oncogenic MET signaling in papillary renal and thyroid carcinomas. Proc. Natl. Acad. Sci. USA 2011, 108, 1439–1444. [Google Scholar] [CrossRef]
- Perrier-Trudova, V.; Huimin, B.W.; Kongpetch, S.; Huang, D.; Ong, P.; Le Formal, A.; Poon, S.L.; Siew, E.Y.; Myint, S.S.; Gad, S.; et al. Fumarate Hydratase-deficient Cell Line NCCFH1 as a New In Vitro Model of Hereditary Papillary Renal Cell Carcinoma Type 2. Anticancer Res. 2015, 35, 6639–6653. [Google Scholar] [PubMed]
- Furge, K.A.; Dykema, K.; Petillo, D.; Westphal, M.; Zhang, Z.; Kort, E.J.; Teh, B.T. Combining differential expression, chromosomal and pathway analyses for the molecular characterization of renal cell carcinoma. J. Can. Urol. Assoc. 2007, 1, 21–27. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saleeb, R.M.; Farag, M.; Lichner, Z.; Brimo, F.; Bartlett, J.; Bjarnason, G.; Finelli, A.; Rontondo, F.; Downes, M.R.; Yousef, G.M. Modulating ATP binding cassette transporters in papillary renal cell carcinoma type 2 enhances its response to targeted molecular therapy. Mol. Oncol. 2018, 12, 1673–1688. [Google Scholar] [CrossRef]
- Lee, Y.H.; Morrison, B.L.; Bottaro, D.P. Synergistic signaling of tumor cell invasiveness by Hepatocyte growth factor and hypoxia. J. Biol. Chem. 2014, 289, 20448–20461. [Google Scholar] [CrossRef] [PubMed]
- Matak, D.; Brodaczewska, K.K.; Szczylik, C.; Koch, I.; Myszczyszyn, A.; Lipiec, M.; Lewicki, S.; Szymanski, L.; Zdanowski, R.; Czarnecka, A.M. Functional significance of CD105-positive cells in papillary renal cell carcinoma. BMC Cancer 2017, 17, 21. [Google Scholar] [CrossRef] [PubMed]
- Sourbier, C.; Liao, P.-J.; Ricketts, C.J.; Wei, D.; Yang, Y.; Baranes, S.M.; Gibbs, B.K.; Ohanjanian, L.; Krane, L.S.; Scroggins, B.T.; et al. Targeting loss of the Hippo signaling pathway in NF2-deficient papillary kidney cancers. Oncotarget 2018, 9, 10723–10733. [Google Scholar] [CrossRef]
- Rosette, K.A.; Lander, S.M.; VanOpstall, C.; Looyenga, B.D. Three-dimensional coculture provides an improved in vitro model for papillary renal cell carcinoma. Am. J. Ren. Physiol. 2021, 321, 33–46. [Google Scholar] [CrossRef]
- Zahmatkesh, E.; Khoshdel-Rad, N.; Mirzaei, H.; Shpichka, A.; Timashev, P.; Mahmoudi, T.; Vosough, M. Evolution of organoid technology: Lessons learnt in Co-Culture systems from developmental biology. Dev. Biol. 2021, 21, 0012–0056. [Google Scholar] [CrossRef]
- Rad, N.K.; Ahmadi, A.; Moghadasali, R. Kidney organoids: Current knowledge and future directions. Cell Tissue Res. 2022, 387, 207–224. [Google Scholar] [CrossRef]
- Bailey, S.T.; Smith, A.M.; Kardos, J.; Wobker, S.E.; Wilson, H.L.; Krishnan, B.; Saito, R.; Lee, H.J.; Zhang, J.; Eaton, S.C.; et al. MYC activation cooperates with Vhl and Ink4a/Arf loss to induce clear cell renal cell carcinoma. Nat. Commun. 2017, 8, 15770. [Google Scholar] [CrossRef]
- Calcagni, A.; Kors, L.; Verschuren, E.; De Cegli, R.; Zampelli, N.; Nusco, E.; Confalonieri, S.; Bertalot, G.; Pece, S.; Settembre, C.; et al. Modelling TFE renal cell carcinoma in mice reveals a critical role of WNT signaling. eLife 2016, 5, e17047. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Huang, D.; Rubera, I.; Futami, K.; Wang, P.; Zlckert, P.; Khoo, S.-K.; Dykema, K.; Zhao, P.; Petillo, D.; et al. Disruption of tubular Flcn expression as a mouse model for renal tumor induction. Kidney Int. 2015, 88, 1057–1069. [Google Scholar] [CrossRef] [PubMed]
- Barré-Sinoussi, F.; Montagutelli, X. Animal models are essential to biological research: Issues and perspectives. Future Sci. OA 2015, 1, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Sobczuk, P.; Brodziak, A.; Khan, M.I.; Chhabra, S.; Fiedorowicz, M.; Wełniak-Kamińska, M.; Synoradzki, K.; Bartnik, E.; Cudnoch-Jędrzejewska, A.; Czarnecka, A.M. Choosing the Right Animal Model for Renal Cancer Research. Transl. Oncol. 2020, 13, 100745. [Google Scholar] [CrossRef]
- Korhonen, M.; Sariola, H.; Gould, V.E.; Kangas, L.; Virtanen, I. Integrins and Laminins in Human Renal Carcinoma Cells and Tumors Grown in Nude Mice. Cancer Res. 1994, 54, 4532–4538. [Google Scholar]
- Pulkkanen, K.J.; Parkkinen, J.J.; Laukkanen, J.M.; Kettunen, M.I.; Tyynela, K.; Kauppinen, R.A.; Ala-Opas, M.Y.; Yla-Herttuala, S. HSV-tk gene therapy for human renal cell carcinoma in nude mice. Cancer Gene Ther. 2001, 8, 529–536. [Google Scholar] [CrossRef]
- Zhou, D.; Kannappan, V.; Chen, X.; Li, J.; Leng, X.; Zhang, J.; Xuan, S. RBP2 induces stem-like cancer cells by promoting EMT and is a prognostic marker for renal cell carcinoma. Exp. Mol. Med. 2016, 48, e238. [Google Scholar] [CrossRef]
- Schuller, A.G.; Barry, E.R.; Jones, R.D.; Henry, R.E.; Frigault, M.M.; Beran, G.; Linsenmayer, D.; Hattersley, M.; Smith, A.; Wilson, J.; et al. The MET Inhibitor AZD6094 (Savolitinib, HMPL-504) induces regression in papillary renal cell carcinoma patient-derived xenograft models. Clin. Cancer Res. 2015, 21, 2811–2819. [Google Scholar] [CrossRef]
- Sivanand, S.; Peña-Llopis, S.; Zhao, H.; Kucejova, B.; Spence, P.; Pavia-Jimenez, A.; Yamasaki, T.; McBride, D.J.; Gillen, J.; Wolff, N.C.; et al. A validated tumorgraft model reveals activity of dovitinib against renal cell carcinoma. Sci. Transl. Med. 2012, 4, 137ra75. [Google Scholar] [CrossRef]
- Khoshdel-rad, N.; Zahmatkesh, E.; Moeinvaziri, F.; Haghparast, N.; Baharvand, H.; Aghdami, N.; Moghadasali, R. Promoting Maturation of Human Pluripotent Stem Cell-Derived Renal Microtissue by Incorporation of Endothelial and Mesenchymal Cells. Stem Cells Dev. 2021, 30, 428–440. [Google Scholar] [CrossRef]
- Hwang, J.W.; Desterke, C.; Féraud, O.; Richard, S.; Ferlicot, S.; Verkarre, V.; Patard, J.J.; Loisel-Duwattez, J.; Foudi, A.; Griscelli, F.; et al. IPSC-derived Cancer Organoids Recapitulate Genomic and Phenotypic Alterations of c-met-mutated Hereditary Kidney Cancer. bioRxiv 2019. [Google Scholar] [CrossRef]
- Casuscelli, J.; Weinhold, N.; Gundem, G.; Wang, L.; Zabor, E.C.; Drill, E.; Wang, P.I.; Nanjangud, G.J.; Redzematovic, A.; Nargund, A.M.; et al. Genomic landscape and evolution of metastatic chromophobe renal cell carcinoma. JCI Insight 2017, 2, e92688. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.F.; Ricketts, C.J.; Wang, M.; Yang, L.; Cherniack, A.D.; Shen, H.; Buhay, C.; Kang, H.; Kim, S.C.; Fahey, C.C.; et al. The somatic genomic landscape of chromophobe renal cell carcinoma. Cancer Cell 2014, 26, 319–330. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, K.; Sakamoto, M.; Ohta, T.; Kanai, Y.; Ohki, M.; Hirohashi, S. Overexpression of KIT in chromophobe renal cell carcinoma. Oncogene 2003, 22, 847–852. [Google Scholar] [CrossRef] [PubMed]
- Zimpfer, A.; Janke, S.; Hühns, M.; Schneider, B.; Kundt, G.; Zettl, H.; Kilic, E.; Maruschke, M.; Hakenberg, O.W.; Erbersdobler, A. C-kit overexpression is not associated with KIT gene mutations in chromophobe renal cell carcinoma or renal oncocytoma. Pathol. Res. Pract. 2014, 210, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Garje, R.; Elhag, D.; Yasin, H.A.; Acharya, L.; Vaena, D.; Dahmoush, L. Comprehensive review of chromophobe renal cell carcinoma. Crit. Rev. Oncol./Hematol. 2021, 160, 103287. [Google Scholar] [CrossRef]
- Pandey, N.; Lanke, V.; Vinod, P.K. Network-based metabolic characterization of renal cell carcinoma. Sci. Rep. 2020, 10, 5955. [Google Scholar] [CrossRef]
- Nagy, A.; Wilhelm, M.; Sükösd, F.; Ljungberg, B.; Kovacs, G. Somatic mitochondrial DNA mutations in human chromophobe renal cell carcinomas. Genes Chromosom. Cancer 2002, 35, 256–260. [Google Scholar] [CrossRef]
- Meierhofer, D.; Mayr, J.A.; Fink, K.; Schmeller, N.; Kofler, B.; Sperl, W. Mitochondrial DNA mutations in renal cell carcinomas revealed no general impact on energy metabolism. Br. J. Cancer 2006, 94, 268–274. [Google Scholar] [CrossRef]
- Xiao, Y.; Clima, R.; Busch, J.; Rabien, A.; Kilic, E.; Villegas, S.L.; Timmermann, B.; Attimonelli, M.; Jung, K.; Meierhofer, D. Decreased mitochondrial DNA content drives OXPHOS dysregulation in chromophobe renal cell carcinoma. Cancer Res. 2020, 80, 3830–3840. [Google Scholar] [CrossRef]
- Liu, G.; Li, Y.; Li, Z.; Zhou, J.; Huo, Z.; Ji, Z. Renal hybrid oncocytic/chromophobe tumor associated with multiple schwannomas. Medicine 2017, 96, e8939. [Google Scholar] [CrossRef] [PubMed]
- Gerharz, C.D.; Moll, R.; Störkel, S.; Ramp, U.; Hildebrandt, B.; Molsberger, G.; Koldovsky, P.; Gabbert, H.E. Establishment and characterization of two divergent cell lines derived from a human chromophobe renal cell carcinoma. Am. J. Pathol. 1995, 146, 953–962. [Google Scholar]
- Valente, M.J.; Henrique, R.; Costa, V.L.; Jerónimo, C.; Carvalho, F.; Bastos, M.L.; de Pinho, P.G.; Carvalho, M. A rapid and simple procedure for the establishment of human normal and cancer renal primary cell cultures from surgical specimens. PLoS ONE 2011, 6, e19337. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Vocke, C.D.; Ricketts, C.J.; Wei, D.; Padilla-Nash, H.M.; Lang, M.; Sourbier, C.; Killian, J.K.; Boyle, S.L.; Worrell, R.; et al. Genomic and metabolic characterization of a chromophobe renal cell carcinoma cell line model (UOK276). Genes Chromosom. Cancer 2017, 56, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Baba, M.; Furihata, M.; Hong, S.-B.; Tessarollo, L.; Haines, D.C.; Southon, E.; Patel, V.; Igarashi, P.; Alvord, W.G.; Leighty, R.; et al. Kidney-targeted Birt-Hogg-Dubé gene inactivation in a mouse model: Erk1/2 and Akt-mTOR activation, cell hyperproliferation, and polycystic kidneys. J. Natl. Cancer Inst. 2008, 100, 140–154. [Google Scholar] [CrossRef] [PubMed]
- Ciszewski, S.; Jakimów, A.; Smolska-Ciszewska, B. Collecting (Bellini) duct carcinoma: A clinical study of a rare tumour and review of the literature. Can. Urol. Assoc. J. 2015, 9, E589–E593. [Google Scholar] [CrossRef]
- Lyu, Z.; Liu, L.; Li, H.; Wang, H.; Liu, Q.; Chen, T.; Xu, M.; Tian, L.; Fu, P. Imaging analysis of 13 rare cases of renal collecting (Bellini) duct carcinoma in northern China: A case series and literature review. BMC Med. Imaging 2021, 21, 42. [Google Scholar] [CrossRef]
- Srigley, J.R.; Delahunt, B.; Eble, J.N.; Egevad, L.; Epstein, J.I.; Grignon, D.; Hes, O.; Moch, H.; Montironi, R.; Tickoo, S.K.; et al. The International Society of Urological Pathology (ISUP) Vancouver Classification. Am. J. Surg. Pathol. 2013, 37, 1469–1489. [Google Scholar] [CrossRef]
- Falcão, G.; Parmanande, A.Q.; Araújo, C.; Barreira, J.V. Bellini duct carcinoma. Autops. Case Rep. 2020, 11, e2020230. [Google Scholar] [CrossRef]
- Schoenberg, M.; Cairns, P.; Brooks, J.D.; Marshall, F.F.; Epstein, J.I.; Isaacs, W.B.; Sidransky, D. Frequent Loss of Chromosome Arms 8p and 13q in Collecting Duct Carcinoma (CDC) of the Kidney. Genes Chromosom. Cancer 1995, 12, 76–80. [Google Scholar] [CrossRef]
- Steiner, G.; Cairns, P.; Polascik, T.J.; Marshall, F.F.; Epstein, J.I.; Sidransky, D.; Schoenberg, M. High-density mapping of chromosomal arm 1q in renal collecting duct carcinoma: Region of minimal deletion at 1q32.1-32.2. Cancer Res. 1996, 56, 5044–5046. [Google Scholar]
- Pal, S.K.; Choueiri, T.K.; Wang, K.; Khaira, D.; Karam, J.A.; Van Allen, E.; Palma, N.A.; Stein, M.N.; Johnson, A.; Squillace, R.; et al. Characterization of Clinical Cases of Collecting Duct Carcinoma of the Kidney Assessed by Comprehensive Genomic Profiling. Eur. Urol. 2016, 70, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Cavazzana, A.O.; Prayer-Galetti, T.; Tirabosco, R.; Macciomei, M.C.; Stella, M.; Lania, L.; Cannada-Bartoli, P.; Passerini-Glazel, L.G.; Pagano, F. Bellini duct carcinoma: A clinical and in vitro study. Eur. Urol. 1996, 30, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Shroff, E.H.; Eberlin, L.S.; Dang, V.M.; Gouw, A.M.; Gabay, M.; Adam, S.J.; Bellovin, D.I.; Tran, P.T.; Philbrick, W.M.; Garcia-Ocana, A.; et al. MYC oncogene overexpression drives renal cell carcinoma in a mouse model through glutamine metabolism. Proc. Natl. Acad. Sci. USA 2015, 112, 6539–6544. [Google Scholar] [CrossRef] [PubMed]
- Msaouel, P.; Hong, A.L.; Mullen, E.A.; Atkins, M.B.; Walker, C.L.; Lee, C.-H.; Carden, M.A.; Genovese, G.; Linehan, W.M.; Rao, P.; et al. Updated recommendations on the diagnosis, management, and clinical trial eligibility criteria for patients with renal medullary carcinoma. Clin. Genitourin. Cancer 2020, 17, 1–6. [Google Scholar] [CrossRef]
- Khan, A.; Thomas, N.; Costello, B.; Jobling, L.; Dekretser, D.; Broadfield, E.; O’Shea, S. Renal medullary carcinoma: Sonographic, computed tomography, magnetic resonance and angiographic findings. Eur. J. Radiol. 2000, 35, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Seo, A.N.; Yoon, G.; Ro, J.Y. Clinicopathologic and molecular pathology of collecting duct carcinoma and related renal cell carcinomas. Adv. Anat. Pathol. 2017, 24, 65–77. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Hong, A.L. Recent Advances in Renal Medullary Carcinoma. Int. J. Mol. Sci. 2022, 23, 7097. [Google Scholar] [CrossRef]
- Stahlschmidt, J.; Cullinane, C.; Roberts, P.; Picton, S.V. Renal medullary carcinoma: Prolonged remission with chemotherapy, immunohistochemical characterisation and evidence of bcr/abl rearrangement. Med. Pediatr. Oncol. 1999, 33, 551–557. [Google Scholar] [CrossRef]
- Wei, D.; Yang, Y.; Ricketts, C.J.; Vocke, C.D.; Ball, M.W.; Sourbier, C.; Wangsa, D.; Wangsa, D.; Guha, R.; Zhang, X.; et al. Novel renal medullary carcinoma cell lines, UOK353 and UOK360, provide preclinical tools to identify new therapeutic treatments. Genes Chromosom. Cancer 2020, 59, 472–483. [Google Scholar] [CrossRef]
- Hakimi, A.A.; Koi, P.T.; Milhoua, P.M.; Blitman, N.M.; Li, M.; Hugec, V.; Dutcher, J.P.; Ghavamian, R. Renal Medullary Carcinoma: The Bronx Experience. Urology 2007, 70, 878–882. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.; Aiello, J.; Avigan, D.E.; Berdeja, J.G.; Borrello, I.M.; Chari, A.; Cohen, A.D.; Ganapathi, K.; Gray, L.; Green, D.; et al. The Society for Immunotherapy of Cancer consensus statement on immunotherapy for the treatment of multiple myeloma. J. Immunother. Cancer 2020, 8, e000734. [Google Scholar] [CrossRef] [PubMed]
- Steffens, S.; Janssen, M.; Roos, F.C.; Becker, F.; Schumacher, S.; Seidel, C.; Wegener, G.; Thüroff, J.W.; Hofmann, R.; Stöckle, M.; et al. Incidence and long-term prognosis of papillary compared to clear cell renal cell carcinoma—A multicentre study. Eur. J. Cancer 2012, 48, 2347–2352. [Google Scholar] [CrossRef] [PubMed]
- Park, I.; Lee, S.H.; Lee, J.L. A Multicenter Phase II Trial of Axitinib in Patients with Recurrent or Metastatic Non–clear-cell Renal Cell Carcinoma Who Had Failed Prior Treatment with Temsirolimus. Clin. Genitourin. Cancer 2018, 16, e997–e1002. [Google Scholar] [CrossRef]
- Campbell, M.T.; Bilen, M.A.; Shah, A.Y.; Lemke, E.; Jonasch, E.; Venkatesan, A.; Altinmakas, E.; Duran, C.; Msaouel, P.; Tannir, N. Cabozantinib for the treatment of patients with metastatic non-clear cell renal cell carcinoma: A retrospective analysis. Eur. J. Cancer 2018, 104, 188–194. [Google Scholar] [CrossRef]
- Chanzá, N.M.; Xie, W.; Bilen, M.A.; Dzimitrowicz, H.; Burkart, J.; Geynisman, D.M.; Balakrishnan, A.; Bowman, I.A.; Jain, R.; Stadler, W.; et al. Cabozantinib in advanced non-clear-cell renal cell carcinoma: A multicentre, retrospective, cohort study. Lancet Oncol. 2019, 20, 581–590. [Google Scholar] [CrossRef]
- Jung, K.S.; Lee, S.J.; Park, S.H.; Lee, J.L.; Lee, S.H.; Lim, J.Y.; Kang, J.H.; Lee, S.; Rha, S.Y.; Lee, K.H.; et al. Pazopanib for the Treatment of Non-clear Cell Renal Cell Carcinoma: A Single-Arm, Open-Label, Multicenter, Phase II Study. Cancer Res. Treat. 2018, 50, 488–494. [Google Scholar] [CrossRef]
- Hutson, T.E.; Michaelson, M.D.; Kuzel, T.M.; Agarwal, N.; Molina, A.M.; Hsieh, J.J.; Vaishampayan, U.N.; Xie, R.; Bapat, U.; Ye, W.; et al. A Single-arm, Multicenter, Phase 2 Study of Lenvatinib Plus Everolimus in Patients with Advanced Non-Clear Cell Renal Cell Carcinoma. Eur. Urol. 2021, 80, 162–170. [Google Scholar] [CrossRef]
- Hutson, T.E.; Michaelson, M.D.; Kuzel, T.M.; Agarwal, N.; Molina, A.M.; Hsieh, J.J.; Vaishampayan, U.; Xie, S.; Bapat, U.; Jain, R.K.; et al. A phase II study of lenvatinib plus everolimus in patients with advanced non-clear cell renal cell carcinoma (nccRCC). J. Clin. Oncol. 2020, 38, 685. [Google Scholar] [CrossRef]
- Feldman, D.R.; Ged, Y.; Lee, C.; Ms, A.K.; Molina, A.M.; Chen, Y.; Chaim, J.; Ms, D.T.C.; Murray, S.; Tickoo, S.K.; et al. Everolimus plus bevacizumab is an effective first-line treatment for patients with advanced papillary variant renal cell carcinoma: Final results from a phase II trial. Cancer 2020, 126, 5247–5255. [Google Scholar] [CrossRef]
- Escudier, B.; Molinie, V.; Bracarda, S.; Maroto, P.; Szczylik, C.; Nathan, P.; Negrier, S.; Weiss, C.; Porta, C.; Grünwald, V.; et al. Open-label phase 2 trial of first-line everolimus monotherapy in patients with papillary metastatic renal cell carcinoma: RAPTOR final analysis. Eur. J. Cancer 2016, 69, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Dutcher, J.P.; de Souza, P.; McDermott, D.; Figlin, R.A.; Berkenblit, A.; Thiele, A.; Krygowski, M.; Strahs, A.; Feingold, J.; Hudes, G. Effect of temsirolimus versus interferon-α on outcome of patients with advanced renal cell carcinoma of different tumor histologies.pdf. Med. Oncol. 2009, 26, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Zanardi, E.; Verzoni, E.; Grassi, P.; Necchi, A.; Giannatempo, P.; Raggi, D.; De Braud, F.G.M.; Procopio, G. Clinical experience with temsirolimus in the treatment of advanced renal cell carcinoma. Ther. Adv. Urol. 2015, 7, 152–161. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, M.J.; Rini, B.I.; Elson, P.; Schwandt, A.; Wood, L.; Trinkhaus, M.; Bjarnason, G.; Knox, J. Temsirolimus in VEGF-refractory metastatic renal cell carcinoma. Ann. Oncol. 2011, 22, 145–148. [Google Scholar] [CrossRef] [PubMed]
- Venugopal, B.; Ansari, J.; Aitchison, M.; Tho, L.M.; Campbell, R.; Jones, R.J. Efficacy of temsirolimus in metastatic chromophobe renal cell carcinoma. BMC Urol. 2013, 13, 26. [Google Scholar] [CrossRef]
- Song, S.H.; Jeong, I.G.; You, D.; Hong, J.H.; Hong, B.; Song, C.; Jung, W.Y.; Cho, Y.M.; Ahn, H.; Kim, C. VEGF/VEGFR2 and PDGF-B/PDGFR-ß expression in non-metastatic renal cell carcinoma: A retrospective study in 1,091 consecutive patients. Int. J. Clin. Exp. Pathol. 2014, 7, 7681–7689. [Google Scholar] [PubMed]
- Lai, Y.; Zhao, Z.; Zeng, T.; Liang, X.; Chen, D.; Duan, X.; Zeng, G.; Wu, W. Crosstalk between VEGFR and other receptor tyrosine kinases for TKI therapy of metastatic renal cell carcinoma. Cancer Cell Int. 2018, 18, 31. [Google Scholar] [CrossRef]
- Ansari, J.; Fatima, A.; Chaudhri, S.; Bhatt, R.I.; Wallace, M.; James, N.D. Sorafenib induces therapeutic response in a patient with metastatic collecting duct carcinoma of kidney. Onkologie 2009, 32, 44–46. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Plantade, A.; Elson, P.; Negrier, S.; Ravaud, A.; Oudard, S.; Zhou, M.; Rini, B.I.; Bukowski, R.M.; Escudier, B. Efficacy of sunitinib and sorafenib in metastatic papillary and chromophobe renal cell carcinoma. J. Clin. Oncol. 2008, 26, 127–131. [Google Scholar] [CrossRef]
- Miyake, H.; Haraguchi, T.; Takenaka, A.; Fujisawa, M. Metastatic collecting duct carcinoma of the kidney responded to sunitinib. Int. J. Clin. Oncol. 2011, 16, 153–155. [Google Scholar] [CrossRef]
- Procopio, G.; Testa, I.; Iacovelli, R.; Grassi, P.; Verzoni, E.; Garanzini, E.; Colecchia, M.; Torelli, T.; De Braud, F. Treatment of collecting duct carcinoma: Current status and future perspectives. Anticancer Res. 2014, 34, 1027–1030. [Google Scholar] [PubMed]
- Miricescu, D.; Balan, D.G.; Tulin, A.; Stiru, O.; Vacaroiu, I.A.; Mihai, D.A.; Popa, C.C.; Papacocea, R.I.; Enyedi, M.; Sorin, N.A.; et al. PI3K/AKT/mTOR signalling pathway involvement in renal cell carcinoma pathogenesis. Exp. Ther. Med. 2021, 21, 540. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-L.; Ziobro, M.; Gafanov, R.; Matveev, V.B.; Suarez, C.; Donskov, F.; Pouliot, F.; Alekseev, B.Y.; Wiechno, P.J.; Tomczak, P.; et al. KEYNOTE-427 cohort B: First-line pembrolizumab (pembro) monotherapy for advanced non-clear cell renal cell carcinoma (NCC-RCC). J. Clin. Oncol. 2019, 37, 4569. [Google Scholar] [CrossRef]
- Sugiyama, S.; Sato, K.; Shibasaki, Y.; Endo, Y.; Uryu, T.; Toyoshima, Y.; Oya, M.; Miyanaga, N.; Saijo, N.; Gemma, A.; et al. Real-world use of temsirolimus in Japanese patients with unresectable or metastatic renal cell carcinoma: Recent consideration based on the results of a post-marketing, all-case surveillance study. Jpn. J. Clin. Oncol. 2020, 50, 940–947. [Google Scholar] [CrossRef]
- Bergmann, L.; Grünwald, V.; Maute, L.; Grimm, M.-O.; Weikert, S.; Schleicher, J.; Klotz, T.; Greiner, J.; Flörcken, A.; Hartmann, A.; et al. A Randomized Phase IIa Trial with Temsirolimus versus Sunitinib in Advanced Non-Clear Cell Renal Cell Carcinoma: An Intergroup Study of the CESAR Central European Society for Anticancer Drug Research-EWIV and the Interdisciplinary Working Group on Renal C. Oncol. Res. Treat. 2020, 43, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Koh, Y.; Lim, H.Y.; Ahn, J.H.; Lee, J.-L.; Rha, S.Y.; Kim, Y.J.; Kim, T.M.; Lee, S.-H. Phase II trial of everolimus for the treatment of nonclear-cell renal cell carcinoma. Ann. Oncol. 2013, 24, 1026–1031. [Google Scholar] [CrossRef]
- Zielli, T.; Gnetti, L.; Buti, S. Activity of lenvatinib plus everolimus combination in a heavily pretreated patient with papillary renal cell carcinoma: A case report. Tumori 2020, 106, NP79–NP83. [Google Scholar] [CrossRef]
- Wiele, A.J.; Bathala, T.K.; Hahn, A.W.; Xiao, L.; Duran, M.; Ross, J.A.; Jonasch, E.; Shah, A.Y.; Campbell, M.T.; Msaouel, P.; et al. Lenvatinib with or without Everolimus in Patients with Metastatic Renal Cell Carcinoma after Immune Checkpoint Inhibitors and Vascular Endothelial Growth Factor Receptor-Tyrosine Kinase Inhibitor Therapies. Oncologist 2021, 26, 476–482. [Google Scholar] [CrossRef]
- Choueiri, T.; Fay, A.; Gray, K.; Callea, M.; Ho, T.; Albiges, L.; Bellmunt, J.; Song, J.; Carvo, I.; Lampron, M.; et al. PD-L1 expression in nonclear-cell renal cell carcinoma. Ann. Oncol. 2014, 25, 2178–2184. [Google Scholar] [CrossRef]
- Blank, C.U.; Haanen, J.B.; Ribas, A.; Schumacher, T.N. The “cancer immunogram” Visualizing the state of cancer-immune system interactions may spur personalized therapy. Science 2016, 352, 658–660. [Google Scholar] [CrossRef]
- McKay, R.R.; Bossé, D.; Xie, W.; Wankowicz, S.A.; Flaifel, A.; Brandao, R.; Lalani, A.K.A.; Martini, D.J.; Wei, X.X.; Braun, D.A.; et al. The Clinical Activity of PD-1/PD-L1 Inhibitors in Metastatic NonClear Cell Renal Cell Carcinoma. Cancer Immunol. Res. 2019, 6, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Zarrabi, K.; Walzer, E.; Zibelman, M. Immune checkpoint inhibition in advanced non-clear cell renal cell carcinoma: Leveraging success from clear cell histology into new opportunities. Cancers 2021, 13, 3652. [Google Scholar] [CrossRef] [PubMed]
- Adashek, J.J.; Genovese, G.; Tannir, N.M.; Msaouel, P. Recent advancements in the treatment of metastatic clear cell renal cell carcinoma: A review of the evidence using second-generation p-values. Cancer Treat. Res. Commun. 2020, 23, 100166. [Google Scholar] [CrossRef] [PubMed]
- Chahoud, J.; Msaouel, P.; Campbell, M.T.; Bathala, T.; Xiao, L.; Gao, J.; Zurita, A.J.; Shah, A.Y.; Jonasch, E.; Sharma, P.; et al. Nivolumab for the Treatment of Patients with Metastatic Non-Clear Cell Renal Cell Carcinoma (nccRCC): A Single-Institutional Experience and Literature Meta-Analysis. Oncologist 2020, 25, 252–258. [Google Scholar] [CrossRef]
- Koshkin, V.S.; Barata, P.C.; Zhang, T.; George, D.J.; Atkins, M.B.; Kelly, W.J.; Vogelzang, N.J.; Pal, S.K.; Hsu, J.; Appleman, L.J.; et al. Clinical activity of nivolumab in patients with non-clear cell renal cell carcinoma. J. Immunother. Cancer 2018, 6, 9. [Google Scholar] [CrossRef]
- Gupta, R.; Ornstein, M.C.; Li, H.; Allman, K.D.; Wood, L.S.; Gilligan, T.; Garcia, J.A.; Von Merveldt, D.; Hammers, H.J.; Rini, B.I. Clinical Activity of Ipilimumab Plus Nivolumab in Patients with Metastatic Non-Clear Cell Renal Cell Carcinoma. Clin. Genitourin. Cancer 2020, 18, 429–435. [Google Scholar] [CrossRef]
- Vogelzang, N.J.; Olsen, M.R.; McFarlane, J.J.; Arrowsmith, E.; Bauer, T.M.; Jain, R.K.; Somer, B.; Lam, E.T.; Kochenderfer, M.D.; Molina, A.; et al. Safety and Efficacy of Nivolumab in Patients with Advanced Non-Clear Cell Renal Cell Carcinoma: Results from the Phase IIIb/IV CheckMate 374 Study. Clin. Genitourin. Cancer 2020, 18, 461–468.e3. [Google Scholar] [CrossRef]
- De Vries-Brilland, M.; Gross-Goupil, M.; Seegers, V.; Boughalem, E.; Beuselinck, B.; Thibault, C.; Chevreau, C.; Ladoire, S.; Barthélémy, P.; Negrier, S.; et al. Are immune checkpoint inhibitors a valid option for papillary renal cell carcinoma? A multicentre retrospective study. Eur. J. Cancer 2020, 136, 76–83. [Google Scholar] [CrossRef]
- Rouvinov, K.; Osyntsov, L.; Shaco-Levy, R.; Baram, N.; Ariad, S.; Mermershtain, W. Rapid Response to Nivolumab in a Patient with Sarcomatoid Transformation of Chromophobe Renal Cell Carcinoma. Clin. Genitourin. Cancer 2017, 15, e1127–e1130. [Google Scholar] [CrossRef]
- Noguchi, G.; Tsutsumi, S.; Yasui, M.; Ohtake, S.; Umemoto, S.; Nakaigawa, N.; Yao, M.; Kishida, T. Significant response to nivolumab for metastatic chromophobe renal cell carcinoma with sarcomatoid differentiation: A case report. BMC Urol. 2018, 18, 26. [Google Scholar] [CrossRef]
- Ged, Y.; Chen, Y.B.; Knezevic, A.; Casuscelli, J.; Redzematovic, A.; DiNatale, R.G.; Carlo, M.I.; Lee, C.H.; Feldman, D.R.; Patil, S.; et al. Metastatic chromophobe renal cell carcinoma: Presence or absence of sarcomatoid differentiation determines clinical course and treatment outcomes. Clin. Genitourin. Cancer 2020, 17, e678–e688. [Google Scholar] [CrossRef] [PubMed]
- Sodji, Q.; Klein, K.; Sravan, K.; Parikh, J. Predictive role of PD-L1 expression in the response of renal Medullary carcinoma to PD-1 inhibition. J. Immunother. Cancer 2017, 5, 62. [Google Scholar] [CrossRef] [PubMed]
- Beckermann, K.E.; Jolly, P.C.; Kim, J.Y.; Bordeaux, J.; Puzanov, I.; Rathmell, W.K.; Johnson, D.B. Clinical and immunologic correlates of response to PD-1 blockade in a patient with metastatic renal medullary carcinoma. J. Immunother. Cancer 2017, 5, 1. [Google Scholar] [CrossRef] [PubMed]
- Oudard, S.; Banu, E.; Vieillefond, A.; Fournier, L.; Priou, F.; Medioni, J.; Banu, A.; Duclos, B.; Rolland, F.; Escudier, B.; et al. Prospective Multicenter Phase II Study of Gemcitabine Plus Platinum Salt for Metastatic Collecting Duct Carcinoma: Results of a GETUG (Groupe d’Etudes des Tumeurs Uro-Génitales) Study. J. Urol. 2007, 177, 1698–1702. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.Y.; Karam, J.A.; Malouf, G.G.; Rao, P.; Lim, Z.D.; Jonasch, E.; Xiao, L.; Gao, J.; Vaishampayan, U.N.; Heng, D.Y.; et al. Management and outcomes of patients with renal medullary carcinoma: A multicentre collaborative study. BJU Int. 2019, 120, 782–792. [Google Scholar] [CrossRef]
| Subtype of nccRCC | Cell Lines |
|---|---|
| pRCC | ACHN, Caki-2, UOK112, UOK268, UOK342, UOK275, SKRC-39, NCCFH1, and UOK262 |
| Chromophobe RCC | UOK276 |
| RMC | UOK353, UOK360 |
| Drug | Mechanism | Histologic Subtype | Therapeutic Effects of Drugs on nccRCC Patients | Survival Outcomes | Reference |
|---|---|---|---|---|---|
| Axitinib following progression on temsirolimus | TKI that targets VEGFRs, PDGFRs, and 2, and c-KIT | Papillary, chromophobe, MiT family translocation | Modest efficacy following progression on temsirolimus | Median PFS, ORR, median OS, and disease control rate were 7.4 months, 37.5%, 12.1 months, and 67.5%, respectively | [74] |
| Cabozantinib | Multi-target TKI that targets VEGFR2, c-MET, RET, Tyro3, Axl, and Mer | Papillary, chromophobe, MiT family translocation, and unclassified | Disease control in patients previously treated with VEGF-TKIs (savolitinib) | Median PFS, ORR, median OS, and disease control rate were 8.6 months, 14.3%, 25.4 months, and 78.6%, respectively | [75] |
| Metastatic papillary, chromophobe, Xp11.2 translocation, unclassified, collecting duct carcinoma | Antitumor activity and safety | Median PFS, ORR, and median OS were 7.0 months, 27%, and 25.4 months, respectively | [76] | ||
| Pazopanib following progression on temsirolimus | Anti-VEGF TKI that targets VEGFRs, FGFR 1 PDGFRs, and 2, and c-KIT | Metastatic papillary, chromophobe, unclassified | Modest efficacy and safety, median PFS and OS | Median PFS and ORR were 16.5 months and 28%, respectively; median overall survival was not reached | [77] |
| Lenvatinib + everolimus | Multi-target TKI (targets VEGFRs, and FGFR) + mTORC1 inhibitor | Papillary, chromophobe, unclassified | Modest efficacy as first-line therapy; may be more effective in chromophobe RCC | Median PFS, ORR, and median OS were 9.23 months, 25.8%, and 15.64 months, respectively | [78,79] |
| Bevacizumab + everolimus | TKI + mTORC1 inhibitor | Papillary, chromophobe, RMC, unclassified RCC | Modest efficacy as an additional option. more effective in pRCC | Median PFS, ORR, and median OS were 13.7 months, 35%, and 33.9 months, respectively | [80] |
| Everolimus | mTORC1 inhibitor | Metastatic pRCC | Favorable median PFS and OS, and safety | Median PFS and median OS were 7.9–11.0 and 28.0–24.2 months, respectively | [81] |
| Temsirolimus | mTORC1 and mTORC2 inhibitor | Papillary, chromophobe | Improved PFS, OS, and stable disease rate | Median TTP, ORR, and median OS were 3.9 months, 5%, and 11.2 months, respectively | [82,83,84,85] |
| Drug | Mechanism | Histologic Subtype | Therapeutic Effects of Drugs on nccRCC Patients | Reference |
|---|---|---|---|---|
| PD-1/PD-L1 blockade monotherapy | PD-1/PD-L1 pathway | Papillary, chromophobe, unclassified, translocation | Modest anti-tumor activity | [101] |
| Type 1 pRCC, type 2 pRCC and unclassified pRCC. | Limited activity in papillary tumor type and disease progression in 53% of patients | [108] | ||
| Nivolumab | PD-1/PD-L1 pathway | Papillary, unclassified, chromophobe, translocation mucinous tubular and spindle cell carcinoma | Clinical activity in unclassified nccRCC with no responses in chromophobe and papillary type 2 patients | [104] |
| Papillary, unclassified, chromophobe, collecting duct, Xp11 translocation and mucinous tubular and spindle cell carcinoma | Anti-tumor activity of nivolumab in papillary, unclassified, and collecting duct histologies | [105] | ||
| Papillary, chromophobe, unclassified, other | Safety and improved ORR, median PFS and median OS | [107] | ||
| Chromophobe | Modest activity as a second line treatment with partial response | [109] | ||
| Metastatic chromophobe | Clinical improvements with no significant side effects | [110] | ||
| Metastatic chromophobe | No objective responses | [111] | ||
| Metastatic renal medullary carcinoma | Responses only in patient 1 followed by progression after 15 months | [112] | ||
| Renal medullary carcinoma | Complete response for more than 9 months. | [113] | ||
| Pembrolizumab | PD-1/PD-L1 pathway | Papillary, chromophobe, unclassified | Safety and anti-tumor activity in nccRCC, more efficient in papillary subtype and unclassified | [93] |
| Ipilimumab + nivolumab | PD-1/PD-L1 pathway + CTLA-4 | Papillary, chromophobe, unclassified adenocarcinoma translocation medullary | Favorable ORR and median PFS | [106] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khoshdel Rad, N.; Vahidyeganeh, M.; Mohammadi, M.; Shpichka, A.; Timashev, P.; Hossein-Khannazer, N.; Vosough, M. Non-Clear Cell Renal Cell Carcinoma: Molecular Pathogenesis, Innovative Modeling, and Targeted Therapeutic Approaches. Int. J. Transl. Med. 2022, 2, 555-573. https://doi.org/10.3390/ijtm2040042
Khoshdel Rad N, Vahidyeganeh M, Mohammadi M, Shpichka A, Timashev P, Hossein-Khannazer N, Vosough M. Non-Clear Cell Renal Cell Carcinoma: Molecular Pathogenesis, Innovative Modeling, and Targeted Therapeutic Approaches. International Journal of Translational Medicine. 2022; 2(4):555-573. https://doi.org/10.3390/ijtm2040042
Chicago/Turabian StyleKhoshdel Rad, Niloofar, Maryam Vahidyeganeh, Mahsa Mohammadi, Anastasia Shpichka, Peter Timashev, Nikoo Hossein-Khannazer, and Massoud Vosough. 2022. "Non-Clear Cell Renal Cell Carcinoma: Molecular Pathogenesis, Innovative Modeling, and Targeted Therapeutic Approaches" International Journal of Translational Medicine 2, no. 4: 555-573. https://doi.org/10.3390/ijtm2040042
APA StyleKhoshdel Rad, N., Vahidyeganeh, M., Mohammadi, M., Shpichka, A., Timashev, P., Hossein-Khannazer, N., & Vosough, M. (2022). Non-Clear Cell Renal Cell Carcinoma: Molecular Pathogenesis, Innovative Modeling, and Targeted Therapeutic Approaches. International Journal of Translational Medicine, 2(4), 555-573. https://doi.org/10.3390/ijtm2040042







