BloodChain: A Blood Donation Network Managed by Blockchain Technologies
Abstract
:1. Introduction
2. Background
2.1. Blockchain Technology
2.2. Permission and Permissionless Blockchain Network
2.3. Hyperledger Fabric
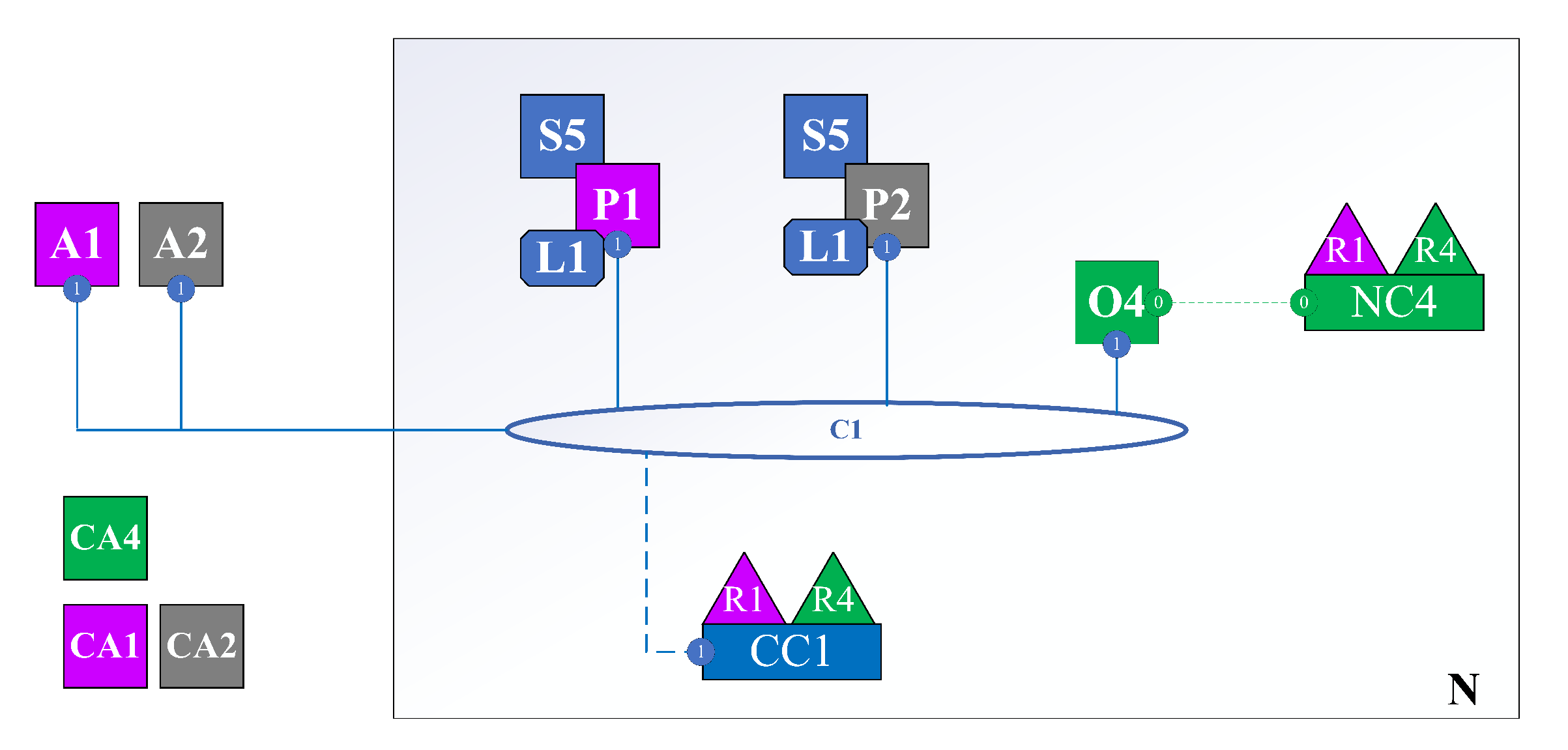
- N: Network.
- NC: Network Configuration.
- C: Channel. A collection of organizations with a certain role in the same business process. For example, two organizations, such as car manufacturers and car distributors, will be in a channel about buying and selling cars.
- CC: Channel Configuration.
- R: Organization.
- O: Orderer Node. In public blockchain, all network nodes participate in the consensus process; in Hyperledger Fabric, only the orderer participates in that process.
- P: Peer is the point of interaction between members of the organization corresponding to the channel. All user actions must go through the peer.
- S: Smart Contract (Chaincode) is installed on the channel, clearly defining structs, actions that users can perform to interact with the state of the struct stored in the ledger.
- CA: Certificate Authority. Issue identity assigned to user or node of the respective organization. For example, user A is a member of Organization R1. When he wants to join the network, he will request CA1. Then, CA1 will generate an identity consisting of a private key, a public key, and associated properties. Then, CA1 returns it to user A. From then on, A uses the identity to perform interactions with the network. The network automatically knows that it is user A from organization R1.
- A: Application. An application or an interface (web, mobile app) helps users interact with the system more easily.
2.4. Hyperledger Caliper
3. Related Work
3.1. Blockchain-Based Medical System
3.2. Blood Supply Chain Management System
3.3. Application of Blockchain Technologies Supply Chain Management
3.4. Limitation of Existing Research
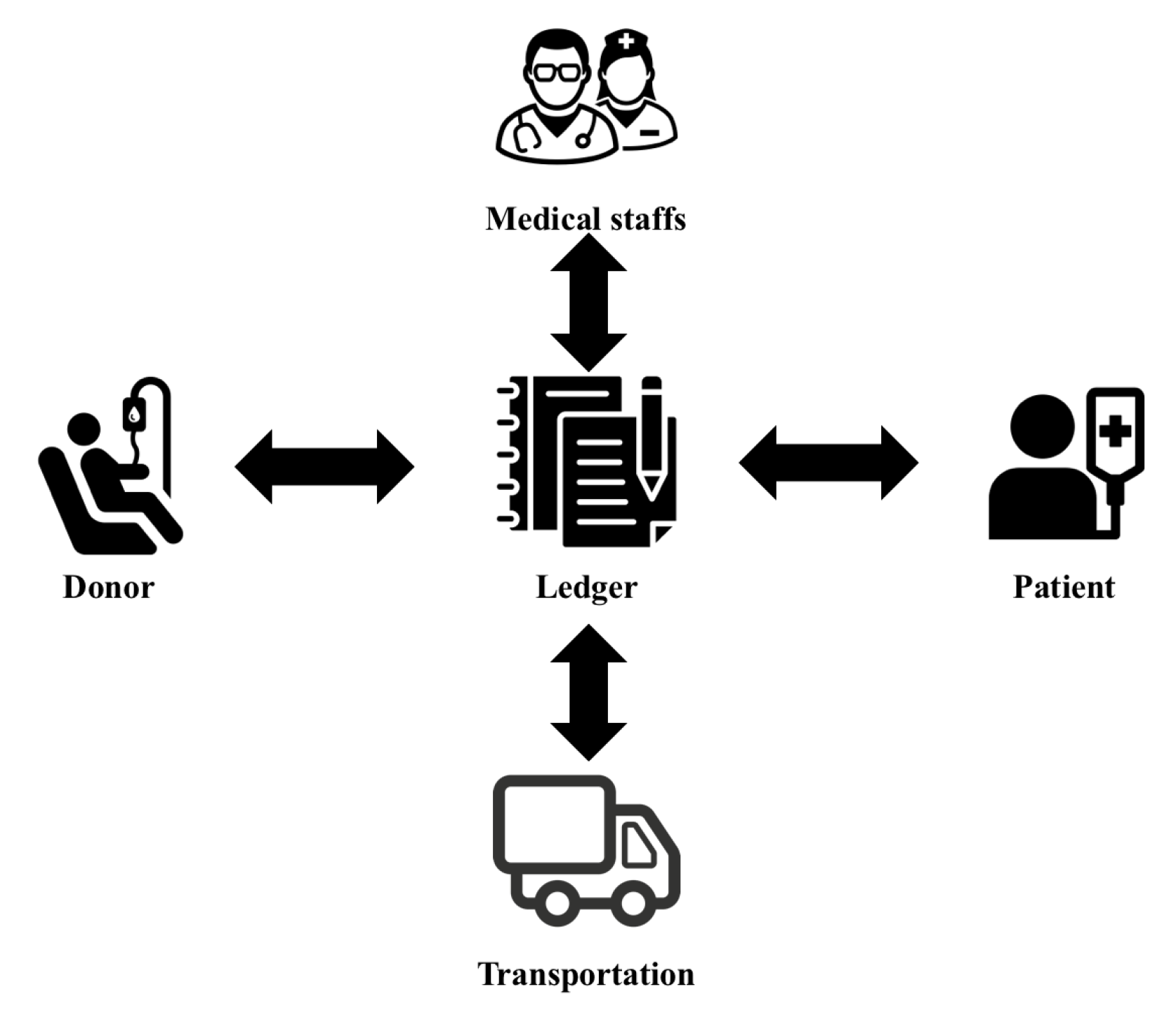
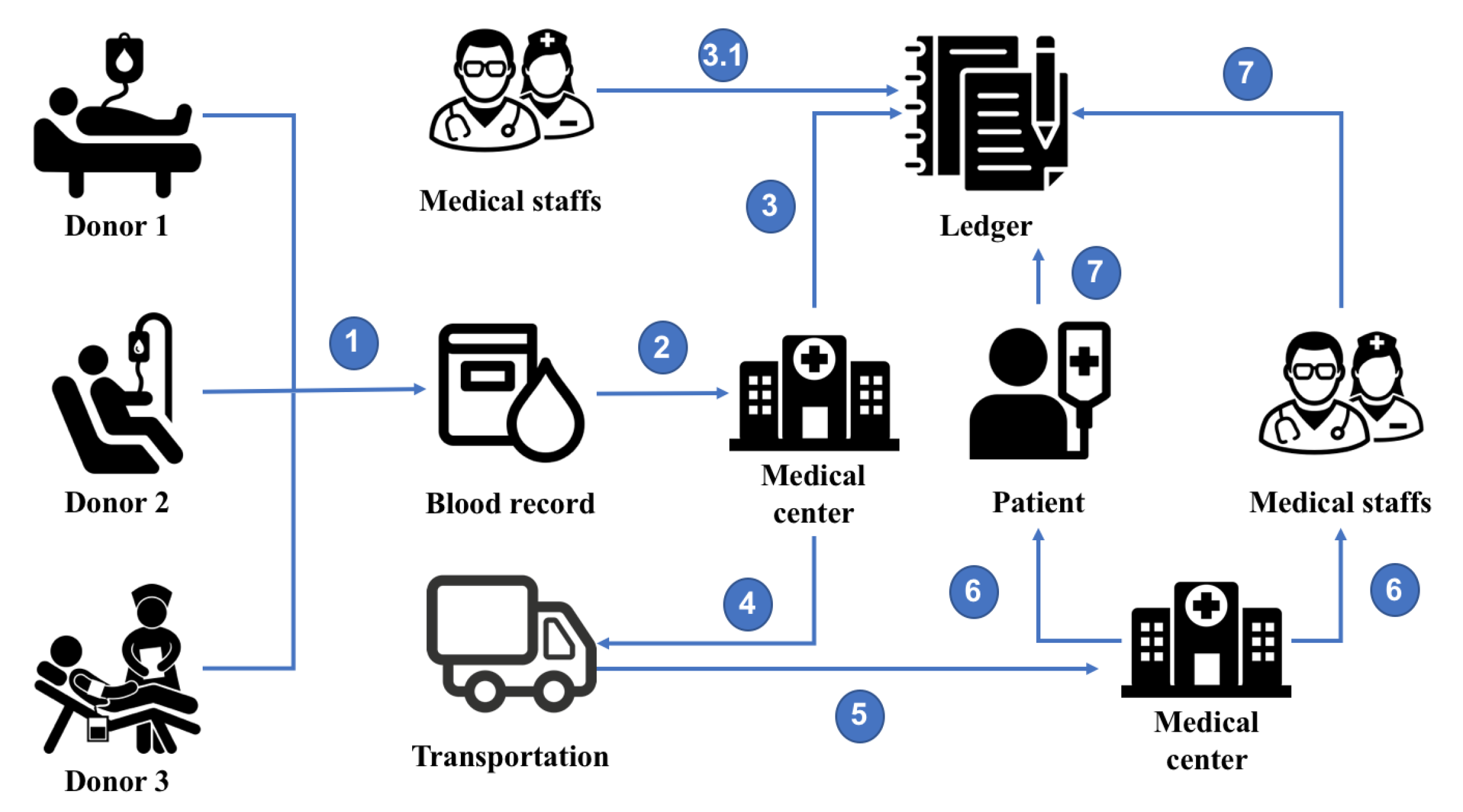
4. BloodChain Architecture
5. Implementation
5.1. Data Structure
5.2. Algorithms
| Algorithm 1: Storing blood samples of Volunteer. |
|
| Algorithm 2: Transportation of blood samples from donation places to medical center. |
|
6. Evaluation Scenarios
6.1. Environment Setting
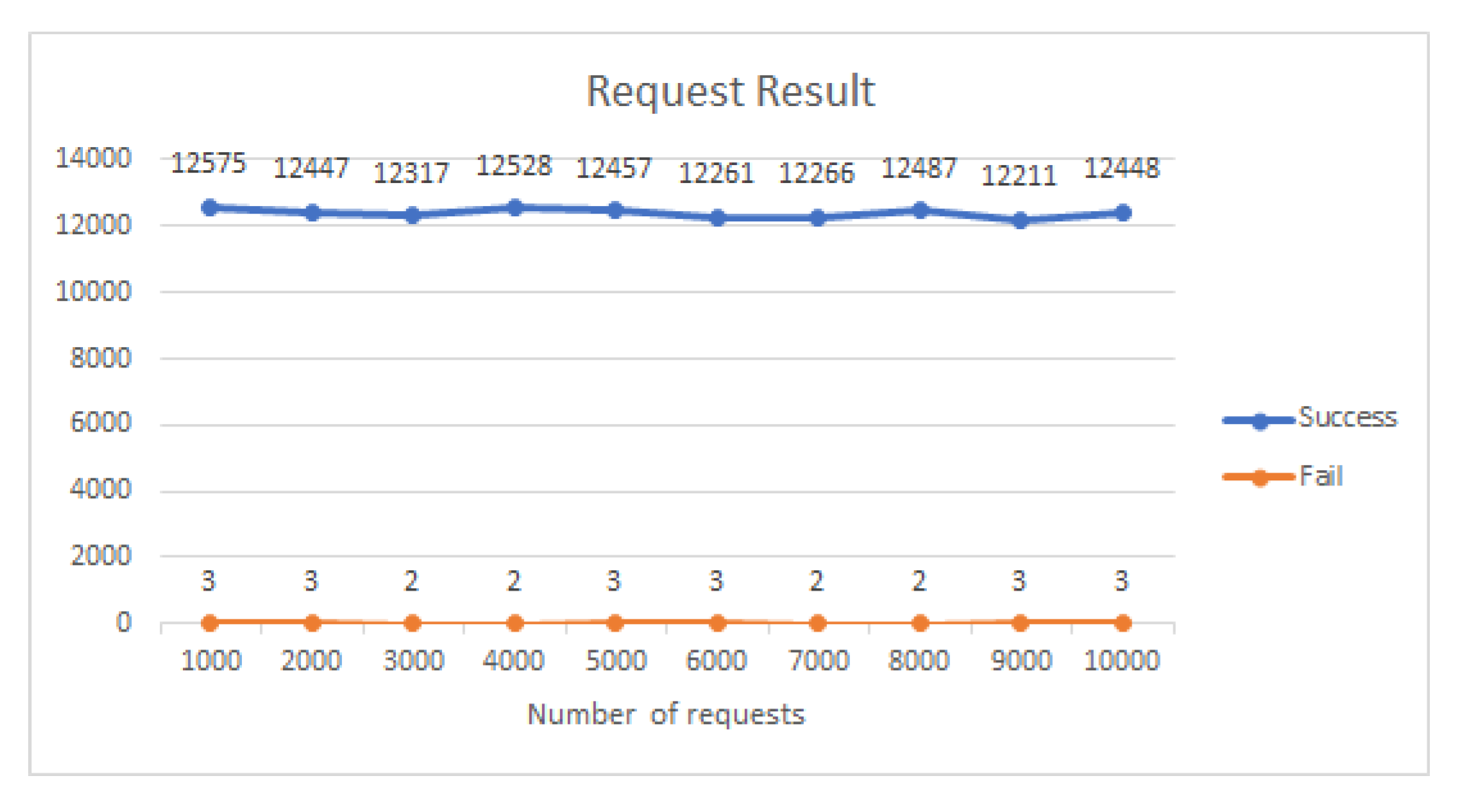
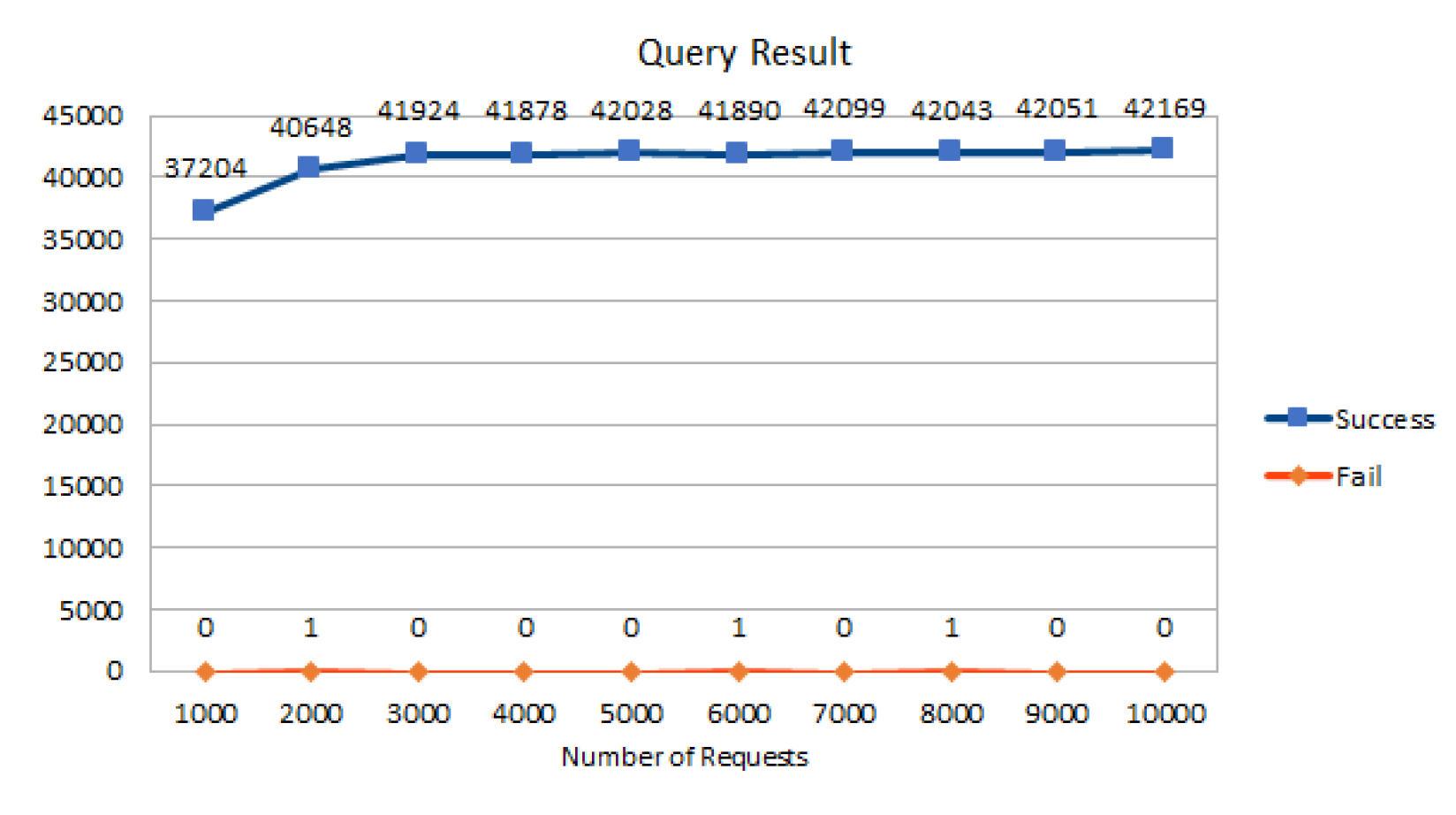
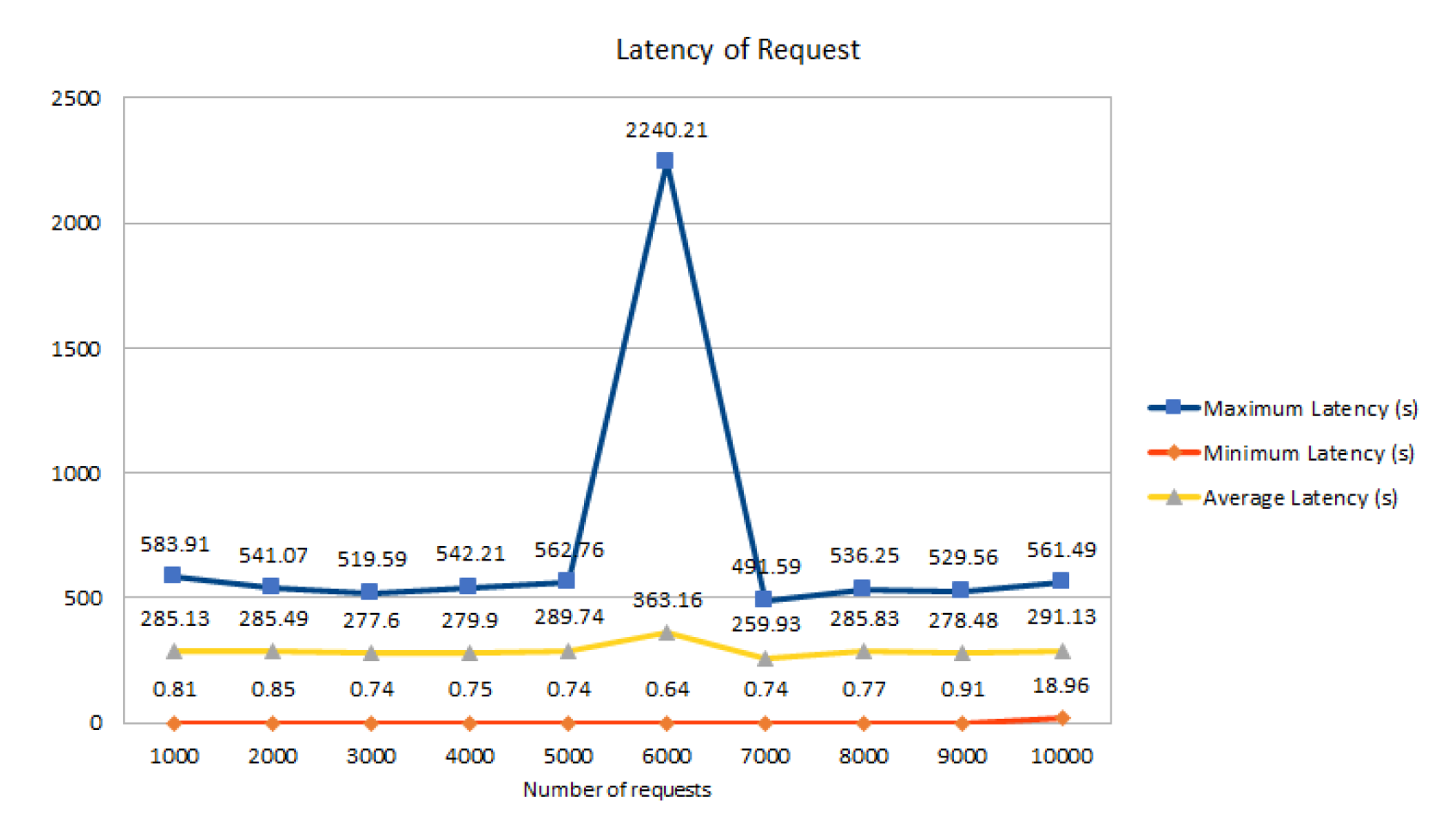
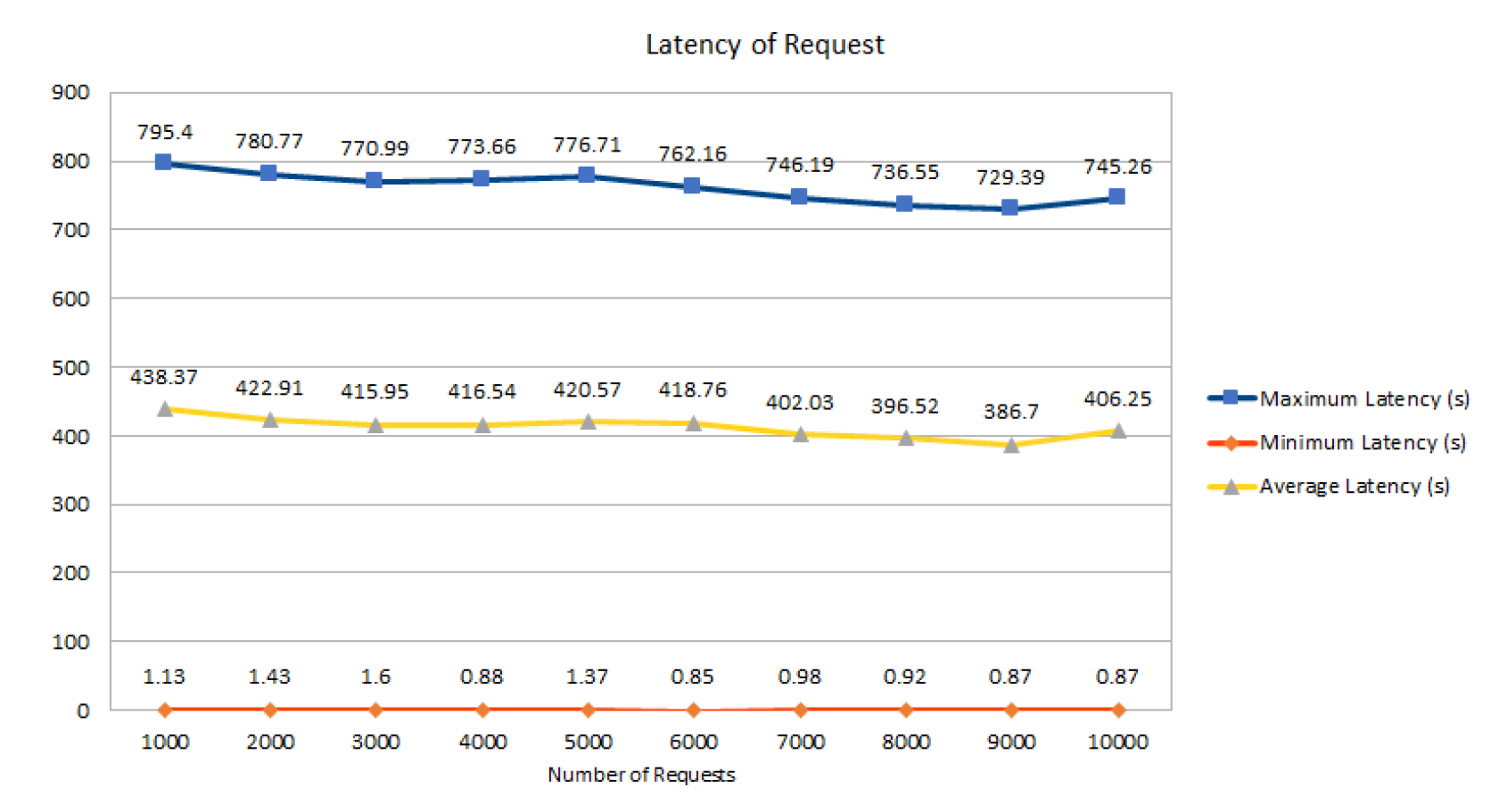
6.2. First Scenario
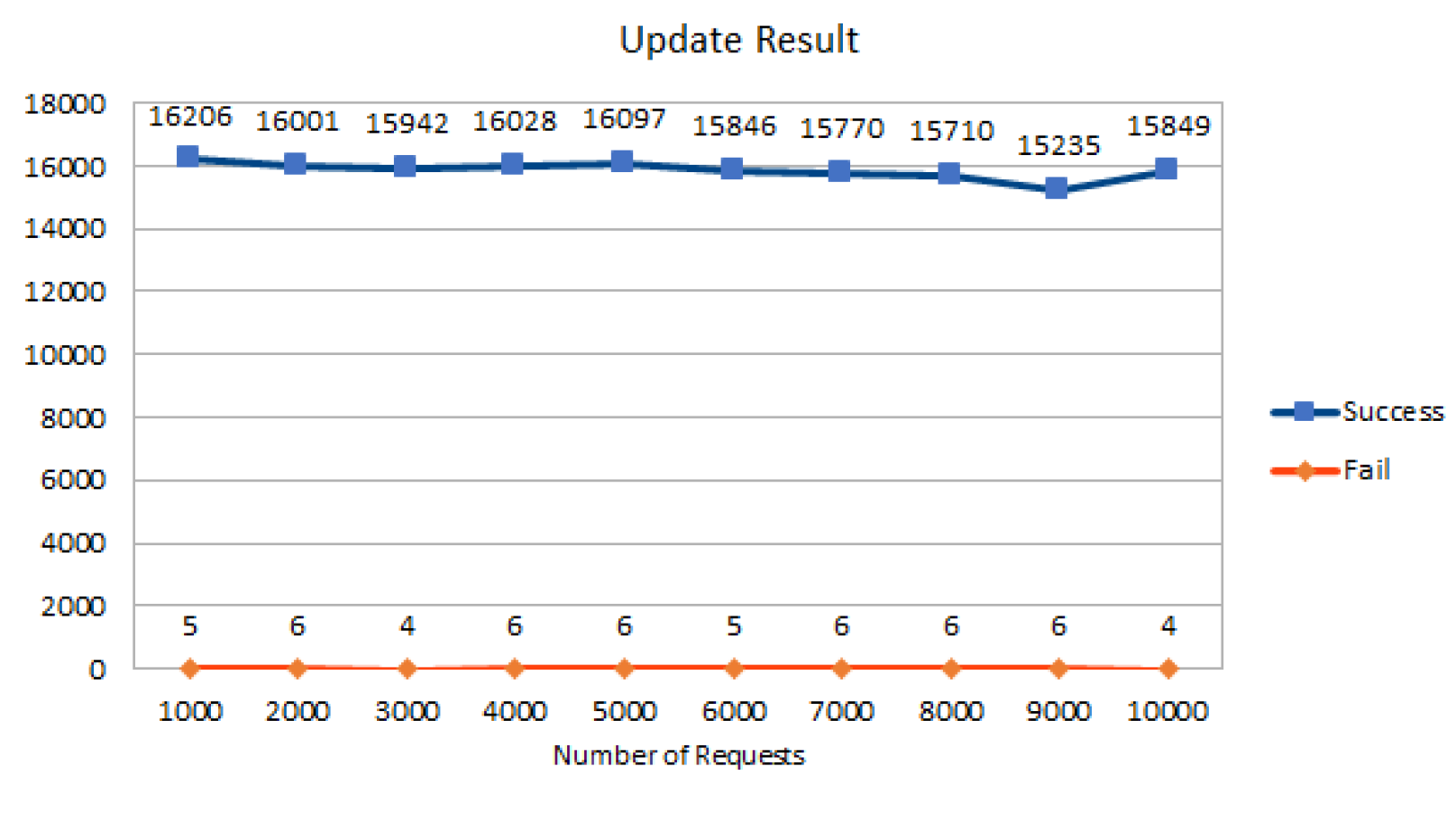
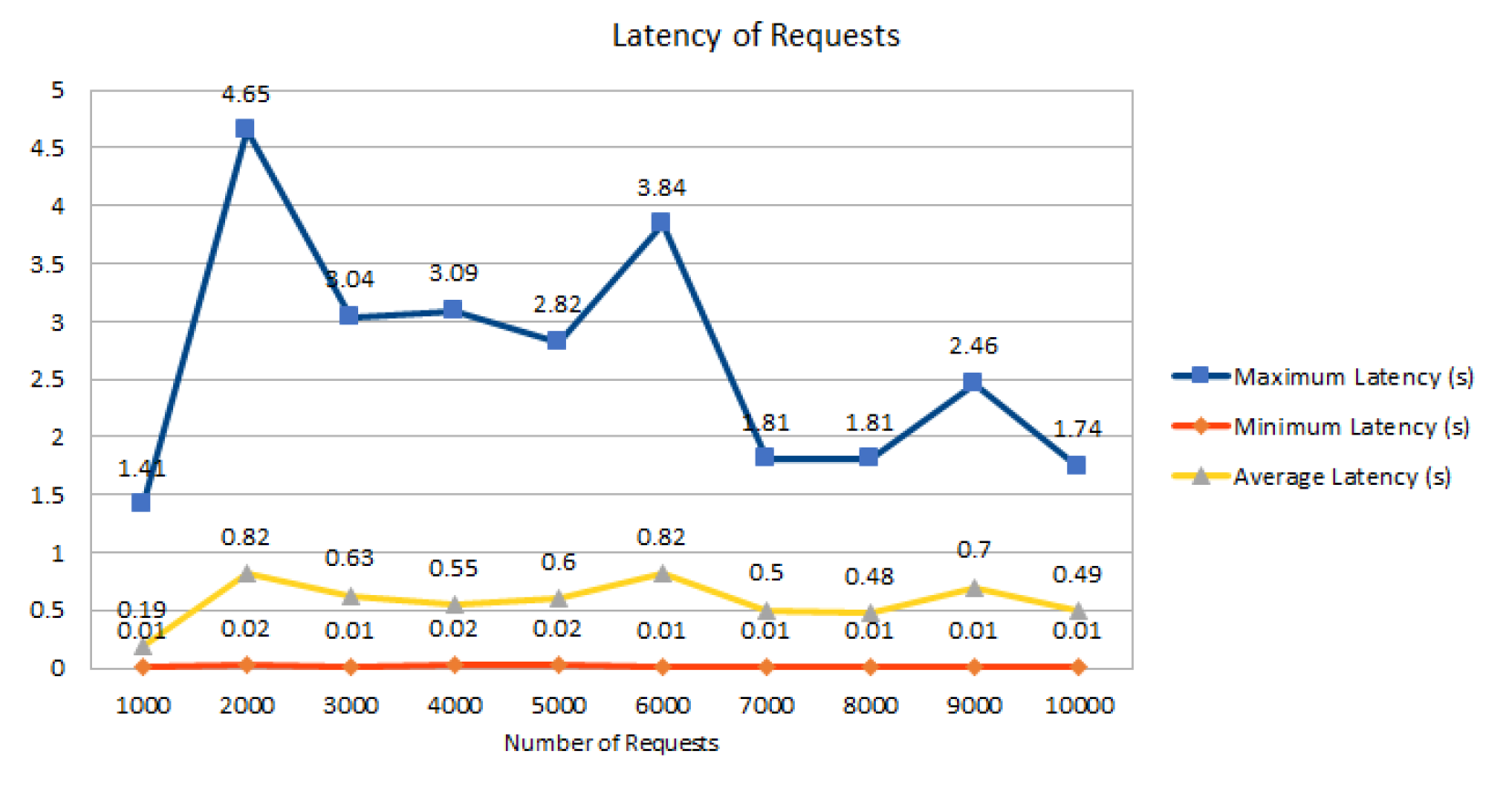
6.3. Second Scenario
6.4. Security and Privacy Discussion
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Nakamoto, S. Bitcoin: A Peer-to-Peer Electronic Cash System. Bitcoin.org. Disponible. 2009. Available online: https://bitcoin.org/en/bitcoin-paper (accessed on 25 November 2021).
- Le, N.T.T.; Nguyen, Q.N.; Phien, N.N.; Duong-Trung, N.; Huynh, T.T.; Nguyen, T.P.; Son, H.X. Assuring Non-fraudulent Transactions in Cash on Delivery by Introducing Double Smart Contracts. Int. J. Adv. Comput. Sci. Appl. 2019, 10, 677–684. [Google Scholar] [CrossRef]
- Le, H.T.; Le, N.T.T.; Phien, N.N.; Duong-Trung, N. Introducing multi shippers mechanism for decentralized cash on delivery system. Int. J. Adv. Comput. Sci. Appl. 2019, 10, 590–597. [Google Scholar] [CrossRef]
- Ha, X.S.; Le, H.T.; Metoui, N.; Duong-Trung, N. Dem-cod: Novel access-control-based cash on delivery mechanism for decentralized marketplace. In Proceedings of the 2020 IEEE 19th International Conference on Trust, Security and Privacy in Computing and Communications (TrustCom), Guangzhou, China, 10–13 November 2020; pp. 71–78. [Google Scholar]
- Ha, X.S.; Le, T.H.; Phan, T.T.; Nguyen, H.H.D.; Vo, H.K.; Duong-Trung, N. Scrutinizing trust and transparency in cash on delivery systems. In Proceedings of the International Conference on Security, Privacy and Anonymity in Computation, Communication and Storage, Nanjing, China, 18–20 December 2020; pp. 214–227. [Google Scholar]
- Son, H.X.; Le, T.H.; Quynh, N.T.T.; Huy, H.N.D.; Duong-Trung, N.; Luong, H.H. Toward a Blockchain-Based Technology in Dealing with Emergencies in Patient-Centered Healthcare Systems. In Proceedings of the International Conference on Mobile, Secure, and Programmable Networking, Paris, France, 28–29 October 2020; pp. 44–56. [Google Scholar]
- Duong-Trung, N.; Son, H.X.; Le, H.T.; Phan, T.T. On Components of a Patient-Centered Healthcare System Using Smart Contract. In Proceedings of the 2020 4th International Conference on Cryptography, Security and Privacy, Nanjing China, 10–12 January 2020; Association for Computing Machinery: New York, NY, USA, 2020; pp. 31–35. [Google Scholar] [CrossRef] [Green Version]
- Duong-Trung, N.; Son, H.X.; Le, H.T.; Phan, T.T. Smart Care: Integrating Blockchain Technology into the Design of Patient-Centered Healthcare Systems. In Proceedings of the 2020 4th International Conference on Cryptography, Security and Privacy, ICCSP 2020, Nanjing, China, 10–12 January 2020; Association for Computing Machinery: New York, NY, USA, 2020; pp. 105–109. [Google Scholar] [CrossRef] [Green Version]
- Thanh, L.N.T.; Nguyen, T.A.; Vo, H.K.; Luong, H.H.; Nguyen, H.T.K.; Dao, A.T.; Ha, X.S. Toward a Unique IoT Network via Single Sign-On Protocol and Message Queue. In Proceedings of the International Conference on Computer Information Systems and Industrial Management, Ełk, Poland, 24–26 September 2021. [Google Scholar]
- Thanh, L.N.T.; Phien, N.N.; Vo, H.K.; Luong, H.H.; Anh, T.D.; Tuan, K.N.H.; Son, H.X. UIP2SOP: A Unique IoT Network applying Single Sign-On and Message Queue Protocol. Int. J. Adv. Comput. Sci. Appl. 2021, 12, 19–30. [Google Scholar] [CrossRef]
- Thanh, L.N.T.; Nguyen, T.A.; Vo, H.K.; Luong, H.H.; Tuan, K.N.H.; Dao, A.T.; Son, H.X. Toward a Security IoT Platform with High Rate Transmission and Low Energy Consumption. In Proceedings of the International Conference on Computational Science and its Applications, Cagliari, Italy, 13–16 September 2021. [Google Scholar]
- Son, H.X.; Nguyen, M.H.; Vo, H.K. Toward an privacy protection based on access control model in hybrid cloud for healthcare systems. In Advances in Intelligent Systems and Computing, Proceedings of the International Joint Conference: 12th International Conference on Computational Intelligence in Security for Information Systems (CISIS 2019) and 10th International Conference on EUropean Transnational Education (ICEUTE 2019), Seville, Spain, 13–15 May 2019; Springer: Cham, Switzerland, 2019; pp. 77–86. [Google Scholar]
- Thanh, L.N.T.; Phien, N.N.; Nguyen, T.A.; Vo, H.K.; Luong, H.H.; Anh, T.D.; Tuan, K.N.H.; Son, H.X. IoHT-MBA: An Internet of Healthcare Things (IoHT) Platform based on Microservice and Brokerless Architecture. Int. J. Adv. Comput. Sci. Appl. 2021, 12. [Google Scholar] [CrossRef]
- Hajipour, V.; Niaki, S.T.A.; Akhgar, M.; Ansari, M. The healthcare supply chain network design with traceability: A novel algorithm. Comput. Ind. Eng. 2021, 161, 107661. [Google Scholar] [CrossRef]
- Ho, G.; Tang, Y.M.; Tsang, K.Y.; Tang, V.; Chau, K.Y. A blockchain-based system to enhance aircraft parts traceability and trackability for inventory management. Expert Syst. Appl. 2021, 179, 115101. [Google Scholar] [CrossRef]
- Emmanuel, J.C. The Blood Cold Chain; WHO Report: Geneva, Switzerland, 2017. [Google Scholar]
- Baek, E.J.; Kim, H.O.; Kim, S.; Park, Q.E.; Oh, D.J. The trends for nationwide blood collection and the supply of blood in Korea during 2002–2006. Korean J. Blood Transfus. 2008, 19, 83–90. [Google Scholar]
- Delaforce, A.; Duff, J.; Munday, J.; Hardy, J. Overcoming barriers to evidence-based patient blood management: A restricted review. Implement. Sci. 2020, 15, 1–13. [Google Scholar] [CrossRef]
- Ahram, T.; Sargolzaei, A.; Sargolzaei, S.; Daniels, J.; Amaba, B. Blockchain technology innovations. In Proceedings of the 2017 IEEE Technology & Engineering Management Conference (TEMSCON), Santa Clara, CA, USA, 8–10 June 2017; pp. 137–141. [Google Scholar]
- Michael, J.; Cohn, A.; Butcher, J.R. Blockchain Technology. Available online: https://www.steptoe.com/images/content/1/7/v3/171269/LIT-FebMar18-Feature-Blockchain.pdf (accessed on 1 December 2021).
- Shahriar Hazari, S.; Mahmoud, Q.H. Improving Transaction Speed and Scalability of Blockchain Systems via Parallel Proof of Work. Future Internet 2020, 12, 125. [Google Scholar] [CrossRef]
- Qu, Q.; Xu, R.; Chen, Y.; Blasch, E.; Aved, A. Enable Fair Proof-of-Work (PoW) Consensus for Blockchains in IoT by Miner Twins (MinT). Future Internet 2021, 13, 291. [Google Scholar] [CrossRef]
- Feng, L.; Zhang, H.; Chen, Y.; Lou, L. Scalable dynamic multi-agent practical byzantine fault-tolerant consensus in permissioned blockchain. Appl. Sci. 2018, 8, 1919. [Google Scholar] [CrossRef] [Green Version]
- Nijsse, J.; Litchfield, A. A Taxonomy of Blockchain Consensus Methods. Cryptography 2020, 4, 32. [Google Scholar] [CrossRef]
- Androulaki, E.; Barger, A.; Bortnikov, V.; Cachin, C.; Christidis, K.; De Caro, A.; Enyeart, D.; Ferris, C.; Laventman, G.; Manevich, Y.; et al. Hyperledger fabric: A distributed operating system for permissioned blockchains. In Proceedings of the Thirteenth EuroSys Conference, Porto, Portugal, 23–26 April 2018; pp. 1–15. [Google Scholar]
- Díaz-Santiso, J.; Fraga-Lamas, P. E-Voting System Using Hyperledger Fabric Blockchain and Smart Contracts. Eng. Proc. 2021, 7, 11. [Google Scholar] [CrossRef]
- Kumar, T.; Ramani, V.; Ahmad, I.; Braeken, A.; Harjula, E.; Ylianttila, M. Blockchain utilization in healthcare: Key requirements and challenges. In Proceedings of the 2018 IEEE 20th International Conference on e-Health Networking, Applications and Services (Healthcom), Ostrava, Czech Republic, 17–20 September 2018; pp. 1–7. [Google Scholar]
- de Oliveira, M.T.; Reis, L.H.; Carrano, R.C.; Seixas, F.L.; Saade, D.C.; Albuquerque, C.V.; Fernandes, N.C.; Olabarriaga, S.D.; Medeiros, D.S.; Mattos, D.M. Towards a blockchain-based secure electronic medical record for healthcare applications. In Proceedings of the ICC 2019-2019 IEEE International Conference on Communications (ICC), Shanghai, China, 20–24 May 2019; pp. 1–6. [Google Scholar]
- Wilber, K.; Vayansky, S.; Costello, N.; Berdik, D.; Jararweh, Y. A Survey on Blockchain for Healthcare Informatics and Applications. In Proceedings of the 2020 7th International Conference on Internet of Things: Systems, Management and Security (IOTSMS), Paris, France, 14–16 December 2020; pp. 1–9. [Google Scholar]
- Shynu, P.; Menon, V.G.; Kumar, R.L.; Kadry, S.; Nam, Y. Blockchain-based secure healthcare application for diabetic-cardio disease prediction in fog computing. IEEE Access 2021, 9, 45706–45720. [Google Scholar] [CrossRef]
- Torky, M.; Hassanien, A.E. COVID-19 blockchain framework: Innovative approach. arXiv 2020, arXiv:2004.06081. [Google Scholar]
- Kim, D. An integrated supply chain management system: A case study in healthcare sector. In Proceedings of the International Conference on Electronic Commerce and Web Technologies, Copenhagen, Denmark, 23–26 August 2005; pp. 218–227. [Google Scholar]
- Shahbaz, M.S.; RM, R.Z.; Bin, M.F.; Rehman, F. What is supply chain risk management? A review. Adv. Sci. Lett. 2017, 23, 9233–9238. [Google Scholar] [CrossRef]
- Lavastre, O.; Gunasekaran, A.; Spalanzani, A. Effect of firm characteristics, supplier relationships and techniques used on supply chain risk management (SCRM): An empirical investigation on French industrial firms. Int. J. Prod. Res. 2014, 52, 3381–3403. [Google Scholar] [CrossRef]
- Nagurney, A.; Masoumi, A.H.; Yu, M. Supply chain network operations management of a blood banking system with cost and risk minimization. Comput. Manag. Sci. 2012, 9, 205–231. [Google Scholar] [CrossRef]
- Armaghan, N.; Pazani, N. A Model For Designing A Blood Supply Chain Network To Earthquake Disasters (Case Study: Tehran City). Int. J. Qual. Res. 2019, 13, 605–624. [Google Scholar] [CrossRef]
- Eskandari-Khanghahi, M.; Tavakkoli-Moghaddam, R.; Taleizadeh, A.A.; Amin, S.H. Designing and optimizing a sustainable supply chain network for a blood platelet bank under uncertainty. Eng. Appl. Artif. Intell. 2018, 71, 236–250. [Google Scholar] [CrossRef]
- Delen, D.; Erraguntla, M.; Mayer, R.J.; Wu, C.N. Better management of blood supply-chain with GIS-based analytics. Ann. Oper. Res. 2011, 185, 181–193. [Google Scholar] [CrossRef]
- Crosby, M.; Pattanayak, P.; Verma, S.; Kalyanaraman, V. Blockchain technology: Beyond bitcoin. Appl. Innov. 2016, 2, 71. [Google Scholar]
- Hackius, N.; Petersen, M. Blockchain in logistics and supply chain: Trick or treat? In Digitalization in Supply Chain Management and Logistics: Smart and Digital Solutions for an Industry 4.0 Environment, Proceedings of the Hamburg International Conference of Logistics (HICL), Hamburg, Germany, 12–13 October 2017; Epubli GmbH: Berlin, Germany, 2017; Volume 23, pp. 3–18. [Google Scholar]
- Mettler, M. Blockchain technology in healthcare: The revolution starts here. In Proceedings of the 2016 IEEE 18th International Conference on e-Health Networking, Applications and Services (Healthcom), Munich, Germany, 14–17 September 2016; pp. 1–3. [Google Scholar]
- Quynh, N.T.T.; Son, H.X.; Le, T.H.; Huy, H.N.D.; Vo, K.H.; Luong, H.H.; Tuan, K.N.H.; Anh, T.D.; Duong-Trung, N. Toward a Design of Blood Donation Management by Blockchain Technologies. In Proceedings of the International Conference on Computational Science and Its Applications, Cagliari, Italy, 13–16 September 2021; pp. 78–90. [Google Scholar]
- Hölbl, M.; Kompara, M.; Kamišalić, A.; Nemec Zlatolas, L. A systematic review of the use of blockchain in healthcare. Symmetry 2018, 10, 470. [Google Scholar] [CrossRef] [Green Version]
- Yaga, D.; Mell, P.; Roby, N.; Scarfone, K. Blockchain technology overview. arXiv 2019, arXiv:1906.11078. [Google Scholar]
- Wüst, K.; Gervais, A. Do you need a blockchain? In Proceedings of the 2018 Crypto Valley Conference on Blockchain Technology (CVCBT), Zug, Switzerland, 20–22 June 2018; pp. 45–54. [Google Scholar]
- Pradhan, N.R.; Singh, A.P.; Kumar, V. Blockchain-enabled traceable, transparent transportation system for blood bank. In Advances in VLSI, Communication, and Signal Processing; Springer: Cham, Switzerland, 2021; pp. 313–324. [Google Scholar]
- Campanile, L.; Iacono, M.; Levis, A.H.; Marulli, F.; Mastroianni, M. Privacy Regulations, Smart Roads, Blockchain, and Liability Insurance: Putting Technologies to Work. IEEE Secur. Priv. 2020, 19, 34–43. [Google Scholar] [CrossRef]
- Kshetri, N. Blockchain’s roles in strengthening cybersecurity and protecting privacy. Telecommun. Policy 2017, 41, 1027–1038. [Google Scholar] [CrossRef] [Green Version]
- Joshi, A.P.; Han, M.; Wang, Y. A survey on security and privacy issues of blockchain technology. Math. Found. Comput. 2018, 1, 121. [Google Scholar] [CrossRef] [Green Version]
- Hoang, N.M.; Son, H.X. A dynamic solution for fine-grained policy conflict resolution. In Proceedings of the 3rd International Conference on Cryptography, Security and Privacy, Kuala Lumpur, Malaysia, 19–21 January 2019; pp. 116–120. [Google Scholar]
- Son, H.X.; Hoang, N.M. A novel attribute-based access control system for fine-grained privacy protection. In Proceedings of the 3rd International Conference on Cryptography, Security and Privacy, Kuala Lumpur, Malaysia, 19–21 January 2019; pp. 76–80. [Google Scholar]
- Son, H.X.; Dang, T.K.; Massacci, F. REW-SMT: A new approach for rewriting xacml request with dynamic big data security policies. In Proceedings of the International Conference on Security, Privacy and Anonymity in Computation, Communication and Storage, Guangzhou, China, 12–15 December 2017; pp. 501–515. [Google Scholar]
- Xuan, S.H.; Tran, L.K.; Dang, T.K.; Pham, Y.N. Rew-xac: An approach to rewriting request for elastic abac enforcement with dynamic policies. In Proceedings of the 2016 International Conference on Advanced Computing and Applications (ACOMP), Tho City, Vietnam, 23–25 November 2016; pp. 25–31. [Google Scholar]
- Son, H.X.; Chen, E. Towards a fine-grained access control mechanism for privacy protection and policy conflict resolution. Int. J. Adv. Comput. Sci. Appl. 2019, 10, 507–516. [Google Scholar] [CrossRef] [Green Version]
- Thi, Q.N.T.; Dang, T.K.; Van, H.L.; Son, H.X. Using json to specify privacy preserving-enabled attribute-based access control policies. In Proceedings of the International Conference on Security, Privacy and Anonymity in Computation, Communication and Storage, Guangzhou, China, 12–25 December 2017; pp. 561–570. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Le, H.T.; Nguyen, T.T.L.; Nguyen, T.A.; Ha, X.S.; Duong-Trung, N. BloodChain: A Blood Donation Network Managed by Blockchain Technologies. Network 2022, 2, 21-35. https://doi.org/10.3390/network2010002
Le HT, Nguyen TTL, Nguyen TA, Ha XS, Duong-Trung N. BloodChain: A Blood Donation Network Managed by Blockchain Technologies. Network. 2022; 2(1):21-35. https://doi.org/10.3390/network2010002
Chicago/Turabian StyleLe, Hai Trieu, Tran Thanh Lam Nguyen, Tuan Anh Nguyen, Xuan Son Ha, and Nghia Duong-Trung. 2022. "BloodChain: A Blood Donation Network Managed by Blockchain Technologies" Network 2, no. 1: 21-35. https://doi.org/10.3390/network2010002
APA StyleLe, H. T., Nguyen, T. T. L., Nguyen, T. A., Ha, X. S., & Duong-Trung, N. (2022). BloodChain: A Blood Donation Network Managed by Blockchain Technologies. Network, 2(1), 21-35. https://doi.org/10.3390/network2010002





