Pilot Study of a Resiliency Based and Trauma Informed Intervention for Veterans
Abstract
1. Background and Introduction
Veteran Extension Project
2. Methods
2.1. Participant Characteristics
2.2. Procedure
2.3. Measures
2.3.1. Treatment Relevance, Use & Satisfaction (TRUSS)
2.3.2. Symptom Questionnaire (SQ)
2.3.3. Daily Functioning Form (DFF)
2.3.4. Brief CRM Questionnaire (Brief CRM)
2.4. Data Analyses
3. Results
3.1. Treatment Relevance, Use & Satisfaction
3.2. Symptom Questionnaire
3.3. Daily Functioning Form
3.4. Brief CRM Questionnaire
4. Discussion
Study Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Substance Abuse and Behavioral health Services Administration. Key Substance Use and Behavioral Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health; (HHS Publication No. PEP20-07-01-001); Center for Behavioral Health Statistics and Quality, Substance Abuse and Behavioral Health Services Administration: Rockville, MD, USA, 2020. Available online: https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR1PDFW090120.pdf (accessed on 15 December 2023).
- Trivedi, R.B.; Post, E.P.; Sun, H.; Pomerantz, A.; Saxon, A.J.; Piette, J.D.; Maynard, C.; Arnow, B.; Curtis, I.; Fihn, S.D.; et al. Prevalence, comorbidity, and prognosis of mental health among US veterans. Am. J. Public Health 2015, 105, 2564–2569. [Google Scholar] [CrossRef] [PubMed]
- Doran, J.M.; Deviva, J. A Naturalistic Evaluation of Evidence-Based Treatments for Veterans With PTSD. Traumatology 2018, 24, 157–167. [Google Scholar] [CrossRef]
- Elbogen, E.B.; Wagner, H.R.; Johnson, S.C.; Kinneer, P.; Kang, H.; Vasterling, J.J.; Timko, C.; Beckham, J.C. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatr. Serv. 2013, 64, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Reijnen, A.; Rademaker, A.R.; Vermetten, E.; Geuze, E. Prevalence of mental health symptoms in Dutch military personnel returning from deployment to Afghanistan: A 2-year longitudinal analysis. Eur. Psychiatry 2015, 30, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Shea, M.T.; Stout, R.L.; Reddy, M.K.; Sevin, E.; Presseau, C.; Lambert, J.; Cameron, A. Treatment of anger problems in previously deployed post-911 veterans: A randomized controlled trial. Depress. Anxiety 2022, 39, 274–285. [Google Scholar] [CrossRef] [PubMed]
- Taft, C.T.; Watkins, L.E.; Stafford, J.; Street, A.E.; Monson, C.M. Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. J. Consult. Clin. Psychol. 2011, 79, 22. [Google Scholar] [CrossRef]
- Scott, J.; Matt, G.; Wroklage, K.; Crnich, C.; Jordan, J.; Southwick, S.; Krystal, J.; Schweinsburg, B. A Quantitative Meta-Analysis of Neurocognitive Functioning in Posttraumatic Stress Disorder. Psychol. Bull. 2015, 141, 105–140. [Google Scholar] [CrossRef] [PubMed]
- Elgoben, E.B.; Cueva, M.; Wagner, H.R.; Sreenivasan, S.; Brancu, M.; Beckham, J.C.; Male, L.V. Screening for violence risk in military veterans: Predictive validity of a brief clinical tool. Am. J. Psychiatry 2014, 171, 749–757. [Google Scholar]
- Herbst, E. Overcoming barriers to care for returning veterans: Expanding services to college campuses. J. Rehabil. Res. Dev. 2013, 50, VII. [Google Scholar]
- US Department of Veterans Affairs. 2023 National Veteran Suicide Prevention Annual Report [PDF]. 2023. Available online: https://www.mentalhealth.va.gov/docs/data-sheets/2023/2023-National-Veteran-Suicide-Prevention-Annual-Report-FINAL-508.pdf (accessed on 20 December 2023).
- Krill Williston, S.; Martinez, J.H.; Abdullah, T. Mental health stigma among people of color: An examination of the impact of racial discrimination. Int. J. Soc. Psychiatry 2019, 65, 458–467. [Google Scholar] [CrossRef]
- Kline, A.C.; Panza, K.E.; Nichter, B.; Tsai, J.; Harpaz-Rotem, I.; Norman, S.B.; Pietrzak, R.H. Mental health care use among US military veterans: Results from the 2019–2020 National Health and Resilience in Veterans Study. Psychiatr. Serv. 2022, 73, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Bovin, M.; Miller, C.; Koenig, C.J.; Lipschitz, J.M.; Zamora, K.A.; Wright, P.; Pyne, J.M.; Burgess, J.F. Veterans’ experiences initiating VA-based behavioral health care. Psychol. Serv. 2019, 16, 612–620. [Google Scholar] [CrossRef]
- Freeman, K.; Baek, K.; Ngo, M.; Karas, E.; Cirtron, S.; Montgomery, S. Exploring the usability of a community resiliency model approach in a high need/low research traumatized community. Community Behav. Health J. 2021, 58, 679–688. [Google Scholar] [CrossRef]
- Perkins, D.F.; Aronson, K.R.; Morgan, N.R.; Bleser, J.A.; Vogt, D.; Copeland, L.A.; Finley, E.P.; Gilman, C. Veterans’ use of programs and services as they transition to civilian life: Baseline assessment for the Veteran Metrics Initiative. J. Soc. Serv. Res. 2020, 46, 241–255. [Google Scholar] [CrossRef]
- Yankellevich, A.; Goodman, Y.; Goodman, Y.C. “You can’t choose these emotions…they simply jump up”: Ambiguities in Resilience-Building Interventions in Israel. Cult. Med. Psychiatry 2017, 41, 56–74. [Google Scholar] [CrossRef] [PubMed]
- Miller-Karas, E. Resilience and trauma defined. In Building Resilience to Trauma; Routledge: London, UK, 2015; pp. 21–29. [Google Scholar]
- Saul, J.; Simon, W. Building Resilience in Families, Communities, and Organizations: A Training Program in Global Behavioral health and Psychosocial Support. Fam. Process 2016, 55, 689–699. [Google Scholar] [CrossRef]
- Kang, S.S.; Erbes, C.R.; Lamberty, G.J.; Thuras, P.; Sponheim, S.R.; Polusny, M.A.; Moran, A.C.; Van Voorhis, A.C.; Lim, K.O. Transcendental meditation for veterans with post-traumatic stress disorder. Psychol. Trauma Theory Res. Pract. Policy 2018, 10, 675. [Google Scholar] [CrossRef]
- Smith, N.B.; Mota, N.; Tsai, J.; Monteith, L.; Harpaz-Rotem, I.; Southwick, S.M.; Pietrzak, R.H. Nature and determinants of suicidal ideation among US veterans: Results from the national health and resilience in veterans study. J. Affect. Disord. 2016, 197, 66–73. [Google Scholar] [CrossRef]
- Isaacs, K.; Mota, N.P.; Tsai, J.; Harpaz-Rotem, I.; Cook, J.M.; Kirwin, P.D.; Krystal, J.H.; Southwick, S.M.; Pietrzak, R.H. Psychological resilience in US military veterans: A 2-year, nationally representative prospective cohort study. J. Psychiatr. Res. 2017, 84, 301–309. [Google Scholar] [CrossRef]
- Villalpando, L.S.; McReynolds, C.J.; Lee, G.; Montgomery, S.; Vermeersch, D. Neurofeedback: An examination of attentional processes in adults with self-reported PTSD symptoms. NeuroRegulation 2020, 7, 142. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Cook, J.M. Psychological resilience in older U.S. veterans: Results from the National Health and Resilience in Veterans Study. Depress Anxiety 2013, 30, 432–443. [Google Scholar] [CrossRef]
- Critchley, H.D.; Garfinkel, S.N. Interoception and emotion. Curr. Opin. Psychol. 2017, 17, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Khalsa, S.S.; Adolphs, R.; Cameron, O.G.; Critchley, H.D.; Davenport, P.W.; Feinstein, J.S.; Feusner, J.D.; Garfinkel, S.N.; Lane, R.D.; Mehling, W.E.; et al. Interoception and mental health: A roadmap. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2018, 3, 501–513. [Google Scholar] [CrossRef] [PubMed]
- Grabbe, L.; Higgins, M.; Jordan, D.; Noxsel, L.; Gibson, B.; Murphy, J. The Community Resiliency Model®: A Pilot of an Interoception Intervention to Increase the Emotional Self-Regulation of Women in Addiction Treatment. Int. J. Behav. Health Addict. 2020, 19, 793–808. [Google Scholar] [CrossRef]
- Grabbe, L.; Miller-Karas, E. The trauma resiliency model: A “bottom-up” intervention for trauma psychotherapy. J. Am. Psychiatr. Nurses Assoc. 2018, 24, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Aréchiga, A.; Freeman, K.; Tan, A.; Lou, J.; Lister, Z.; Buckles, B.; Montgomery, S. Building resilience and improving wellbeing in Sierra Leone using the community resiliency model post Ebola. Int. J. Ment. Health 2023, 53, 111–123. [Google Scholar] [CrossRef]
- Habimana, S.; Biracyaza, E.; Habumugisha, E.; Museka, E.; Mutabaruka, J.; Montgomery, S.B. Role of community resiliency model skills trainings in trauma healing among 1994 Tutsi genocide survivors in Rwanda. Psychol. Res. Behav. Manag. 2021, 14, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Benasi, G.; Fava, G.A.; Rafanelli, C. Kellner’s symptom questionnaire, a highly sensitive patient-reported outcome measure: Systematic review of clinimetric properties. Psychother. Psychosom. 2020, 89, 74–89. [Google Scholar] [CrossRef] [PubMed]
- Kellner, R. A symptom questionnaire. J. Clin. Psychiatry 1987, 48, 268–274. [Google Scholar]
- Marshall, A.D.; Panuzio, J.; Taft, C.T. Intimate partner violence among military veterans and active duty servicemen. Clin. Psychol. Rev. 2005, 25, 862–876. [Google Scholar] [CrossRef]
- Orth, U.; Wieland, E. Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: A meta-analysis. J. Consult. Clin. Psychol. 2006, 74, 698. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic Characteristics (N = 46) | n (%) |
|---|---|
| Age (28–74) | Mean = 62.75 (SD = 20.54) years |
| Gender 1 | |
| Female | 21 (58%) |
| Male | 15 (42%) |
| Ethnicity | |
| African-American | 6 (17%) |
| Asian | 1 (3%) |
| Caucasian | 21 (58%) |
| Latino | 10 (28%) |
| Native American | 8 (22%) |
| Years Lived in Community (1–60 years) | Mean = 20.52 (SD = 17.10) years |
| Used Mental Health Services 2 | |
| No | 8 (30%) |
| Yes | 19 (70%) |
| Skills (1–5) | Satisfaction | Preparedness | ||
|---|---|---|---|---|
| m (sd) | t | m (sd) | t | |
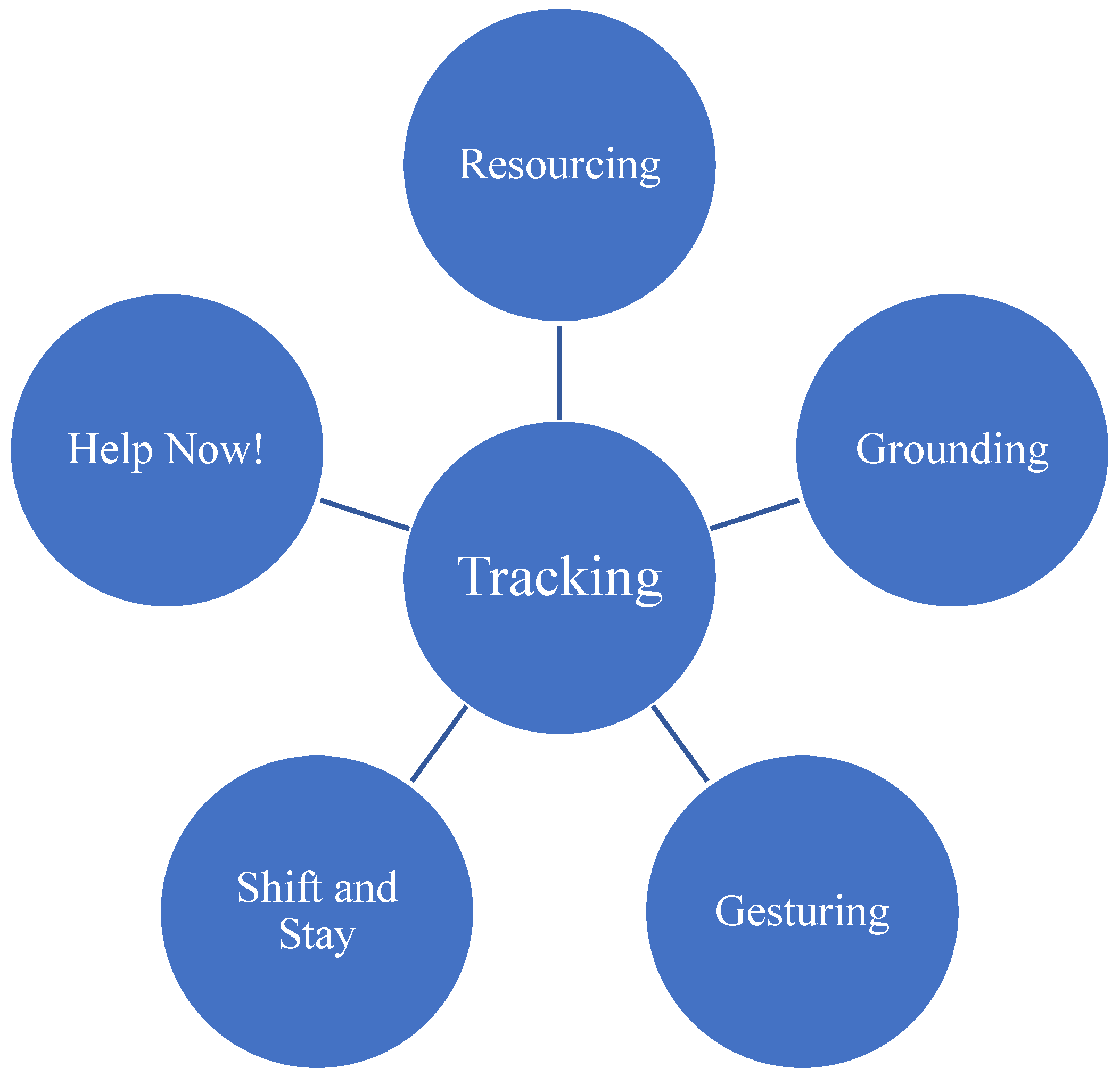
| Tracking | ||||
| Post | 4.65 (0.59) | 1.98 | 4.35 (0.73) | 0.48 |
| Follow-up | 4.32 (0.72) | 4.25 (0.89) | ||
| Resourcing | ||||
| Post | 4.71 (0.52) | 1.06 | 4.38 (0.74) | 0.16 |
| Follow-up | 4.56 (0.58) | 4.35 (0.73) | ||
| Resource Intensification | ||||
| Post | 4.62 (0.55) | 1.95 | 4.27 (0.80) | 0.28 |
| Follow-up | 4.25 (0.84) | 4.21 (0.88) | ||
| Grounding | ||||
| Post | 4.47 (0.66) | 1.6 | 4.24 (0.75) | 0.48 |
| Follow-up | 4.18 (0.77) | 4.14 (0.89) | ||
| Shift and Stay | ||||
| Post | 4.50 (0.57) | 0.85 | 4.21 (0.78) | 0.15 |
| Follow-up | 4.36 (0.73) | 4.18 (0.82) | ||
| Distress Indicators | n | Mean Scores | Changes in Mean Scores | |||
|---|---|---|---|---|---|---|
| Pre | Post | F/U | Pre-Post Change | Pre-F/U Change | ||
| Anxiety | 25 | 5.78 | 2.52 | 3.22 | 3.96 *** | 2.20 * |
| Depression | 25 | 4.81 | 1.34 | 1.89 | 4.43 *** | 2.49 * |
| Somatic | 30 | 4.60 | 3.44 | 2.71 | 1.18 * | 2.17 * |
| Hostility | 25 | 5.26 | 1.61 | 2.84 | 3.62 *** | 2.63 ** |
| Well-Being Indicators | ||||||
| Relaxed | 31 | 4.81 | 5.73 | 5.84 | −2.99 ** | −1.82 |
| Contentment | 29 | 5.17 | 5.53 | 5.81 | −1.54 | −1.67 |
| Somatic | 18 | 3.04 | 3.17 | 3.33 | −0.41 | −2.31 * |
| Friendly | 31 | 5.62 | 5.97 | 5.80 | −2.17 * | −1.17 |
| n | Mean Scores | Changes in Mean Scores | ||||
|---|---|---|---|---|---|---|
| Total Score (0–39) | Pre | Post | F/U | Pre-Post Change | Pre-F/U Change | |
| Daily Functioning | 27 | 11.73 | 8.31 | 10.23 | 3.18 ** | 0.78 |
| Individual Experiences (0–3) | ||||||
| Stressors | 33 | 1.28 | 1.03 | 1.40 | 1.76 * | −0.40 |
| Public Interaction | 33 | 0.84 | 0.75 | 0.84 | 0.57 | 0.42 |
| Angry | 33 | 0.75 | 0.41 | 0.68 | 2.98 ** | 0.90 |
| Better Way | 32 | 0.74 | 0.48 | 0.50 | 1.44 | 0.16 |
| Judgement | 32 | 0.84 | 0.58 | 0.58 | 2.11 * | 1.45 |
| Amped | 30 | 1.13 | 0.48 | 0.50 | 3.93 *** | 3.42 ** |
| Aggressive | 32 | 0.66 | 0.56 | 0.64 | 0.77 | 0.68 |
| Self-Medicate | 29 | I0.82 | 0.50 | 0.65 | 2.54 * | 0.59 |
| Energy | 30 | 1.21 | 0.93 | 0.88 | 1.35 | 1.37 |
| Road Rage | 29 | 0.75 | 0.89 | 0.79 | −0.66 | −0.31 |
| Sleep | 29 | 1.25 | 1.07 | 1.36 | 1.04 | −1.66 |
| Emotions | 29 | 0.86 | 0.46 | 0.88 | 3.03 ** | −0.36 |
| Confidence | 29 | 0.79 | 0.57 | 0.58 | 1.24 | 0.49 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baek, K.; Freeman, K.R.; Truong, S.; Bell, C.; Montgomery, S.B. Pilot Study of a Resiliency Based and Trauma Informed Intervention for Veterans. Trauma Care 2024, 4, 75-86. https://doi.org/10.3390/traumacare4010007
Baek K, Freeman KR, Truong S, Bell C, Montgomery SB. Pilot Study of a Resiliency Based and Trauma Informed Intervention for Veterans. Trauma Care. 2024; 4(1):75-86. https://doi.org/10.3390/traumacare4010007
Chicago/Turabian StyleBaek, Kelly, Kimberly R. Freeman, Sophia Truong, Christi Bell, and Susanne B. Montgomery. 2024. "Pilot Study of a Resiliency Based and Trauma Informed Intervention for Veterans" Trauma Care 4, no. 1: 75-86. https://doi.org/10.3390/traumacare4010007
APA StyleBaek, K., Freeman, K. R., Truong, S., Bell, C., & Montgomery, S. B. (2024). Pilot Study of a Resiliency Based and Trauma Informed Intervention for Veterans. Trauma Care, 4(1), 75-86. https://doi.org/10.3390/traumacare4010007






