Current Concepts in Pediatric Pelvic Ring Fractures: A Narrative Review
Abstract
:1. Introduction
2. Epidemiology
3. Mechanism of Injury
4. Anatomical Considerations
5. Associated Injury
6. Diagnosis
6.1. Clinical Examinations
6.2. Imaging
6.2.1. Plain Radiographs
6.2.2. Computed Tomography (CT)
6.2.3. Magnetic Resonance Imaging (MRI)
7. Classification
- -
- Simple pelvic trauma (90%): pelvic fracture associated with instability of osteo-ligamentous structures and mild soft tissue injuries;
- -
- Complex pelvic trauma: pelvic fracture related to severe soft tissue injuries;
- -
- Unstable pelvic fracture associated with hemodynamic instability
- -
- Traumatic hemipelvectomy: partial or complete dislocation of hemipelvis with disruption of pelvic neurovascular structures [11].
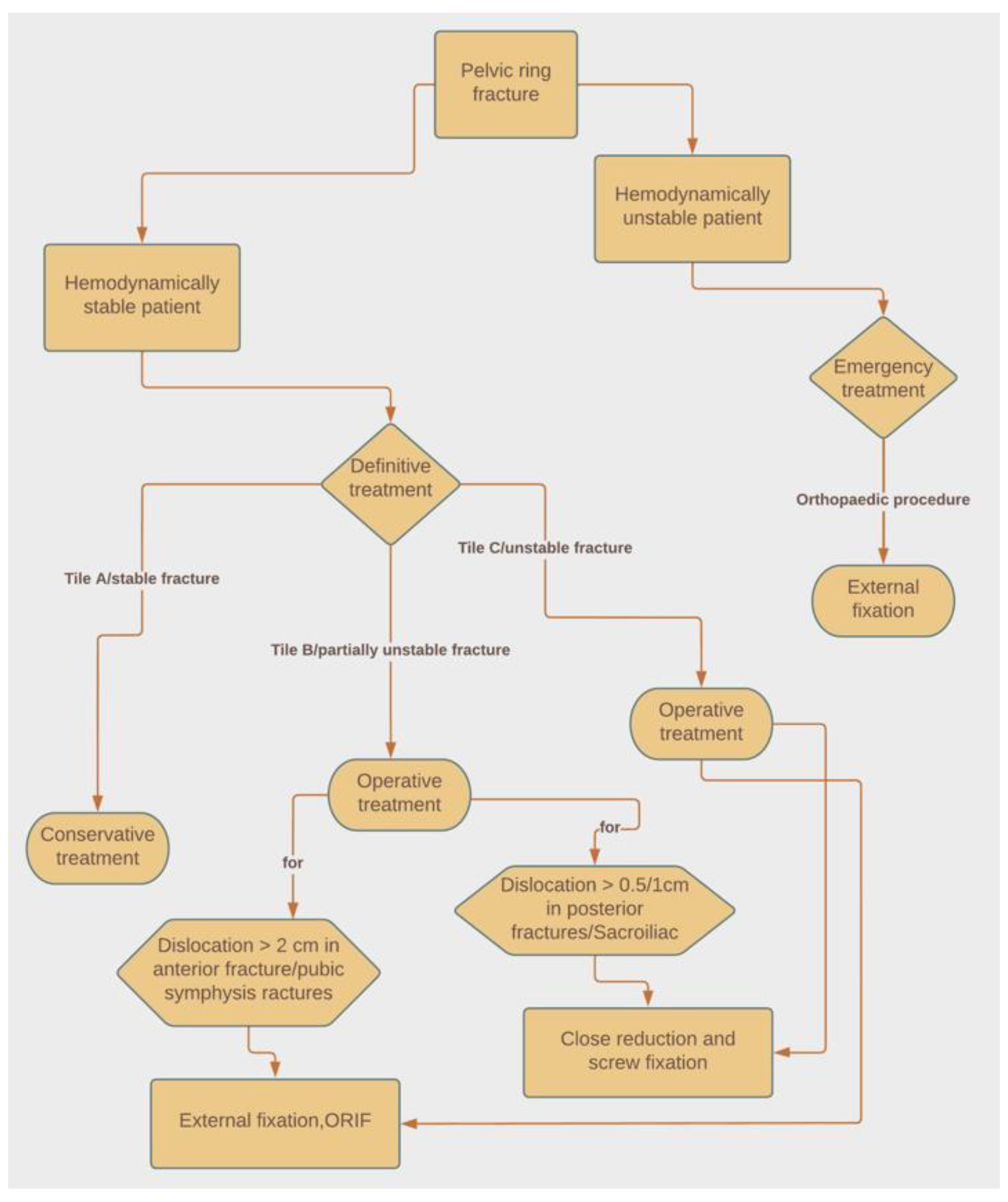
8. Treatment
8.1. Emergency Treatment
8.2. Definitive Treatment
8.2.1. Stable Fractures
8.2.2. Partial Unstable Fractures
8.2.3. Unstable Pelvic Fractures
9. Outcomes
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WISQARS (Web-based Injury Statistics Query and Reporting System)|Injury Center|CDC. Available online: https://www.cdc.gov/injury/wisqars/index.html (accessed on 14 April 2022).
- Haller, J.A. Pediatric trauma. The No. 1 killer of children. JAMA 1983, 249, 47. [Google Scholar] [CrossRef] [PubMed]
- Snyder, C.L.; Jain, V.N.; Saltzman, D.A.; Strate, R.G.; Perry, J.F.; Leonard, A.S. Blunt trauma in adults and children: A comparative analysis. J. Trauma 1990, 30, 1239–1245. [Google Scholar] [CrossRef] [PubMed]
- Keshishyan, R.A.; Rozinov, V.M.; Malakhov, O.A.; Kuznetsov, L.E.; Strunin, E.G.; Chogovadze, G.A.; Tsukanov, V.E. Pelvic polyfractures in children. Radiographic diagnosis and treatment. Clin. Orthop. Relat. Res. 1995, 28–33. Available online: https://pubmed.ncbi.nlm.nih.gov/7586836/ (accessed on 14 April 2022).
- Kruppa, C.G.; Khoriaty, J.D.; Sietsema, D.L.; Dudda, M.; Schildhauer, T.A.; Jones, C.B. Pediatric pelvic ring injuries: How benign are they? Injury 2016, 47, 2228–2234. [Google Scholar] [CrossRef] [PubMed]
- Shaath, M.K.; Koury, K.L.; Gibson, P.D.; Adams, M.R.; Sirkin, M.S.; Reilly, M.C. Associated Injuries in Skeletally Immature Children with Pelvic Fractures. J. Emerg. Med. 2016, 51, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Zwingmann, J.; Lefering, R.; Maier, D.; Hohloch, L.; Eberbach, H.; Neumann, M.; Strohm, P.C.; Südkamp, N.P.; Hammer, T. Pelvic fractures in severely injured children: Results from the TraumaRegister DGU. Medicine 2018, 97, e11955. [Google Scholar] [CrossRef]
- Salášek, M.; Havránek, P.; Havlas, V.; Pavelka, T.; Pešl, T.; Stančák, A.; Hendrych, J.; Džupa, V. Paediatric pelvic injuries: A retrospective epidemiological study from four level 1 trauma centers. Int. Orthop. 2021, 45, 2033–2048. [Google Scholar] [CrossRef]
- DeFrancesco, C.J.; Sankar, W.N. Traumatic pelvic fractures in children and adolescents. Semin. Pediatr. Surg. 2017, 26, 27–35. [Google Scholar] [CrossRef]
- Guillaume, J.M.; Pesenti, S.; Jouve, J.L.; Launay, F. Pelvic fractures in children (pelvic ring and acetabulum). Orthop. Traumatol. Surg. Res. 2020, 106, S125–S133. [Google Scholar] [CrossRef]
- Gänsslen, A.; Heidari, N.; Weinberg, A.M. Fractures of the pelvis in children: A review of the literature. Eur. J. Orthop. Surg. Traumatol. 2013, 23, 847–861. [Google Scholar] [CrossRef]
- Yeager, K.C.; Silva, S.R.; Richter, D.L. Pelvic Avulsion Injuries in the Adolescent Athlete. Clin. Sports Med. 2021, 40, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Ding, S.; Zhu, Z.-H.; Yang, Y.-C.; Wei, Z.-Q.; Zhu, C.; Liu, Y.-L.; Li, Y. Clinical analysis of 60 children with pelvic fracture and associated injuries: An observational study. Ann. Ital. Chir. 2022, 92, 102–107. [Google Scholar] [PubMed]
- Alhammoud, A.; Moghamis, I.; Abdelrahman, H.; Ghouri, S.I.; Asim, M.; Babikir, E.; Al-Thani, H.; El-Menyar, A. Clinical characteristics, injury pattern and management of pediatric pelvic fracture: An observational retrospective study from a level I trauma center. BMC Musculoskelet. Disord. 2021, 22, 626. [Google Scholar] [CrossRef] [PubMed]
- Currey, J.; Butler, G. The mechanical properties of bone tissue in children. J. Bone Jt. Surg. Am. 1975, 57, 810–814. [Google Scholar] [CrossRef]
- Stuhler, T.; Stanković, P.; Krause, P.; Koch, A. Pelvic fractures in children: Clinic, late results, biomechanic (author’s transl). Arch. Orthop. Unfallchir. 1977, 90, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Ogden, J.A. Skeletal Injury in the Child; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2000. [Google Scholar] [CrossRef] [Green Version]
- Dale Blasier, R.; McAtee, J.; White, R.; Mitchell, D.T. Disruption of the pelvic ring in pediatric patients. Clin. Orthop. Relat. Res. 2000, 376, 87–95. [Google Scholar] [CrossRef]
- Chia, J.P.Y.; Holland, A.J.A.; Little, D.; Cass, D.T. Pelvic fractures and associated injuries in children. J. Trauma Acute Care Surg. 2004, 56, 83–88. [Google Scholar] [CrossRef]
- Grisoni, N.; Connor, S.; Marsh, E.; Thompson, G.H.; Cooperman, D.R.; Blakemore, L.C. Pelvic fractures in a pediatric level I trauma center. J. Orthop. Trauma 2002, 16, 458–463. [Google Scholar] [CrossRef]
- Junkins, E.P.; Furnival, R.A.; Bolte, R.G. The clinical presentation of pediatric pelvic fractures. Pediatr. Emerg. Care 2001, 17, 15–18. [Google Scholar] [CrossRef]
- Silber, J.S.; Flynn, J.M.; Koffler, K.M.; Dormans, J.P.; Drummond, D.S. Analysis of the cause, classification, and associated injuries of 166 consecutive pediatric pelvic fractures. J. Pediatr. Orthop. 2001, 21, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Spiguel, L.; Glynn, L.; Liu, D.; Statter, M. Pediatric pelvic fractures: A marker for injury severity. Am. Surg. 2006, 72, 481–484. [Google Scholar] [CrossRef] [PubMed]
- Hauschild, O.; Strohm, P.C.; Culemann, U.; Pohlemann, T.; Suedkamp, N.P.; Koestler, W.; Schmal, H. Mortality in patients with pelvic fractures: Results from the German pelvic injury register. J. Trauma Acute Care Surg. 2008, 64, 449–455. [Google Scholar] [CrossRef]
- Banerjee, S.; Barry, M.J.; Paterson, J.M.H. Paediatric pelvic fractures: 10 years experience in a trauma centre. Injury 2009, 40, 410–413. [Google Scholar] [CrossRef]
- Galano, G.J.; Vitale, M.A.; Kessler, M.W.; Hyman, J.E.; Vitale, M.G. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J. Pediatr. Orthop. 2005, 25, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.; Shurnas, P.; Morgan, S.; Agudelo, J.; Luszko, G.; Knox, E.C.; Georgopoulos, G. Clinical outcomes of unstable pelvic fractures in skeletally immature patients. J. Bone Jt. Surg. Am. 2005, 87, 2423–2431. [Google Scholar] [CrossRef]
- Galos, D.; Doering, T.A. High-Energy Fractures of the Pelvis and Acetabulum in Pediatric Patients. J. Am. Acad. Orthop. Surg. 2020, 28, 353–362. [Google Scholar] [CrossRef]
- Kenawey, M.; Krettek, C.; Addosooki, A.; Salama, W.; Liodakis, E. Unstable paediatric pelvic injuries: The patho-anatomical patterns of pelvic ring failure and the role of avulsion of the iliac apophysis. Bone Jt. J. 2015, 97, 696–704. [Google Scholar] [CrossRef]
- Hermans, E.; Cornelisse, S.T.; Biert, J.; Tan, E.C.T.H.; Edwards, M.J.R. Paediatric pelvic fractures: How do they differ from adults? J. Child Orthop. 2017, 11, 49. [Google Scholar] [CrossRef]
- Nasef, H.; Elhessy, A.; Abushaban, F.; Alhammoud, A. Pelvic fracture instability-associated L5 transverse process fracture, fact or myth? A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 885–891. [Google Scholar] [CrossRef]
- Zwingmann, J.; Aghayev, E.; Südkamp, N.P.; Neumann, M.; Bode, G.; Stuby, F.; Schmal, H. Pelvic Fractures in Children Results from the German Pelvic Trauma Registry: A Cohort Study. Medicine 2015, 94, e2325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tosounidis, T.H.; Sheikh, H.; Giannoudis, P.V. Pelvic Fractures in Paediatric Polytrauma Patients: Classification, Concomitant Injuries and Early Mortality. Open Orthop. J. 2015, 9, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Chotai, N.; Alazzawi, S.; Zehra, S.S.; Barry, M. Paediatric pelvic fractures: A review of 2 cohorts over 22 years. Injury 2018, 49, 613–617. [Google Scholar] [CrossRef] [PubMed]
- De La Calva, C.; Jover, N.; Alonso, J.; Salom, M. Pediatric Pelvic Fractures and Differences Compared with the Adult Population. Pediatr. Emerg. Care 2020, 36, 519–522. [Google Scholar] [CrossRef]
- Ismail, N.; Bellemare, J.F.; Mollitt, D.L.; DiScala, C.; Koeppel, B.; Tepas, J.J. Death from pelvic fracture: Children are different. J. Pediatr. Surg. 1996, 31, 82–85. [Google Scholar] [CrossRef]
- Cothren, C.C.; Osborn, P.M.; Moore, E.E.; Morgan, S.J.; Johnson, J.L.; Smith, W.R. Preperitonal pelvic packing for hemodynamically unstable pelvic fractures: A paradigm shift. J. Trauma Acute Care Surg. 2007, 62, 834–839. [Google Scholar] [CrossRef]
- Gänsslen, A.; Hildebrand, F.; Heidari, N.; Weinberg, A.M. Pelvic ring injuries in children. Part I: Epidemiology and primary evaluation. A review of the literature. Acta Chir. Orthop. Traumatol. Cechoslov. 2012, 79, 493–498. [Google Scholar]
- Mosheiff, R.; Suchar, A.; Porat, S.; Shmushkevich, A.; Segal, D.; Liebergall, M. The “crushed open pelvis” in children. Injury 1999, 30 (Suppl. 2), B14–B18. [Google Scholar] [CrossRef]
- Mulder, M.B.; Maggart, M.J.; Yang, W.J.; Perez, E.A.; Namias, N.; Sola, J.E.; Proctor, K.G.; Thorson, C.M. Outcomes of Pediatric Pelvic Fractures: A Level I Trauma Center’s 20-Year Experience. J. Surg. Res. 2019, 243, 515–523. [Google Scholar] [CrossRef]
- Shlamovitz, G.Z.; Mower, W.R.; Bergman, J.; Crisp, J.; DeVore, H.K.; Hardy, D.; Sargent, M.; Shroff, S.D.; Snyder, E.; Morgan, M.T. Poor test characteristics for the digital rectal examination in trauma patients. Ann. Emerg. Med. 2007, 50, 25–33e1. [Google Scholar] [CrossRef] [PubMed]
- Shore, B.J.; Palmer, C.S.; Bevin, C.; Johnson, M.B.; Torode, I.P. Pediatric pelvic fracture: A modification of a preexisting classification. J. Pediatr. Orthop. 2012, 32, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, D.W.E.; Schuette, J.J.; Knight, V.; Johnson, E.; Denise, J.; Walker, A.R. Necessity of routine pelvic radiograph in the pediatric blunt trauma patient. Clin. Pediatr. 2008, 47, 935–940. [Google Scholar] [CrossRef]
- Gonzalez, R.P.; Fried, P.Q.; Bukhalo, M. The utility of clinical examination in screening for pelvic fractures in blunt trauma. J. Am. Coll. Surg. 2002, 194, 121–125. [Google Scholar] [CrossRef]
- Kwok, M.Y.; Yen, K.; Atabaki, S.; Adelgais, K.; Garcia, M.; Quayle, K.; Kooistra, J.; Bonsu, B.K.; Page, K.; Borgialli, D. Sensitivity of plain pelvis radiography in children with blunt torso trauma. Ann. Emerg. Med. 2015, 65, 63–71e1. [Google Scholar] [CrossRef] [PubMed]
- Guillamondegui, O.D.; Mahboubi, S.; Stafford, P.W.; Nance, M.L. The utility of the pelvic radiograph in the assessment of pediatric pelvic fractures. J. Trauma Acute Care Surg. 2003, 55, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Kevill, K.; Wong, A.M.; Goldman, H.S.; Gershel, J.C. Is a complete trauma series indicated for all pediatric trauma victims? Pediatr. Emerg. Care 2002, 18, 75–77. [Google Scholar] [CrossRef]
- Quick, T.J.; Eastwood, D.M. Pediatric fractures and dislocations of the hip and pelvis. Clin. Orthop. Relat. Res. 2005, 432, 87–96. [Google Scholar] [CrossRef]
- Fayad, L.M.; Corl, F.; Fishman, E.K. Pediatric skeletal trauma: Use of multiplanar reformatted and three-dimensional 64-row multidetector CT in the emergency department. Radiographics 2009, 29, 135–150. [Google Scholar] [CrossRef] [Green Version]
- Kenawey, M. MRI Evaluation of the Posterior Pelvic Bony and Soft Tissue Injuries With Tile C Displaced Pelvic Fractures in Young Children. J. Pediatr. Orthop. 2020, 40, e579–e586. [Google Scholar] [CrossRef]
- Key, J.A.; Conwell, H.E. Management of Fractures, Dislocations and Sprains; The C. V. Mosby Company: St. Louis, MO, USA, 1951. [Google Scholar]
- Torode, I.; Zieg, D. Pelvic fractures in children. J. Pediatr. Orthop. 1985, 5, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Marsh, J.; Slongo, T.F.; Agel, J.; Broderick, J.S.; Creevey, W.; DeCoster, T.A.; Prokuski, L.; Sirkin, M.S.; Ziran, B.; Henley, B. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J. Orthop. Trauma 2007, 21 (Suppl. 10), S1–S133. [Google Scholar] [CrossRef] [PubMed]
- Pohlemann, T. Pelvic ring injuries: Assessment and concepts of surgical management. In AO Principles of Fracture Management; Rüedi, T.P., Murphy, W.M., Eds.; Thieme-Verlag: Stuttgart, Germany, 2000; pp. 391–414. [Google Scholar]
- Tscherne, H.; Pohlemann, T.; Gansslen, A. Classification, staging, urgency and indications in pelvic injuries. Zentralbl. Chir. 2000, 125, 717–724. [Google Scholar] [CrossRef] [PubMed]
- De Billy, B.; Chrestian, P.; Garnier, E. Polytraumatisme de L’enfant; Published online; 2000. [Google Scholar]
- Sathya, C.; Alali, A.S.; Wales, P.W.; Scales, D.C.; Karanicolas, P.J.; Burd, R.S.; Nance, M.L.; Xiong, W.; Nathens, A.B. Mortality among Injured Children Treated at Different Trauma Center Types. JAMA Surg. 2015, 150, 874–881. [Google Scholar] [CrossRef] [PubMed]
- Qasim, Z.; Masood, R.; Mateen, M. Successful use of angiographic embolization to control hemorrhage from blunt pelvic trauma in a pediatric patient. J. Pak. Med. Assoc. 2004, 54, 32–33. [Google Scholar]
- Bond, S.J.; Gotschall, C.S.; Eichelberger, M.R. Predictors of abdominal injury in children with pelvic fracture. J. Trauma 1991, 31, 1169–1173. [Google Scholar] [CrossRef]
- Demetriades, D.; Karaiskakis, M.; Velmahos, G.C.; Alo, K.; Murray, J.; Chan, L. Pelvic fractures in pediatric and adult trauma patients: Are they different injuries? J. Trauma Acute Care Surg. 2003, 54, 1146–1151. [Google Scholar] [CrossRef]
- Tötterman, A.; Madsen, J.E.; Skaga, N.O.; Røise, O. Extraperitoneal pelvic packing: A salvage procedure to control massive traumatic pelvic hemorrhage. J. Trauma Acute Care Surg. 2007, 62, 843–852. [Google Scholar] [CrossRef] [Green Version]
- Amorosa, L.F.; Kloen, P.; Helfet, D.L. High-energy pediatric pelvic and acetabular fractures. Orthop. Clin. N. Am. 2014, 45, 483–500. [Google Scholar] [CrossRef]
- Schwarz, N.; Posch, E.; Mayr, J.; Fischmeister, F.M.; Schwarz, A.F.; Öhner, T. Long-term results of unstable pelvic ring fractures in children. Injury 1998, 29, 431–433. [Google Scholar] [CrossRef]
- Gordon, R.G.; Karpik, K.; Hardy, S.; Mears, D.C. Techniques of operative reductionand fixation of pediatric and adolescent pelvic fractures. Oper. Tech. Orthop. 1995, 2, 95–114. [Google Scholar] [CrossRef]
- Lindahl, J.; Hirvensalo, E.; Böstman, O.; Santavirta, S. Failure of reduction with an external fixator in the management of injuries of the pelvic ring. Long-term evaluation of 110 patients. J. Bone Jt. Surg. Br. 1999, 81, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Sridharan, S.S.; You, D.; Ponich, B.; Parsons, D.; Schneider, P. Outcomes following pelvic ring fractures in the paediatric population: A systematic review. J. Clin. Orthop. Trauma 2020, 11, 963–969. [Google Scholar] [CrossRef]
- McIntyre, R.C., Jr.; Bensard, D.D.; Moore, E.E.; Chambers, J.; Moore, F.A. Pelvic fracture geometry predicts risk of life-threatening hemorrhage in children. J. Trauma 1993, 35, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, C.A. Rockwood and Wilkin’s Fractures in Children; Lippincott Williams & Wilkins: New York, NY, USA, 2019. [Google Scholar]
- Wharton, R.M.H.; Trowbridge, S.; Simpson, A.; Sarraf, K.M.; Jabbar, Y. Anatomic, diagnostic and management challenges in paediatric pelvic injuries: A review. J. Pediatr. Orthop. Part B 2019, 28, 476–486. [Google Scholar] [CrossRef] [PubMed]





| Study and Year | Age N | Head % | Chest % | Abdomen % | Pelvic Hematoma % | Limb Fractures % | Urogenital % |
|---|---|---|---|---|---|---|---|
| Sheng Ding 2022 | 2–15 60 | 30 | NR | NR | 13.3 | 23.3 | 23 |
| Alhammoud 2021 | 0–18 109 | 24 | 46 | 34.5 | 5.9 | 17.6 Lower Limb | NR |
| Mulder 2019 | 0–17 163 | 25 | 48 | 75 | 5 | 60 | 11 |
| De La Cava 2018 | 1–14 81 | 49.4 | NR | 24.7 | NR | 55 | 11.1 |
| Herrans 2017 | 3–16 51 | 43 | 24 | 37 | 4 | 76 | 12 |
| Shaat 2016 | 2–14 60 | 60 | 40 | 26.7 | 3.3 | 100 | NR |
| Tosounidis 2015 | 0–17 49 | 67.3 | 61 * | 38.7 ** | NR | 34 | 6.1 |
| MTZ type | Frequency | Description |
|---|---|---|
| Type I | 3% | Avulsion fractures |
| Type II | 15% | Iliac wing fractures caused by lateral forces (II-A: apophyseal; II-B: bony) |
| Type III | 55% | Simple pelvic ring fractures, stable:
|
| Type IV | 28% | Multifocal fractures with pelvic ring disruptions, unstable (e.g., unstable pelvic segment, straddle fractures, associated acetabular fractures, anterior and posterior ring fractures). |
| Type | Frequency | Description |
|---|---|---|
| Type I | 38–56% | Isolated fracture not involving the pelvic ring (e.g., avulsion, iliac wing, pubis/ischium rami, sacrum, or coccyx fracture)fractures |
| Type II | 28–43% | Single break in the pelvic ring (e.g., fracture of two ipsilateral pubic rami, symphysis pubis disruption, SI joint disruption) |
| Type III | 11–12% | Double break in the pelvic ring (e.g., anterior-posterior or straddle fracture) |
| Type IV | 5–9% | Acetabular fracture |
| Type | Subtype | Description |
|---|---|---|
| APC | Anterior-posterior compression (APC), result of frontal impact forces | |
| APC-I | Mild symphyseal (<2.5 cm), intact SI joint; external rotation displacement of hemipelvis, stable pattern. | |
| APC-II | Severe symphyseal diastasis (>2.5 cm) with anterior SI joint disruption; external rotation displacement of hemipelvis, rotationally unstable and vertically stable. | |
| APC-III | Type II with posterior SI joint disruption; external rotation displacement of hemipelvis, rotationally and vertically unstable. | |
| LC | Lateral compression (LC), result of side-on collision (e.g., run over pedestrian) | |
| LC-I | Ipsilateral sacral compression or ipsilateral horizontal pubic rami fractures; internal rotation displacement of hemipelvis, stable pattern. | |
| LC-II | Ipsilateral iliac wing fracture or posterior SI joint disruption; internal rotation displacement of hemipelvis, rotationally unstable and vertically stable. | |
| LC-III | Type I with contralateral APC (“wind-swept pelvis”); mixed displacement of hemipelvis, rotationally and vertically unstable. | |
| VS | Vertical shear (VS), result of inferior-superior forces (e.g., fall from height), characterized by vertical pubic rami fractures and SI joint disruption; cranial displacement of hemipelvis, rotationally and vertically unstable. |
| Type | Group | Subgroup | |||
|---|---|---|---|---|---|
| Type A | Stable, no displacement of the posterior arch. | A1 | Avulsion fractures | A1.1 | ASIS |
| A1.2 | AIIS | ||||
| A1.3 | Ischial tuberosity | ||||
| A2 | Complete fracture without displacement of the pelvic ring, with | A2.1 | Iliac wing fracture | ||
| A2.2 | Unilateral fracture of the anterior arch | ||||
| A2.3 | Bilateral fracture of the anterior arch | ||||
| A3 | Transverse fracture of sacrum and coccyx | ||||
| Type B | Partial unstable, with incomplete posterior arch disruption | B1 | Anterior arch injuries without rotational instability | B1.1 | Lateral compression (LC) |
| B1.2 | Anterior-posterior compression (APC, “open book”) | ||||
| B2 | Rotationally unstable, with unilateral posterior injury | B2.1 | LC fracture of the sacrum with internal rotation instability. | ||
| B2.2 | LC fracture of the ilium (“crescent”) with internal rotation instability. | ||||
| B2.3 | Open book or external rotation instability. | ||||
| B3 | Rotationally unstable, with bilateral posterior injury | B3.1 | Internal rotationally unstable/ER rotationally unstable contralateral. | ||
| B3.2 | Bilateral LC sacral fracture. | ||||
| B3.3 | Open book or external rotation instability. | ||||
| Type C | Global unstable, with complete posterior arch disruption | C1 | Unilateral posterior injury (vertical shear), with | C1.1 | Iliac fracture |
| C1.2 | SI joint disruption | ||||
| C1.3 | Sacral fracture | ||||
| C2 | Bilateral posterior injury, with one hemipelvis injury complete disruption and contralateral hemipelvis injury incomplete disruption through | C2.1 | Ilium | ||
| C2.2 | SI joint | ||||
| C2.3 | Sacrum | ||||
| C3 | Bilateral posterior injury, with complete bilateral disruption (vertical shear). | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aprato, A.; Giudice, C.; Bedino, P.; Audisio, A.; Massè, A. Current Concepts in Pediatric Pelvic Ring Fractures: A Narrative Review. Trauma Care 2022, 2, 359-372. https://doi.org/10.3390/traumacare2020029
Aprato A, Giudice C, Bedino P, Audisio A, Massè A. Current Concepts in Pediatric Pelvic Ring Fractures: A Narrative Review. Trauma Care. 2022; 2(2):359-372. https://doi.org/10.3390/traumacare2020029
Chicago/Turabian StyleAprato, Alessandro, Carmelo Giudice, Paolo Bedino, Andrea Audisio, and Alessandro Massè. 2022. "Current Concepts in Pediatric Pelvic Ring Fractures: A Narrative Review" Trauma Care 2, no. 2: 359-372. https://doi.org/10.3390/traumacare2020029
APA StyleAprato, A., Giudice, C., Bedino, P., Audisio, A., & Massè, A. (2022). Current Concepts in Pediatric Pelvic Ring Fractures: A Narrative Review. Trauma Care, 2(2), 359-372. https://doi.org/10.3390/traumacare2020029






