Low-Intensity Pulsed Ultrasound in the Treatment of Nonunions and Fresh Fractures: A Case Series
Abstract
:1. Introduction
2. Materials and Methods
2.1. LIPUS Treatment Protocol
2.2. Data Collection and Clinical Assessment
2.3. Statistical Methods
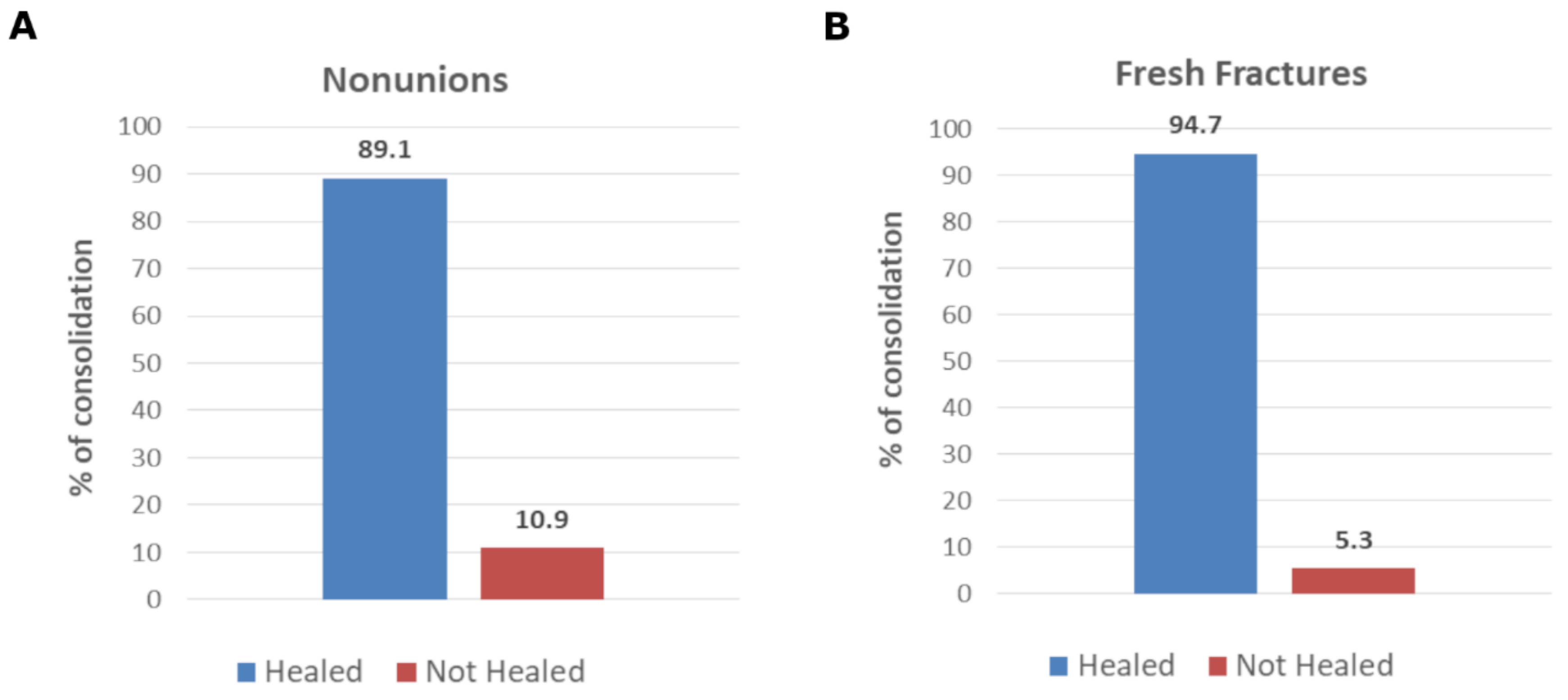
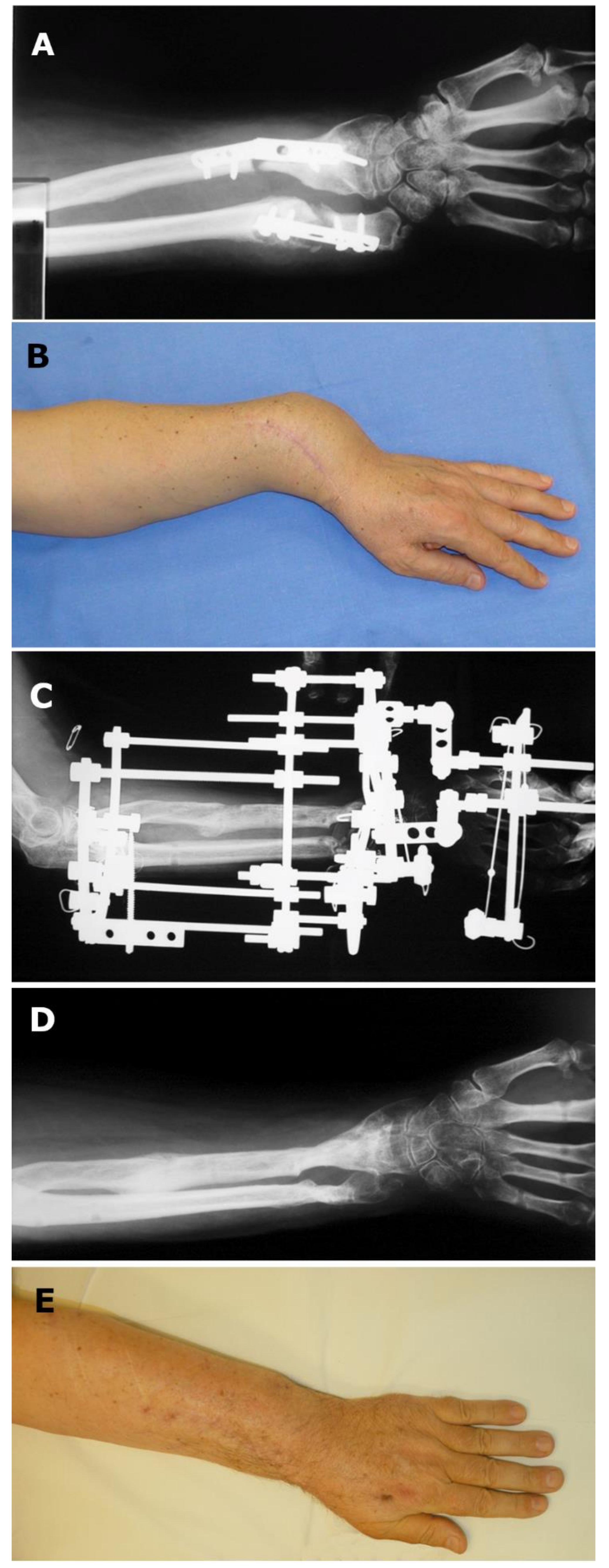
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zura, R.; Xiong, Z.; Einhorn, T.; Watson, J.T.; Ostrum, R.F.; Prayson, M.J.; Della Rocca, G.J.; Mehta, S.; McKinley, T.; Wang, Z.; et al. Epidemiology of Fracture Nonunion in 18 Human Bones. JAMA Surg. 2016, 151, e162775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekegren, C.; Edwards, E.; de Steiger, R.; Gabbe, B. Incidence, Costs and Predictors of Non-Union, Delayed Union and Mal-Union Following Long Bone Fracture. Int. J. Environ. Res. Public. Health 2018, 15, 2845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, C.-C.; Shih, C.-H. Distal Tibial Nonunion Treated by Intramedullary Reaming with External Immobilization. J. Orthop. Trauma 1996, 10, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Marsh, D.R.; Shah, S.; Elliott, J.; Kurdy, N. The Ilizarov method in nonunion, malunion and infection of fractures. J. Bone Joint Surg. Br. 1997, 79-B, 273–279. [Google Scholar] [CrossRef]
- Massari, L.; Benazzo, F.; Falez, F.; Perugia, D.; Pietrogrande, L.; Setti, S.; Osti, R.; Vaienti, E.; Ruosi, C.; Cadossi, R. Biophysical Stimulation of Bone and Cartilage: State of the Art and Future Perspectives. Int. Orthop. 2019, 43, 539–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duarte, L.R. The Stimulation of Bone Growth by Ultrasound. Arch. Orthop. Trauma. Surg. Arch. Orthop. Unf.-Chir. 1983, 101, 153–159. [Google Scholar] [CrossRef]
- Pilla, A.A.; Mont, M.A.; Nasser, P.R.; Khan, S.A.; Figueiredo, M.; Kaufman, J.J.; Siffert, R.S. Non-Invasive Low-Intensity Pulsed Ultrasound Accelerates Bone Healing in the Rabbit. J. Orthop. Trauma 1990, 4, 246–253. [Google Scholar] [CrossRef]
- Rubin, C.; Bolander, M.; Ryaby, J.P.; Hadjiargyrou, M. The Use of Low-Intensity Ultrasound to Accelerate the Healing of Fractures. J. Bone Jt. Surg.-Am. Vol. 2001, 83, 259–270. [Google Scholar] [CrossRef]
- Massari, L.; Cadossi, R. Physical Regulation of Skeletal Repair. In American Academy of Orthopaedic Surgeons: Rosemont, Ill, 1st ed.; American Academy of Orthopaedic Surgeons, Aaron, R.K., Bolander, M.E., Eds.; 2005; ISBN 978-0-89203-363-8. [Google Scholar]
- Koso, R.E.; Terhoeve, C.; Steen, R.G.; Zura, R. Healing, Nonunion, and Re-Operation after Internal Fixation of Diaphyseal and Distal Femoral Fractures: A Systematic Review and Meta-Analysis. Int. Orthop. 2018, 42, 2675–2683. [Google Scholar] [CrossRef]
- Marongiu, G.; Contini, A.; Cozzi Lepri, A.; Donadu, M.; Verona, M.; Capone, A. The Treatment of Acute Diaphyseal Long-Bones Fractures with Orthobiologics and Pharmacological Interventions for Bone Healing Enhancement: A Systematic Review of Clinical Evidence. Bioengineering 2020, 7, 22. [Google Scholar] [CrossRef] [Green Version]
- Ismailidis, P.; Suhm, N.; Clauss, M.; Mündermann, A.; Cadosch, D. Scope and Limits of Teriparatide Use in Delayed and Nonunions: A Case Series. Clin. Pract. 2021, 11, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Corradi, C.; Cozzolino, A. Effect of ultrasonics on the development of osseous callus in fractures. Arch. Ortop. 1953, 66, 77–98. [Google Scholar] [PubMed]
- Corradi, C.; Mattai Del Moro, V. Two years experience of ultrasonic therapy in orthopedics. Arch. Ortop. 1953, 66, 52–76. [Google Scholar]
- Heckman, J.D.; Ryaby, J.P.; McCabe, J.; Frey, J.J.; Kilcoyne, R.F. Acceleration of Tibial Fracture-Healing by Non-Invasive, Low-Intensity Pulsed Ultrasound. J. Bone Joint Surg. Am. 1994, 76, 26–34. [Google Scholar] [CrossRef]
- Leung, K.-S.; Lee, W.-S.; Tsui, H.-F.; Liu, P.P.-L.; Cheung, W.-H. Complex Tibial Fracture Outcomes Following Treatment with Low-Intensity Pulsed Ultrasound. Ultrasound Med. Biol. 2004, 30, 389–395. [Google Scholar] [CrossRef]
- Kristiansen, T.K.; Ryaby, J.P.; McCabe, J.; Frey, J.J.; Roe, L.R. Accelerated Healing of Distal Radial Fractures with the Use of Specific, Low-Intensity Ultrasound. A Multicenter, Prospective, Randomized, Double-Blind, Placebo-Controlled Study. J. Bone Joint Surg. Am. 1997, 79, 961–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schofer, M.D.; Block, J.E.; Aigner, J.; Schmelz, A. Improved Healing Response in Delayed Unions of the Tibia with Low-Intensity Pulsed Ultrasound: Results of a Randomized Sham-Controlled Trial. BMC Musculoskelet. Disord. 2010, 11, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zura, R.; Della Rocca, G.J.; Mehta, S.; Harrison, A.; Brodie, C.; Jones, J.; Steen, R.G. Treatment of Chronic (>1 Year) Fracture Nonunion: Heal Rate in a Cohort of 767 Patients Treated with Low-Intensity Pulsed Ultrasound (LIPUS). Injury 2015, 46, 2036–2041. [Google Scholar] [CrossRef] [Green Version]
- Romano, C.L.; Romano, D.; Logoluso, N. Low-Intensity Pulsed Ultrasound for the Treatment of Bone Delayed Union or Nonunion: A Review. Ultrasound Med. Biol. 2009, 35, 529–536. [Google Scholar] [CrossRef]
- Traina, G.C.; Fontanesi, G.; Costa, P.; Mammi, G.I.; Pisano, F.; Giancecchi, F.; Adravanti, P. Effect of Electromagnetic Stimulation on Patients Suffering from Non-Union. A Retrospective Study with a Control Group. J. Bioelectr. 1991, 10, 101–117. [Google Scholar] [CrossRef]
- Leighton, R.; Watson, J.T.; Giannoudis, P.; Papakostidis, C.; Harrison, A.; Steen, R.G. Healing of Fracture Nonunions Treated with Low-Intensity Pulsed Ultrasound (LIPUS): A Systematic Review and Meta-Analysis. Injury 2017, 48, 1339–1347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watanabe, Y.; Arai, Y.; Takenaka, N.; Kobayashi, M.; Matsushita, T. Three Key Factors Affecting Treatment Results of Low-Intensity Pulsed Ultrasound for Delayed Unions and Nonunions: Instability, Gap Size, and Atrophic Nonunion. J. Orthop. Sci. 2013, 18, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Bhan, K.; Patel, R.; Hasan, K.; Pimplé, M.; Sharma, S.; Nandwana, V.; Basta, M. Fracture Nonunions and Delayed Unions Treated With Low-Intensity Pulsed Ultrasound Therapy: A Clinical Series. Cureus 2021, 13, e17067. [Google Scholar] [CrossRef] [PubMed]
- Nolte, P.; Anderson, R.; Strauss, E.; Wang, Z.; Hu, L.; Xu, Z.; Steen, R.G. Heal Rate of Metatarsal Fractures: A Propensity-Matching Study of Patients Treated with Low-Intensity Pulsed Ultrasound (LIPUS) vs. Surgical and Other Treatments. Injury 2016, 47, 2584–2590. [Google Scholar] [CrossRef] [Green Version]
- Majeed, H.; Karim, T.; Davenport, J.; Karski, M.; Smith, R.; Clough, T.M. Clinical and Patient-Reported Outcomes Following Low Intensity Pulsed Ultrasound (LIPUS, Exogen) for Established Post-Traumatic and Post-Surgical Nonunion in the Foot and Ankle. Foot Ankle Surg. 2020, 26, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Busse, J.W.; Morton, E.; Lacchetti, C.; Guyatt, G.H.; Bhandari, M. Current Management of Tibial Shaft Fractures: A Survey of 450 Canadian Orthopedic Trauma Surgeons. Acta Orthop. 2008, 79, 689–694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hannemann, P.F.W.; Mommers, E.H.H.; Schots, J.P.M.; Brink, P.R.G.; Poeze, M. The Effects of Low-Intensity Pulsed Ultrasound and Pulsed Electromagnetic Fields Bone Growth Stimulation in Acute Fractures: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Arch. Orthop. Trauma Surg. 2014, 134, 1093–1106. [Google Scholar] [CrossRef]
- Lou, S.; Lv, H.; Li, Z.; Zhang, L.; Tang, P. The Effects of Low-Intensity Pulsed Ultrasound on Fresh Fracture: A Meta-Analysis. Medicine 2017, 96, e8181. [Google Scholar] [CrossRef]
| Parameter | N | % |
|---|---|---|
| Sex | ||
| Male | 35 | 76.1 |
| Female | 11 | 23.9 |
| Fracture type | ||
| Closed | 31 | 67.4 |
| Open | 15 | 32.6 |
| Location of fracture | ||
| Femur | 13 | 28.3 |
| Tibia/Fibula | 12 | 26.1 |
| Humerus | 8 | 17.4 |
| Radius/Ulna | 8 | 17.4 |
| Phalanges | 2 | 4.3 |
| Metatarsus | 1 | 2.2 |
| Patella | 1 | 2.2 |
| Scaphoid | 1 | 2.2 |
| Treatment | ||
| Cast | 3 | 6.5 |
| Brace | 5 | 10.9 |
| Fixator | 19 | 41.3 |
| Nail | 9 | 19.6 |
| Plate | 5 | 10.9 |
| Wire | 4 | 8.7 |
| ND | 1 | 2.2 |
| Infection | ||
| Yes | 15 | 32.6 |
| No | 31 | 67.4 |
| Risk factors | ||
| Smoke | 18 | 39.1 |
| Diabetes | 2 | 4.3 |
| Osteoporosis | 1 | 2.2 |
| None | 25 | 54.3 |
| Parameter | N | % |
|---|---|---|
| Sex | ||
| Male | 11 | 57.9 |
| Female | 8 | 42.1 |
| Fracture type | ||
| Closed | 16 | 84.2 |
| Open | 3 | 15.8 |
| Location of fracture | ||
| Femur | 6 | 31.6 |
| Tibia/Fibula | 3 | 15.8 |
| Humerus | 2 | 10.5 |
| Radius/Ulna | 5 | 26.3 |
| Clavicle | 2 | 10.5 |
| Metatarsus | 1 | 5.3 |
| Treatment | ||
| Cast | 7 | 36.8 |
| Brace | 5 | 26.3 |
| External Fixator | 3 | 15.8 |
| Nail | 3 | 15.8 |
| Wire | 4 | 21.1 |
| ND | 1 | 5.3 |
| Infection | ||
| Yes | 2 | 10.5 |
| No | 17 | 89.5 |
| Risk factors | ||
| Smoke | 4 | 21.1 |
| Diabetes | 2 | 10.5 |
| Osteoporosis | 1 | 5.3 |
| Corticosteroids | 1 | 5.3 |
| Serious Osteomalacia | 1 | 5.3 |
| None | 10 | 52.6 |
| Parameter | N | % |
|---|---|---|
| Sex | ||
| Male | 15 | 93.7 |
| Female | 1 | 6.3 |
| Fracture type | ||
| Closed | 10 | 62.5 |
| Open | 6 | 37.5 |
| Location of fracture | ||
| Femur | 5 | 31.3 |
| Tibia/Fibula | 5 | 31.3 |
| Humerus | 4 | 25.0 |
| Radius/Ulna | 2 | 12.5 |
| Treatment | ||
| Fixator | 7 | 43.7 |
| Nail | 4 | 25.0 |
| Plate | 3 | 18.7 |
| Wire | 1 | 6.3 |
| Removal of infected tissue | 1 | 6.3 |
| Infection | ||
| Yes | 8 | 50.0 |
| No | 8 | 50.0 |
| Risk factors | ||
| Smoke | 11 | 68.7 |
| Diabetes | 1 | 6.3 |
| None | 4 | 25.0 |
| Age | N of Patients | Healed | Healing Rate |
|---|---|---|---|
| ≤40 years | 21 | 17 | 81% |
| >41 years | 21 | 20 | 95% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romanò, C.L.; Kirienko, A.; Sandrone, C.; Toro, G.; Toro, A.; Valente, E.P.; Caporale, M.; Imbimbo, M.; Falzarano, G.; Setti, S.; et al. Low-Intensity Pulsed Ultrasound in the Treatment of Nonunions and Fresh Fractures: A Case Series. Trauma Care 2022, 2, 174-184. https://doi.org/10.3390/traumacare2020014
Romanò CL, Kirienko A, Sandrone C, Toro G, Toro A, Valente EP, Caporale M, Imbimbo M, Falzarano G, Setti S, et al. Low-Intensity Pulsed Ultrasound in the Treatment of Nonunions and Fresh Fractures: A Case Series. Trauma Care. 2022; 2(2):174-184. https://doi.org/10.3390/traumacare2020014
Chicago/Turabian StyleRomanò, Carlo Luca, Alexander Kirienko, Clemente Sandrone, Giuseppe Toro, Antonio Toro, Ettore Piero Valente, Manlio Caporale, Margareth Imbimbo, Gabriele Falzarano, Stefania Setti, and et al. 2022. "Low-Intensity Pulsed Ultrasound in the Treatment of Nonunions and Fresh Fractures: A Case Series" Trauma Care 2, no. 2: 174-184. https://doi.org/10.3390/traumacare2020014
APA StyleRomanò, C. L., Kirienko, A., Sandrone, C., Toro, G., Toro, A., Valente, E. P., Caporale, M., Imbimbo, M., Falzarano, G., Setti, S., & Meani, E. (2022). Low-Intensity Pulsed Ultrasound in the Treatment of Nonunions and Fresh Fractures: A Case Series. Trauma Care, 2(2), 174-184. https://doi.org/10.3390/traumacare2020014






