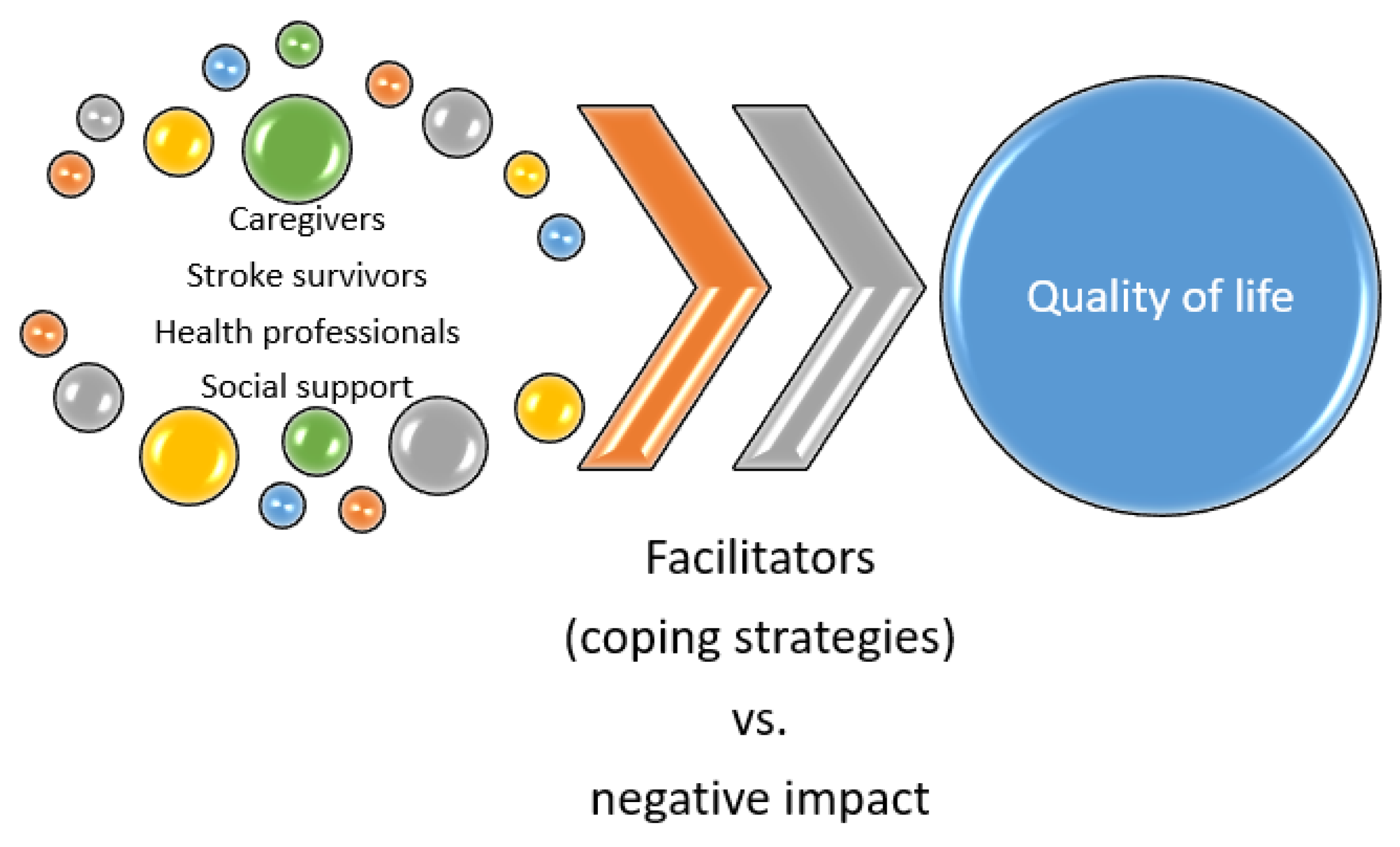
A Scoping Review on Coping Strategies and Quality of Life of Stroke Caregivers: Often Underestimated Variables in Stroke Recovery Process?
Abstract
1. Introduction
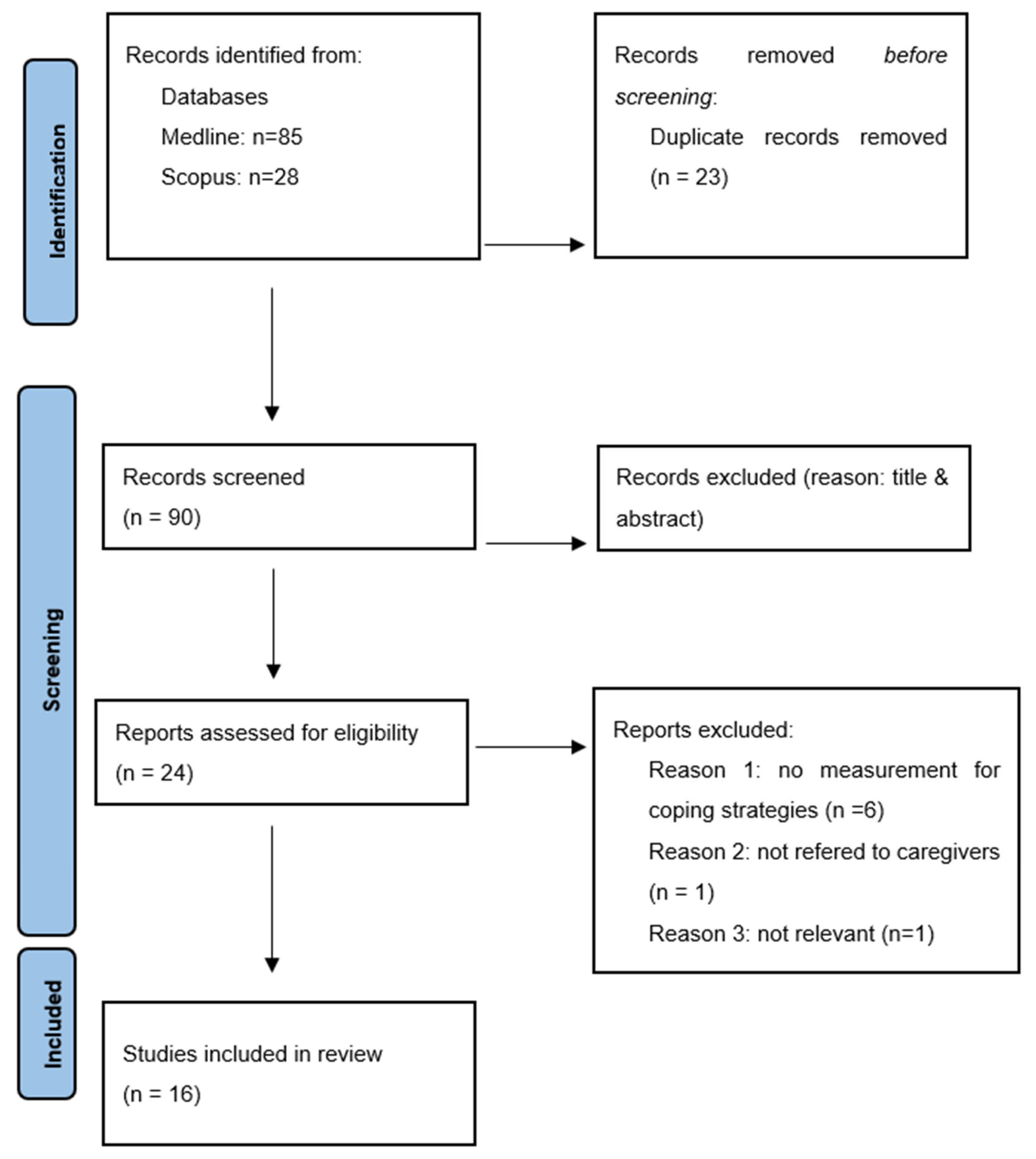
2. Methods
2.1. Research Strategy
2.2. Selection Criteria
2.3. Data Extraction
3. Results
3.1. Database Searches
3.2. Type of Research
3.3. Caregivers’ Characteristics
3.4. Time since Stroke Onset and Duration of Care for Stroke Survivors
3.5. Outcomes on Quality of Life
3.6. Outcomes on Coping Strategies
3.6.1. Mutuality
3.6.2. Social Support
3.6.3. Preparedness
3.6.4. Resilience
3.6.5. Spirituality
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feigin, V.L.; Norrving, B.; Mensah, G.A. Global Burden of Stroke. Circ. Res. 2017, 120, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Pindus, D.M.; Mullis, R.; Lim, L.; Wellwood, I.; Rundell, A.V.; Abd Aziz, N.A.; Mant, J. Stroke Survivors’ and Informal Caregivers’ Experiences of Primary Care and Community Healthcare Services—A Systematic Review and Meta-Ethnography. PLoS ONE 2018, 13, e0192533. [Google Scholar] [CrossRef]
- Visser-Meily, A.; Post, M.; Gorter, J.W.; Berlekom, S.B.V.; Van Den Bos, T.; Lindeman, E. Rehabilitation of Stroke Patients Needs a Family-Centred Approach. Disabil. Rehabil. 2006, 28, 1557–1561. [Google Scholar] [CrossRef] [PubMed]
- Panzeri, A.; Rossi Ferrario, S.; Vidotto, G. Interventions for Psychological Health of Stroke Caregivers: A Systematic Review. Front. Psychol. 2019, 10, 2045. [Google Scholar] [CrossRef] [PubMed]
- Cameron, J.I.; Gignac, M.A.M. “Timing It Right”: A Conceptual Framework for Addressing the Support Needs of Family Caregivers to Stroke Survivors from the Hospital to the Home. Patient Educ. Couns. 2008, 70, 305–314. [Google Scholar] [CrossRef]
- Tsai, P.-C.; Yip, P.-K.; Tai, J.J.; Lou, M.-F. Needs of Family Caregivers of Stroke Patients: A Longitudinal Study of Caregivers’ Perspectives. Patient Prefer. Adherence 2015, 9, 449–457. [Google Scholar] [CrossRef]
- MacIsaac, L.; Harrison, M.B.; Buchanan, D.; Hopman, W.M. Supportive Care Needs after an Acute Stroke: A Descriptive Enquiry of Caregivers’ Perspective. J. Neurosci. Nurs. 2011, 43, 132–140. [Google Scholar] [CrossRef]
- Cullinane, J.P.; Plowright, C.I. Patients’ and Relatives’ Experiences of Transfer from Intensive Care Unit to Wards. Nurs. Crit. Care 2013, 18, 289–296. [Google Scholar] [CrossRef]
- Fens, M.; van Heugten, C.M.; Beusmans, G.; Metsemakers, J.; Kester, A.; Limburg, M. Effect of a Stroke-Specific Follow-up Care Model on the Quality of Life of Stroke Patients and Caregivers: A Controlled Trial. J. Rehabil. Med. 2014, 46, 7–15. [Google Scholar] [CrossRef]
- Visser-Meily, A.; Post, M.; van de Port, I.; van Heugten, C.; van den Bos, T. Psychosocial Functioning of Spouses in the Chronic Phase after Stroke: Improvement or Deterioration between 1 and 3 Years after Stroke? Patient Educ. Couns. 2008, 73, 153–158. [Google Scholar] [CrossRef]
- Lazarus, R.S. Emotion and Adaptation; Oxford University Press: New York, NY, USA, 1991; p. 557. ISBN 978-0-19-506994-5. [Google Scholar]
- Penley, J.A.; Tomaka, J.; Wiebe, J.S. The Association of Coping to Physical and Psychological Health Outcomes: A Meta-Analytic Review. J. Behav. Med. 2002, 25, 551–603. [Google Scholar] [CrossRef]
- Yu, Y.; Hu, J.; Efird, J.T.; McCoy, T.P. Social Support, Coping Strategies and Health-Related Quality of Life among Primary Caregivers of Stroke Survivors in China. J. Clin. Nurs. 2013, 22, 2160–2171. [Google Scholar] [CrossRef]
- Visser-Meily, A.; Post, M.; van de Port, I.; Maas, C.; Forstberg-Wärleby, G.; Lindeman, E. Psychosocial Functioning of Spouses of Patients with Stroke from Initial Inpatient Rehabilitation to 3 Years Poststroke: Course and Relations with Coping Strategies. Stroke 2009, 40, 1399–1404. [Google Scholar] [CrossRef]
- White, C.L.; Mayo, N.; Hanley, J.A.; Wood-Dauphinee, S. Evolution of the Caregiving Experience in the Initial 2 Years Following Stroke. Res. Nurs. Health 2003, 26, 177–189. [Google Scholar] [CrossRef]
- Li, T.-C.; Lee, Y.-D.; Lin, C.-C.; Amidon, R.L. Quality of Life of Primary Caregivers of Elderly with Cerebrovascular Disease or Diabetes Hospitalized for Acute Care: Assessment of Well-Being and Functioning Using the SF-36 Health Questionnaire. Qual. Life Res. 2004, 13, 1081–1088. [Google Scholar] [CrossRef]
- Jönsson, A.-C.; Lindgren, I.; Hallström, B.; Norrving, B.; Lindgren, A. Determinants of Quality of Life in Stroke Survivors and Their Informal Caregivers. Stroke 2005, 36, 803–808. [Google Scholar] [CrossRef]
- Morimoto, T.; Schreiner, A.S.; Asano, H. Caregiver Burden and Health-Related Quality of Life among Japanese Stroke Caregivers. Age Ageing 2003, 32, 218–223. [Google Scholar] [CrossRef]
- Clark, P.C.; Aycock, D.M.; Reiss, A.; Tanner, D.; Shenvi, N.V.; Easley, K.A.; Wolf, S.L. Potential Benefits for Caregivers of Stroke Survivors Receiving BTX-A and Exercise for Upper Extremity Spasticity. Rehabil. Nurs. 2015, 40, 188–196. [Google Scholar] [CrossRef]
- Chow, S.K.Y.; Wong, F.K.Y.; Poon, C.Y.F. Coping and Caring: Support for Family Caregivers of Stroke Survivors. J. Clin. Nurs. 2007, 16, 133–143. [Google Scholar] [CrossRef]
- Ekwall, A.K.; Sivberg, B.; Hallberg, I.R. Older Caregivers’ Coping Strategies and Sense of Coherence in Relation to Quality of Life. J. Adv. Nurs. 2007, 57, 584–596. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Alquwez, N.; Alshahrani, A.M. Influence of Spiritual Coping and Social Support on the Mental Health and Quality of Life of the Saudi Informal Caregivers of Patients with Stroke. J. Relig. Health 2021, 60, 787–803. [Google Scholar] [CrossRef] [PubMed]
- El Masry, Y.; Mullan, B.; Hackett, M. Psychosocial Experiences and Needs of Australian Caregivers of People with Stroke: Prognosis Messages, Caregiver Resilience, and Relationships. Top. Stroke Rehabil. 2013, 20, 356–368. [Google Scholar] [CrossRef] [PubMed]
- Pucciarelli, G.; Lyons, K.S.; Petrizzo, A.; Ambrosca, R.; Simeone, S.; Alvaro, R.; Lee, C.S.; Vellone, E. Protective Role of Caregiver Preparedness on the Relationship between Depression and Quality of Life in Stroke Dyads. Stroke 2022, 53, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Pucciarelli, G.; Lyons, K.S.; Simeone, S.; Lee, C.S.; Vellone, E.; Alvaro, R. Moderator Role of Mutuality on the Association between Depression and Quality of Life in Stroke Survivor-Caregiver Dyads. J. Cardiovasc. Nurs. 2021, 36, 245–253. [Google Scholar] [CrossRef]
- Pucciarelli, G.; Vellone, E.; Bolgeo, T.; Simeone, S.; Alvaro, R.; Lee, C.S.; Lyons, K.S. Role of Spirituality on the Association between Depression and Quality of Life in Stroke Survivor-Care Partner Dyads. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e006129. [Google Scholar] [CrossRef]
- Dewilde, S.; Annemans, L.; Lloyd, A.; Peeters, A.; Hemelsoet, D.; Vandermeeren, Y.; Desfontaines, P.; Brouns, R.; Vanhooren, G.; Cras, P.; et al. The Combined Impact of Dependency on Caregivers, Disability, and Coping Strategy on Quality of Life after Ischemic Stroke. Health Qual. Life Outcomes 2019, 17, 31. [Google Scholar] [CrossRef]
- Dharma, K.K.; Damhudi, D.; Yardes, N.; Haeriyanto, S. Increase in the Functional Capacity and Quality of Life among Stroke Patients by Family Caregiver Empowerment Program Based on Adaptation Model. Int. J. Nurs. Sci. 2018, 5, 357–364. [Google Scholar] [CrossRef]
- Anderson, M.A.; Buffo, C.; Ketcher, D.; Nguyen, H.; MacKenzie, J.J.; Reblin, M.; Terrill, A.L. Applying the RISE Model of Resilience in Partners Post-Stroke: A Qualitative Analysis. Ann. Behav. Med. 2022, 56, 270–281. [Google Scholar] [CrossRef]
- Mores, G.; Whiteman, R.M.; Ploeg, J.; Knobl, P.; Cahn, M.; Klaponski, L.; Lindley, A.; Fisher, K. An Evaluation of the Family Informal Caregiver Stroke Self-Management Program. Can. J. Neurol. Sci. 2018, 45, 660–668. [Google Scholar] [CrossRef]
- Cecil, R.; Thompson, K.; Parahoo, K.; McCaughan, E. Towards an Understanding of the Lives of Families Affected by Stroke: A Qualitative Study of Home Carers. J. Adv. Nurs. 2013, 69, 1761–1770. [Google Scholar] [CrossRef]
- Gholamzadeh, S.; Tengku Aizan, H.; Sharif, F.; Hamidon, B.; Rahimah, I. TExploration the Supportive Needs and Coping Behaviors of Daughter and Daughter In-Law Caregivers of Stroke Survivors, Shiraz-Iran: A Qualitative Content Analysis. Int. J. Community Based Nurs. Midwifery 2015, 3, 205–215. [Google Scholar]
- López-Espuela, F.; González-Gil, T.; Amarilla-Donoso, J.; Cordovilla-Guardia, S.; Portilla-Cuenca, J.C.; Casado-Naranjo, I. Critical Points in the Experience of Spouse Caregivers of Patients Who Have Suffered a Stroke. A Phenomenological Interpretive Study. PLoS ONE 2018, 13, e0195190. [Google Scholar] [CrossRef]
- Kruithof, W.J.; Post, M.W.M.; van Mierlo, M.L.; van den Bos, G.A.M.; de Man-van Ginkel, J.M.; Visser-Meily, J.M.A. Caregiver Burden and Emotional Problems in Partners of Stroke Patients at Two Months and One Year Post-Stroke: Determinants and Prediction. Patient Educ. Couns. 2016, 99, 1632–1640. [Google Scholar] [CrossRef]
- Sadler, E.; Sarre, S.; Tinker, A.; Bhalla, A.; McKevitt, C. Developing a Novel Peer Support Intervention to Promote Resilience after Stroke. Health Soc. Care Community 2017, 25, 1590–1600. [Google Scholar] [CrossRef]
- Hallam, W.; Morris, R. Post-Traumatic Growth in Stroke Carers: A Comparison of Theories. Br. J. Health Psychol. 2014, 19, 619–635. [Google Scholar] [CrossRef]
- Anderson, C. Presenting and Evaluating Qualitative Research. Am. J. Pharm. Educ. 2010, 74, 141. [Google Scholar] [CrossRef]
- Greenwood, N.; Mackenzie, A.; Cloud, G.C.; Wilson, N. Informal Primary Carers of Stroke Survivors Living at Home-Challenges, Satisfactions and Coping: A Systematic Review of Qualitative Studies. Disabil. Rehabil. 2009, 31, 337–351. [Google Scholar] [CrossRef]
- Kelle, U. Combining Qualitative and Quantitative Methods in Research Practice: Purposes and Advantages. Qual. Res. Psychol. 2006, 3, 293–311. [Google Scholar]
- Caruana, E.J.; Roman, M.; Hernández-Sánchez, J.; Solli, P. Longitudinal Studies. J. Thorac. Dis. 2015, 7, E537–E540. [Google Scholar] [CrossRef]
- Ohman, M.; Söderberg, S. The Experiences of Close Relatives Living with a Person with Serious Chronic Illness. Qual. Health Res. 2004, 14, 396–410. [Google Scholar] [CrossRef] [PubMed]
- Azadarmaki, T.; Bahar, M. Families in Iran: Changes, Challenges and Future. J. Comp. Fam. Stud. 2006, 37, 589–608. [Google Scholar] [CrossRef]
- Brereton, L.; Nolan, M. “You Do Know He’s Had a Stroke, Don’t You?” Preparation for Family Care-Giving—The Neglected Dimension. J. Clin. Nurs. 2000, 9, 498–506. [Google Scholar] [CrossRef] [PubMed]
- Dale, L.; Gallant, M.; Kilbride, L.; Klene, D.; Lyons, A.; Parnin, L.; Soderquist, S.; Wilder, S. Stroke Caregivers: Do They Feel Prepared? Occup. Ther. Health Care 1997, 11, 39–59. [Google Scholar] [CrossRef] [PubMed]
- Schmall, V.L. Family Caregiver Education and Training: Enhancing Self-Efficacy. J. Case Manag. 1995, 4, 156–162. [Google Scholar]
- Schaefer, J.A.; Moos, R.H. The Context for Posttraumatic Growth: Life Crises, Individual and Social Resources, and Coping. In Posttraumatic Growth: Positive Changes in the Aftermath of Crisis; The LEA Series in Personality and Clinical Psychology; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 1998; pp. 99–125. ISBN 978-0-8058-2319-6. [Google Scholar]
- Tedeschi, R.G.; Calhoun, L.G. Target Article: “Posttraumatic Growth: Conceptual Foundations and Empirical Evidence”. Psychol. Inq. 2004, 15, 1–18. [Google Scholar] [CrossRef]
- Parveen, S.; Morrison, V.; Robinson, C.A. Does Coping Mediate the Relationship between Familism and Caregiver Outcomes? Aging Ment. Health 2014, 18, 255–259. [Google Scholar] [CrossRef]
- Darlington, A.-S.E.; Dippel, D.W.J.; Ribbers, G.M.; van Balen, R.; Passchier, J.; Busschbach, J.J.V. A Prospective Study on Coping Strategies and Quality of Life in Patients after Stroke, Assessing Prognostic Relationships and Estimates of Cost-Effectiveness. J. Rehabil. Med. 2009, 41, 237–241. [Google Scholar] [CrossRef]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and Evaluating Complex Interventions: The New Medical Research Council Guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef]
- Harandi, T.F.; Taghinasab, M.M.; Nayeri, T.D. The Correlation of Social Support with Mental Health: A Meta-Analysis. Electron. Physician 2017, 9, 5212–5222. [Google Scholar] [CrossRef]
- Helgeson, V.S. Social Support and Quality of Life. Qual. Life Res. 2003, 12 (Suppl. 1), 25–31. [Google Scholar] [CrossRef]
- Wang, J.; Mann, F.; Lloyd-Evans, B.; Ma, R.; Johnson, S. Associations between Loneliness and Perceived Social Support and Outcomes of Mental Health Problems: A Systematic Review. BMC Psychiatry 2018, 18, 156. [Google Scholar] [CrossRef]
- Cruz, J.P.; Colet, P.C.; Qubeilat, H.; Al-Otaibi, J.; Coronel, E.I.; Suminta, R.C. Religiosity and Health-Related Quality of Life: A Cross-Sectional Study on Filipino Christian Hemodialysis Patients. J. Relig. Health 2016, 55, 895–908. [Google Scholar] [CrossRef]
- Kao, T.-W.; Chen, P.-C.; Hsieh, C.-J.; Chiang, H.-W.; Tsang, L.-Y.; Yang, I.-F.; Tsai, T.-J.; Chen, W.-Y. Correlations between Spiritual Beliefs and Health-Related Quality of Life of Chronic Hemodialysis Patients in Taiwan. Artif. Organs 2009, 33, 576–579. [Google Scholar] [CrossRef]
- Gonçalves, J.P.B.; Lucchetti, G.; Menezes, P.R.; Vallada, H. Religious and Spiritual Interventions in Mental Health Care: A Systematic Review and Meta-Analysis of Randomized Controlled Clinical Trials. Psychol. Med. 2015, 45, 2937–2949. [Google Scholar] [CrossRef]
- Bonelli, R.; Dew, R.E.; Koenig, H.G.; Rosmarin, D.H.; Vasegh, S. Religious and Spiritual Factors in Depression: Review and Integration of the Research. Depress. Res. Treat. 2012, 2012, 962860. [Google Scholar] [CrossRef]
- Qiu, Y.; Li, S. Stroke: Coping Strategies and Depression among Chinese Caregivers of Survivors during Hospitalisation. J. Clin. Nurs. 2008, 17, 1563–1573. [Google Scholar] [CrossRef]
- Rochette, A.; Bravo, G.; Desrosiers, J.; St-Cyr/Tribble, D.; Bourget, A. Adaptation Process, Participation and Depression over Six Months in First-Stroke Individuals and Spouses. Clin. Rehabil. 2007, 21, 554–562. [Google Scholar] [CrossRef]
- McCullagh, E.; Brigstocke, G.; Donaldson, N.; Kalra, L. Determinants of Caregiving Burden and Quality of Life in Caregivers of Stroke Patients. Stroke 2005, 36, 2181–2186. [Google Scholar] [CrossRef]

| Database | Search Strategy |
|---|---|
| Pubmed | “stroke” AND “quality of life” AND “coping strategies” AND “caregivers” |
| Scopus | TITLE-ABS-KEY (“stroke” AND “quality of life” AND “coping strategies” AND “caregivers”) |
| 1st Author (Year) | Study Design, Participants (n), Caregivers’ Age (Years) | Time Since Stroke Onset | Caregivers’ Type | Caregiver’s Characteristics | QoL and Psycho-Emotional Status Scales | Coping Strategies Scales | Coping Strategies Identified | Main Findings | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Yu (2013) [13] |
| After discharge at home | Informal (spouse, adult children, siblings, other relatives, friends and sitters) |
| SF-36 | Brief COPE Inventory (BCI), Multidimensional Scale of Perceived Social Support (MSPSS) | Acceptance, active coping, positive reframing and planning |
|
| 2 | Alquwez (2021) [23] |
| Home care | Informal (family members) |
| WHO QOL-BREF, Hospital Anxiety and Depression Scale | Spiritual Coping Strategies scale, Multidimensional Scale of Perceived Social Support | Spiritual coping strategies (attending to mosques, performing Salah, reading and reciting the Qur’an (i.e., holy book), attending Umrah, and trusting Allah (i.e., God) |
|
| 3 | El Masry (2013) [24] |
| After discharge at home 3 months prior to the interview, admitted to rehabilitation services | Informal (family members) |
| N/A | Semi-structured interviews: themes; relationship and support, caregiver factors, stroke survivors, external stressors factors, positive outcomes | Cognitive strategies: seeking, attention diversion, goal setting, solution-focused problem solving |
|
| 4 | Pucciarelli (2022) [25] |
| 3 months to 1 year after discharge from hospital | Primary informal caregiver |
| WHOQOL-BREF (World Health Organization Quality of Life—BREF), Caregiver Burden Inventory, Hospital Anxiety and Depression Scale, | Mutuallity scale, Caregiver Preparedness Scale | Preparedness |
|
| 5 | Pucciarelli (2021) [26] |
| Sub-acute, chronic phase | Informal |
| Hospital Anxiety and Depression Scale, WHOQOL-BREF (World Health Organization Quality of Life—BREF), Caregiver Burden Inventory | Mutuality Scale | mutuality |
|
| 6 | Pucciarelli (2020) [27] |
| After discharge at home | Informal |
| QOL, WHOQOL-BRIEF (World Health Organization Quality of life-BRIEF), Hospital Anxiety and Depression Scale | WH OQoL-SRPB scale | Spirituality |
|
| 7 | Dewilde (2019) [28] |
| 3–36 months after hospital discharge | N/A | N/A | EQ-5D-3L | Dependency on caregivers scale, Brandtstädter and Renner Coping questionnaire | Assimilative coping (tenacious goal pursuit-TGP), accomadative (flexible goal adjustment-FGA) |
|
| 8 | Dharma (2018) [29] |
| Post-discharge from hospital of less than one month (currently undergoing treatment at home) | Informal |
| Stroke-specific quality of life (SSQoL) | N/A | Adaptive coping strategies |
|
| 9 | Anderson (2022) [30] |
| 0.5–6.5 years after stroke | Informal |
| N/A |
| Resilience |
|
| 10 | Mores (2018) [31] |
|
| Informal |
| Oberst Caregiving Burden scale | Bacas Caregiving Outcome Scale | Self-management |
|
| 11 | Cecil (2013) [32] |
| 6 weeks following hospital discharge | Informal |
| N/A | Qualitative data were collected through semistructured interviews | Intrinsic factors that help a carer to cope with the new role |
|
| 12 | Gholamzadeh (2015) [33] |
| Acute phase of stroke recovery at home | Informal |
| Focus group discussion (FGD) and individual in-depth interviews | Focus group discussion (FGD) and individual in-depth interviews |
|
|
| 13 | Lopez-Espuela (2018) [34] |
| 6 months after discharge | Informal |
| Individual, semi-structured, in-depth interviews | Quality data through semistructured interviews | Identification of coping strategies through critical points from the interviews |
|
| 14 | Kruithof (2016) [35] |
| Within the first week post-stroke | Informal |
| Caregiver Strain Index (CSI), Hospital Anxiety and Depression Scale (HADS) | Utrecht Proactive Coping Competence Scale (UPCC), General Self-efficacy Scale (GSES), Social Support List-Interaction (SSL-12-I) | Proactive coping, self-efficacy, relationship satisfaction and everyday support |
|
| 15 | Sadler (2017) [36] |
| 8–22 months post stroke | Informal |
| HRQoL-SF12 | Ιnterviews, Brief resilience scale | Qualitative analysis |
|
| 16 | Hallam (2014) [37] |
| Mean caring period 9.2 ± 7.1 years post-stroke | informal |
| Adult Carer Quality of Life | The Coping Orientation to Problems Experienced, The Post-Traumatic Growth Inventory, Multidimensional Scale of Social Support, The Rumination Scale |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsiakiri, A.; Vlotinou, P.; Paschalidou, A.; Konstantinidis, C.; Christidi, F.; Tsiptsios, D.; Detsaridou, G.; Petridou, A.; Gkantzios, A.; Karatzetzou, S.; et al. A Scoping Review on Coping Strategies and Quality of Life of Stroke Caregivers: Often Underestimated Variables in Stroke Recovery Process? BioMed 2023, 3, 349-368. https://doi.org/10.3390/biomed3030029
Tsiakiri A, Vlotinou P, Paschalidou A, Konstantinidis C, Christidi F, Tsiptsios D, Detsaridou G, Petridou A, Gkantzios A, Karatzetzou S, et al. A Scoping Review on Coping Strategies and Quality of Life of Stroke Caregivers: Often Underestimated Variables in Stroke Recovery Process? BioMed. 2023; 3(3):349-368. https://doi.org/10.3390/biomed3030029
Chicago/Turabian StyleTsiakiri, Anna, Pinelopi Vlotinou, Aikaterini Paschalidou, Christos Konstantinidis, Foteini Christidi, Dimitrios Tsiptsios, Georgia Detsaridou, Alexandra Petridou, Aimilios Gkantzios, Stella Karatzetzou, and et al. 2023. "A Scoping Review on Coping Strategies and Quality of Life of Stroke Caregivers: Often Underestimated Variables in Stroke Recovery Process?" BioMed 3, no. 3: 349-368. https://doi.org/10.3390/biomed3030029
APA StyleTsiakiri, A., Vlotinou, P., Paschalidou, A., Konstantinidis, C., Christidi, F., Tsiptsios, D., Detsaridou, G., Petridou, A., Gkantzios, A., Karatzetzou, S., Tsamakis, K., Giannakou, E., Emmanouilidou, M., Vadikolias, K., & Aggelousis, N. (2023). A Scoping Review on Coping Strategies and Quality of Life of Stroke Caregivers: Often Underestimated Variables in Stroke Recovery Process? BioMed, 3(3), 349-368. https://doi.org/10.3390/biomed3030029








