Observational Study on the Success Rate of Osseointegration: A Prospective Analysis of 15,483 Implants in a Public Health Setting
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Study Procedures
2.3. Outcome
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
Abbreviations
| SUS | Unified Health System |
| CNES | National Register of Health Establishment |
References
- Brazil. Ministry of Health. Ordinance no. 718, of December 20, 2010. Table of Procedures, Drugs, Orthoses, Prostheses and Special Materials (OPM) of the Unified Health System (SUS). Official Gazette of the Federative Republic of Brazil, Brasília (DF); 2010 Dec 31; Section 1: 101–113. Available online: https://www.gov.br/saude/pt-br (accessed on 31 December 2010).
- Brazil. Presidency of the Republic. Law No. 8,080, of September 19, 1990: 1990 [online]. Brasília: Civil House. 1990. Available online: http://www.planalto.gov.br/ccivil_03/leis/L8080.htm (accessed on 2 December 2018).
- Wally, Z.J.; Haque, A.M.; Feteira, A.; Claeyssens, F.; Goodall, R.; Reilly, G.C. Selective laser melting processed Ti6Al4V lattices with graded porosities for dental applications. J. Mech. Behav. Biomed. Mater. 2018, 90, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Albertini, M.; Yagüe, M.F.; Lazaro, P.; Herrero-Climent, M.; Ríos-Santos, J.; Bullon, P.; Gil, F. Advances in surfaces and osseointegration in implantology. Med. Oral Patol. Oral Cir. Bucal. 2015, 20, e316–e325. [Google Scholar] [CrossRef] [PubMed]
- Barfeie, A.; Wilson, J.; Rees, J. Implant surface characteristics and their effect on osseointegration. Br. Dent. J. 2015, 218, E9. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Liu, X.; Zhang, S.; Wang, L.; Ding, F.; Song, S.; Chen, X.; Deng, B.; Song, Y. Selective laser melted titanium implants play a positive role in early osseointegration in type 2 diabetes mellitus rats. Dent. Mater. J. 2020, 39, 214–221. [Google Scholar] [CrossRef] [PubMed]
- von Wilmowsky, C.V.; Moest, T.; Nkenke, E.; Stelzle, F.; Schlegel, K.A. Implants in bone: Part I. A current overview about tissue response, surface modifications and future perspectives. Oral Maxillofac. Surg. 2014, 18, 243–257. [Google Scholar] [CrossRef]
- Chowdary, S.G.; Satwalekar, P.; Nalla, S.; Reddy, R. Clinical evaluation of osseointegration using resonance frequency analysis. J. Indian Prosthodont. Soc. 2015, 15, 192–199. [Google Scholar] [CrossRef]
- Meng, H.-W.; Chien, E.Y.; Chien, H.-H. Dental implant bioactive surface modifications and their effects on osseointegration: A review. Biomark. Res. 2016, 4, 24. [Google Scholar] [CrossRef]
- Al-Sabbagh, M.; Bhavsar, I. Key Local and Surgical Factors Related to Implant Failure. Dent. Clin. N. Am. 2015, 59, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Hafezeqoran, A.; Koodaryan, R. Effect of Zirconia Dental Implant Surfaces on Bone Integration: A Systematic Review and Meta-Analysis. BioMed. Res. Int. 2017, 2017, 9246721. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Zhang, Y.; Shen, X.; Tao, B.; Liu, J.; Yuan, Z.; Cai, K. The fabrication and in vitro properties of antibacterial polydopamine-LL-37-POPC coatings on micro-arc oxidized titanium. Colloids Surf. B Biointerfaces 2018, 170, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Mikhail, F.F.; El-Din, M.; Ibrahim, T.; Zekry, K.; Nemat, A.H.; Nasry, S. Effect of Laser Therapy on the Osseointegration of Immediately Loaded Dental Implants in Patients under Vitamin C, Omega-3 and Calcium Therapy. Open Access Maced. J. Med. Sci. 2018, 6, 1468–1474. [Google Scholar] [CrossRef] [PubMed]
- Moy, P.K.; Medina, D.; Shetty, V.; Aghaloo, T.L. Dental implant failure rates and associated risk factors. Int. J. Oral Maxillofac. Implant. 2005, 20, 569–577. [Google Scholar]
- Arakeeb, M.A.A.; Zaky, A.A.; Harhash, T.A.-H.; Salem, W.S.; El-Mofty, M. Effect of Combined Application of Growth Factors and Diode Laser Bio-Stimulation on the Osseo Integration of Dental Implants. Open Access Maced. J. Med. Sci. 2019, 7, 2520–2527. [Google Scholar] [CrossRef]
- Jung, R.E.; Thoma, D.S.; Zembic, A.; Zwahlen, M.; Pjetursson, B.E. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin. Oral Implant. Res. 2012, 23, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Thoma, D.; Jung, R.; Zwahlen, M.; Zembic, A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin. Oral Implant. Res. 2012, 23, 22–38. [Google Scholar] [CrossRef] [PubMed]
- Annunziata, M.; Guida, L. The Effect of Titanium Surface Modifications on Dental Implant Osseointegration. Front Oral Biol. 2015, 17, 62–77. [Google Scholar] [CrossRef] [PubMed]
- Manju, V.; Iyer, S.; Menon, D.; Nair, S.V.; Nair, M.B. Evaluation of osseointegration of staged or simultaneously placed dental implants with nanocomposite fibrous scaffolds in rabbit mandibular defect. Mater. Sci. Eng. C Mater Biol. Appl. 2019, 104, 109864. [Google Scholar] [CrossRef]
- Parithimarkalaignan, S.; Padmanabhan, T.V. Osseointegration: An Update. J. Indian Prosthodont. Soc. 2013, 13, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Kreve, S.; dos Reis, A.C. Influence of the electrostatic condition of the titanium surface on bacterial adhesion: A systematic review. J. Prosthet. Dent. 2020, 125, 416–420. [Google Scholar] [CrossRef] [PubMed]
- Sakka, S.; Baroudi, K.; Nassani, M.Z. Factors associated with early and late failure of dental implants. J. Investig. Clin. Dent. 2012, 3, 258–261. [Google Scholar] [CrossRef]
- Hoyos-Nogués, M.; Buxadera-Palomero, J.; Ginebra, M.-P.; Manero, J.M.; Gil, F.; Mas-Moruno, C. All-in-one trifunctional strategy: A cell adhesive, bacteriostatic and bactericidal coating for titanium implants. Colloids Surf. B Biointerfaces 2018, 169, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Fadanelli, A.B.; Stemmer, A.C.; Beltrão, G.C. Premature oral implant failure. Odonto Sci. Mag. 2005, 20, 170–176. [Google Scholar]
- Zavanelli, R.A.; Guilherme, A.S.; Castro, A.T.; Fernandes, J.C.A.; Pereira, R.E.; Garcia, R.R. Local and systemic factors related to patients that can affect osseointegration. RGO—Rev Gaúcha Odontol. 2011, 59, 133–146. [Google Scholar]
- Ferraris, S.; Warchomicka, F.; Ramskogler, C.; Tortello, M.; Cochis, A.; Scalia, A.; di Confiengo, G.G.; Keckes, J.; Rimondini, L.; Spriano, S. Surface structuring by Electron Beam for improved soft tissues adhesion and reduced bacterial contamination on Ti-grade 2. J. Mater. Process. Technol. 2018, 266, 518–529. [Google Scholar] [CrossRef]
- Lekholm, U.; Zarb, G.A. Patient selection and preparation. In Tissue Integrated Prostheses: Osseointegration in Clinical Dentistry; Branemark, P.I., Zarb, G.A., Albrektsson, T., Eds.; Quintessence: Chicago, IL, USA, 1985; pp. 199–209. [Google Scholar]
- Norton, M.R.; Gamble, C. Bone classification: An objective scale of bone density using the computerized tomography scan. Clin. Oral Implant. Res. 2001, 12, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Brägger, U.; Lang, N.P.; Zwahlen, M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin. Oral Implant. Res. 2007, 18 (Suppl. 3), 97–113, Erratum in: Clin. Oral Implant. Res. 2008, 19, 326–328. [Google Scholar] [CrossRef] [PubMed]
- Windael, S.; Vervaeke, S.; De Buyser, S.; De Bruyn, H.; Collaert, B. The Long-Term Effect of Smoking on 10 Years’ Survival and Success of Dental Implants: A Prospective Analysis of 453 Implants in a Non-University Setting. J. Clin. Med. 2020, 9, 1056. [Google Scholar] [CrossRef] [PubMed]
- Lindh, C.; Obrant, K.; Petersson, A. Maxillary bone mineral density and its relationship to the bone mineral density of the lumbar spine and hip. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2004, 98, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, H.S.; Jansen, J.A. The development and future of dental implants. Dent. Mater. J. 2020, 39, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Drage, N.A.; Palmer, R.M.; Blake, G.; Wilson, R.; Crane, F.; Fogelman, I. A comparison of bone mineral density in the spine, hip and jaws of edentulous subjects. Clin. Oral Implant. Res. 2007, 18, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of Workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, S286–S291. [Google Scholar] [CrossRef]
- Alsaadi, G.; Quirynen, M.; Komárek, A.; Van Steenberghe, D. Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. J. Clin. Periodontol. 2007, 34, 610–617. [Google Scholar] [CrossRef] [PubMed]
- Huynh-Ba, G.; Friedberg, J.R.; Vogiatzi, D.; Ioannidou, E. Implant failure predictors in the posterior maxilla: A retrospective study of 273 consecutive implants. J. Periodontol. 2008, 79, 2256–2261. [Google Scholar] [CrossRef] [PubMed]
- Koldsland, O.C.; Scheie, A.A.; Aass, A.M. Prevalence of Implant Loss and the Influence of Associated Factors. J. Periodontol. 2009, 80, 1069–1075. [Google Scholar] [CrossRef]
- Baqain, Z.H.; Moqbel, W.Y.; Sawair, F.A. Early dental implant failure: Risk factors. Br. J. Oral Maxillofac. Surg. 2012, 50, 239–243. [Google Scholar] [CrossRef]
- Busenlechner, D.; Fürhauser, R.; Haas, R.; Watzek, G.; Mailath, G.; Pommer, B. Long-term implant success at the Academy for Oral Implantology: 8-year follow-up and risk factor analysis. J. Periodontal Implant. Sci. 2014, 44, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Jemt, T. Implant Survival in the Posterior Partially Edentulous Arch—30 Years of Experience. Part IV: A Retro-Prospective Multivariable Regression Analysis on Implant Failures Related to Arch and Implant Surface. Int. J. Prosthodont. 2019, 32, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Friberg, B.; Jemt, T.; Lekholm, U. Early failures in 4,641 consecutively placed Brånemark dental implants: A study from stage 1 surgery to the connection of completed prostheses. Int. J. Oral Maxillofac. Implants. 1991, 6, 142–146. [Google Scholar]
- Chrcanovic, B.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Factors Influencing Early Dental Implant Failures. J. Dent. Res. 2016, 95, 995–1002. [Google Scholar] [CrossRef]
- Elsubeihi, E.S.; Zarb, G.A. Implant prosthodontics in medically challenged patients: The University of Toronto experience. J. Can. Dent. Assoc. 2002, 68, 103–108. [Google Scholar]
- Goiato, M.C.; dos Santos, D.M.; Santiago, J.F., Jr.; Moreno, A.; Pellizzer, E.P. Longevity of dental implants in type IV bone: A systematic review. Int. J. Oral Maxillofac. Surg. 2014, 43, 1108–1116. [Google Scholar] [CrossRef] [PubMed]
- Sayardoust, S.; Omar, O.; Norderyd, O.; Thomsen, P. Clinical, radiological, and gene expression analyses in smokers and non-smokers, Part 2: RCT on the late healing phase of osseointegration. Clin. Implant Dent. Relat. Res. 2017, 19, 901–915. [Google Scholar] [CrossRef]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar] [CrossRef]
- Ribeiro-Rotta, R.F.; Lindh, C.; Pereira, A.C.; Rohlin, M. Ambiguity in bone tissue characteristics as presented in studies on dental implant planning and placement: A systematic review. Clin. Oral Implant. Res. 2011, 22, 789–801. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-J.; Yun, P.-Y.; Chang, N.-H.; Kim, Y.-K. The long-term evaluation of the prognosis of implants with acid-etched surfaces sandblasted with alumina: A retrospective clinical study. Maxillofac. Plast. Reconstr. Surg. 2010, 42, 10–19. [Google Scholar] [CrossRef]
- Yu, H.-C.; Kang, D.-W.; Kim, Y.-K. Long-term observation of immediately-installed implants after extraction: Retrospective clinical study. Oral Biol. Res. 2019, 43, 130–135. [Google Scholar] [CrossRef]
- Martinez, H.; Davarpanah, M.; Missika, P.; Celletti, R.; Lazzara, R. Optimal implant stabilization in low density bone. Clin. Oral Implant. Res. 2001, 12, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Lian, M.; Zhao, K.; Wang, F.; Huang, W.; Zhang, X.; Wu, Y. Stud vs Bar Attachments for Maxillary Four-Implant–Supported Overdentures: 3- to 9-year Results from a Retrospective Study. Int. J. Oral Maxillofac. Implant. 2019, 34, 936–946. [Google Scholar] [CrossRef]
- Davarpanah, M.; Martinez, H.; Kebir, M.; Tecucianu, J.F. Manual of Clinical Implantology; Artmed Editora: São Paulo, Brazil, 2003. [Google Scholar]
- Biguetti, C.C.; Cavalla, F.; Silveira, E.M.; Fonseca, A.C.; Vieira, A.E.; Tabanez, A.P.; Rodrigues, D.C.; Trombone, A.P.F.; Garlet, G.P. Oral implant osseointegration model in C57Bl/6 mice: Microtomographic, histological, histomorphometric and molecular characterization. J. Appl. Oral Sci. 2018, 26, e20170601. [Google Scholar] [CrossRef]
- Geckili, O.; Bilhan, H.; Geckili, E.; Cilingir, A.; Mumcu, E.; Bural, C. Evaluation of Possible Prognostic Factors for the Success, Survival, and Failure of Dental Implants. Implant. Dent. 2014, 23, 44–50. [Google Scholar] [CrossRef]
- Yue, G.; Edani, H.; Sullivan, A.; Jiang, S.; Kazerani, H.; Saghiri, M.A. Is maxillary diastema an appropriate site for implantation in rats? Int. J. Implant. Dent. 2020, 6, 8. [Google Scholar] [CrossRef]
- Montes, C.C.; Pereira, F.A.; Thomé, G.; Alves, E.D.M.; Acedo, R.V.; de Souza, J.R.; Melo, A.C.M.; Trevilatto, P.C. Failing Factors Associated With Osseointegrated Dental Implant Loss. Implant. Dent. 2007, 16, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Bassir, S.H.; El Kholy, K.; Chen, C.; Lee, K.H.; Intini, G. Outcome of early dental implant placement versus other dental implant placement protocols: A systematic review and meta-analysis. J. Periodontol. 2019, 90, 493–506. [Google Scholar] [CrossRef] [PubMed]
- Berberi, A.N.; Tehini, G.E.; Noujeim, Z.F.; Khairallah, A.A.; Abousehlib, M.N.; Salameh, Z.A. Influence of Surgical and Prosthetic Techniques on Marginal Bone Loss around Titanium Implants. Part I: Immediate Loading in Fresh Extraction Sockets. J. Prosthodont. 2014, 23, 521–527. [Google Scholar] [CrossRef] [PubMed]
- García-García, M.; Mir-Mari, J.; Benic, G.I.; Figueiredo, R.; Valmaseda-Castellón, E. Accuracy of periapical radiography in assessing bone level in implants affected by peri-implantitis: A cross-sectional study. J. Clin. Periodontol. 2016, 43, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Sahm, N.; Mihatovic, I.; Golubovic, V.; Becker, J. Surgical therapy of advanced ligature-induced peri-implantitis defects: Cone-beam computed tomographic and histological analysis. J. Clin. Periodontol. 2011, 38, 939–949. [Google Scholar] [CrossRef] [PubMed]
| Municipality | Dental Specialist Center | National Registry of Health Establishments (CNES) |
|---|---|---|
| Brejo do Cruz—PB | Brejo do Cruz | 7481772 |
| Mogeiro—PB | Mogeiro | 7983565 |
| Pombal—PB | Pompal | 3990931 |
| Sumé—PB | Imaculada Conceição | 3738558 |
| Inclusion | Exclusion |
|---|---|
| Age | Age |
| 18–75 years | <18 or >75 years |
| Chronic disease | Chronic disease |
| No | Yes |
| Implant | Implant |
| Systhex® | No Systhex® |
| ≥8.5 mm | <8.5 mm |
| Bone installed | Graft installed |
| ≥20 N·cm2 | <20 N.cm2 |
| Prosthesis installation | Prosthesis installation |
| 06 months | < or > 06 months |
| Same surgical team | Different surgical team |
| Variables | N (%) |
|---|---|
| Age | |
| 18–75 years | 3690 (100%) |
| Sex | |
| Men | 1550 (42%) |
| Women | 2140 (58%) |
| Color | |
| White | 960 (26%) |
| Brown/Black | 2730 (74%) |
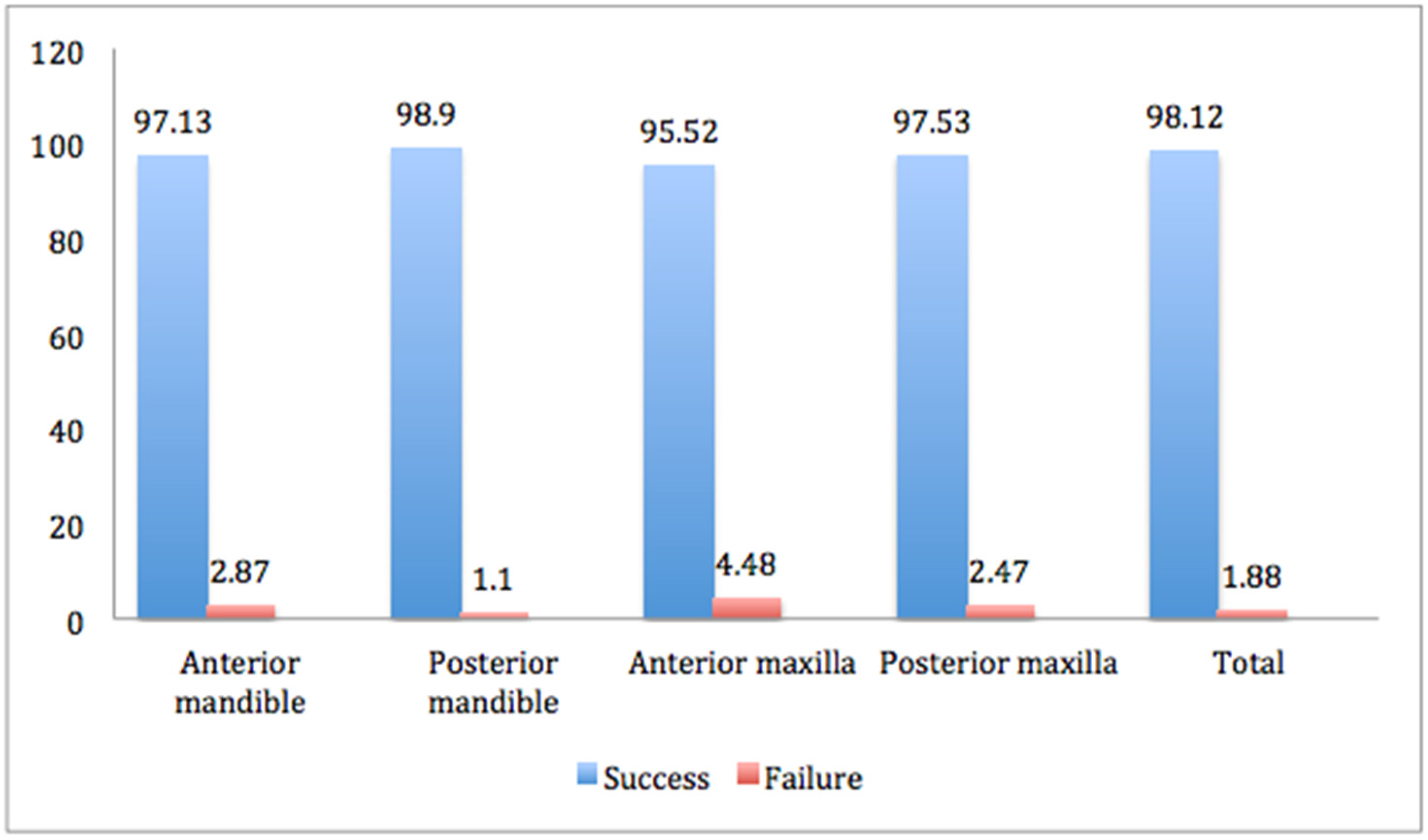
| Implant Region | Total Implants | Success | Failure | ||
|---|---|---|---|---|---|
| Number | Rate, % | Number | Rate, % | ||
| Mandible | |||||
| Anterior | 1115 | 1083 | 97.13 | 32 | 2.87 |
| Posterior | 8844 | 8747 | 98.90 | 97 | 1.10 |
| Maxilla | |||||
| Anterior | 1272 | 1215 | 95.52 | 57 | 4.48 |
| Posterior | 4252 | 4147 | 97.53 | 105 | 2.47 |
| Study Groups | p Value * |
|---|---|
| Anterior mandible vs. posterior mandible | 0.001 |
| Anterior mandible vs. anterior maxilla | 0.035 |
| Anterior mandible vs. posterior maxilla | 0.470 |
| Posterior mandible vs. anterior maxilla | <0.001 |
| Posterior mandible vs. posterior maxilla | <0.001 |
| Anterior maxilla vs. posterior maxilla | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simão, B.S., Jr.; Costa, D.D.; Cangussu, M.C.T.; Sotto-Maior, B.S.; Devita, R.L.; de Carvalho, J.J.; da Silva Brum, I. Observational Study on the Success Rate of Osseointegration: A Prospective Analysis of 15,483 Implants in a Public Health Setting. BioMed 2022, 2, 422-430. https://doi.org/10.3390/biomed2040033
Simão BS Jr., Costa DD, Cangussu MCT, Sotto-Maior BS, Devita RL, de Carvalho JJ, da Silva Brum I. Observational Study on the Success Rate of Osseointegration: A Prospective Analysis of 15,483 Implants in a Public Health Setting. BioMed. 2022; 2(4):422-430. https://doi.org/10.3390/biomed2040033
Chicago/Turabian StyleSimão, Butruz Sarkis, Jr., Denis Damião Costa, Maria Cristina Teixeira Cangussu, Bruno Salles Sotto-Maior, Renan Lana Devita, Jorge José de Carvalho, and Igor da Silva Brum. 2022. "Observational Study on the Success Rate of Osseointegration: A Prospective Analysis of 15,483 Implants in a Public Health Setting" BioMed 2, no. 4: 422-430. https://doi.org/10.3390/biomed2040033
APA StyleSimão, B. S., Jr., Costa, D. D., Cangussu, M. C. T., Sotto-Maior, B. S., Devita, R. L., de Carvalho, J. J., & da Silva Brum, I. (2022). Observational Study on the Success Rate of Osseointegration: A Prospective Analysis of 15,483 Implants in a Public Health Setting. BioMed, 2(4), 422-430. https://doi.org/10.3390/biomed2040033






