Healthy Aging in Place with the Aid of Smart Technologies: A Systematic Review
Abstract
1. Introduction
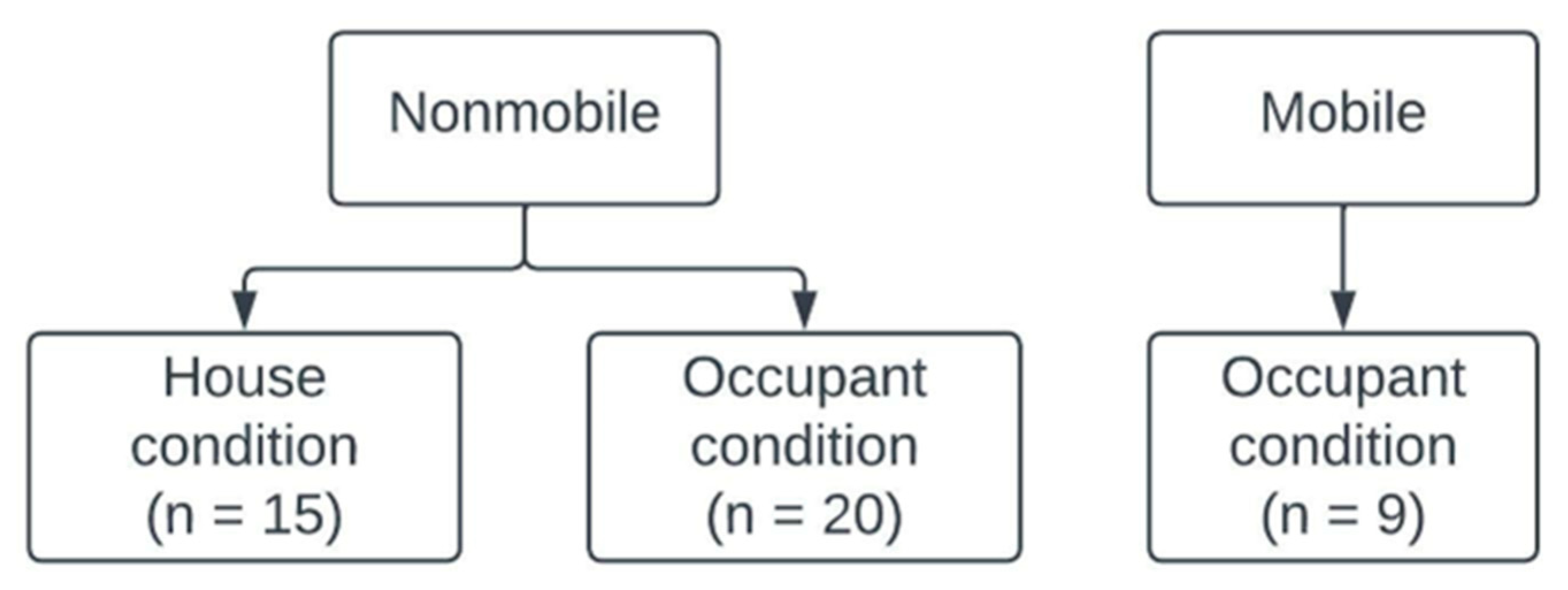
2. Method and Materials
3. Descriptive Statistics
4. Results
4.1. Types of Smart Technologies
4.2. Physical Health Benefits
4.2.1. Monitoring Home Conditions
4.2.2. Monitoring Older Adults’ Physical Conditions
4.2.3. Benefits of Long-Term Independent Living
4.3. Mental Health Benefits (Social Connectivity)
4.3.1. Maintaining Social Connections and Improvements in Mental Health
4.3.2. Positive Image of Using New Technologies
4.4. Cost Benefits
4.4.1. Reduction in Healthcare Costs
4.4.2. Long-Term Care Cost Savings
4.4.3. Economic Benefits for Caregivers
4.4.4. Addressing Financial Barriers
4.4.5. Long-Term Financial Sustainability
4.5. Barriers to Smart Technology Adoption
4.5.1. Privacy Concerns
4.5.2. Lack of Understanding of Technology
4.5.3. Cost of Devices
4.5.4. Technical Defects
5. Discussion and Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Ageing and Health. World Health Organization. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health#:~:text=By%202050%2C%20the%20world's%20population,2050%20to%20reach%20426%20million. (accessed on 2 August 2022).
- United Nations. World Population Ageing. 2019. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf (accessed on 20 October 2022).
- Boldy, D.; Grenade, L.; Lewin, G.; Karol, E.; Burton, E. Older people’s decisions regarding ‘ageing in place’: A Western Australian case study: Ageing in place decisions of older people. Aust. J. Ageing 2011, 30, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Roy, N.; Dubé, R.; Després, C.; Freitas, A.; Légaré, F. Choosing between staying at home or moving: A systematic review of factors influencing housing decisions among frail older adults. PLoS ONE 2018, 13, e0189266. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; the PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.K.; Thompson, H.J.; Demiris, G. Use of an Internet-of-Things Smart Home System for Healthy Aging in Older Adults in Residential Settings: Pilot Feasibility Study. JMIR Aging 2020, 3, e21964. [Google Scholar] [CrossRef]
- Arthanat, S.; Wilcox, J.; Macuch, M. Profiles and predictors of smart home technology adoption by older adults. OTJR Occup. Particip. Health 2019, 39, 247–256. [Google Scholar] [CrossRef]
- Choi, Y.K.; Thompson, H.J.; Demiris, G. Internet-of-Things Smart Home Technology to Support Aging-in-Place: Older Adults’ Perceptions and Attitudes. J. Gerontol. Nurs. 2021, 47, 15–21. [Google Scholar] [CrossRef]
- Chaparro, J.D.; Ruiz, J.F.-B.; Romero, M.J.S.; Peño, C.B.; Irurtia, L.U.; Perea, M.G.; Garcia, X.d.T.; Molina, F.J.V.; Grigoleit, S.; Lopez, J.C. The SHAPES Smart Mirror Approach for Independent Living, Healthy and Active Ageing. Sensors 2021, 21, 7938. [Google Scholar] [CrossRef]
- Borelli, E.; Paolini, G.; Antoniazzi, F.; Barbiroli, M.; Benassi, F.; Chesani, F.; Chiari, L.; Fantini, M.; Fuschini, F.; Galassi, A. HABITAT: An IoT solution for independent elderly. Sensors 2019, 19, 1258. [Google Scholar] [CrossRef]
- Jachan, D.E.; Müller-Werdan, U.; Lahmann, N.A.; Strube-Lahmann, S. Smart@ Home–Supporting safety and mobility of elderly and care dependent people in their own homes through the use of technical assistance systems and conventional mobility supporting tools: A cross-sectional survey. BMC Geriatr. 2021, 21, 205. [Google Scholar] [CrossRef]
- Nauha, L.; Keränen, N.S.; Kangas, M.; Jämsä, T.; Reponen, J. Assistive technologies at home for people with a memory disorder. Dementia 2018, 17, 909–923. [Google Scholar] [CrossRef]
- Dasios, A.; Gavalas, D.; Pantziou, G.; Konstantopoulos, C. Hands-on experiences in deploying cost-effective ambient-assisted living systems. Sensors 2015, 15, 14487–14512. [Google Scholar] [CrossRef] [PubMed]
- Barakat, A.; Woolrych, R.D.; Sixsmith, A.; Kearns, W.D.; Kort, H.S. eHealth Technology Competencies for Health Professionals Working in Home Care to Support Older Adults to Age in Place: Outcomes of a Two-Day Collaborative Workshop. Medicine 2.0 2013, 2, e10. [Google Scholar] [CrossRef] [PubMed]
- Offermann-van Heek, J.; Schomakers, E.-M.; Ziefle, M. Bare necessities? How the need for care modulates the acceptance of ambient assisted living technologies. Int. J. Med. Inform. 2019, 127, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Bedaf, S.; Marti, P.; Amirabdollahian, F.; de Witte, L. A multi-perspective evaluation of a service robot for seniors: The voice of different stakeholders. Disabil. Rehabil. Assist. Technol. 2018, 13, 592–599. [Google Scholar] [CrossRef]
- Arthanat, S. Promoting information communication technology adoption and acceptance for aging-in-place: A randomized controlled trial. J. Appl. Gerontol. 2021, 40, 471–480. [Google Scholar] [CrossRef]
- Freeman, S.; Marston, H.R.; Olynick, J.; Musselwhite, C.; Kulczycki, C.; Genoe, R.; Xiong, B. Intergenerational effects on the impacts of technology use in later life: Insights from an international, multi-site study. Int. J. Environ. Res. Public Health 2020, 17, 5711. [Google Scholar] [CrossRef]
- Wong, J.K.W.; Leung, J.; Skitmore, M.; Buys, L. Technical requirements of age-friendly smart home technologies in high-rise residential buildings: A system intelligence analytical approach. Autom. Constr. 2017, 73, 12–19. [Google Scholar] [CrossRef]
- Yu, J.; An, N.; Hassan, T.; Kong, Q. A Pilot Study on a Smart Home for Elders Based on Continuous In-Home Unobtrusive Monitoring Technology. HERD Health Environ. Res. Des. J. 2019, 12, 206–219. [Google Scholar] [CrossRef]
- Wu, C.-L.; Chen, Y.-H.; Chien, Y.-W.; Tsai, M.-J.; Li, T.-Y.; Cheng, P.-H.; Fu, L.-C.; Chen, C.C.-H. Nonparametric activity recognition system in smart homes based on heterogeneous sensor data. IEEE Trans. Autom. Sci. Eng. 2018, 16, 678–690. [Google Scholar] [CrossRef]
- Chung, J.; Bleich, M.; Wheeler, D.C.; Winship, J.M.; McDowell, B.; Baker, D.; Parsons, P. Attitudes and Perceptions Toward Voice-Operated Smart Speakers Among Low-Income Senior Housing Residents: Comparison of Pre- and Post-Installation Surveys. Gerontol. Geriatr. Med. 2021, 7, 233372142110058. [Google Scholar] [CrossRef]
- Charness, N.; Best, R.; Evans, J. Supportive home health care technology for older adults: Attitudes and implementation. Gerontechnology 2016, 15, 233–242. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lazarou, I.; Karakostas, A.; Stavropoulos, T.G.; Tsompanidis, T.; Meditskos, G.; Kompatsiaris, I.; Tsolaki, M. A novel and intelligent home monitoring system for care support of elders with cognitive impairment. J. Alzheimer’s Dis. 2016, 54, 1561–1591. [Google Scholar] [CrossRef] [PubMed]
- Corbett, C.F.; Combs, E.M.; Wright, P.J.; Owens, O.L.; Stringfellow, I.; Nguyen, T.; Van Son, C.R. Virtual home assistant use and perceptions of usefulness by older adults and support person dyads. Int. J. Environ. Res. Public Health 2021, 18, 1113. [Google Scholar] [CrossRef] [PubMed]
- Woods, O.; Kong, L. New cultures of care? The spatio-temporal modalities of home-based smart eldercare technologies in Singapore. Soc. Cult. Geogr. 2020, 21, 1307–1327. [Google Scholar] [CrossRef]
- Rocha, A.; Martins, A.; Junior, J.C.F.; Boulos, M.N.K.; Vicente, M.E.; Feld, R.; van de Ven, P.; Nelson, J.; Bourke, A.; ÓLaighin, G. Innovations in health care services: The CAALYX system. Int. J. Med. Inform. 2013, 82, e307–e320. [Google Scholar] [CrossRef]
- Bock, C.; Demiris, G.; Choi, Y.; Le, T.; Thompson, H.J.; Samuel, A.; Huang, D. Engaging older adults in the visualization of sensor data facilitated by an open platform for connected devices. Technol. Health Care 2016, 24, 541–550. [Google Scholar] [CrossRef]
- Cao, Y.; Erdt, M.; Robert, C.; Naharudin, N.B.; Lee, S.Q.; Theng, Y.-L. Decision-making Factors Toward the Adoption of Smart Home Sensors by Older Adults in Singapore: Mixed Methods Study. JMIR Aging 2022, 5, e34239. [Google Scholar] [CrossRef]
- Street, J.; Barrie, H.; Eliott, J.; Carolan, L.; McCorry, F.; Cebulla, A.; Phillipson, L.; Prokopovich, K.; Hanson-Easey, S.; Burgess, T.; et al. Older Adults’ Perspectives of Smart Technologies to Support Aging at Home: Insights from Five World Café Forums. Int. J. Environ. Res. Public Health 2022, 19, 7817. [Google Scholar] [CrossRef]
- Demiris, G.; Oliver, D.P.; Dickey, G.; Skubic, M.; Rantz, M. Findings from a participatory evaluation of a smart home application for older adults. Technol. Health Care 2008, 16, 111–118. [Google Scholar] [CrossRef]
- Aggar, C.; Sorwar, G.; Seton, C.; Penman, O.; Ward, A. Smart home technology to support older people’s quality of life: A longitudinal pilot study. Int. J. Older People Nurs. 2022, 18, e12489. [Google Scholar] [CrossRef]
- Houston, D.; Wu, J.; Ong, P.; Winer, A. Structural disparities of urban traffic in Southern California: Implications for vehicle-related air pollution exposure in minority and high-poverty neighborhoods. J. Urban Aff. 2004, 26, 565–592. [Google Scholar] [CrossRef]
- National Council on Aging Get the Facts on Falls Prevention. Available online: https://ncoa.org/article/get-the-facts-on-falls-prevention (accessed on 5 December 2022).
- Centers for Disease Control and Prevention Facts About Falls. Available online: https://www.cdc.gov/falls/facts.html (accessed on 5 December 2022).
- Santini, Z.I.; Jose, P.E.; York Cornwell, E.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Cacioppo, S. Older adults reporting social isolation or loneliness show poorer cognitive function 4 years later. Evid.-Based Nurs. 2014, 17, 59–60. [Google Scholar] [CrossRef] [PubMed]
- Taylor, H.O.; Taylor, R.J.; Nguyen, A.W.; Chatters, L. Social Isolation, Depression, and Psychological Distress Among Older Adults. J. Aging Health 2018, 30, 229–246. [Google Scholar] [CrossRef]
- Sixsmith, A.; Gutman, G.M. Technologies for Active Aging; International Perspectives on Aging; Springer: New York, NY, USA, 2013; ISBN 978-1-4419-8348-0. [Google Scholar]
- Gemworth Since 2004, Families Across America Have Counted on Us to Help Them Understand the Cost of Care. Available online: https://www.genworth.com/aging-and-you/finances/cost-of-care/cost-of-care-trends-and-insights.html (accessed on 5 December 2022).
- Tural, E.; Lu, D.; Austin Cole, D. Safely and actively aging in place: Older adults’ attitudes and intentions toward smart home technologies. Gerontol. Geriatr. Med. 2021, 7, 23337214211017340. [Google Scholar] [CrossRef]
- Hela, S.; Amel, B.; Badran, R. Early anomaly detection in smart home: A causal association rule-based approach. Artif. Intell. Med. 2018, 91, 57–71. [Google Scholar] [CrossRef]
- Morris, M.E.; Adair, B.; Ozanne, E.; Kurowski, W.; Miller, K.J.; Pearce, A.J.; Santamaria, N.; Long, M.; Ventura, C.; Said, C.M. Smart technologies to enhance social connectedness in older people who live at home: Smart technology and social connectedness. Australas. J. Ageing 2014, 33, 142–152. [Google Scholar] [CrossRef]


| Author | Year | Method | Tech Type |
|---|---|---|---|
| Choi et al. [6] | 2020 | Quantitative study | IoT smart home devices (multipurpose sensors to detect motion, temperature and luminosity, voice-assisted smart speaker, door and window sensor, monitoring cameras) |
| Arthanat et al. [7] | 2019 | Quantitative | Carbon monoxide alarm, manually programmable thermostat, auto set thermostat, motion sensor lights, backup generator, home security system, voice-activated assistant, emergency alert system, water leak detector, motion-activated camera, auto shutoff stove, smart home control, remote monitoring |
| Choi et al. [8] | 2021 | Quantitative study | IoT smart home devices (multipurpose sensors to detect motion, temperature, and luminosity, voice-assisted smart speaker, door and window sensor, monitoring cameras) |
| Chaparro et al. [9] | 2021 | Qualitative study | Smart sensors to detect fall and physical activity, voice assistant, calendar reminder, home monitoring system |
| Borelli et al. [10] | 2019 | Quantitative and Qualitative | Wall light for indoor localization, armchair for sitting posture monitoring, wall panel and mobile devices |
| Jachan et al. [11] | 2021 | Quantitative study | Smart home solution (tablet, stove safety, lightening control, LED strip, visual doorbell, door detector, automatic switch, inactivity detector, fall detection sensors, home emergency call) |
| Nauha et al. [12] | 2018 | Qualitative study | Smart technologies (smart flower stand, fall alarm, bed alarm, medicine dispenser, GPS safety bracelet, web chat tablet computer, motion sensor, reminder with motion sensor, motion sensor, calendar clock, talking album, weighted ball blanket, therapy apron, and cube) |
| Dasios et al. [13] | 2015 | Qualitative | an AAL-based prototype system for elderly home care monitoring based on the recording of environmental parameters |
| Barakat et al. [14] | 2013 | Qualitative study | eHealth Technology (e.g., remote telecare and AAL, mobile health, and fall detection systems) |
| Offermann-van Heek et al. [15]. | 2019 | Quantitative study | Ambient assistive technology (microphone system, camera, motion detector, smart watch, emergency button) |
| Bedaf et al. [16] | 2017 | Qualitative | Robot that contains image sensors that can detect learning and detection |
| Arthanat [17] | 2021 | Quantitative study | Individualized community and home-based access to technology training (ict training) program |
| Freeman et al. [18] | 2020 | Quantitative and Qualitative | digital/video game console, internet at home, SNSs, email, cellphone, computer |
| Wong et al. [19] | 2017 | Qualitative study | Smart home devices |
| Yu et al. [20] | 2019 | Quantitative study (pilot study) | Unobtrusive sensors in multiple rooms to monitor temperature, humidity, pressure water meter, and electricity meter |
| Wu et al. [21] | 2018 | Quantitative study | Smart home environment, ambient sensors, and on-body sensors |
| Chung et al. [22] | 2021 | Quantitative study | Voice-operated smart speaker |
| Charness et al. [23] | 2016 | Quantitative study | Wrist-worn health monitoring device |
| Lazarou et al. [24] | 2016 | Quantitative | Home monitoring system (camera sensor, sleep sensor, bracelet, wireless tags and plugs, mobile devices in an Ambient Assisted Living (AAL) context) |
| Corbett et al. [25] | 2021 | Qualitative and Quantitative study | Virtual home assistant equipment |
| Woods and Kong [26] | 2020 | Qualitative study | Smart eldercare technologies |
| Rocha et al. [27] | 2015 | Quantitative | Mobile system equipped with a set of wellbeing sensors, home system to collect medical data, wearable light device (WLD) that has ECG instruments, an SpO2 meter, a temperature sensor and a fall and mobility sensor |
| Bock et al. [28] | 2016 | Qualitative study | Multi-sensors to detect and collect data on individual’s motion, home temperature, luminosity, and humidity |
| Cao et al. [29] | 2022 | Qualitative study | Smart home sensors (motion sensors and smart plug, door contact, key tag, a mobile app) |
| Street et al. [30] | 2022 | Qualitative study | Smart technology |
| Demiris et al. [31] | 2008 | Qualitative study | In-Home Monitoring (wireless sensors to detect motions, stove temperature sensors, bed sensors) |
| Aggar et al. [32] | 2022 | Quantitative study | Smart home technology and assistive technology (Google Hub, smart watches, Chromecast, Phillips Hue Smart Lightning, smoke detector, light strips, smart mop, smart lock, smart doorbell, motion sensor, security camera) |
| Houston et al. [33] | 2004 | Quantitative study | Sensors, Smart home technologies |
| National Council on Aging [34] | 2022 | Quantitative study | Smart home devices |
| Centers for Disease Control and Prevention [35] | 2022 | Quantitative study | Smart home devices |
| Santini et al. [36] | 2020 | Qualitative study | Smart technology |
| Cacioppo et al. [37] | 2014 | Quantitative study | Smart sensors to detect fall and physical activity, voice assistant, calendar reminder, home monitoring system |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, M.; Han, S.; Ghorbany, S.; Zhang, K. Healthy Aging in Place with the Aid of Smart Technologies: A Systematic Review. Encyclopedia 2024, 4, 1918-1932. https://doi.org/10.3390/encyclopedia4040125
Hu M, Han S, Ghorbany S, Zhang K. Healthy Aging in Place with the Aid of Smart Technologies: A Systematic Review. Encyclopedia. 2024; 4(4):1918-1932. https://doi.org/10.3390/encyclopedia4040125
Chicago/Turabian StyleHu, Ming, Soojin Han, Siavash Ghorbany, and Kai Zhang. 2024. "Healthy Aging in Place with the Aid of Smart Technologies: A Systematic Review" Encyclopedia 4, no. 4: 1918-1932. https://doi.org/10.3390/encyclopedia4040125
APA StyleHu, M., Han, S., Ghorbany, S., & Zhang, K. (2024). Healthy Aging in Place with the Aid of Smart Technologies: A Systematic Review. Encyclopedia, 4(4), 1918-1932. https://doi.org/10.3390/encyclopedia4040125








