Technological Resources for Hemodialysis Patients: A Scoping Review
Abstract
1. Introduction
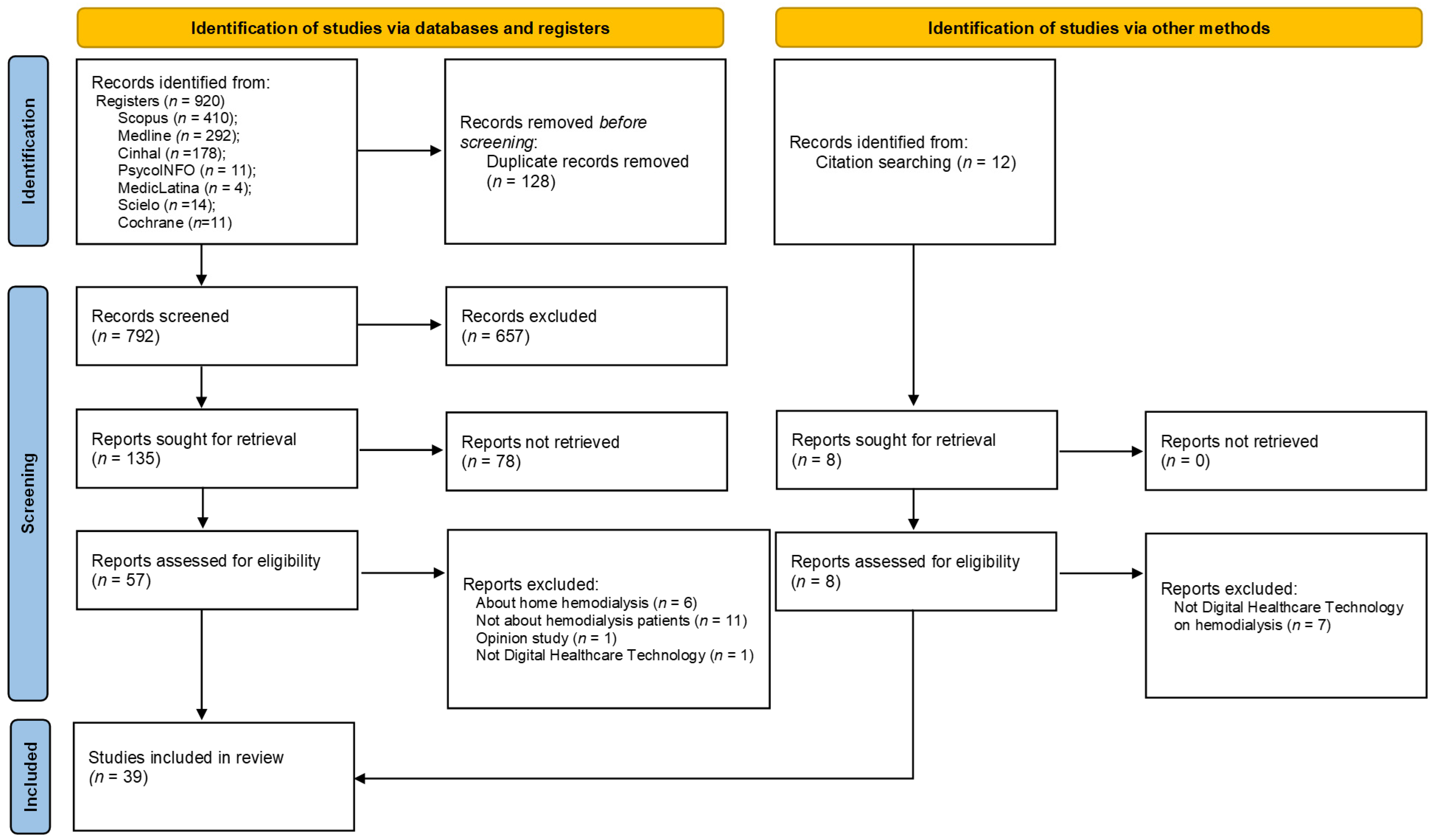
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Data Analysis
3. Results
3.1. Characteristics of the Included Studies
3.2. Characteristics of Participants
3.3. Characteristics Technologies Resources
3.4. Outcomes of the Technologies Resources
4. Discussion
4.1. Mobile Applications (Apps)
4.2. Virtual Reality
4.3. Exergames
4.4. Other Health Information Technologies
4.5. Impact of Technological Resources on Health Outcomes
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Search Strategies According to the Database
| Database | Research Strategy |
| MEDLINE | (((MH “Patients”) OR (MH “Patient Education as Topic”) OR (“Patient*”) OR (“Adult*”) OR (“Person”) OR (“Aged”)) AND ((MH “Educational Technology”) OR (MH “Digital Technology”) OR (MH “Games, Recreational”) OR (MH “Video Games”) OR (MH “Gamification”) OR (MH “Play and Playthings”) OR (MH “Mobile Applications”) OR (MH “Digital Technology”) OR (MH “Technology”) OR (MH “virtual reality”) OR (“Game*”) OR (“Gamification”) OR (“APPs”) OR (“Video Game*”) OR (“virtual reality”) OR (“Boardgame”) OR (“Digital Technology”) OR (“Mobile Application”) OR (“Web System”)) AND ((MH “Renal Dialysis”) OR (MH “Kidneys, Artificial”) OR (MH “Intermittent Renal Replacement Therapy”) OR (MM “Renal Insufficiency, Chronic”) OR (MH “hemodialysis Units, Hospital”) OR (MH “Renal Replacement Therapy”) OR (MH “Dialysis”) OR (“hemodialysis”) OR (“hemodialysis”) OR (“Renal Dialysis”) OR (“Renal Insufficiency”) OR (“Kidney Failure”))) |
| CINAHL | (((MH “Patients”) OR (MH “Patient Education”) OR (MH “Dialysis Patients”) OR (“Patient*”) OR (“Adult*”) OR (“Person”) OR (“Aged”)) AND ((MH “Educational Technology”) OR (MH “Digital Technology”) OR (MH “Games, Recreational”) OR (MH “Video Games”) OR (MH “Gamification”) OR (MH “Play and Playthings”) OR (MH “Mobile Applications”) OR (MH “Technology”) OR (MH “virtual reality”) OR (“Game*”) OR (“Gamification”) OR (“APPs”) OR (“Video Game*”) OR (“virtual reality”) OR (“Boardgame”) OR (“Digital Technology”) OR (“Mobile Application”) OR (“Web System”)) AND (((MH “hemodialysis”) OR (MH “hemodialysis Therapy (Iowa NIC)”) OR (MH “Dialysis Centers”) OR (MH “Renal Replacement Therapy”) OR (MH “Kidney Failure, Chronic”) OR (“hemodialysis”) OR (“hemodialysis”) OR (“Renal Dialysis”) OR (“Renal Insufficiency”) OR (“Kidney Failure”))) |
| PsycINFO | ((DE “PATIENTS”) OR (DE “PATIENT care”) OR (DE “PATIENT education”) OR (DE “hemodialysis patients”) OR (“Patient Education”) OR (“Dialysis Patients”) OR (“Patient*”) OR (“Adult*”) OR (“Person”) OR (“Aged”) AND (DE “GAMIFICATION”) OR (DE “GAMES”) OR (DE “GAMES & technology”) OR (DE “GAMES -- Therapeutic use”) OR (DE “EDUCATIONAL games”) OR (DE “VIDEO game software”) OR (DE “VIDEO games”) OR (DE “TECHNOLOGY”) OR (DE “EDUCATIONAL technology”) OR (“Educational Technology”) OR (“Digital Technology”) OR (“Games Recreational”) OR (“Video Games”) OR (“Gamification”) OR (“APPS”) OR (“Play and Playthings”) OR (“Mobile Applications”) OR (“Technology”) OR (“virtual reality”) OR (“Game*”) OR (“Gamification”) OR (“Video Game*”) OR (“virtual reality”) OR (“Boardgame”) OR (“Digital Technology”) OR (“Mobile Application”) OR (“Web System”)) AND ((DE “KIDNEY disease treatments”) OR (DE “RENAL replacement therapy”) OR (DE “HEMODIALYSIS”) OR (DE “KIDNEY disease treatments”) |
| Scopus | (TITLE-ABS-KEY ((“Patient Education”) OR (“Dialysis Patients”)) AND TITLE-ABS-KEY ((“Educational Technology”) OR (“Digital Technology”) OR (“Games Recreational”) OR (“Video Games”) OR (“Gamification”) OR (“APPS”) OR (“Play and Playthings”) OR (“Mobile Applications”) OR (“Technology”) OR (“virtual reality”) OR (“Game*”) OR (“Gamification”) OR (“Video Game*”) OR (“virtual reality”) OR (“Boardgame”) OR (“Digital Technology”) OR (“Mobile Application”) OR (“Web System”)) AND TITLE-ABS-KEY ((“Renal Dialysis”) OR (“Kidneys Artificial”) OR (“Renal Therapy”) OR (“hemodialysis Units”) OR (“Dialysis”) OR (“hemodialysis”) OR (“hemodialysis”) OR (“Renal Insufficiency”))) |
| SciELO | (((“Patient Education”) OR (“Dialysis Patients”)) AND ((“Educational Technology”) OR (“Digital Technology”) OR (“Games Recreational”) OR (“Video Games”) OR (“Gamification”) OR (“APPS”) OR (“Play and Playthings”) OR (“Mobile Applications”) OR (“Technology”) OR (“virtual reality”) OR (“Game*”) OR (“Gamification”) OR (“Video Game*”) OR (“virtual reality”) OR (“Boardgame”) OR (“Digital Technology”) OR (“Mobile Application”) OR (“Web System”)) AND ((“Renal Dialysis”) OR (“Kidneys Artificial”) OR (“Renal Therapy”) OR (“hemodialysis Units”) OR (“Dialysis”) OR (“hemodialysis”) OR (“hemodialysis”) OR (“Renal Insufficiency”))) |
| MedicLatina | (((“Patient Education”) OR (“Dialysis Patients”)) AND ((“Educational Technology”) OR (“Digital Technology”) OR (“Games Recreational”) OR (“Video Games”) OR (“Gamification”) OR (“APPS”) OR (“Play and Playthings”) OR (“Mobile Applications”) OR (“Technology”) OR (“virtual reality”) OR (“Game*”) OR (“Gamification”) OR (“Video Game*”) OR (“virtual reality”) OR (“Boardgame”) OR (“Digital Technology”) OR (“Mobile Application”) OR (“Web System”)) AND ((“Renal Dialysis”) OR (“Kidneys Artificial”) OR (“Renal Therapy”) OR (“hemodialysis Units”) OR (“Dialysis”) OR (“hemodialysis”) OR (“hemodialysis”) OR (“Renal Insufficiency”))) |
| Cochrane Library | (((“Patient Education”) OR (“Dialysis Patients”)) AND ((“Educational Technology”) OR (“Digital Technology”) OR (“Games Recreational”) OR (“Video Games”) OR (“Gamification”) OR (“APPS”) OR (“Play and Playthings”) OR (“Mobile Applications”) OR (“Technology”) OR (“virtual reality”) OR (“Game*”) OR (“Gamification”) OR (“Video Game*”) OR (“virtual reality”) OR (“Boardgame”) OR (“Digital Technology”) OR (“Mobile Application”) OR (“Web System”)) AND ((“Renal Dialysis”) OR (“Kidneys Artificial”) OR (“Renal Therapy”) OR (“hemodialysis Units”) OR (“Dialysis”) OR (“hemodialysis”) OR (“hemodialysis”) OR (“Renal Insufficiency”))) |
References
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024, 105, S117–S314. [Google Scholar] [CrossRef]
- Daugirdas, J.; Blake, P.; Ing, T. Handbook of Dialysis, 5th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2015. [Google Scholar]
- Luyckx, V.; Tonelli, M.; Stanifer, J. The global burden of kidney disease and the sustainable development goals. Bull. World Health Organ. 2018, 96, 414–422D. [Google Scholar] [CrossRef]
- Chironda, G.; Bhengu, B. Contributing Factors to Non-Adherence among Chronic Kidney Disease (CKD) Patients: A Systematic Review of Literature. Med. Clin. Rev. 2016, 2, 29. [Google Scholar] [CrossRef]
- Farinha, A. Symptom control in End Stage Renal Disease. Port. J. Nephrol. Hypertens. 2017, 31, 192–199. [Google Scholar]
- Sułkowski, L.; Rynkowski, W.; Szyszkowska, A.; Rezmerska, L.; Krajewska, M. Social Support and Quality of Life in Hemo-dialysis Patients: A Comparative Study with Healthy Controls. Healthcare 2024, 12, 1219. [Google Scholar] [CrossRef]
- Scott, I.; Scuffham, P.; Gupta, D.; Harch, T.; Borchi, J.; Richards, B. Going digital: A narrative overview of the effects, quality and utility of mobile apps in chronic disease self-management. Aust. Health Rev. 2020, 44, 62–82. [Google Scholar] [CrossRef]
- Diamantidis, C.J.; Becker, S. Health information technology (IT) to improve the care of patients with chronic kidney disease (CKD). BMC Nephrol. 2014, 15, 7. [Google Scholar] [CrossRef]
- Yang, Y.; Chen, H.; Qazi, H.; Morita, P. Intervention and Evaluation of Mobile Health Technologies in Management of Patients Undergoing Chronic Dialysis: Scoping Review. JMIR Mhealth Uhealth 2020, 8, e15549. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Strategy on Digital Health 2020–2025. 2021. Available online: https://apps.who.int/iris/bitstream/handle/10665/344249/9789240020924-eng.pdf (accessed on 9 June 2025).
- Moulaei, K.; Moulaei, R.; Bahaadinbeigy, K. Barriers and facilitators of using health information technologies by women: A scoping review. BMC Med. Inform. Decis. Mak. 2023, 23, 176. [Google Scholar] [CrossRef]
- Agarwal, P.; Gordon, D.; Griffith, J.; Kithulegoda, N.; Witteman, H.; Bhatia, R.; Kushniruk, A.; Borycki, E.; Lamothe, L.; Springall, E.; et al. Assessing the quality of mobile applications in chronic disease management: A scoping review. NPJ Digit. Med. 2021, 4, 46. [Google Scholar] [CrossRef]
- Kessel, R.; Wong, B.; Clemens, T.; Brand, H. Digital health literacy as a super determinant of health: More than simply the sum of its parts. Internet Interv. 2022, 27, 100500. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. eHealth. 2022. Available online: https://www.emro.who.int/health-topics/ehealth/ (accessed on 9 June 2025).
- World Health Organization. MHealth: Use of Appropriate Digital Technologies for Public Health. 2018. Available online: https://apps.who.int/gb/ebwha/pdf_files/WHA71/A71_20-en.pdf (accessed on 9 June 2025).
- Lee, H.J.; Son, Y.J. Prevalence and Associated Factors of Frailty and Mortality in Patients with End-Stage Renal Disease Undergoing hemodialysis: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 3471. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Flythe, J.E.; Watnick, S. Dialysis for Chronic Kidney Failure: A Review. JAMA 2024, 332, 1559–1573. [Google Scholar] [CrossRef] [PubMed]
- Siddique, A.B.; Krebs, M.; Alvarez, S.; Greenspan, I.; Patel, A.; Kinsolving, J.; Koizumi, N. Mobile Apps for the Care Management of Chronic Kidney and End-Stage Renal Diseases: Systematic Search in App Stores and Evaluation. JMIR Mhealth Uhealth 2019, 7, e12604. [Google Scholar] [CrossRef]
- Verweel, L.; Newman, A.; Michaelchuck, W.; Packham, T.; Goldstein, R.; Brooks, D. The effect of digital interventions on related health literacy and skills for individuals living with chronic diseases: A systematic review and meta-analysis. Int. J. Med. Inform. 2023, 177, 105114. [Google Scholar] [CrossRef]
- Aromataris, E.; Lockwood, C.; Porritt, K.; Pilla, B.; Jordan, Z. JBI Manual for Evidence Synthesis. JBI. 2024. Available online: https://synthesismanual.jbi.global (accessed on 9 June 2025). [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Martínez-Olmos, F.J.; Gómez-Conesa, A.A.; García-Testal, A.; Ortega-Pérez-de-Villar, L.; Valtueña-Gimeno, N.; Gil-Gómez, J.A.; Garcia-Maset, R.; Segura-Ortí, E. An intradialytic non-immersive virtual reality exercise programme: A crossover randomized controlled trial. Nephrol. Dial. Transplant. 2022, 37, 1366–1374. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Al-Ali, F.; Kang, G.E.; Hamad, A.I.; Ibrahim, R.A.; Talal, T.K.; Najafi, B. Application of Wearables to Facilitate Virtually Supervised Intradialytic Exercise for Reducing Depression Symptoms. Sensors 2020, 20, 1571. [Google Scholar] [CrossRef]
- Meléndez-Oliva, E.; Sánchez-Romero, E.A.; Segura-Ortí, E.; Gil-Gómez, J.A.; Soto-Goñi, X.A.; Poveda-Pagán, E.J. Effect of a virtual reality Exercise on Patients Undergoing Haemodialysis: A Randomised Controlled Clinical Trial Research Protocol. Int. J. Environ. Res. Public Health 2023, 20, 4116. [Google Scholar] [CrossRef]
- Smyth, W.; McArdle, J.; Body-Dempsey, J.; Manickam, V.; Swinbourne, A.; Lee, I.; Holdsworth, J.; Omonaiye, O.; Nagle, C. Immersive virtual reality in a northern Queensland haemodialysis unit: Study protocol for a cross-over randomized controlled feasibility trial (ACTRN12621000732886). Contemp. Clin. Trials Commun. 2022, 28, 100956. [Google Scholar] [CrossRef] [PubMed]
- Turoń-Skrzypińska, A.; Tomska, N.; Mosiejczuk, H.; Rył, A.; Szylińska, A.; Marchelek-Myśliwiec, M.; Ciechanowski, K.; Nagay, R.; Rotter, I. Impact of virtual reality exercises on anxiety and depression in hemodialysis. Sci. Rep. 2023, 13, 12435. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, R.; Burrows, B.; Browning, M.H.; Solai, K.; Fast, D.; Litbarg, N.O.; Wilund, K.R.; Moskowitz, J.T. Mindfulness-based virtual reality Intervention in hemodialysis Patients: A Pilot Study on End-user Perceptions and Safety. Kidney360 2021, 2, 435–444. [Google Scholar] [CrossRef]
- Maynard, L.G.; de Menezes, D.L.; Lião, N.S.; de Jesus, E.M.; Andrade, N.L.S.; Santos, J.C.D.; da Silva Júnior, W.M.; Bastos, K.; Barreto Filho, J.A.S. Effects of Exercise Training Combined with virtual reality in Functionality and Health-Related Quality of Life of Patients on hemodialysis. Games Health J. 2019, 8, 339–348. [Google Scholar] [CrossRef]
- Finco, M.G.; Najafi, B.; Zhou, H.; Hamad, A.; Ibrahim, R.; Al-Ali, F. Game-based intradialytic non-weight-bearing exercise training on gait speed and balance in older adults with diabetes: A single-blind randomized controlled trial. Sci. Rep. 2023, 13, 14225. [Google Scholar] [CrossRef]
- García-Testal, A.; Martínez-Olmos, F.J.; Gil-Gómez, J.A.; Villalón-Coca, J.; Ortiz-Ramón, R.; Cana-Poyatos, A.; García-Maset, R.; Segura-Ortí, E. Impact of an intradialysis virtual-reality-based exercise program on healthcare resources expenditure: A micro-costing analysis. BMC Nephrol. 2022, 23, 230. [Google Scholar] [CrossRef]
- Hudson, J.L.; Moss-Morris, R.; Game, D.; Carroll, A.; McCrone, P.; Hotopf, M.; Yardley, L.; Chilcot, J. Improving distress in dialysis (iDiD): A feasibility two-arm parallel randomised controlled trial of an online cognitive behavioural therapy intervention with and without therapist-led telephone support for psychological distress in patients undergoing haemodialysis. BMJ Open 2016, 6, e011286. [Google Scholar] [CrossRef]
- Santana, C.; Freitas, A.; Oliveira Barreto, G.; Sousa De Avelar, I.; Mazaro-Costa, R.; Bueno, G.; Ribeiro, D.; Damasceno Silva, G.; Naghettini, A. Serious Game on a Smartphone for Adolescents Undergoing hemodialysis: Development and Evaluation. JMIR Serious Games 2020, 8, e17979. [Google Scholar] [CrossRef]
- Hayashi, A.; Yamaguchi, S.; Waki, K.; Fujiu, K.; Hanafusa, N.; Nishi, T.; Tomita, H.; Kobayashi, H.; Fujita, H.; Kadowaki, T.; et al. Testing the feasibility and usability of a novel smartphone-based self-management support system for dialysis patients: A pilot study. JMIR Res. Protoc. 2017, 6, e63. [Google Scholar] [CrossRef]
- Hosseini, A.; Jackson, A.C.; Chegini, N.; Dehghan, M.F.; Mazloum, D.; Haghani, S.; Bahramnezhad, F. The effect of an educational app on hemodialysis patients’ self-efficacy and self-care: A quasi-experimental longitudinal study. Chronic Illn. 2023, 19, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, R.; Yabe, H.; Hibino, T.; Morishita, S.; Watanabe, M.; Nishioka, K.; Ishikawa, H. The study of exercise therapy using a virtual reality system on healthy subjects assuming hospital use and intradialytic exercise. Nagoya J. Med. Sci. 2023, 85, 490–503. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.H.; Li, D. Understanding how virtual reality forest experience promote physiological and psychological health for patients undergoing hemodialysis. Front. Psychiatry 2022, 13, 1007396. [Google Scholar] [CrossRef]
- Bers, M.U.; Gonzalez-Heydrich, J.; Demaso, D.R. Use of a computer-based application in a pediatric hemodialysis unit: A pilot study. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Segura-Ortí, E.; Pérez-Domínguez, B.; Ortega-Pérez de Villar, L.; Meléndez-Oliva, E.; Martínez-Gramage, J.; García-Maset, R.; Gil-Gómez, J.A. Virtual reality exercise intradialysis to improve physical function: A feasibility randomized trial. Scand. J. Med. Sci. Sports 2019, 29, 89–94. [Google Scholar] [CrossRef]
- Feizalahzadeh, H.; Tafreshi, M.Z.; Moghaddasi, H.; Farahani, M.A.; Khosrovshahi, H.T.; Zareh, Z.; Mortazavi, F. Development and validation of a theory-based multimedia application for educating Persian patients on hemodialysis. Comput. Inform. Nurs. 2014, 32, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Agapito, G.; Simeoni, M.; Calabrese, B.; Caré, I.; Lamprinoudi, T.; Guzzi, P.; Pujia, A.; Fuiano, G.; Cannataro, M. DIETOS: A dietary recommender system for chronic diseases monitoring and management. Comput. Methods Programs Biomed. 2018, 153, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Chettati, M.; Bouchemla, N.; Fadili, W.; Laouad, I. Use of the TestObs mobile application for the evaluation of therapeutic adherence in chronic hemodialysis patients: Technological monitoring model of treatment adherence and determining factors. Nephrol. Ther. 2022, 18, 557–564. [Google Scholar] [CrossRef]
- Chiang, Y.; Chang, Y.; Lin, S.; Lin, C.; Hsu, P.; Hsu, Y.; Wu, T. Effects of Individualized Dietary Phosphate Control Program With a Smartphone Application in hemodialysis Patients in Taiwan. Biol. Res. Nurs. 2021, 23, 375–381. [Google Scholar] [CrossRef]
- Cho, H.; Sohng, K. The effect of a virtual reality exercise program on physical fitness, body composition, and fatigue in hemodialysis patients. J. Phys. Ther. Sci. 2014, 26, 1661–1665. [Google Scholar] [CrossRef]
- Chou, H.; Chen, S.; Yen, T.; Han, H. Effect of a virtual reality-Based Exercise Program on Fatigue in Hospitalized Taiwanese End-Stage Renal Disease Patients Undergoing hemodialysis. Clin. Nurs. Res. 2020, 29, 368–374. [Google Scholar] [CrossRef]
- Connelly, K.; Siek, K.; Chaudry, B.; Jones, J.; Astroth, K.; Welch, J. An offline mobile nutrition monitoring intervention for varying-literacy patients receiving hemodialysis: A pilot study examining usage and usability. J. Am. Med. Inform. Assoc. 2012, 19, 705–712. [Google Scholar] [CrossRef]
- Costa, F.; Delage, P.; Santana, M.; Nascimento, M.; Teixeira, E. Alfa test of a gamified technology for children and adolescents in hemodialysis. Anna Nery Sch. J. Nurs. Esc. Anna Nery Rev. Enferm. 2021, 25, e20200514. [Google Scholar] [CrossRef]
- Dingwall, K.; Sweet, M.; Cass, A.; Hughes, J.; Kavanagh, D.; Howard, K.; Barzi, F.; Brown, S.; Sajiv, C.; Majoni, S.; et al. Effectiveness of Wellbeing Intervention for Chronic Kidney Disease (WICKD): Results of a randomised controlled trial. BMC Nephrol. 2021, 22, 136. [Google Scholar] [CrossRef]
- Khoury, C.; Crutzen, R.; Schols, J.; Halfens, R.; Karavetian, M. A Dietary Mobile App for Patients Undergoing hemodialysis: Prospective Pilot Study to Improve Dietary Intakes. J. Med. Internet Res. 2020, 22, e17817. [Google Scholar] [CrossRef]
- Hernandez, R.; Wilund, K.; Solai, K.; Tamayo, D.; Fast, D.; Venkatesan, P.; Lash, J.; Lora, C.; Martinez, L.; Alemañy, G.; et al. Positive Psychological Intervention Delivered Using virtual reality in Patients on hemodialysis with Comorbid Depression: Protocol and Design for the Joviality Randomized Controlled Trial. JMIR Res. Protoc. 2023, 12, e45100. [Google Scholar] [CrossRef]
- Min, Y.; Park, M. Effects of a Mobile-App-Based Self-Management Support Program For Elderly hemodialysis Patients. Healthc. Inform. Res. 2020, 26, 93–103. [Google Scholar] [CrossRef]
- Minatodani, D.; Berman, S. Home telehealth in high-risk dialysis patients: A 3-year study. Telemed. e-Health 2013, 19, 520–522. [Google Scholar] [CrossRef]
- Ong, S.; Jassal, S.; Miller, J.; Porter, E.; Cafazzo, J.; Seto, E.; Thorpe, K.; Logan, A. Integrating a Smartphone-Based Self-Management System into Usual Care of Advanced CKD. Clin. J. Am. Soc. Nephrol. 2016, 11, 1054–1062. [Google Scholar] [CrossRef]
- Pack, S.; Lee, J. Randomised controlled trial of a smartphone application-based dietary self-management program on haemodialysis patients. J. Clin. Nurs. 2021, 30, 840–848. [Google Scholar] [CrossRef] [PubMed]
- Park, O.; Kim, S. Integrated self-management program effects on hemodialysis patients: A quasi-experimental study. Jpn. J. Nurs. Sci. 2019, 16, 396–406. [Google Scholar] [CrossRef] [PubMed]
- Ren, Q.; Lian, M.; Liu, Y.; Thomas-Hawkins, C.; Zhu, L.; Shen, Q. Effects of a transtheoretical model-based WeChat health education programme on self-management among haemodialysis patients: A longitudinal experimental intervention study. J. Adv. Nurs. 2019, 75, 3554–3565. [Google Scholar] [CrossRef] [PubMed]
- Rocco, M.; Rigaud, M.; Ertel, C.; Russell, G.; Zemdegs, J.; Vecchio, M. Fluid Intake Management in Maintenance hemodialysis Using a Smartphone-Based Application: A Pilot Study. Kidney Med. 2023, 5, 100703. [Google Scholar] [CrossRef] [PubMed]
- Saadatifar, B.; Sharifi, S.; Faghihi, H.; Googhary, N. Effect of mHealth Training on Treatment Adherence in hemodialysis Patients. Med. Surg. Nurs. J. 2022, 11, e134851. [Google Scholar] [CrossRef]
- Teong, L.; Khor, B.; Ng, H.; Sahathevan, S.; Purba, K.; Narayanan, S.; Gafor, A.; Goh, B.; Bee, B.; Yahya, R.; et al. Effectiveness of a Nutritional Mobile Application for Management of Hyperphosphatemia in Patients on hemodialysis: A Multicenter Open-Label Randomized Clinical Trial. J. Pers. Med. 2022, 12, 961. [Google Scholar] [CrossRef]
- Khah, M.; Farsi, Z.; Sajadi, S. Comparing the effects of mHealth application based on micro-learning method and face-to-face training on treatment adherence and perception in haemodialysis patients: A randomised clinical trial. BMJ Open 2023, 13, e071982. [Google Scholar] [CrossRef] [PubMed]
- Willis, M.; Hein, L.; Hu, Z.; Saran, R.; Argentina, M.; Bragg-Gresham, J.; Krein, S.; Gillespie, B.; Zheng, K.; Veinot, T. Usability evaluation of a tablet-based intervention to prevent intradialytic hypotension in dialysis patients during in-clinic dialysis: Mixed methods study. JMIR Hum. Factors 2021, 8, e26012. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Kosa, S.; Monize, J.; D’Souza, M. Nutritional Mobile APPlications for CKD Patients: Systematic Review. Kidney Int. Rep. 2018, 4, 399–407. [Google Scholar] [CrossRef]
- Russell, C.; Zigan, C.; Wozniak, K.; Soni, K.; Gallant, K.; Friedman, A. A Systematic Review and Qualitative Analysis of Existing Dietary Mobile Applications for People With Chronic Kidney Disease. J. Ren. Nutr. 2022, 32, 382–388. [Google Scholar] [CrossRef]
- Stevenson, J.K.; Campbell, Z.C.; Webster, A.C. E-Health interventions for people with chronic kidney disease. Cochrane Database Syst. Rev. 2019, 8, CD012379. [Google Scholar] [CrossRef]
- Campbell, J.; Porter, J. Dietary mobile apps and their effect on nutritional indicators in chronic renal disease: A systematic review. Nephrology 2015, 20, 744–751. [Google Scholar] [CrossRef]
- Chen, J.F.; Wu, L.L.; Chou, S.C. Effects of Journaling Dietary Intake App on the Health Outcomes of Chronic Kidney Disease Stage 3B-5. In Proceedings of the 2016 49th Hawaii International Conference on System Sciences, Koloa, HI, USA, 5–8 January 2016; pp. 3379–3388. [Google Scholar] [CrossRef]
- Shen, H. Electronic Health Self-Management Interventions for Patients With Chronic Kidney Disease: Systematic Review of Quantitative and Qualitative Evidence. J. Med. Internet Res. 2019, 21, e12384. [Google Scholar] [CrossRef] [PubMed]
- Ventura, S.; Brivio, E.; Riva, G.; Baños, R.M. Immersive versus non-immersive experience: Exploring the feasibility of memory assessment through 360° technology. Front. Psychol. 2019, 10, 2509. [Google Scholar] [CrossRef]
- Burrai, F.; Othman, S.; Brioni, E.; Silingardi, M.; Micheluzzi, V.; Luppi, M.; Apuzzo, L.; La Manna, G. Virtual reality in dialysis: A new perspective on care. J. Ren. Care 2018, 44, 195–196. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, C.S.; Magalhães, B.; Gomes, J.A.; Santos, C. Exergames to improve Rehabilitation after Anterior Cruciate Ligament Injury: Systematic review and GRADE evidence synthesis. Int. J. Orthop. Trauma Nurs. 2022, 44, 100917. [Google Scholar] [CrossRef] [PubMed]
- Perez, F.M.; Henrique, P.P.; Marchi, A.C. Kinesiotherapeutic intervention protocol with exergames for muscle strength and balance in elderly—A systematic literature review. Res. Soc. Dev. 2021, 10, e113101321063. [Google Scholar] [CrossRef]
- Hu, H.; Liu, X.; Chau, P.H.; Choi, E.P.H. Effects of intradialytic exercise on health-related quality of life in patients undergoing maintenance haemodialysis: A systematic review and meta-analysis. Qual. Life Res. 2022, 31, 1915–1932. [Google Scholar] [CrossRef]
- Sabate, E. Adherence to Long-Term Therapies: Evidence for Action; Report of WHO Adherence to Longterm Therapies Project; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Martins, A.R.; Ferreira, M.C.; Fernandes, C.S. Emerging technologies for supporting patients during hemodialysis: A scoping review. Int. J. Med. Inform. 2024, 181, 105664. [Google Scholar] [CrossRef]
- Shahgholian, N.; Yousefi, H. The lived experiences of patients undergoing hemodialysis with the concept of care: A phenomenological study. BMC Nephrol. 2018, 19, 338. [Google Scholar] [CrossRef] [PubMed]
- Sukartini, T.; Efendi, F.; Putri, N.S. A phenomenological study to explore patient experience of fluid and dietary restrictions imposed by hemodialysis. J. Vasc. Nurs. 2022, 40, 105–111. [Google Scholar] [CrossRef]
- Kim, S.; Lee, H.Z. The lived self-care experiences of patients undergoing long-term haemodialysis: A phenomenological study. Int. J. Environ. Res. Public Health 2023, 20, 4690. [Google Scholar] [CrossRef]
- Murali, K.M.; Mullan, J.; Roodenrys, S.; Hassan, H.C.; Lambert, K.; Lonergan, M. Strategies to improve dietary, fluid, dialysis or medication adherence in patients with end stage kidney disease on dialysis: A systematic review and meta-analysis of randomized intervention trials. PLoS ONE 2019, 14, e0211479. [Google Scholar] [CrossRef] [PubMed]
- Bonner, A.; Gillespie, K.; Campbell, K.L.; Corones-Watkins, K.; Hayes, B.; Harvie, B.; Kelly, J.T.; Havas, K. Evaluating the prevalence and opportunity for technology use in chronic kidney disease patients: A cross-sectional study. BMC Nephrol. 2018, 19, 28. [Google Scholar] [CrossRef] [PubMed]
- Sobrinho, A.; da Silva, L.D.; Perkusich, A.; Pinheiro, M.; Cunha, P. Design and evaluation of a mobile application to assist the self-monitoring of the chronic kidney disease in developing countries. BMC Med. Inform. Decis. Mak. 2018, 18, 7. [Google Scholar] [CrossRef] [PubMed]
- Gulliksen, J.; Göransson, B.; Boivie, I.; Blomkvist, S.; Persson, J.; Cajander, A. Key principles for user-centred systems design. Behav. Inf. Technol. 2003, 22, 397–409. [Google Scholar] [CrossRef]

| ID. | Author(s), Year, and Country | Objective | Study Design | Participants | Resource Type | Tech Objective | Intervention Time | Assessment Tools | Results |
|---|---|---|---|---|---|---|---|---|---|
| E1 | Martínez-Olmos et al. (2022) [22] Spain | Evaluate whether a virtual reality exercise program during hemodialysis improves walking speed. | RCT | 56 adult patients on hemodialysis | Exergame | Physical exercise practice | 12 weeks | STS; OLS; SPPB; 6MWT; TUG | Increased walking speed; improved One-Leg Stance Test results and Sit-to-Stand Test-60 results. Decreased Timed Up-and-Go results; reduced execution time in Sit-to-Stand Test 5 and 10, indicating improvement. |
| E2 | Zhou et al. (2020) [23] Qatar | Assess the feasibility, acceptability, and effectiveness of this program in alleviating depressive symptoms. | Clinical trial | 73 adult patients on hemodialysis | Exergame | Physical exercise practice | 4 weeks | Demographic/health info; FES-I; MMSE; ABI; VPT; CES-D | The number of participants at risk for clinical depression decreased in scores on the Center for Epidemiologic Studies Depression Scale. |
| E3 | Meléndez-Oliva et al. (2023) [24] Spain | To evaluate the effectiveness of a non-immersive virtual reality intradialytic exercise program on inflammatory markers, and the impact on functional capacity and psychological well-being. | Clinical trial | 80 adult patients on hemodialysis | Non-immersive virtual reality | Physical exercise practice | 12 weeks | SPPB; 6MWT; STS; TUG; CAIQ-RDQ; BDI-II; STAI | Both exercise groups (non-immersive VR and static pedal) are anticipated to experience a reduction in inflammatory marker levels, along with improvements in functional capacity and psychological well-being. |
| E4 | Smyth et al. (2022) [25] Australia | Compare participant adherence to hemodialysis regimens. | RCT | 40 adult patients on hemodialysis | Immersive virtual reality | Immersive experiences | 4 weeks | Attendance rates; Adherence proportions; AQoL; UES-SF | The outcomes will be assessed based on participants’ attendance at scheduled dialysis sessions. |
| E5 | Turoń-Skrzypińska et al. (2023) [26] Poland | Assess the impact of regular physical exercise using non-immersive virtual reality on the occurrence of anxiety and depression symptoms. | RCT | 85 adult patients on hemodialysis | Non-immersive virtual reality | Physical exercise practice | March 2021 to February 2022 | Borg; BDI; GAD-7; Demographic/health/lifestyle questionnaire | Reduction in depressive symptoms. Decrease in the frequency of anxiety and depression symptoms. |
| E6 | Hernandez et al. (2021) [27] USA | To assess whether virtual reality aggravates symptoms commonly associated with hemodialysis. | Pilot study | 20 adult patients on hemodialysis | Immersive virtual reality | Meditation/Awareness Program | 25 min on two occasions | Sociodemographic/health survey; SSQ; IPQ; SUS | Patients found the program enjoyable and easy to use. During the first use, a significant reduction in symptoms such as fatigue, nausea, oculomotor issues, and disorientation, was observed. |
| E7 | Maynard et al. (2019) [28] Brazil | Examine the effects of combining physical exercise and virtual reality on the functional abilities and quality of life in individuals receiving hemodialysis. | RCT | 45 adult patients on hemodialysis | Non-immersive virtual reality | Physical exercise practice | 12 weeks | TUG; Gait speed; DASI; CES-D; KDQOL-SF | Marked enhancement in functional capacity. Improvements in the Timed Up-and-Go test and the Duke Activity Status Index. Significant changes in quality-of-life metrics. Reduction in depressive symptoms. |
| E8 | Finco et al. (2023) [29] Qatar | Assess the impact of an exergame program on gait speed and postural control in elderly patients with diabetes undergoing hemodialysis. | RCT | 70 adult patients on hemodialysis | Exergame | Physical exercise practice | 4 weeks | Ankle/hip oscillation; Gait speed; Single-task walking; Balance (BalanSens™ semi-tandem test) | Gait speed enhancement and postural sway stabilization in elderly individuals undergoing hemodialysis. |
| E9 | García-Testal et al. (2022) [30] Spain | Assess variations in healthcare resource utilization and micro-costs among patients undergoing hemodialysis. | RCT | 33 adult patients on hemodialysis | Non-immersive virtual reality | Physical exercise practice | 12 weeks | Lab tests; Radiology exams; Outpatient consults; ED services; Hospitalizations | Healthcare resource expenses significantly declined following participation in an intradialytic virtual reality exercise program. Micro-cost reductions were observed in laboratory tests, radiological exams, and outpatient consultations. |
| E10 | Hudson et al. (2016) [31] United Kingdom | Assess the feasibility and acceptability of implementing a universal screening process for patients undergoing hemodialysis. | Pilot study | 60 adult patients on hemodialysis | Website | Improve psychological distress | 6 weeks | PHQ-9; GAD-7; EQ-5D; BIPQ | The outcomes cover feasibility and acceptability, as well as descriptive data on recruitment, randomization, retention, and treatment adherence rates. |
| E11 | Santana et al. (2020) [32] Brazil | Design a game that motivates adolescents undergoing hemodialysis to practice self-care. | Pilot study | 7 adolescents on hemodialysis | App | Care of a character in the context of hemodialysis | 60 days | SSIs; OBSs | The game served as a motivating factor for the participants, who gained insights into the conditions that could lead to potential hospitalizations. |
| E12 | Hayashi et al. (2017) [33] Japan | To evaluate the feasibility and usability of the SMART-D system. | Pilot study | 20 adult patients on hemodialysis | App | Disease management | 2 weeks | t-test; QoL-Q; DQ | No significant differences in interdialytic weight gain, serum potassium levels, and serum phosphorus levels. The Social Functioning score showed a notable improvement, while the other scores from the Quality-of-Life Questionnaire remained stable. |
| E13 | Hosseini et al. (2023) [34] Iran | Assessing the effect of patient education in hemodialysis via an application on patients’ self-care and self-efficacy. | Quasi-experimental study | 59 adult patients on hemodialysis | App | Self-efficacy and self-care | October 2020 to March 2021 | SCQ; SEQ; DQ | The average scores for self-care and self-efficacy assessed after the intervention were significantly higher than those recorded before the intervention, demonstrating the application’s effectiveness. |
| E14 | Takahashi et al. (2023) [35] Japan | To summarize basic data on the safety and efficacy of the system in healthy individuals, providing a foundation for future applications in patients. | Pilot study | 15 university students | Immersive virtual reality | Physical exercise practice | Not applicable | DQ; SSQ; BP/HR; Borg; BMI | This study demonstrated that virtual reality does not induce motion sickness or virtual interruptions and results in higher workload as measured by heart rate during exercise in VR conditions. |
| E15 | Hsieh & Li (2022) [36] Taiwan | Examine alterations in physiological health outcomes and explore psychological responses in dialysis patients after experiencing 360-degree nature videos through immersive virtual reality. | Clinical trial | 24 adult patients on hemodialysis | Immersive virtual reality | Immersive experience | 3 weeks | SSIs; PQs; PAD; HR; ECG | The virtual reality experience had a positive impact on heart rate. This intervention reduced stress during hemodialysis, lowering sympathetic nervous system activity and diminishing negative emotions. |
| E16 | Bers et al. (2003) [37] USA | Create technological resources to assist families dealing with pediatric illnesses. | Pilot study | 7 children on hemodialysis | Computer app (video game) | Disease management | 3 months | SSIs | Patients described Zora as a valuable tool for discreetly communicating with one another during the public hemodialysis setting. It allowed some individuals to share personal concerns without the pressure of face-to-face or real-time discussions. |
| E17 | Segura-Ortí et al. (2019) [38] Spain | To evaluate the practicality of implementing a non-immersive virtual reality exercise intervention during intradialysis sessions. | Pilot study | 18 adult patients on hemodialysis | Non-immersive virtual reality | Physical exercise practice | 16 weeks | STS; 6MWT; GS; HRT | Sit-to-Stand test significantly improved over time; gait speed increased. |
| E18 | Feizalahzadeh et al. (2014) [39] Iran | To outline the development and validation steps for evidence-based multimedia education apps, guided by Mayer’s Cognitive Theory, for Persian patients undergoing hemodialysis. | Pilot study | 14 adult patients on hemodialysis 12 healthcare professionals in hemodialysis | App | Health education | Not applicable | SSIs | The app was created through an iterative design process, including input from hemodialysis patients and experts. The study’s results showed that it can enhance the educational experience for patients undergoing hemodialysis. |
| E19 | Agapito et al. (2018) [40] Italy | Improving the quality of life of healthy individuals and people with chronic diseases related to nutrition. | Pilot study | 20 healthy individuals and 20 dialysis adult patients | App | Diet and weight management | 3 months | Questionnaires | DIETOS has high specificity and sensitivity, allowing the determination of a user’s health profile and providing personalized nutritional recommendations that best match the individual’s health status. |
| E20 | Chettati et al. (2022) [41] Morocco | Evaluate adherence to long-term prescribed medications and determine the main factors influencing adherence. | Descriptive prospective study | 90 adult patients on hemodialysis | App | Medication adherence | 6 months | Questionnaires | The statistically significant factors influencing adherence were the number of pills taken per day and the presence of a vision problem. |
| E21 | Chiang et al. (2021) [42] Taiwan | Evaluate the impact of an app-assisted care program on dietary phosphate control in patients undergoing regular hemodialysis. | Quasi-experimental study | 60 adult patients on hemodialysis (30 ACP—App-assisted caring program) (30 SCP—Standard education) | App | Dietary management | 3 months | SES; KTs | The study demonstrated that using the app increased patients’ self-care efficacy and knowledge about dietary phosphate control, leading to a significant decrease in serum phosphate levels compared to the control group. |
| E22 | Cho & Sohng (2014) [43] South Korea | Investigate the effects of a virtual reality exercise program on physical fitness, body composition, and fatigue in hemodialysis patients. | RCT | 46 adult patients on hemodialysis (23 intervention group, 23 control group) | Non-immersive virtual reality | Physical exercise practice | 8 weeks | PFA; InBody S10; VAS | The study showed that the intervention group experienced significant improvements in dorsal strength, leg strength, and flexibility. Skeletal muscle mass and balance also increased. The exercise group exhibited a drastic reduction in fatigue levels compared to the control group. |
| E23 | Chou et al. (2020) [44] Taiwan | Evaluate the effect of a virtual reality-based exercise program on fatigue in patients with end-stage renal disease undergoing hemodialysis. | Quasi-experimental study | 64 adult patients on hemodialysis (32 intervention group, 32 control group). | Non-immersive virtual reality | Physical exercise practice | 4 weeks | NFSHD; Q-PCC | Patients in the experimental group showed significantly lower overall fatigue levels, reduced vigor and motivation, less distress, and better mood control. Additionally, they had higher hemoglobin levels compared to the control group. |
| E24 | Connelly et al. (2012) [45] USA | Design and evaluation of the Dietary Intake Monitoring Application (DIMA) to assist hemodialysis patients with varying literacy levels in adhering to prescribed dietary regimes. | Pilot study | 18 adult patients on hemodialysis | App | Dietary management | 6 weeks | Qs; IDWLs | The participants were able to use the DIMA successfully. However, they faced difficulties in using the barcode scanner. The most commonly used feature in DIMA was the ability to view previous meals, which served as the primary reflective mechanism for users. |
| E25 | Costa et al. (2021) [46] Brazil | Presenting the alpha test of the gamified technology prototype, Nefro Hero®, focusing on the Health-Related Quality of Life (HRQoL) of pediatric patients undergoing hemodialysis treatment. | Qualitative study | 8 pediatric patients, ages 8 to 16, undergoing hemodialysis | Video game | Quality of life | 3 months | DISABKIDS HRQoL; FDs; BSs | Improvements were identified in the mental domain of HRQoL for the patients. The enhancement in emotional scores demonstrated the potential of gamification in possibly re-framing aspects related to treatment, thereby strengthening resilience in the patients. |
| E26 | Dingwall et al. (2021) [47] Australia | Examine the effectiveness of the Stay Strong app in improving psychological distress, depressive symptoms, quality of life, and adherence to dialysis. | Pilot study | 156 adult patients on hemodialysis | App | Improvement in psychological distress | 3 months | K10; PHQ-9; EQ-5D | The results suggest that using apps for treatment may improve the well-being of individuals undergoing dialysis. |
| E27 | Khoury et al. (2020) [48] United Arab Emirates | Estimate the potential effectiveness of a dietary intervention using a person-centered, theory-based smartphone app. | Pilot study | 23 adult patients on hemodialysis | App | Dietary management | 2 weeks | Biochemical parameters | The average protein intake increased. The intake of dietary minerals remained unchanged, except for sodium, which decreased. There were no significant changes in the average serum levels of phosphorus, potassium, or albumin. |
| E28 | Hernandez et al. (2023) [49] USA | Test the feasibility and preliminary efficacy of a positive psychological intervention. | RCT | 84 adult patients on hemodialysis with depression | Virtual reality | Reduction in depressive symptoms | 5 weeks | BDI-II; PROMIS; PSS; KDQOL-SF; EMRs | This trial will be the first to test a customized virtual reality software to provide a positive psychological intervention aimed at reducing depressive symptoms. |
| E29 | Min & Park (2020) [50] South Korea | Identify the effects of a self-management program based on a mobile application. | RCT | 56 adult patients on hemodialysis (28 intervention group, 28 control group). | APP | Self-efficacy | 10 weeks | Q-AB/PN/SE/DCs; CRs | Patient adherence behavior increased. Self-efficacy improved after 10 weeks of intervention. No significant differences in serum phosphate and potassium levels were observed. |
| E30 | Minatodani & Berman (2013) [51] USA | Evaluate a telehealth pilot project in terms of improved health outcomes and significant cost savings. | Pilot study | 99 adult patients on hemodialysis (43 intervention group, 56 control group). | Remote technology | Telemonitoring | 3 years | HOSP-N; ERV-N; HOSP-D; PMs (BP, HR, W, SpO2, BG) | Costs associated with hospital admissions and emergency visits were significantly lower. The number of medical and technical incidents decreased drastically, leading to fewer nurse contacts. |
| E31 | Ong et al. (2016) [52] Canada | Evaluate the acceptability of this enhanced smartphone system in the management of patients with advanced CKD and examine changes in various clinical parameters. | Pilot study | 47 adult patients on hemodialysis | App | Self-management | 6 months | Eval-N; Eval-C/R; SSIs; CD | The app simplified important tasks and supported patients’ real-time decision-making through embedded algorithms for each behavioral component. |
| E32 | Pack & Lee (2021) [53] South Korea | Develop a dietary self-management program for hemodialysis patients based on a smartphone app and examine its effects on biochemical markers. | Prospective study | 75 adult patients on hemodialysis (37 intervention group, 38 control group). | App | Dietary management | 12 weeks | CD; Qs; KDQOL-SF | In the experimental group, phosphate levels decreased to within the normal range, in contrast with the control group. Self-efficacy and quality of life improved significantly over time among hemodialysis patients. |
| E33 | Park & Kim (2019) [54] South Korea | Evaluate the effects of an integrated self-management program using a mobile app. | Quasi-experimental study | 84 adult patients on hemodialysis (42 intervention group, 42 control group). | App | Self-management | 8 weeks | CPRB; IDWG/DW; Serum K + /P; DCs | Scores related to self-efficacy and treatment adherence were significantly higher. Interdialytic weight gain and dry weight significantly decreased. |
| E34 | Ren et al. (2019) [55] China | Develop and evaluate the effects of a health education program using WeChat. | Clinical trial | 85 adult patients on hemodialysis (49 intervention group, 36 control group). | Digital platform (WeChat) | Self-management | 3 months | SMS-HD; CPKQ; CDSES; DCs | Patients in the intervention group showed a significant increase in self-management scores, knowledge about hemodialysis, and self-efficacy immediately following the health education program via WeChat. |
| E35 | Rocco et al. (2023) [56] USA | Evaluate the utility and safety of a mobile application (app) that allows self-monitoring of daily fluid intake. | Pilot study | 25 adult patients on hemodialysis | App | Self-management | 3 months | SIs; CD; AppUse% | 61% of participants experienced a decrease in interdialytic weight gain while using the app. |
| E36 | Saadatifar et al. (2022) [57] Iran | Examine the effect of mHealth training on treatment adherence in hemodialysis patients in Zahedan. | Quasi-experimental study | 80 adult patients on hemodialysis | App | Adherence | 3 months | DIF; MLQ; ESRD-AQ | Contrary to expectations, the adherence scores of the control group, which received routine training from healthcare staff, were higher than those of the group that received mHealth training. |
| E37 | Teong et al. (2022) [58] Malaysia | Determine the effectiveness of a phosphate mobile application (PMA) in hemodialysis (HD) patients with hyperphosphatemia. | RCT | 74 adult patients on hemodialysis (38 intervention group, 36 control group). | App | Dietary management | 12 weeks | BP; Q; IDIs; MMAS-4; SD | Hemodialysis patients with hyperphosphatemia using the app experienced reductions in serum phosphate levels and dietary phosphate intake, along with improved knowledge of phosphate and increased adherence to phosphate binder medication. |
| E38 | Khah et al. (2023) [59] Iran | Compare the effects of a mobile health (mHealth) application based on microlearning with in-person training on treatment adherence and perception. | RCT | 70 adult patients on hemodialysis (35 intervention group, 35 control group) | App | Treatment adherence | 12 weeks | ESRD-AQ | The results showed that the overall effect of the mHealth method was superior to that of in-person education in treatment adherence. The lower average scores obtained by hemodialysis patients before the intervention were associated with water and dietary restrictions, respectively. |
| E39 | Willis et al. (2021) [60] USA | Test the usability of a tablet-based intervention that includes theory-informed educational modules and mentoring. | Pilot study | 14 adult patients on hemodialysis | App | Health education | Not applicable | SSIs | Four general restrictions were identified when designing for dialysis patients: touch dexterity and interface navigation, movement limitations and device positioning during dialysis, readability, and vision challenges for older patients due to small text size. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martins, A.R.; Moreira, M.T.; Lima, A.; Ferreira, S.; Campos Ferreira, M.; Fernandes, C.S. Technological Resources for Hemodialysis Patients: A Scoping Review. Kidney Dial. 2025, 5, 44. https://doi.org/10.3390/kidneydial5030044
Martins AR, Moreira MT, Lima A, Ferreira S, Campos Ferreira M, Fernandes CS. Technological Resources for Hemodialysis Patients: A Scoping Review. Kidney and Dialysis. 2025; 5(3):44. https://doi.org/10.3390/kidneydial5030044
Chicago/Turabian StyleMartins, Ana Rita, Maria Teresa Moreira, Andreia Lima, Salomé Ferreira, Marta Campos Ferreira, and Carla Silva Fernandes. 2025. "Technological Resources for Hemodialysis Patients: A Scoping Review" Kidney and Dialysis 5, no. 3: 44. https://doi.org/10.3390/kidneydial5030044
APA StyleMartins, A. R., Moreira, M. T., Lima, A., Ferreira, S., Campos Ferreira, M., & Fernandes, C. S. (2025). Technological Resources for Hemodialysis Patients: A Scoping Review. Kidney and Dialysis, 5(3), 44. https://doi.org/10.3390/kidneydial5030044









