Optimizing Clinical Nursing Interventions for Hemodialysis Patients with Arteriovenous Fistula
Abstract
1. Introduction
2. The Necessity of Clinical Nurses’ Education on AVFs/AVG Management
| Author, Year | Design | Sample Size | Received Educational Program | Experimental Tools | Main Results |
|---|---|---|---|---|---|
| Abou Elazayiem Bayumi et al. [10], 2020 | quasi-experimental study | 40 dialysis nurses | Yes | Structured interviewing questionnaire and Observational checklists | Prior to intervention: 54% of dialysis nurses showed inadequate clinical practices. After the intervention: 93% showed improvement competent performance levels in AVF care |
| Smith and Ayars [15], 2025 | quasi-experimental study | 34 dialysis nurses and 25 patient care technicians | Yes | knowledge test | A gap between knowledge and practical application, indicating the need for targeted training. Active learning strategies were found to be more effective for staff in managing vascular access. |
| Alsolami and Alobaidi [17], 2024 | Cross-sectional study | 197 dialysis nurses | No | previously validated questionnaire | 37% of participants had specialized training in vascular access management. Self-efficacy in VA cannulation was high, with 98% confident in performing AVF and AVG assessments before cannulation. Nurses with an undergraduate degree were 92% more likely to be knowledgeable about AVF or AVG (p < 0.05) |
| Chen et al. [18], 2022 | Cross-sectional study | 222 dialysis nurses | No | A questionnaire that was validated by the authors (Cronbach’s a was 0.896) | The total vascular access knowledge score was 87.52 ± 13.71, with basic knowledge (3.88 ± 0.60), assessment (3.62 ± 0.65), and AVF puncture techniques (3.22 ± 0.71). Multiple linear regression identified that longer work experience, advanced training, and working in a public hospital were significant predictors of higher vascular access knowledge (p < 0.05). |
| Meng et al. [16], 2024 | Multicenter study cross-sectional study | 70 dialysis nurses (23 nurses from community centers and 47 from tertiary hospitals) | No | The 37-items survey consists of four dimensions of questions relating to vascular access cannulation and management: knowledge, attitude, practice and self-efficacy. | The participants exhibited a satisfactory level of knowledge, though some gaps were identified. Additionally, the results highlighted the nurses’ strong self-efficacy and positive attitude toward incorporating ultrasound into vascular access cannulation |
| Yousif et al. [14], 2017 | Multicenter pilot study | 61 dialysis nurses working at dialysis centers in Khartoum State, Sudan | Yes | K/DOQI questionnaire | Twenty-two individual variables assessing knowledge based on the K/DOQI guidelines showed significant improvement in nurses’ knowledge after the educational intervention (p < 0.001). The structured educational program based on K/DOQI guidelines significantly enhanced dialysis nurses’ knowledge in vascular access care. The knowledge gained was maintained for at least three months post-intervention. |
3. Clinical Nursing Practices in the Care of AVFs
4. Key Factors for Successful AVF/AVG Cannulation in HD Patients
5. Challenges and Optimal Management of AVF/AVG in Elderly HD Patients
6. Challenges and Management of Dialysis Access-Associated Steal Syndrome
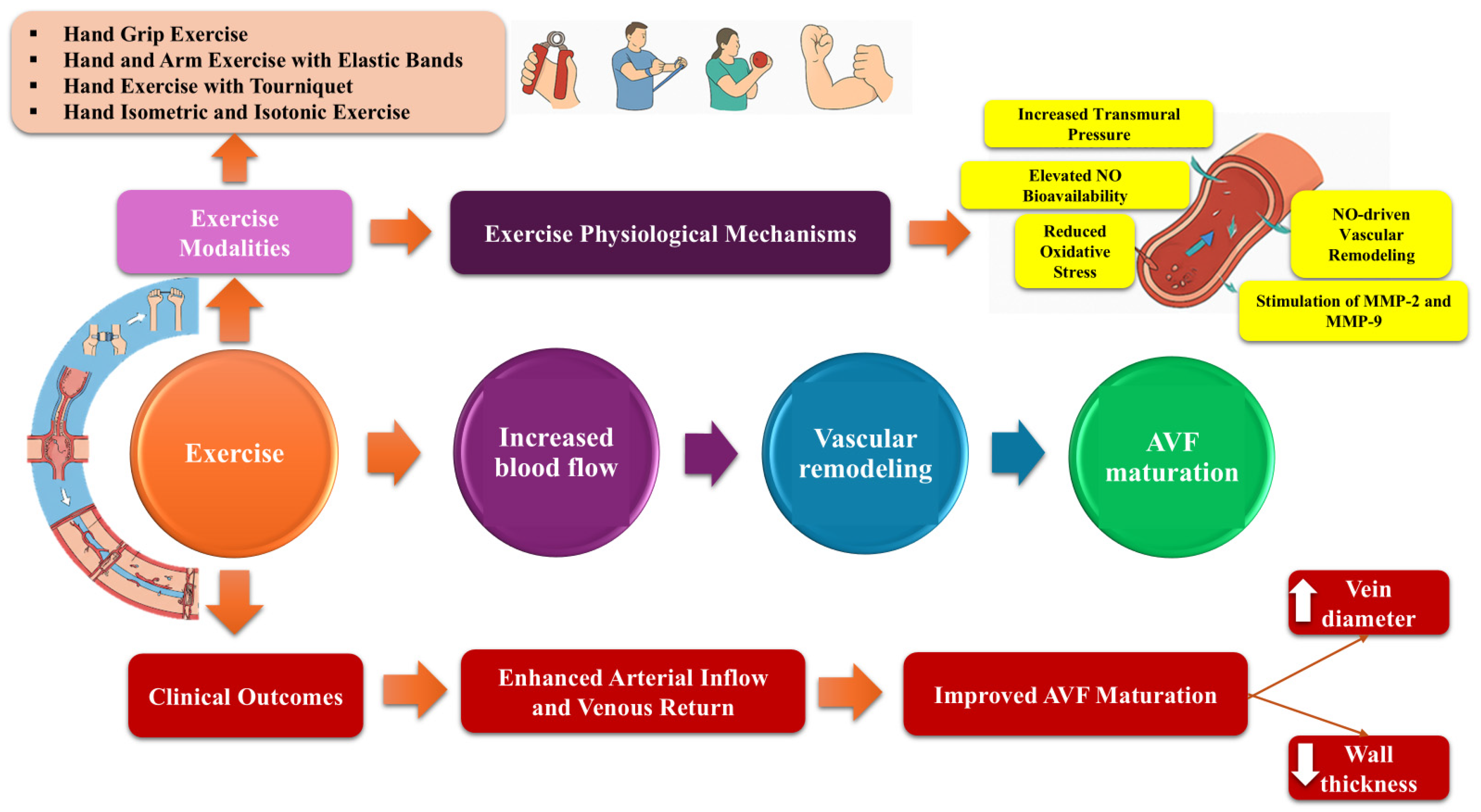
7. Upper Limb Exercise Intervention May Benefit AVF
8. Contextual Variations in AVF Management Practices
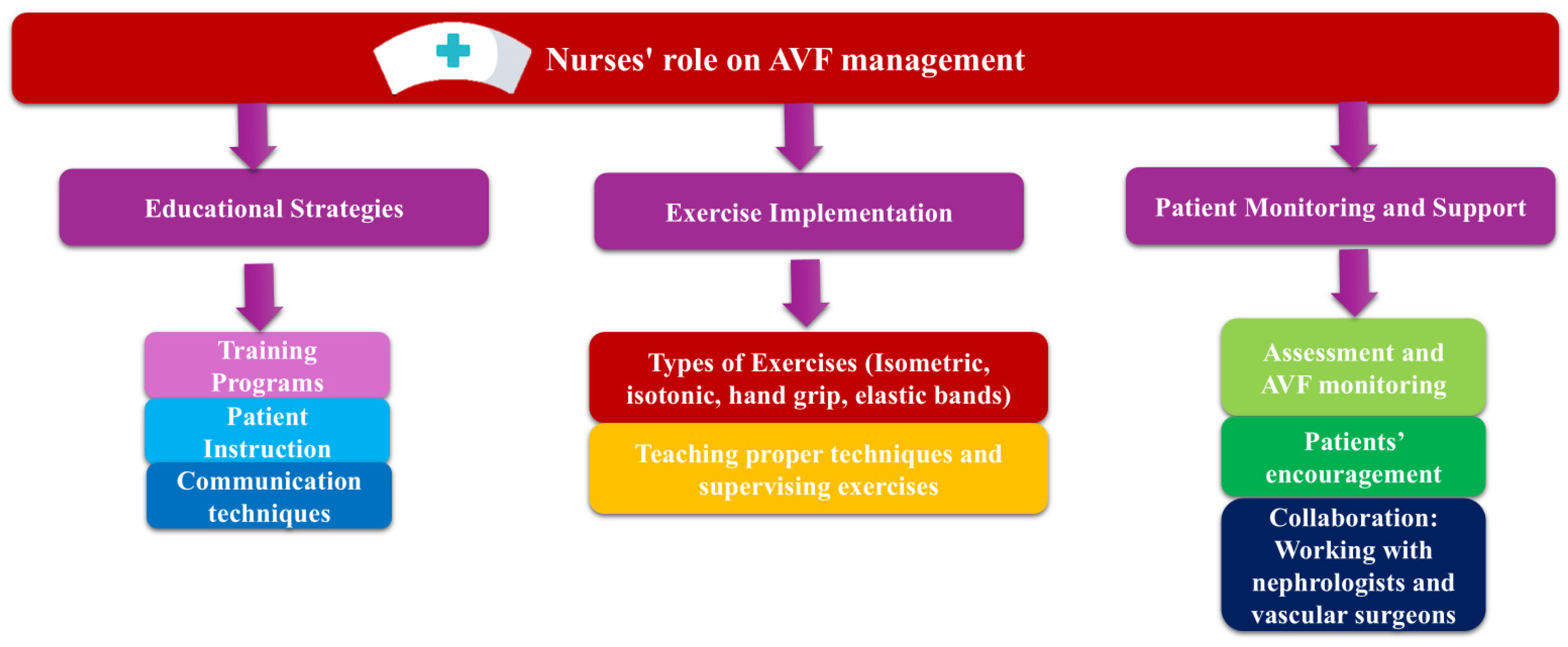
9. Suggestions on How to Improve AVF Management
10. Conclusions
Funding
Data Availability Statement
Conflicts of Interest
References
- Pinto, R.; Sousa, C.; Salgueiro, A.; Fernandes, I. Arteriovenous fistula cannulation in hemodialysis: A vascular access clinical practice guidelines narrative review. J. Vasc. Access 2022, 23, 825–831. [Google Scholar] [CrossRef]
- Qin, H.Y.; Jia, P.; Liu, H. Nursing Strategies for Patients with Chronic Renal Failure Undergoing Maintenance Hemodialysis Treatment by Arteriovenous Fistula. Iran. J. Public Health 2016, 45, 1270–1275. [Google Scholar] [PubMed]
- Wang, A.Y.; Sherrington, C.; Toyama, T.; Gallagher, M.P.; Cass, A.; Hirakawa, Y.; Li, Q.; Sukkar, L.; Snelling, P.; Jardine, M.J. Muscle strength, mobility, quality of life and falls in patients on maintenance haemodialysis: A prospective study. Nephrology 2017, 22, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Wang, J. Comprehensive Nursing Care for Vascular Access in Hemodialysis Patients with End-Stage Renal Disease. Int. J. Public Health Med. Res. 2024, 2, 42–46. [Google Scholar] [CrossRef]
- Kong, S.; Lee, K.S.; Kim, J.; Jang, S.H. The Effect of Two Different Hand Exercises on Grip Strength, Forearm Circumference, and Vascular Maturation in Patients Who Underwent Arteriovenous Fistula Surgery. Ann. Rehabil. Med. 2014, 38, 648. [Google Scholar] [CrossRef]
- Oder, T.F.; Teodorescu, V.; Uribarri, J. Effect of Exercise on the Diameter of Arteriovenous Fistulae in Hemodialysis Patients. ASAIO J. 2003, 49, 554–555. [Google Scholar] [CrossRef]
- González, I.T.; Simó, V.E.; Pallares, S.I.; Guzman, F.M.; Nicolás, M.F.; Gallego, V.D.; Solé, A.S.; Potau, M.P.; Campos, M.Y.; Serna, M.R.d.A. Upper limb isometric exercise protocolled programme and arteriovenous fistula maturation process. Clin. Kidney J. 2021, 14, 688–695. [Google Scholar] [CrossRef]
- Nantakool, S.; Srisuwan, T.; Reanpang, T.; Rerkasem, K.; Prasannarong, M. A randomized controlled trial of the effect of postoperative hand exercise training on arteriovenous fistula maturation in patients with chronic kidney disease. J. Vasc. Surg. 2022, 75, 230–237. [Google Scholar] [CrossRef]
- Mo, Y.; Song, L.; Sun, C.; Huang, J.; Zhou, L.; Zheng, S.; Zhuang, T.; Chen, Y.; Liu, S.; Liang, X.; et al. Effect of Dumbbell Exercise on Arteriovenous Fistula in Patients Undergoing Maintenance Haemodialysis: A Prospective Randomized Controlled Trial. Blood Purif. 2020, 49, 16–24. [Google Scholar] [CrossRef]
- Bayumi, H.A.E.; ElGammal, W.E.; Awad, R.D.H.; Elsayed, S.M. Effect of Educational Program on Nurses’ Performance regarding Arteriovenous Fistula among Hemodialysis Patients. Egypt. J. Health Care 2020, 11, 1278–1289. [Google Scholar] [CrossRef]
- Khalifa, M.I. Nurses’ Knowledge and Performance about Maintenance and prevention of Vascular Access Complications in Pediatric Hemodialysis Units. IOSR J. Nurs. Health Sci. 2017, 06, 87–99. [Google Scholar] [CrossRef]
- Zhongmei, H. Observation of the Nursing Intervention Effects on Arteriovenous Fistula in Hemodialysis Patients. MEDS Clin. Med. 2023, 4, 29–35. [Google Scholar]
- Yuan, L.; Yuan, H.; Feng, Q.; Zhao, J. Effect of continuous nursing on quality of life of hemodialysis patients: A protocol for systematic review and meta-analysis. Medicine 2021, 100, e24942. [Google Scholar] [CrossRef] [PubMed]
- Yousif, K.; Abu-Aisha, H.; Abboud, O. The effect of an educational program for vascular access care on nurses’ knowledge at dialysis centers in Khartoum State, Sudan. Saudi J. Kidney Dis. Transpl. 2017, 28, 1027. [Google Scholar]
- Smith, K.; Ayars, C. Improving vascular access knowledge and assessment skill of hemodialysis staff. J. Osteopat. Med. 2025, 125, 321–327. [Google Scholar] [CrossRef]
- Meng, L.; Guo, W.; Lou, L.; Teo, B.W.; Ho, P. Dialysis nurses’ knowledge, attitude, practice and self-efficacy regarding vascular access: A cross-sectional study in Singapore. J. Vasc. Access 2024, 25, 1432–1442. [Google Scholar] [CrossRef]
- Alsolami, E.; Alobaidi, S. Hemodialysis nurses’ knowledge, attitude, and practices in managing vascular access: A cross-sectional study in Saudi Arabia. Medicine 2024, 103, e37310. [Google Scholar] [CrossRef]
- Chen, H.; Chen, L.; Zhang, Y.; Shi, M.; Zhang, X. Knowledge of vascular access among hemodialysis unit nurses and its influencing factors: A cross-sectional study. Ann. Palliat. Med. 2022, 11, 3494–3502. [Google Scholar] [CrossRef]
- Lok, C.E.; Yuo, T.; Lee, T. Hemodialysis Vascular Access: Core Curriculum 2025. Am. J. Kidney Dis. 2025, 85, 236–252. [Google Scholar] [CrossRef]
- Leopaldi, D.; di PA, G.M. Vascular Access Management and Care: Arteriovenous Fistula (AVF). In Principles of Nursing in Kidney Care Principles of Specialty Nursing; Masià-Plana, A., Liossatou, A., Eds.; Springer: Cham, Switzerland, 2024. [Google Scholar]
- Coventry, L.L.; Hosking, J.M.; Chan, D.T.; Coral, E.; Lim, W.H.; Towell-Barnard, A.; Twigg, D.E.; Rickard, C.M. Variables associated with successful vascular access cannulation in hemodialysis patients: A prospective cohort study. BMC Nephrol. 2019, 20, 197. [Google Scholar] [CrossRef]
- Harwood, L.E.; Wilson, B.M.; Oudshoorn, A. Improving vascular access outcomes: Attributes of arteriovenous fistula cannulation success. Clin. Kidney J. 2016, 9, 303–309. [Google Scholar] [CrossRef] [PubMed]
- McCann, M.; Einarsdottir, H.; Van Waeleghem, J.P.; Murphy, F.; Sedgwick, J. Continuing Education Article Vascular Access Management Ii: Avf/Avg Cannulation Techniques And Complications. J. Ren. Care 2009, 35, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Etkin, Y.; Woo, K.; Guidry, L. Options for Dialysis and Vascular Access Creation. Surg. Clin. N. Am. 2023, 103, 673–684. [Google Scholar] [CrossRef] [PubMed]
- Vachharajani, T.J.; Hassanein, M.; Liaqat, A.; Haddad, N. Vessel Preservation in Chronic Kidney Disease. Adv. Chronic Kidney Dis. 2020, 27, 177–182. [Google Scholar] [CrossRef]
- Qian, J.Z.; McAdams-DeMarco, M.; Ng, D.K.; Lau, B. Arteriovenous Fistula Placement, Maturation, and Patency Loss in Older Patients Initiating Hemodialysis. Am. J. Kidney Dis. 2020, 76, 480–489.e1. [Google Scholar] [CrossRef]
- Hod, T.; Patibandla, B.K.; Vin, Y.; Brown, R.S.; Goldfarb-Rumyantzev, A.S. Arteriovenous Fistula Placement in the Elderly. J. Am. Soc. Nephrol. 2015, 26, 448–456. [Google Scholar] [CrossRef]
- Moist, L.M.; Lok, C.E.; Vachharajani, T.J.; Xi, W.; AlJaishi, A.; Polkinghorne, K.R.; Vazquez, M.; Lee, T.C. Optimal Hemodialysis Vascular Access in the Elderly Patient. Semin. Dial. 2012, 25, 640–648. [Google Scholar] [CrossRef]
- Menegolo, M.; Xodo, A.; Alessi, M.; Maturi, C.; Simioni, F.; Rossi, B.; Calò, L.A.; Antonello, M.; Grego, F. Elderly patient: Which vascular access? Choice and management of vascular access in the elderly patient. Nephrol. Point Care 2018, 4, 205930071875562. [Google Scholar] [CrossRef]
- Misskey, J.; Faulds, J.; Sidhu, R.; Baxter, K.; Gagnon, J.; Hsiang, Y. An age-based comparison of fistula location, patency, and maturation for elderly renal failure patients. J. Vasc. Surg. 2018, 67, 1491–1500. [Google Scholar] [CrossRef]
- Wang, B.; Rao, A.; Pappas, K.; Silpe, J.; Garlapati, A.; Talathi, S.; Mussa, F.; Landis, G.S.; Etkin, Y. Maturation Rates of Arteriovenous Fistulas Using Small Veins in the Era of Endovascular Interventions. Ann. Vasc. Surg. 2021, 71, 208–214. [Google Scholar] [CrossRef]
- Davidson, D.; Louridas, G.; Guzman, R.; Tanner, J.; Weighell, W.; Spelay, J.; Chateau, D. Steal syndrome complicating upper extremity hemoaccess procedures: Incidence and risk factors. Can. J. Surg. 2003, 46, 408–412. [Google Scholar] [PubMed]
- Stoecker, J.B.; Li, X.; Clark, T.W.I.; Mantell, M.P.; Trerotola, S.O.; Vance, A.Z. Dialysis Access-Associated Steal Syndrome and Management. Cardiovasc. Interv. Radiol. 2023, 46, 1168–1181. [Google Scholar] [CrossRef]
- Mohamed, A.S.; Peden, E.K. Dialysis-associated steal syndrome (DASS). J. Vasc. Access 2017, 18, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Green, D.J.; Hopman, M.T.E.; Padilla, J.; Laughlin, M.H.; Thijssen, D.H.J. Vascular Adaptation to Exercise in Humans: Role of Hemodynamic Stimuli. Physiol. Rev. 2017, 97, 495–528. [Google Scholar] [CrossRef]
- Green, D.J.; Bilsborough, W.; Naylor, L.H.; Reed, C.; Wright, J.; O’Driscoll, G.; Walsh, J.H. Comparison of forearm blood flow responses to incremental handgrip and cycle ergometer exercise: Relative contribution of nitric oxide. J. Physiol. 2005, 562, 617–628. [Google Scholar] [CrossRef]
- Brahmbhatt, A.; Remuzzi, A.; Franzoni, M.; Misra, S. The molecular mechanisms of hemodialysis vascular access failure. Kidney Int. 2016, 89, 303–316. [Google Scholar] [CrossRef]
- Nantakool, S.; Reanpang, T.; Prasannarong, M.; Pongtam, S.; Rerkasem, K. Upper limb exercise for arteriovenous fistula maturation in people requiring permanent haemodialysis access. Cochrane Database Syst. Rev. 2022, 2022, CD013327. [Google Scholar]
- Salimi, F.; Nassiri, G.M.; Moradi, M.; Keshavarzian, A.; Farajzadegan, Z.; Saleki, M.; Nikpoor, A.; Ghane, M. Assessment of Effects of Upper Extremity Exercise with Arm Tourniquet on Maturity of Arteriovenous Fistula in Hemodialysis Patients. J. Vasc. Access 2013, 14, 239–244. [Google Scholar] [CrossRef]
- Fontseré, N.; Mestres, G.; Yugueros, X.; López, T.; Yuguero, A.; Bermudez, P.; Gomez, F.; Riambau, V.; Maduell, F.; Campistol, J.M. Effect of a postoperative exercise program on arteriovenous fistula maturation: A randomized controlled trial. Hemodial. Int. 2016, 20, 306–314. [Google Scholar] [CrossRef]
- Pessoa, N.R.C.; Lima, L.H.d.S.S.; dos Santos, G.A.; Frazão, C.M.F.d.Q.; Sousa, C.N.; Ramos, V.P. Self-care actions for the maintenance of the arteriovenous fistula: An integrative review. Int. J. Nurs. Sci. 2020, 7, 369–377. [Google Scholar]
- Lok, C.E.; Huber, T.S.; Lee, T.; Shenoy, S.; Yevzlin, A.S.; Abreo, K.; Allon, M.; Asif, A.; Astor, B.C.; Glickman, M.H.; et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am. J. Kidney Dis. 2020, 75, S1–S164. [Google Scholar] [CrossRef] [PubMed]
- Baharani, J.; Vincent, L.; Vachharajani, T.J. Long-Term Dialysis Vascular Access in East Africa: Unique Challenges and Novel Solutions. Kidney 360 2023, 4, 1143–1146. [Google Scholar] [CrossRef] [PubMed]
- Bvumbwe, T.; Mtshali, N. Nursing education challenges and solutions in Sub Saharan Africa: An integrative review. BMC Nurs. 2018, 17, 3. [Google Scholar] [CrossRef] [PubMed]
- Vanholder, R.; Van Biesen, W.; Fox, J.G.; Nagler, E.V. The new European Renal Best Practice guideline on arteriovenous access: Why worthwhile to read. Nephrol. Dial. Transpl. 2019, 34, 1071–1074. [Google Scholar] [CrossRef]
- Wilmink, T. Vascular Access: Clinical Practice Guidelines of the European Society for Vascular Surgery. Eur. J. Vasc. Endovasc. Surg. 2018, 55, 753–754. [Google Scholar] [CrossRef]
- Ramachandran, R.; Bhargava, V.; Jasuja, S.; Gallieni, M.; Jha, V.; Sahay, M.; Alexender, S.; Mostafi, M.; Pisharam, J.K.; Wai, T.S.C.; et al. Interventional nephrology and vascular access practice: A perspective from South and Southeast Asia. J. Vasc. Access 2022, 23, 849–860. [Google Scholar] [CrossRef]
- Agustina, F.; Yetti, K.; Sukmarini, L. Contributing factors to hemodialysis adherence in Aceh, Indonesia. Enferm. Clin. 2019, 29, 238–242. [Google Scholar] [CrossRef]
- Polkinghorne, K.R.; Chin, G.K.; MacGinley, R.J.; Owen, A.R.; Russell, C.; Talaulikar, G.S.; Vale, E.; Lopez-Vargas, P.A. KHA-CARI Guideline: Vascular access—Central venous catheters, arteriovenous fistulae and arteriovenous grafts. Nephrology 2013, 18, 701–705. [Google Scholar] [CrossRef]
- Dhgahkms, P.K. Hemodialysis. In Haemodialysis ANZDATA Thirty Fourth Annual Report; McDonald, S.H.K., Ed.; Australia and New Zealand Dialysis and Transplant Registry: Adelaide, SA, Australia, 2011; pp. 25–31. [Google Scholar]

| Author, Year | Design | Sample Size | Duration, Measurements, Type of Exercise and Groups | Main Results | Stenghs/Limitations or Potential Bias |
|---|---|---|---|---|---|
| Kong et al. [5], 2014 | RCT | 18 HD patients that have AVF surgery | 4 weeks exercise program Group A: n = 10 HD patients, who performed hand-squeezing exercise with a handgrip tool (GD grip) Group B: n = 8 HD patients used a soft ball | GD Grip and Soft Ball exercises both improved cephalic vein size, blood flow volume, and forearm circumference. GD Grip was more effective in enhancing pinch and grip strength, while blood flow velocity remained unchanged in both groups. | Lack of randomization and control group limits causality; small sample size reduces statistical power; single-center design limits generalizability. |
| Oder et al. [6], 2003 | cross-sectional study | 23 HD patients with newly created AVF (mean 2.8 months) | Acute exercise Duplex ultrasound was used to assess the fistula diameter three times before and after a 5-min rubber ball squeezing exercise. | An increase in diameter was observed in 20 out of 23 patients, with a statistically significant average increase of 9.3% (p < 0.0001). | Small sample size and lack of a well-defined control group limit findings; conducted over two decades ago, which may reduce relevance due to changes in clinical practices. |
| Mo et al. [9], 2020 | RCT | 86 HD patients | 3 months exercise program Group A: n = 38 HD patients, held 6-pound dumbbells on non-dialysis days Group B: n = 40, squeezed rubber balls | The study found a significant increase in blood flow of the draining vein in the dumbbell exercise group at three months, with a mean difference of 359.50 mL/min (95% CI: 111.90–829.05; p = 0.001). However, no significant differences were observed between the groups regarding blood flow in the AVF proximal artery and brachial artery, draining vein diameter, or adverse event incidence. | Randomization strengthens reliability; however, variations in participants’ baseline physical fitness were not addressed, which could have influenced the results. |
| Fontseré et al. [40], 2016 | RCT | 69 HD patients | Group A: n = 38 HD patients that followed an ambulatory daily exercise program with flex band for 1 month after arteriovenous fistula creation. Group B: n = 31 HD patients that did not exercise | The study found no statistically significant differences in clinical or ultrasonographic maturation rates between exercise and control groups (94.7% vs. 80.6%, p = 0.069; 81.6% vs. 74.2%, p= 0.459). However, after adjusting for confounding factors such as AVF localization using stepwise logistic regression, the exercise group demonstrated significantly greater odds of clinical maturation (OR 5.861, 95% CI: 1.006–34.146), though no significant difference was observed for ultrasonographic maturation (OR 2.403, 95% CI: 0.66–8.754). | Short follow-up period limits long-term AVF durability conclusions; did not account for baseline vascular health differences among participants. |
| Salmi et al. [39], 2013 | RCT | 50 HD patients | Group A: n = 25 HD patients followed simple hand exercise (opening and closing the fingers), two days after the AVF surgery. Group B: n = 25 HD patients followed an isometric exercise program, which was initiated for two days postoperatively and implemented through a combination of supervised sessions and home-based practice. | Post-exercise ultrasound assessments revealed significant increases in draining vein diameter, vein wall thickness, vein area, and blood flow rate (p = 0.009, 0.04, 0.02, and 0.02, respectively). Additionally, a significantly higher number of patients in the exercise group achieved clinical AVF maturation compared to the control group (13 vs. 5; p = 0.008). | Reported improved vein dilation; lacked clear exercise intensity/frequency details; cross-sectional design limits long-term outcome tracking. |
| Tapia Gonzalez et al. [7], 2021 | prospective study | 60 HD patients | 8 weeks exercise and follow-up after 24-months Group A: n = 30 HD patients followed isometric exercise protocoled program. Group B: n = 30 HD patients received usual care. Muscle strength, Doppler ultrasound parameters, AVF maturation, and vascular access complications were assessed at 4 and 8 weeks to evaluate the impact of an upper limb isometric exercise program on AVF maturation. | The exercise group demonstrated higher clinical maturation rates at 4 weeks (control group 33.3% vs. exercise group 70%, p = 0.009) and 8 weeks (control group 33.3% vs. exercise group 76.7%, p = 0.002). Additionally, duple ultrasound maturation was better in the exercise group in both 4 weeks (control group 40% vs. exercise group 80%, p = 0.003) and 8 weeks (control group 43.3% vs. exercise group 83.3%, p = 0.003). | Observational design raises bias concerns; self-reported adherence may overestimate compliance. |
| Nantakool et al. [8], 2022 | RCT | 50 HD patients | 10 weeks exercise program Group A: n = 25 HD patients followed an isometric hand exercise program. Group B: n = 25 HD patients followed an isotonic hand exercise program. intensity of 30% maximum voluntary contraction every day for 10 weeks | At weeks 6 and 10, the group A showed significantly larger cephalic vein diameters compared to the group B (week 6: 7.1 ± 1.2 mm vs. 6.2 ± 1.0 mm; week 10: 7.1 ± 1.0 mm vs. 6.2 ± 1.1 mm). The group A also demonstrated a higher number of patients achieving ultrasound-defined maturation at weeks 2, 6, and 10 (8 vs. 2; 16 vs. 8; 21 vs. 12, respectively), as well as greater clinical maturation at week 10 (25 vs. 18). No adverse events were reported during the study period. | Robust design with randomization and control group enhances validity; lacks assessment of confounding factors like baseline physical activity. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michou, V. Optimizing Clinical Nursing Interventions for Hemodialysis Patients with Arteriovenous Fistula. Kidney Dial. 2025, 5, 31. https://doi.org/10.3390/kidneydial5030031
Michou V. Optimizing Clinical Nursing Interventions for Hemodialysis Patients with Arteriovenous Fistula. Kidney and Dialysis. 2025; 5(3):31. https://doi.org/10.3390/kidneydial5030031
Chicago/Turabian StyleMichou, Vasiliki. 2025. "Optimizing Clinical Nursing Interventions for Hemodialysis Patients with Arteriovenous Fistula" Kidney and Dialysis 5, no. 3: 31. https://doi.org/10.3390/kidneydial5030031
APA StyleMichou, V. (2025). Optimizing Clinical Nursing Interventions for Hemodialysis Patients with Arteriovenous Fistula. Kidney and Dialysis, 5(3), 31. https://doi.org/10.3390/kidneydial5030031







