Abstract
Previous findings assessing the relationship between high-density lipoprotein cholesterol (HDL-c) and kidney function have demonstrated contradictory results including positive, negative, and U-shaped relationships. Many prior studies in this area have been conducted in healthy populations, but few have considered the influence of metabolic health status. In the present study, a cross-sectional analysis was conducted using complex survey sample weighting in the assessment of 6455 subjects from the 2013–2018 National Health and Nutrition Examination Surveys (NHANES), representative of 94,993,502 United States citizens. Subjects were classified as metabolically healthy or unhealthy and linear regression analyses were performed to evaluate the influence of HDL-c on estimated glomerular filtration rate (eGFR). HDL-c was found to be negatively associated with eGFR in the metabolically healthy, unhealthy, and combined groups (B = −0.16, p < 0.0001, B = −0.21, p < 0.0001, and B = −0.05, p = 0.0211, respectively). This relationship persisted after adjustment for confounding variables (B = −0.24, p < 0.0001, B = −0.17, p < 0.001, and B = −0.18, p < 0.0001, respectively). The relationship between HDL-c and eGFR was found to be a negative linear association, rather than a U-shaped association, and it persisted in all models tested, despite statistical adjustment for confounding variables. After controlling the samples for outliers, the negative relationship between HDL-c and eGFR was attenuated in the healthy and total groups but remained significant in the MetS group, indicating a stronger relationship between HDL-c and eGFR in those with poorer health.
Keywords:
chronic kidney disease; CKD; high-density lipoprotein; HDL-c; renal function; inflammation 1. Introduction
Kidney function is influenced by many factors, both modifiable (i.e., physical activity [PA], dietary habits, substance use) and non-modifiable (i.e., age, gender, race). The major contributors to significant renal decline and subsequent chronic kidney disease (CKD) in the United States (US) are hypertension (HTN) and hyperglycemia [1], two risk factors that may have modifiable components [2,3,4,5]. These two risk factors also contribute to metabolic syndrome (MetS), which is diagnosed when an individual has three or more of the five metabolic risk factors defined by the harmonized definition of MetS [6]. MetS has been demonstrated to be strongly associated with CKD [7], though the relationship is complex and not all metabolic risk factors have the same effect on renal function.
While prior research has demonstrated strong connections between HTN, hyperglycemia, and CKD, there have been conflicting results regarding the relationship between high-density lipoprotein cholesterol (HDL-c) and renal function. Traditionally, low HDL-c cholesterol has been classified as a metabolic risk factor because of its association with atherosclerotic cardiovascular disease (ASCVD) and CKD [8]. Higher levels of HDL-c are thought to be protective due to the scavenger role HDL-c contributes to reverse cholesterol transport, nitric oxide production, and prevention of fat oxidation. However, recent assessments of the relationship between HDL-c and ASCVD have proven equivocal [9] and attempts to improve HDL-c pharmacologically have not been demonstrated to be clinically beneficial [10].
Prior research has demonstrated mixed results when comparing the relationship between HDL-c and renal function. Several studies, including a meta-analysis [11] and Mendelian randomization studies [12,13], have reported that higher HDL-c levels are linked with slightly better eGFR [14] and, in published findings, lower risk of all-cause mortality in individuals with CKD [15]. However, contradictory results have also been published which demonstrate U-shaped associations between HDL-c and eGFR [16] as well as HDL-c and all-cause mortality in those with and without CKD [17]. Other authors have demonstrated an inverse, or negative, relationship between HDL-c and eGFR, indicating that lower levels of HDL-c were associated with higher levels of eGFR [18,19]. Several hypotheses have been established to explain these conflicting findings, including a rare impairment of scavenger receptor BI [20], the ratio of HDL-c subtypes [21], and the age and quality of the HDL-c molecules themselves [22,23,24], but none have definitively identified the reason for these mixed findings.
While prior studies have been conducted in many different populations and using different modalities, most were done in otherwise healthy subjects who were free of metabolic disease. Further research is warranted to develop a better understanding of the association between HDL-c cholesterol and renal function and to establish if the relationship changes in the milieu of metabolic dysregulation. The aim of the present study was to determine the relationship between HDL-c and eGFR in a large US-based study sample which includes both metabolically healthy and unhealthy subjects. A secondary focus was understanding the risk factors associated with MetS in a large, diverse US sample.
2. Materials and Methods
The present study utilized deidentified data that are publicly available online via the Centers for Disease Control and Prevention (CDC) website [25]. Therefore, the institutional review board (IRB) at the sponsoring university determined that the study was exempt from IRB review (IRB ID# 1505514-1).
2.1. Study Sample
The NHANES sample consists of civilian, non-institutionalized individuals who live within the US. The sample design is a multiyear, stratified, clustered four-stage sample, with oversampling of underrepresented groups such as ethnic minorities, impoverished individuals, children, and older adults. Unique sample weights are assigned to each subject and can be used in statistical analyses to produce health statistics that are representative of the greater US population. Weighting considers the known probability of selection, non-responders, and the differences between the sample and the US population. The sample weighting is conducted in three steps. The first accounts for the oversampling of minority groups, the second adjusts for non-responders, and the third is a post-stratification that matches the sample to the known civilian, non-institutionalized population US which is determined by information from the US Census Bureau. The sample weighting variables, which include masked variance pseudo-primary sampling unit (PSU), masked variance pseudo-stratum, and fasting subsample 2-year mobile examination center weights, are published online by the National Center for Health Statistics (NCHS) in 2-year cycles alongside Sample Design and Estimation Procedure documents which describe each cycle’s study design and how to use the weighting procedures in detail [26,27,28]. The present study consists of the three most recently published study cycles that contain complete data (2013–2018) and utilizes statistical techniques to incorporate the complex survey sample weighting procedures that render the results more appropriate and generalizable to the US population.
The present study included subjects between the ages of 18 to 79 who completed study procedures pertaining to metabolic and renal health. The upper age limit was chosen for our study because age is top-coded at 80 in the NHANES datasets to prevent subject identification. Pregnant subjects and those who reported using renal dialysis in the year leading up to the study were excluded from analysis. The primary analyses included 6455 study subjects who were representative of 94,993,502 US citizens when statistical adjustments for sample weighting techniques were applied.
2.2. Demographic and Variable Information
Procedures for the NHANES questionnaires, examinations, and laboratory data are outline on the CDC website [29]. Questionnaire data were obtained in subjects’ residences using the Computer-Assisted Personal Interview (CAPI) system guided by trained interviewers. For the present study, two 24 h dietary interviews were combined to create a composite dietary intake value. Individuals who fell at or below 100% of the poverty line were considered low socioeconomic status (SES). Subjects were identified as smokers if they smoked more than 100 cigarettes in their entire life and/or reported tobacco use in the 5 days prior to the study. Physically active individuals were those who engaged in ≥ 150 min per week of moderate-intensity recreational PA, ≥ 75 min per week of vigorous-intensity recreational PA, or an equivalent combination of the two [30,31]. Codes from the International Classification of Diseases, Tenth Revision (ICD-10) were assigned to participants who completed the drug use questionnaire. The present study utilized ICD-10 codes for pharmacological information pertaining to hyperglycemia (codes R73, E11, E11.2, E11.2P, E11.4, and E11.P), dyslipidemia (codes E78.0, E78.0P, and E78.1), and hypertension (codes I10 and I10.P). Waist to height ratio was determined by dividing waist circumference (WC) in centimeters (cm) by height (cm).
Metabolic syndrome was defined by the confirmation of three or more of the five metabolic risk factors outlined in the harmonized definition of MetS published by Alberti et al., in 2009 [6]. The MetS risk factors include: elevated waist circumference (≥ 102 cm in males, ≥ 88 cm in females, ≥90 cm in Asian males, or ≥ 80 cm in Asian females), elevated triglycerides (≥ 150 mg/dL) or pharmacological treatment for elevated triglycerides, reduced HDL-c (< 40 mg/dL in males or < 50 mg/dL in females) or drug treatment for reduced HDL-c, elevated blood pressure (systolic ≥ 130 mmHg and/or diastolic ≥ 85 mmHg) or antihypertensive drug treatment, and elevated fasting glucose (≥ 100 mg/dL) or drug treatment for hyperglycemia. In the present study, metabolically unhealthy individuals were defined as those who had three or more metabolic risk factors. Renal function was calculated using the CKD-EPI equation [32] and reported as a measure of estimated glomerular filtration rate (eGFR) in ml/min/1.73 m2. CKD was defined as an eGFR < 60 mL/min/1.73 m2 or an albumin to creatinine ratio ≥ 30.
2.3. Statistical Analyses
Normality tests were conducted for variables by the assessment of skewness, kurtosis, Kolmogorov–Smirnov tests, histograms, and P-P and Q-Q plots. Normally distributed continuous data were analyzed and reported as mean (x) and standard deviation (SD) whereas non-normal data were reported as median (M) and interquartile range (IQR). Categorical data were reported as frequency and percentage. Survey sample weights were incorporated by assigning cluster, strata, and weight variables within the SURVEY procedure(s) in SAS. All weighted subsamples were analyzed using a DOMAIN statement to ensure that the number of elements in the sample and the standard errors were correctly calculated. Demographic differences between the metabolically healthy and unhealthy subsamples were determined using simple regression and χ2 tests. The main analyses were determined a priori and were conducted using multiple regression models with the SURVEYREG procedure, which accounted for survey sample weights. Two-sided probability values were considered significant at the α < 0.05 level. All values are reported using survey sample weighting, unless otherwise noted. Statistical analyses and normality tests were conducted in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
3. Results
A sample of 6455 individuals represented 94,933,502 US citizens using the complex survey sample weighting techniques. The subject demographics are listed in Table 1. Nearly half (40%) of the sample analyzed met the criteria for MetS, indicative of the health status of the country. Those who were metabolically unhealthy were older in age, were more likely to be non-Hispanic White, had greater BMI, greater measures of inflammation, reported greater use of prescription drugs, were less likely to engage in physical activity, more likely to smoke, had lower HDL-c, and lower renal function. There were no statistical differences between healthy and unhealthy groups regarding sex and SES.

Table 1.
Demographics Table.
The regression analyses completed in healthy subjects (Table 2) demonstrated a small yet significant negative relationship between HDL-c and eGFR (B = −0.16, p < 0.0001 in Model 1 and depicted in Figure 1a), indicating that for every 1-point increase in HDL-c, there was a 0.16-point reduction in eGFR. This result was strengthened in subsequent models which controlled for possible confounding variables listed in the footers of Table 2, Table 3 and Table 4. The adjusted models for the healthy subsample demonstrated a larger influence of HDL-c on eGFR, when all other variables were held constant (B = −0.18, p < 0.001 in Model 2 and B = −0.24, p < 0.0001 in Model 3). These results were attenuated when the middle 50% of the sample was considered (Table 5). Table 3 demonstrates adjusted and unadjusted results for the relationship between HDL-c and eGFR in the metabolically unhealthy group (B = −0.21, p < 0.0001, unadjusted, in Model 4 and depicted in Figure 1b). This effect was consistent in the models that were adjusted for confounding variables (B = −0.16, p = 0.0006 in Model 5 and B = −0.17, p = 0.0008 in Model 6). This relationship remained significant when the middle 98%, 90%, 80%, and 50% were analyzed in Table 5 and Table 6. The models with the whole sample (Table 4) utilized all individuals in the NHANES datasets with complete metabolic and renal data and included both metabolically healthy and unhealthy individuals. The unadjusted model yielded a weak yet statistically significant negative relationship between HDL-c and eGFR (B= −0.05, p = 0.0211, unadjusted, in Model 7 and depicted in Figure 1c). After adjustment for confounding variables, the relationship was slightly strengthened (B = −0.10, p = 0.01 in Model 8 and B = −0.18, p < 0.0001 in Model 9). The negative relationship between HDL-c and eGFR was not preserved when the middle 50–90% of the sample was considered. The restricted cubic spline plots in Figure 2 demonstrate the predicted curve associated with HDL-c and eGFR in the total sample and subsamples, with nonlinear relationships depicted between the interior knots. There were no U-shaped associations found between HDL-c and eGFR in the three samples. Figure 3 is an unweighted scatterplot demonstrating the relationships between healthy and MetS groups, with an unweighted regression line depicting the relationship of the total group.

Table 2.
Relationship Between eGFR and HDL-c in Healthy Subjects.
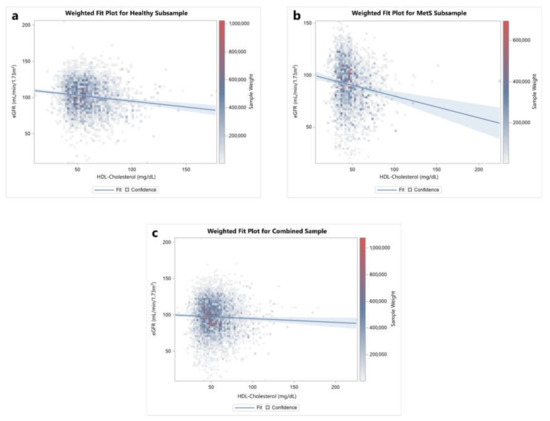
Figure 1.
Figure comparing weighted, unadjusted regression plots for the effects of HDL-c on eGFR in (a) the healthy subsample, (b) the subsample with metabolic syndrome, and (c) the combined sample.

Table 3.
Relationship Between eGFR and HDL-c in MetS Subjects.

Table 4.
Relationship Between eGFR and HDL-c in Whole Sample.

Table 5.
Weighted Simple Regression of eGFR and HDL-c.

Table 6.
Unweighted Pearson’s Correlations for eGFR and HDL-C.
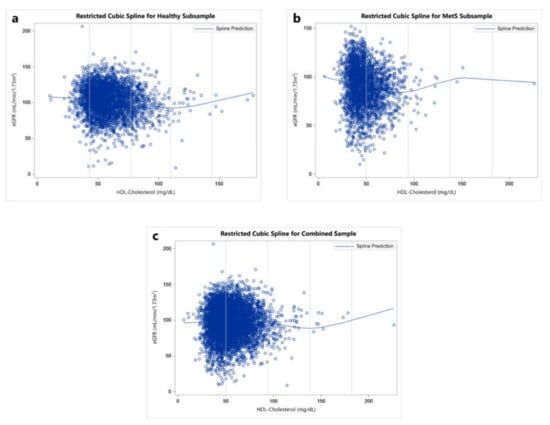
Figure 2.
Figure comparing unweighted cubic spline plots for the effects of HDL-c on eGFR in (a) the healthy subsample, (b) the subsample with metabolic syndrome, and (c) the combined sample.
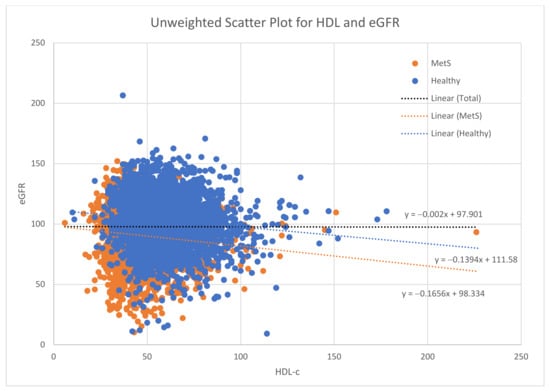
Figure 3.
Unweighted scatterplots for each group, with regression lines. This figure shows the negative relationship between HDL-c and eGFR in the healthy and MetS groups (blue and orange regression lines, respectively), while there is no relationship in the total group, demonstrated by the black regression line.
4. Discussion
The cardinal findings of the present study indicate a negative relationship between HDL-c and eGFR in both the metabolically healthy and unhealthy subjects in the US. This relationship between HDL-c and eGFR was strengthened when potential confounders were controlled for in all samples. The relationship was attenuated when considering the middle 50% of HDL-c values for the total and healthy samples yet persisted in the MetS sample. Prior research findings linking HDL-c and eGFR have produced mixed results, with studies reporting a broad range of associations including a positive relationship between HDL-c and eGFR [11,12,13,14], a U-shaped, or biphasic, relationship between HDL-c and eGFR [16], and a negative relationship, similar to the findings of the present study [18,19]. While most research in this area has been conducted in populations free of metabolic disease, our study demonstrates a negative relationship between HDL-c and eGFR in the overall sample, as well as in the metabolically healthy and unhealthy subsamples. This relationship remained persistent after adjustment for confounding variables, however it was attenuated in the total and healthy groups after controlling for outliers.
A prior Mendelein randomization study by Lanktree et al. [13] demonstrated a significant positive association between HDL-c and eGFR, reporting that a 17-mg/dL increase in HDL-c was associated with a 0.8% increase in eGFR. Though our methodology is distinct from that of Lanktree et al., it is worth noting that in the present study a 17-mg/dL increase in HDL-c would result in a 3.57% decrease in eGFR in the total sample, using estimates from the most adjusted model (Model 9). In fact, the main regression models demonstrated in the present study indicate that higher values of HDL-c are associated with lower estimates of eGFR, regardless of metabolic health status and adjustment for other risk factors and/or confounding variables. Though a negative association between HDL-c and eGFR appears counterintuitive, there is evidence that others have found discordant results as well. In a recent original article, Melsom et al. reported that higher HDL-c levels were associated with a steeper decline in eGFR over time, with a decrease of 0.53 mL/min/1.73 m2 per year for those in the high HDL-c group (> 61 mg/dL) in the most adjusted model, though they also lacked sufficient evidence to explain a cause for the relationship.
More recent study authors suggest that a focus on quantity of HDL-c does not help to identify those at risk for various disease states such as ASCVD or CKD. Measured HDL-c is a composite of HDL-cholesterol load and particle number, but it primarily reflects large buoyant HDL (HDL2) and neglects the contribution of smaller, denser subfractions such as HDL3 and preβ. Our current assessment was limited to the standard clinical measurement of HDL-c, and therefore the observed relationship is not specific enough to distinguish between cholesterol load and particle number, nor does it account for the functionality of the individual HDL subfractions [33,34]. Carnuta et. al., reported that the HDL2 and HDL3 subfractions were dysfunctional in ASCVD patients in their study [33]. This dysfunction was caused by enzymatic changes associated with inflammation that converted the HDL3 subfractions into pro-inflammatory and pro-oxidant HDL-c. The increase in HDL-c was associated with increased ASCVD outcomes. This increase in quantity but not quality could explain why, in the present study, higher levels of HDL-c were associated with lower levels of eGFR. Additionally, Bonizzi et al., suggests triglyceride levels could be a clinically relevant measurement for identifying dysfunctional HDL-c, as dysfunctional HDL-c is associated with an altered lipid and protein composition [34]. One novelty of the present study is that a similar relationship was identified in both the metabolically healthy and unhealthy study participants after controlling for confounding variables that may influence HDL-c and eGFR. These findings suggest new approaches for identifying dysfunctional HDL-c through clinical approaches and testing and new therapies to impact HDL-c quality.
Although most studies assessing HDL-c and eGFR have classified the relationship as linear, a unique biphasic effect of HDL-c has also been demonstrated in some studies, as indicated by a U-shaped, or biphasic, association between HDL-c and the outcome of interest. Bowe et al. [16] found that both low and high levels of HDL-c were associated with greater risk of CKD and lower renal function. The authors hypothesized that at higher concentrations, HDL-c may lose its protective properties. While we did not find a distinct U-shaped association in our cubic spline plots, this theory may help explain why we saw a significant negative association between HDL-c and eGFR in the healthy and total samples that dropped off after exclusion of the outer 50%, 20%, 10%, and 2%. The biphasic theory associated with HDL-c functionality is supported in an article by Huang et al. [35] which reported that an HDL-c level equivalent to 40–80 mg/dL in humans impaired the viability of endothelial progenitor cells (EPC) and paradoxically enhanced their senescence (i.e., it halted the EPC replication process and reduced cell number). Huang et al. also found that HDL-c only demonstrated protective effects in the direct presence of oxidized LDL-c (oxLDL-c). The present study was limited to a single measure of LDL-c in the NHANES datasets, but, given the proposed importance of oxLDL-c in the functionality of HDL-c, future studies should consider viewing the impact of HDL-c in light of plasma oxLDL-c levels.
Factors that have been known to influence the function of HDL-c include older age, systemic inflammation, oxidative stress, hyperglycemia, and dyslipidemia. Many of these factors were present in those classified with MetS in our study, as indicated by older average age in the MetS subsample (53.54 vs. 41.07 years), greater levels of high-sensitivity C-reactive protein (hsCRP, 4.86 vs. 2.91 mg/L), a higher fasting glucose (121.87 vs. 98.25 mg/dL), higher triglycerides (159.43 vs. 84.19 mg/dL), and lower average HDL-c (47.69 vs. 59.07 mg/dL). Prior researchers have hypothesized that HDL-c may be artificially elevated in the milieus of metabolic dysregulation and/or CKD [12,16,17,36,37] due to dysfunctional varieties of HDL-c, as mentioned previously, created by these environments. A recent review by Rysz et al., expounded on the effects of CKD and HDL-c functionality [38]. It is known that CKD is associated with disturbances in lipoprotein metabolism such as increased atherogenic particles, increased density of LDL-c, and greater dysfunction of HDL-c particles. Lower eGFR levels are linked to reduced levels of apoA-1 and apoA-2, which may reduce anti-atherosclerotic properties in immature HDL particles, rendering them less effective in reverse cholesterol transport. Higher levels of dysfunctional HDL-c are associated with increase in LDL-c, while the milieu of CKD also includes increased triglycerides, and therefore greater risk of ASCVD. By comparing the metabolically healthy subgroup to those with metabolic syndrome, our study demonstrated that a negative relationship exists between HDL-c and eGFR despite adjustment. We controlled for possible confounding variables in the regression analyses in order to determine if factors such as physical activity, cholesterol medication, smoking, hs-CRP, sex, race, albumin levels, triglycerides, waist-to-height ratio, and caloric intake influenced the relationship between HDL-c and eGFR. We found that controlling for these variables made the relationship stronger in the healthy and total groups, while it slightly attenuated the relationship in the MetS group. This may indicate that lifestyle and other risk factors play a more important role in the health of individuals who have already developed MetS. Interventional efforts focused on lifestyle improvements, such as beginning an exercise routine, improving diet, and cessation of smoking may be most beneficial to those with MetS.
A majority of the studies assessing HDL-c, including the present study, use a sole measure of serum HDL-c to determine its influence on renal function and other measurable outcomes. However, there are many other measurable characteristics of HDL-c, including particle size, composition, and quality [39] which could aid in capturing the complex and highly dynamic process of HDL-c’s role in cholesterol transport. For instance, the larger HDL-c particles (HDL3-HDL5) have been reported to be negatively associated with coronary artery disease (CAD), whereas the smaller particles (HDL1-HDL2) have been reported to be positively associated with CAD [21]. However, these measurements are not routinely taken in clinical and research settings for many reasons, including the wide variety of techniques used to measure the components of HDL-c, such as ultracentrifugation, nuclear magnetic resonance (NMR), high performance liquid chromatography (HPLC), tandem mass spectrometry (MS/MS), and liquid chromatography-mass spectrometry (LC-MS), to name a few [39]. Large amounts of data can be produced from these tests, given that HDL-c particles are associated with over 200 different proteins, 200 lipids, and 26 subfractions. However, there is no “gold standard” for measuring HDL-c particles and therefore results are difficult to interpret, and little research is available for comparison. Lastly, these comprehensive measurements are costly and are not covered by insurance agencies, preventing them from being conducted in a routine manner. Nevertheless, the current standards for clinical HDL-c measurement considerably limit the scientific insight that could be gained by taking additional measures of HDL-c and studying their relationship with renal function.
Ancillary findings from our study indicate that the metabolically healthy and those with MetS did not statistically differ in terms of SES or sex. Additionally, there were only small differences in race noted among the two subgroups, with the main difference being that a higher proportion of non-Hispanic (NH) white individuals were classified with MetS and a slightly lower proportion of Hispanic and NH Black individuals were classified as having MetS. Modifiable risk factors such as PA level, smoking status, and caloric intake were statistically different among the two subgroups. Fewer individuals with MetS met the recommendations for daily PA (60.85%) compared to the metabolically healthy group (73.40%), though these values were obtained from self-report questionnaires and are likely both inflated [40]. Additionally, smoking was more frequent among those with MetS (51.76%) than those without (42.66%). Metabolically healthy individuals reported consuming slightly more calories per day compared to those with MetS (2136 and 2054 kcal/day, respectively), yet they maintained a significantly lower BMI (26.81 and 32.98 kg/m2, respectively). Though diet is classically difficult to assess through self-report [41], the lower intake reported in the MetS subsample could be indicative of caloric restriction and/or greater use of dieting. It is possible that the modifiable risk factors mentioned have played a role in the development of MetS over the long-term, though without temporal data there is no way to confirm.
Strengths and Limitations
The strengths of the present study include a large, diverse sample obtained from the CDC NHANES database. The unique sample weighting procedures outlined in the NHANES survey methods and analytic guidelines allowed us to extrapolate our findings to the greater US population, increasing generalizability and power in our study. While our results are similar to recent findings by Melsom et al. [19], our study included both metabolically healthy and unhealthy individuals from a racially and ethnically diverse sample. Our study was limited by the cross-sectional nature of the data, which reduces our understanding of HDL-c’s role in the progression of CKD. Additionally, we were constrained to single-timepoint measures of eGFR and hsCRP, which should each be tested twice with 3-months and 2-weeks separation, respectively, in clinical settings. Other measures of lipid profiles such as oxidized LDL-c content and HDL-c particle size, composition, and quality were not available in the NHANES database and could have provided greater insight into the counterintuitive relationship found between HDL-c and eGFR measurements. Additionally, some data collected by NHANES researchers are self-reported, such as PA and dietary habits. Lastly, our main regression analyses were determined a priori based on prior research surrounding HDL-c and renal function. Many other analyses could have been conducted to provide differing results.
5. Conclusions
In the assessment of a large sample of individuals from the 2013–2018 NHANES datasets, we found a negative association between HDL-c and eGFR. This relationship persisted despite adjustment for confounding variables but was attenuated in the healthy and total samples when only the middle 50%, 80%, 90%, and 98% of HDL values were considered. The figures included in our study demonstrated a negative linear correlation, rather than a U-shaped relationship, between HDL-c and eGFR. Additionally, we found that the metabolically healthy and unhealthy groups did not differ by sex or SES, but modifiable risk factors such as smoking and PA were statistically different between groups. Future research efforts should focus on other measures of HDL-c, such as particle concentrations, size, and quality, to better understand the negative relationship reported between HDL-c and renal function in this study and prior published research.
Author Contributions
Conceptualization, K.A.R., L.T.R. and R.G.B.; Data curation, K.A.R.; Formal analysis, K.A.R.; Funding acquisition, R.G.B.; Investigation, K.A.R., L.T.R. and R.G.B.; Methodology, K.A.R., L.T.R. and R.G.B.; Project administration, R.G.B.; Resources, K.A.R.; Software, K.A.R. and R.G.B.; Supervision, R.G.B.; Visualization, K.A.R. and L.T.R.; Writing—original draft, K.A.R. and R.G.B.; Writing—review & editing, K.A.R., L.T.R. and R.G.B. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by Brown Foundation Fund, Baylor University.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the secondary nature of the CDC datasets.
Informed Consent Statement
Patient consent was waived due to the nature of the secondary datasets. The consent documents are posted on the CDC website.
Data Availability Statement
All data are available from the CDC at https://wwwn.cdc.gov/nchs/nhanes/ (accessed on 14 January 2022).
Acknowledgments
The faculty and staff at Baylor University.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2019; US Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2019.
- Dunaief, D.M.; Fuhrman, J.; Dunaief, J.L.; Ying, G. Glycemic and cardiovascular parameters improved in type 2 diabetes with the high nutrient density (HND) diet. Open J. Prev. Med. 2012, 2, 364–371. [Google Scholar] [CrossRef] [Green Version]
- Lim, E.L.; Hollingsworth, K.G.; Aribisala, B.S.; Chen, M.J.; Mathers, J.C.; Taylor, R. Reversal of type 2 diabetes: Normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 2011, 54, 2506–2514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDougall, J.; Thomas, L.E.; McDougall, C.; Moloney, G.; Saul, B.; Finnell, J.S.; Richardson, K.; Petersen, K.M. Effects of 7 days on an ad libitum low-fat vegan diet: The McDougall Program cohort. Nutr. J. 2014, 13, 99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnard, N.D.; Cohen, J.; Jenkins, D.J.; Turner-McGrievy, G.; Gloede, L.; Green, A.; Ferdowsian, H. A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: A randomized, controlled, 74-wk clinical trial. Am. J. Clin. Nutr. 2009, 89, 1588S–1596S. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the Metabolic Syndrome. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [Green Version]
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (adult Treatment Panel III): Final Report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Voight, B.F.; Peloso, G.M.; Orho-Melander, M.; Frikke-Schmidt, R.; Barbalic, M.; Jensen, M.K.; Hindy, G.; Hólm, H.; Ding, E.L.; Johnson, T.; et al. Plasma HDL cholesterol and risk of myocardial infarction: A mendelian randomisation study. Lancet 2012, 380, 572–580. [Google Scholar] [CrossRef] [Green Version]
- Keene, D.; Price, C.; Shun-Shin, M.J.; Francis, D.P. Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: Meta-analysis of randomised controlled trials including 117 411 patients. BMJ 2014, 349, g4379. [Google Scholar] [CrossRef] [Green Version]
- Thomas, G.; Sehgal, A.R.; Kashyap, S.R.; Srinivas, T.R.; Kirwan, J.P.; Navaneethan, S.D. Metabolic Syndrome and Kidney Disease: A Systematic Review and Meta-analysis. Clin. J. Am. Soc. Nephrol. 2011, 6, 2364–2373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.-B.; Sheng, L.-T.; Wei, W.; Guo, H.; Yang, H.; Min, X.; Guo, K.; Yang, K.; Zhang, X.; He, M.; et al. Association of blood lipid profile with incident chronic kidney disease: A Mendelian randomization study. Atherosclerosis 2020, 300, 19–25. [Google Scholar] [CrossRef]
- Lanktree, M.B.; Thériault, S.; Walsh, M.; Paré, G. HDL Cholesterol, LDL Cholesterol, and Triglycerides as Risk Factors for CKD: A Mendelian Randomization Study. Am. J. Kidney Dis. 2018, 71, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Lo, J.C.; Go, A.S.; Chandra, M.; Fan, D.; Kaysen, G.A. GFR, Body Mass Index, and Low High-Density Lipoprotein Concentration in Adults With and Without CKD. Am. J. Kidney Dis. 2007, 50, 552–558. [Google Scholar] [CrossRef]
- Navaneethan, S.D.; Schold, J.D.; Walther, C.P.; Arrigain, S.; Jolly, S.E.; Virani, S.S.; Winkelmayer, W.C.; Nally, J.V. High-density lipoprotein cholesterol and causes of death in chronic kidney disease. J. Clin. Lipidol. 2018, 12, 1061–1071.e7. [Google Scholar] [CrossRef] [PubMed]
- Bowe, B.; Xie, Y.; Xian, H.; Balasubramanian, S.; Al-Aly, Z. Low levels of high-density lipoprotein cholesterol increase the risk of incident kidney disease and its progression. Kidney Int. 2016, 89, 886–896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowe, B.; Xie, Y.; Xian, H.; Balasubramanian, S.; Zayed, M.A.; Al-Aly, Z. High Density Lipoprotein Cholesterol and the Risk of All-Cause Mortality among U.S. Veterans. Clin. J. Am. Soc. Nephrol. 2016, 11, 1784–1793. [Google Scholar] [CrossRef] [Green Version]
- Krikken, J.A.; Gansevoort, R.T.; Dullaart, R.P.F. Lower HDL-C and apolipoprotein A-I are related to higher glomerular filtration rate in subjects without kidney disease. J. Lipid Res. 2010, 51, 1982–1990. [Google Scholar] [CrossRef] [Green Version]
- Melsom, T.; Norvik, J.V.; Enoksen, I.T.; Stefansson, V.; Rismo, R.; Jenssen, T.; Solbu, M.D.; Eriksen, B.O. Association of High-Density Lipoprotein Cholesterol With GFR Decline in a General Nondiabetic Population. Kidney Int. Rep. 2021, 6, 2084–2094. [Google Scholar] [CrossRef]
- Zanoni, P.; Khetarpal, S.A.; Larach, D.B.; Hancock-Cerutti, W.F.; Millar, J.S.; Cuchel, M.; DerOhannessian, S.; Kontush, A.; Surendran, P.; Saleheen, D.; et al. Rare variant in scavenger receptor BI raises HDL cholesterol and increases risk of coronary heart disease. Science 2016, 351, 1166–1171. [Google Scholar] [CrossRef] [Green Version]
- Kwiterovich, P.O. The metabolic pathways of high-density lipoprotein, low-density lipoprotein, and triglycerides: A current review. Am. J. Cardiol. 2000, 86, 5–10. [Google Scholar] [CrossRef]
- Rosenson, R.S.; Brewer, H.B.; Ansell, B.J.; Barter, P.; Chapman, M.J.; Heinecke, J.W.; Kontush, A.; Tall, A.R.; Webb, N.R. Dysfunctional HDL and atherosclerotic cardiovascular disease. Nat. Rev. Cardiol. 2016, 13, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Ansell, B.J.; Navab, M.; Hama, S.; Kamranpour, N.; Fonarow, G.; Hough, G.; Rahmani, S.; Mottahedeh, R.; Dave, R.; Reddy, S.T.; et al. Inflammatory/Antiinflammatory Properties of High-Density Lipoprotein Distinguish Patients From Control Subjects Better Than High-Density Lipoprotein Cholesterol Levels and Are Favorably Affected by Simvastatin Treatment. Circulation 2003, 108, 2751–2756. [Google Scholar] [CrossRef] [PubMed]
- Park, K.-H.; Cho, K.-H. High-Density Lipoprotein (HDL) From Elderly and Reconstituted HDL Containing Glycated Apolipoproteins A-I Share Proatherosclerotic and Prosenescent Properties With Increased Cholesterol Influx. J. Gerontol. Ser. A 2011, 66A, 511–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention (CDC); National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire (or Examination Protocol, or Laboratory Protocol); U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Hyattsville, MD, USA, 2019. Available online: https://wwwn.cdc.gov/nchs/nhanes/ (accessed on 21 January 2022).
- Chen, T.; Clark, J.; Riddles, M.; Mohadjer, L.; Fakhouri, T. National Health and Nutrition Examination Survey, 2015–2018: Sample Design and Estimation Procedures; National Center for Health Statistics: Washington, DC, USA, 2020.
- Chen, T.; Parker, J.; Clark, J.; Shin, H.; Rammon, J.; Burt, V. National Health and Nutrition Examination Survey: Estimation Procedures, 2011–2014; National Center for Health Statistics: Washington, DC, USA, 2018.
- Johnson, C.; Dohrmann, S.; Burt, V.; Mohadjer, L. National Health and Nutrition Examination Survey: Sample Design, 2011–2014; National Center for Health Statistics: Washington, DC, USA, 2014.
- NHANES—National Health and Nutrition Examination Survey Homepage. Available online: https://www.cdc.gov/nchs/nhanes/index.htm (accessed on 21 January 2022).
- Physical Activity Guidelines for Americans. Physical Activity Guidelines Advisory Committee Report, 2019; US Department of Health and Human Services: Washington, DC, USA, 2018.
- Fang, J.; Zhang, Z.; Ayala, C.; Thompson-Paul, A.M.; Loustalot, F. Cardiovascular Health among Non-Hispanic Asian Americans: NHANES, 2011–2016. J. Am. Heart Assoc. 2019, 8, e011324. [Google Scholar] [CrossRef] [Green Version]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.; Castro, A.F.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009, 150, 604. [Google Scholar] [CrossRef] [PubMed]
- Carnuta, M.G.; Stancu, C.S.; Toma, L.; Sanda, G.M.; Niculescu, L.S.; Deleanu, M.; Popescu, A.C.; Popescu, M.R.; Vlad, A.; Dimulescu, D.R.; et al. Dysfunctional high-density lipoproteins have distinct composition, diminished anti-inflammatory potential and discriminate acute coronary syndrome from stable coronary artery disease patients. Sci. Rep. 2017, 7, 7295. [Google Scholar] [CrossRef]
- Bonizzi, A.; Piuri, G.; Corsi, F.; Cazzola, R.; Mazzucchelli, S. HDL Dysfunctionality: Clinical Relevance of Quality Rather Than Quantity. Biomedicines 2021, 9, 729. [Google Scholar] [CrossRef]
- Huang, C.-Y.; Lin, F.-Y.; Shih, C.-M.; Au, H.-K.; Chang, Y.-J.; Nakagami, H.; Morishita, R.; Chang, N.-C.; Shyu, K.-G.; Chen, J.-W. Moderate to High Concentrations of High-Density Lipoprotein From Healthy Subjects Paradoxically Impair Human Endothelial Progenitor Cells and Related Angiogenesis by Activating Rho-Associated Kinase Pathways. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 2405–2417. [Google Scholar] [CrossRef] [Green Version]
- Barter, P. Lipoprotein metabolism and CKD: Overview. Clin. Exp. Nephrol. 2014, 18, 243–246. [Google Scholar] [CrossRef]
- Reiss, A.B.; Voloshyna, I.; De Leon, J.; Miyawaki, N.; Mattana, J. Cholesterol Metabolism in CKD. Am. J. Kidney Dis. 2015, 66, 1071–1082. [Google Scholar] [CrossRef] [Green Version]
- Rysz, J.; Gluba-Brzózka, A.; Rysz-Górzyńska, M.; Franczyk, B. The Role and Function of HDL in Patients with Chronic Kidney Disease and the Risk of Cardiovascular Disease. Int. J. Mol. Sci. 2020, 21, 601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hafiane, A.; Genest, J. High density lipoproteins: Measurement techniques and potential biomarkers of cardiovascular risk. BBA Clin. 2015, 3, 175–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozemek, C.; Lavie, C.J.; Rognmo, Ø. Global physical activity levels—Need for intervention. Prog. Cardiovasc. Dis. 2019, 62, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Gemming, L.; Jiang, Y.; Swinburn, B.; Utter, J.; Mhurchu, C.N. Under-reporting remains a key limitation of self-reported dietary intake: An analysis of the 2008/09 New Zealand Adult Nutrition Survey. Eur. J. Clin. Nutr. 2014, 68, 259–264. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).