Effects of Diet and Exercise on Metabolic Parameters and Health in Moderate to Advanced Kidney Disease
Abstract
:1. Introduction
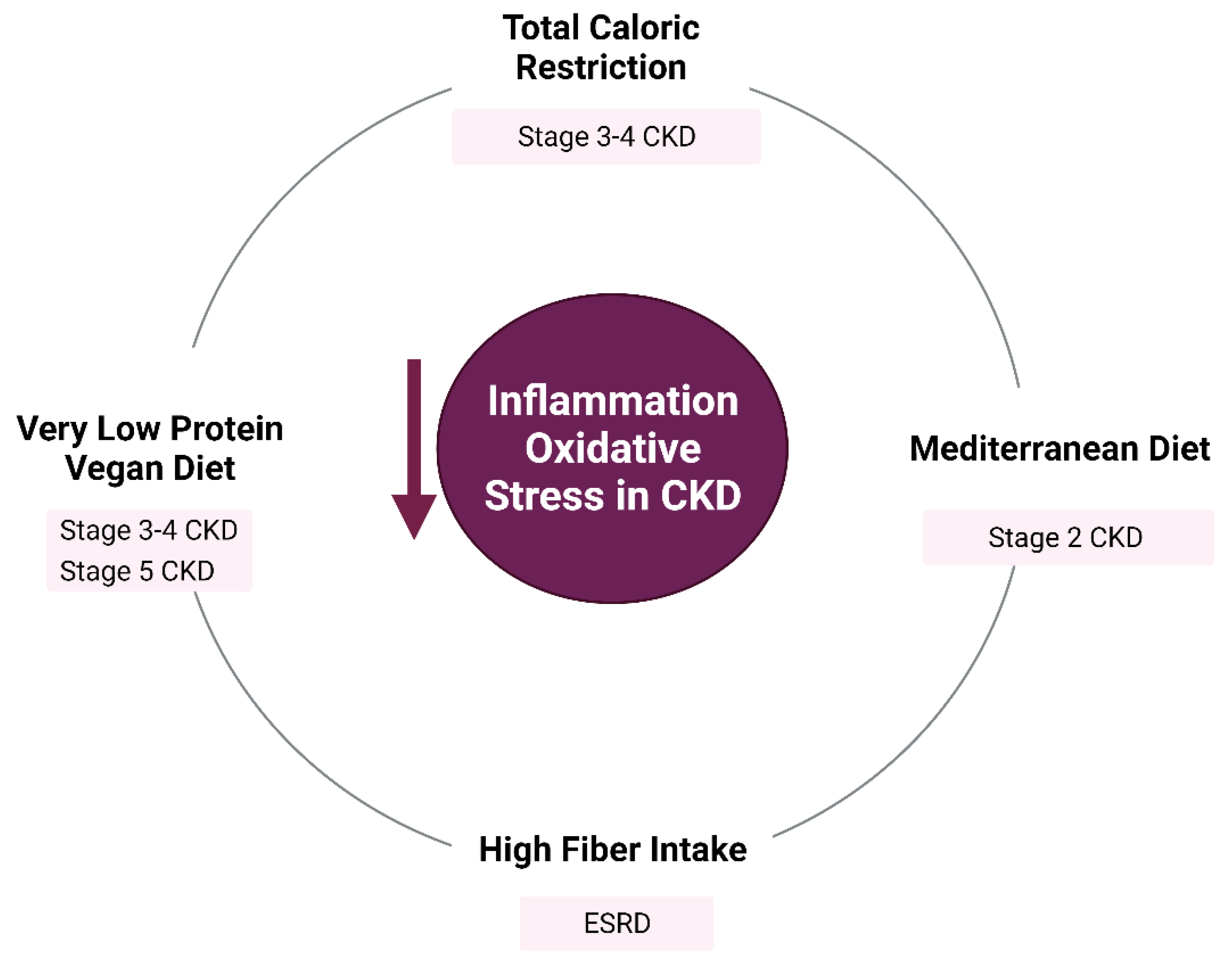
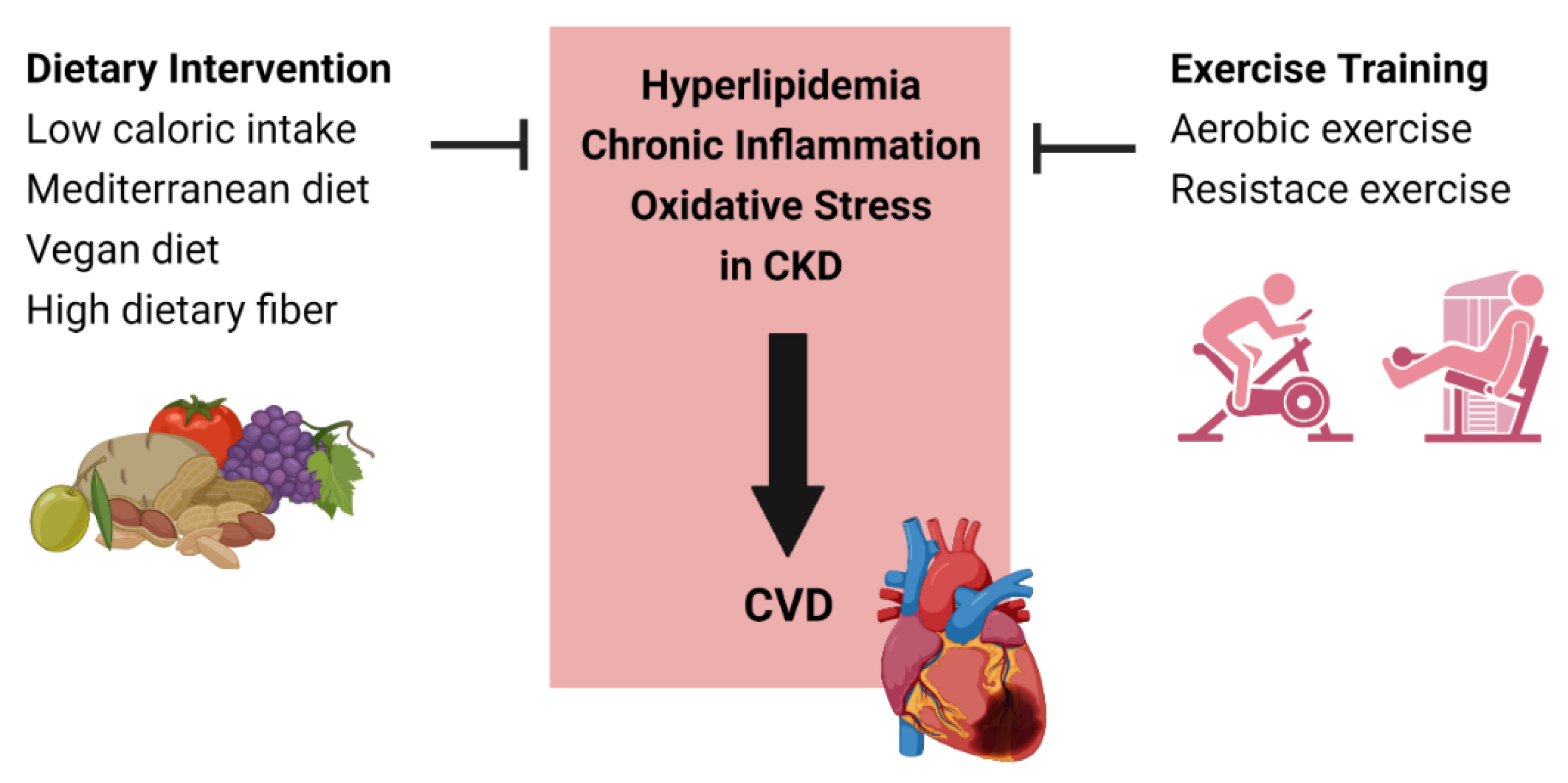
2. Diet
2.1. Total Caloric Intake
2.2. Dietary Patterns
2.2.1. Mediterranean Diet
2.2.2. Vegan Diet
2.3. Dietary Fiber
3. Exercise
3.1. Effects of Exercise on Body Composition
3.2. Exercise and Dysmetabolism of Kidney Disease
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Go, A.S.; Chertow, G.M.; Fan, D.; McCulloch, C.E.; Hsu, C.Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 2004, 351, 1296–1305. [Google Scholar] [CrossRef] [PubMed]
- Hager, M.R.; Narla, A.D.; Tannock, L.R. Dyslipidemia in patients with chronic kidney disease. Rev. Endocr. Metab. Disord. 2017, 18, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Romão, J.E., Jr.; Haiashi, A.R.; Elias, R.M.; Luders, C.; Ferraboli, R.; Castro, M.C.; Abensur, H. Positive acute-phase inflammatory markers in different stages of chronic kidney disease. Am. J. Nephrol. 2006, 26, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Ramos, L.F.; Shintani, A.; Ikizler, T.A.; Himmelfarb, J. Oxidative Stress and Inflammation Are Associated with Adiposity in Moderate to Severe CKD. J. Am. Soc. Nephrol. 2008, 19, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Gupta, J.; Mitra, N.; Kanetsky, P.A.; Devaney, J.; Wing, M.R.; Reilly, M.; Shah, V.O.; Balakrishnan, V.S.; Guzman, N.J.; Girndt, M.; et al. Association between albuminuria, kidney function, and inflammatory biomarker profile in CKD in CRIC. Clin. J. Am. Soc. Nephrol. 2012, 7, 1938–1946. [Google Scholar] [CrossRef] [Green Version]
- Liakopoulos, V.; Roumeliotis, S.; Gorny, X.; Dounousi, E.; Mertens, P.R. Oxidative Stress in Hemodialysis Patients: A Review of the Literature. Oxid. Med. Cell. Longev. 2017, 2017, 3081856. [Google Scholar] [CrossRef]
- Vaziri, N.D. Roles of oxidative stress and antioxidant therapy in chronic kidney disease and hypertension. Curr. Opin. Nephrol. Hypertens 2004, 13, 93–99. [Google Scholar] [CrossRef]
- Gomes, E.C.; Silva, A.N.; de Oliveira, M.R. Oxidants, antioxidants, and the beneficial roles of exercise-induced production of reactive species. Oxid. Med. Cell. Longev. 2012, 2012, 756132. [Google Scholar] [CrossRef]
- Oberg, B.P.; McMenamin, E.; Lucas, F.L.; McMonagle, E.; Morrow, J.; Ikizler, T.A.; Himmelfarb, J. Increased prevalence of oxidant stress and inflammation in patients with moderate to severe chronic kidney disease. Kidney Int. 2004, 65, 1009–1016. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Bello, J.A.; Gómez-Díaz, R.A.; Contreras-Rodríguez, A.; Talavera, J.O.; Mondragón-González, R.; Sanchez-Barbosa, L.; Diaz-Flores, M.; Valladares-Salgado, A.; Gallardo, J.M.; Aguilar-Kitsu, A.; et al. Carotid intima media thickness, oxidative stress, and inflammation in children with chronic kidney disease. Pediatr. Nephrol. 2014, 29, 273–281. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hwang, W.J.; Kang, S.J. Interventions to Reduce the Risk of Cardiovascular Disease among Workers: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public. Health 2020, 17, 2267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraus, W.E.; Houmard, J.A.; Duscha, B.D.; Knetzger, K.J.; Wharton, M.B.; McCartney, J.S.; Bales, C.W.; Henes, S.; Samsa, G.P.; Otvos, J.D.; et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N. Engl. J. Med. 2002, 347, 1483–1492. [Google Scholar] [CrossRef]
- Zheng, G.; Qiu, P.; Xia, R.; Lin, H.; Ye, B.; Tao, J.; Chen, L. Effect of Aerobic Exercise on Inflammatory Markers in Healthy Middle-Aged and Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Aging Neurosci. 2019, 11, 98. [Google Scholar] [CrossRef] [Green Version]
- Cena, H.; Calder, P.C. Defining a Healthy Diet: Evidence for The Role of Contemporary Dietary Patterns in Health and Disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef] [Green Version]
- Zarraga, I.G.; Schwarz, E.R. Impact of dietary patterns and interventions on cardiovascular health. Circulation 2006, 114, 961–973. [Google Scholar] [CrossRef] [PubMed]
- Heidemann, C.; Schulze, M.B.; Franco, O.H.; van Dam, R.M.; Mantzoros, C.S.; Hu, F.B. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation 2008, 118, 230–237. [Google Scholar] [CrossRef]
- Ikizler, T.A.; Robinson-Cohen, C.; Ellis, C.; Headley, S.A.E.; Tuttle, K.; Wood, R.J.; Evans, E.E.; Milch, C.M.; Moody, K.A.; Germain, M.; et al. Metabolic Effects of Diet and Exercise in Patients with Moderate to Severe CKD: A Randomized Clinical Trial. J. Am. Soc. Nephrol. 2018, 29, 250–259. [Google Scholar] [CrossRef]
- Mekki, K.; Bouzidi-bekada, N.; Kaddous, A.; Bouchenak, M. Mediterranean diet improves dyslipidemia and biomarkers in chronic renal failure patients. Food Funct. 2010, 1, 110–115. [Google Scholar] [CrossRef]
- Bergesio, F.; Monzani, G.; Guasparini, A.; Ciuti, R.; Gallucci, M.; Cristofano, C.; Castrignano, E.; Cupisti, A.; Barsotti, G.; Marcucci, R.; et al. Cardiovascular risk factors in severe chronic renal failure: The role of dietary treatment. Clin. Nephrol. 2005, 64, 103–112. [Google Scholar] [CrossRef]
- Garneata, L.; Stancu, A.; Dragomir, D.; Stefan, G.; Mircescu, G. Ketoanalogue-Supplemented Vegetarian Very Low-Protein Diet and CKD Progression. J. Am. Soc. Nephrol. 2016, 27, 2164–2176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlsen, M.H.; Halvorsen, B.L.; Holte, K.; Bøhn, S.K.; Dragland, S.; Sampson, L.; Willey, C.; Senoo, H.; Umezono, Y.; Sanada, C.; et al. The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutr. J. 2010, 9, 3. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, L.S.; Cho, W.-K.; Kim, Y. Obesity and chronic kidney disease: A population-based study among South Koreans. PLoS ONE 2018, 13, e0193559. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Obesity and Overweight. 2022. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 17 January 2022).
- Keaney, J.F., Jr.; Larson, M.G.; Vasan, R.S.; Wilson, P.W.; Lipinska, I.; Corey, D.; Massaro, J.M.; Sutherland, P.; Vita, J.A.; Benjamin, E.J. Obesity and systemic oxidative stress: Clinical correlates of oxidative stress in the Framingham Study. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 434–439. [Google Scholar] [CrossRef] [Green Version]
- Timpson, N.J.; Nordestgaard, B.G.; Harbord, R.M.; Zacho, J.; Frayling, T.M.; Tybjærg-Hansen, A.; Smith, G.D. C-reactive protein levels and body mass index: Elucidating direction of causation through reciprocal Mendelian randomization. Int. J. Obes. 2011, 35, 300–308. [Google Scholar] [CrossRef] [Green Version]
- Cohen, E.; Margalit, I.; Shochat, T.; Goldberg, E.; Krause, I. Markers of Chronic Inflammation in Overweight and Obese Individuals and the Role of Gender: A Cross-Sectional Study of a Large Cohort. J. Inflamm. Res. 2021, 14, 567–573. [Google Scholar] [CrossRef]
- Choi, J.; Joseph, L.; Pilote, L. Obesity and C-reactive protein in various populations: A systematic review and meta-analysis. Obes. Rev. 2013, 14, 232–244. [Google Scholar] [CrossRef]
- Wing, M.R.; Yang, W.; Teal, V.; Navaneethan, S.; Tao, K.; Ojo, A.; Guzman, N.N.; Reilly, M.; Wolman, M.; Rosas, S.E.; et al. Race modifies the association between adiposity and inflammation in patients with chronic kidney disease: Findings from the chronic renal insufficiency cohort study. Obesity 2014, 22, 1359–1366. [Google Scholar] [CrossRef] [Green Version]
- Kraus, W.E.; Bhapkar, M.; Huffman, K.M.; Pieper, C.F.; Krupa Das, S.; Redman, L.M.; Villareal, D.T.; Rochon, J.; Roberts, S.B.; Ravussin, E.; et al. 2 years of calorie restriction and cardiometabolic risk (CALERIE): Exploratory outcomes of a multicentre, phase 2, randomised controlled trial. Lancet Diabetes Endocrinol. 2019, 7, 673–683. [Google Scholar] [CrossRef]
- Harvie, M.N.; Pegington, M.; Mattson, M.P.; Frystyk, J.; Dillon, B.; Evans, G.; Cuzick, J.; Jebb, S.A.; Martin, B.; Cutler, R.G.; et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: A randomized trial in young overweight women. Int. J. Obes. 2011, 35, 714–727. [Google Scholar] [CrossRef] [Green Version]
- Dandona, P.; Mohanty, P.; Ghanim, H.; Aljada, A.; Browne, R.; Hamouda, W.; Prabhala, A.; Afzal, A.; Garg, R. The suppressive effect of dietary restriction and weight loss in the obese on the generation of reactive oxygen species by leukocytes, lipid peroxidation, and protein carbonylation. J. Clin. Endocrinol. Metab. 2001, 86, 355–362. [Google Scholar]
- Aydemir, N.; Pike, M.M.; Alsouqi, A.; Headley, S.A.E.; Tuttle, K.; Evans, E.E.; Milch, C.M.; Moody, K.A.; Germain, M.; Lipworth, L.; et al. Effects of diet and exercise on adipocytokine levels in patients with moderate to severe chronic kidney disease. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1375–1381. [Google Scholar] [CrossRef]
- Lambert, K.; Beer, J.; Dumont, R.; Hewitt, K.; Manley, K.; Meade, A.; Salamon, K.; Campbell, K. Weight management strategies for those with chronic kidney disease: A consensus report from the Asia Pacific Society of Nephrology and Australia and New Zealand Society of Nephrology 2016 renal dietitians meeting. Nephrology 2018, 23, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Ikizler, T.A. Optimal nutrition in hemodialysis patients. Adv. Chronic. Kidney Dis. 2013, 20, 181–189. [Google Scholar] [CrossRef] [Green Version]
- Soltani, S.; Jayedi, A.; Shab-Bidar, S.; Becerra-Tomás, N.; Salas-Salvadó, J. Adherence to the Mediterranean Diet in Relation to All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2019, 10, 1029–1039. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef]
- Steckhan, N.; Hohmann, C.-D.; Kessler, C.; Dobos, G.; Michalsen, A.; Cramer, H. Effects of different dietary approaches on inflammatory markers in patients with metabolic syndrome: A systematic review and meta-analysis. Nutrition 2016, 32, 338–348. [Google Scholar] [CrossRef]
- Chrysohoou, C.; Panagiotakos, D.B.; Pitsavos, C.; Das, U.N.; Stefanadis, C. Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: The ATTICA Study. J. Am. Coll. Cardiol. 2004, 44, 152–158. [Google Scholar] [CrossRef] [Green Version]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [Green Version]
- Huang, X.; Jiménez-Moleón, J.J.; Lindholm, B.; Cederholm, T.; Arnlöv, J.; Risérus, U.; Sjögren, P.; Carrero, J.J. Mediterranean diet, kidney function, and mortality in men with CKD. Clin. J. Am. Soc. Nephrol. 2013, 8, 1548–1555. [Google Scholar] [CrossRef] [Green Version]
- Smyth, A.; Griffin, M.; Yusuf, S.; Mann, J.F.; Reddan, D.; Canavan, M.; Newell, J.; O’Donnell, M. Diet and Major Renal Outcomes: A Prospective Cohort Study. The NIH-AARP Diet and Health Study. The NIH-AARP Diet and Health Study. J. Ren. Nutr 2016, 26, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Fung, T.T.; Hu, F.B.; Curhan, G.C. Association of Dietary Patterns With Albuminuria and Kidney Function Decline in Older White Women: A Subgroup Analysis From the Nurses’ Health Study. Am. J. Kidney Dis. 2011, 57, 245–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banerjee, T.; Crews, D.C.; Tuot, D.S.; Pavkov, M.E.; Burrows, N.R.; Stack, A.G.; Saran, R.; Bragg-Gresham, J.; Powe, N.R. Poor accordance to a DASH dietary pattern is associated with higher risk of ESRD among adults with moderate chronic kidney disease and hypertension. Kidney Int. 2019, 95, 1433–1442. [Google Scholar] [CrossRef] [Green Version]
- Saglimbene, V.M.; Wong, G.; Craig, J.C.; Ruospo, M.; Palmer, S.C.; Campbell, K.; Garcia-Larsen, V.; Natale, P.; Teixeira-Pinto, A.; Carrero, J.-J.; et al. The Association of Mediterranean and DASH Diets with Mortality in Adults on Hemodialysis: The DIET-HD Multinational Cohort Study. J. Am. Soc. Nephrol. 2018, 29, 1741–1751. [Google Scholar] [CrossRef] [PubMed]
- Bowden, K.; Gray, N.A.; Swanepoel, E.; Wright, H.H. A Mediterranean lifestyle is associated with favourable cardiometabolic markers in people with non-dialysis dependent chronic kidney disease. J. Nutr. Sci. 2021, 10, e42. [Google Scholar] [CrossRef]
- Picard, K.; Senior, P.A.; Adame Perez, S.; Jindal, K.; Richard, C.; Mager, D.R. Low Mediterranean Diet scores are associated with reduced kidney function and health related quality of life but not other markers of cardiovascular risk in adults with diabetes and chronic kidney disease. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 1445–1453. [Google Scholar] [CrossRef]
- Pronczuk, A.; Kipervarg, Y.; Hayes, K.C. Vegetarians have higher plasma alpha-tocopherol relative to cholesterol than do nonvegetarians. J. Am. Coll. Nutr. 1992, 11, 50–55. [Google Scholar] [CrossRef]
- Wang, F.; Zheng, J.; Yang, B.; Jiang, J.; Fu, Y.; Li, D. Effects of Vegetarian Diets on Blood Lipids: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2015, 4, e002408. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.K.; Cho, S.W.; Park, Y.K. Long-term vegetarians have low oxidative stress, body fat, and cholesterol levels. Nutr. Res. Pract. 2012, 6, 155–161. [Google Scholar] [CrossRef] [Green Version]
- Matsumoto, S.; Beeson, W.L.; Shavlik, D.J.; Siapco, G.; Jaceldo-Siegl, K.; Fraser, G.; Knutsen, S.F. Association between vegetarian diets and cardiovascular risk factors in non-Hispanic white participants of the Adventist Health Study-2. J. Nutr. Sci. 2019, 8, e6. [Google Scholar] [CrossRef] [Green Version]
- Menzel, J.; Biemann, R.; Longree, A.; Isermann, B.; Mai, K.; Schulze, M.B.; Abraham, K.; Weikert, C. Associations of a vegan diet with inflammatory biomarkers. Sci. Rep. 2020, 10, 1933. [Google Scholar] [CrossRef]
- Shah, B.; Newman, J.D.; Woolf, K.; Ganguzza, L.; Guo, Y.; Allen, N.; Zhong, J.; Fisher, E.A.; Slater, J. Anti-Inflammatory Effects of a Vegan Diet Versus the American Heart Association-Recommended Diet in Coronary Artery Disease Trial. J. Am. Heart Assoc. 2018, 7, e011367. [Google Scholar] [CrossRef] [Green Version]
- Haghighatdoost, F.; Bellissimo, N.; Totosy de Zepetnek, J.O.; Rouhani, M.H. Association of vegetarian diet with inflammatory biomarkers: A systematic review and meta-analysis of observational studies. Public Health Nutr. 2017, 20, 2713–2721. [Google Scholar] [CrossRef]
- Kahleova, H.; Matoulek, M.; Malinska, H.; Oliyarnik, O.; Kazdova, L.; Neskudla, T.; Skoch, A.; Hajek, M.; Hill, M.; Kahle, M.; et al. Vegetarian diet improves insulin resistance and oxidative stress markers more than conventional diet in subjects with Type 2 diabetes. Diabet. Med. 2011, 28, 549–559. [Google Scholar] [CrossRef] [Green Version]
- Ornish, D.; Brown, S.E.; Billings, J.H.; Scherwitz, L.W.; Armstrong, W.T.; Ports, T.A.; McLanahan, S.M.; Kirkeeide, R.L.; Gould, K.L.; Brand, R.J. Can lifestyle changes reverse coronary heart disease?: The Lifestyle Heart Trial. Lancet 1990, 336, 129–133. [Google Scholar] [CrossRef]
- Crowe, F.L.; Appleby, P.N.; Travis, R.C.; Key, T.J. Risk of hospitalization or death from ischemic heart disease among British vegetarians and nonvegetarians: Results from the EPIC-Oxford cohort study. Am. J. Clin. Nutr. 2013, 97, 597–603. [Google Scholar] [CrossRef] [Green Version]
- Orlich, M.J.; Singh, P.N.; Sabaté, J.; Jaceldo-Siegl, K.; Fan, J.; Knutsen, S.; Beeson, W.L.; Fraser, G.E. Vegetarian Dietary Patterns and Mortality in Adventist Health Study 2. JAMA Intern. Med. 2013, 173, 1230–1238. [Google Scholar] [CrossRef]
- Wu, T.T.; Chang, C.Y.; Hsu, W.M.; Wang, I.K.; Hsu, C.H.; Cheng, S.H.; Liang, C.C.; Chang, C.T.; Huang, C.C. Nutritional status of vegetarians on maintenance haemodialysis. Nephrology 2011, 16, 582–587. [Google Scholar] [CrossRef]
- Patel, K.P.; Luo, F.J.G.; Plummer, N.S.; Hostetter, T.H.; Meyer, T.W. The production of p-cresol sulfate and indoxyl sulfate in vegetarians versus omnivores. Clin. J. Am. Soc. Nephrol. CJASN 2012, 7, 982–988. [Google Scholar] [CrossRef]
- Moe, S.M.; Zidehsarai, M.P.; Chambers, M.A.; Jackman, L.A.; Radcliffe, J.S.; Trevino, L.L.; Donahue, S.E.; Asplin, J.R. Vegetarian compared with meat dietary protein source and phosphorus homeostasis in chronic kidney disease. Clin. J. Am. Soc. Nephrol. 2011, 6, 257–264. [Google Scholar] [CrossRef] [Green Version]
- Clegg, D.J.; Gallant, K.M.H. Plant-Based Diets in CKD. Clin. J. Am. Soc. Nephrol. 2019, 14, 141–143. [Google Scholar] [CrossRef] [PubMed]
- Goraya, N.; Simoni, J.; Jo, C.-H.; Wesson, D.E. A Comparison of Treating Metabolic Acidosis in CKD Stage 4 Hypertensive Kidney Disease with Fruits and Vegetables or Sodium Bicarbonate. Clin. J. Am. Soc. Nephrol. 2013, 8, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Tyson, C.C.; Lin, P.-H.; Corsino, L.; Batch, B.C.; Allen, J.; Sapp, S.; Barnhart, H.; Nwankwo, C.; Burroughs, J.; Svetkey, L.P. Short-term effects of the DASH diet in adults with moderate chronic kidney disease: A pilot feeding study. Clin. Kidney J. 2016, 9, 592–598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernier-Jean, A.; Wong, G.; Saglimbene, V.; Ruospo, M.; Palmer, S.C.; Natale, P.; Garcia-Larsen, V.; Johnson, D.W.; Tonelli, M.; Hegbrant, J.; et al. Dietary Potassium Intake and All-Cause Mortality in Adults Treated with Hemodialysis. Clin. J. Am. Soc. Nephrol. 2021, 16, 1851–1861. [Google Scholar] [CrossRef] [PubMed]
- Aparicio, M.; Chauveau, P.; Précigout, V.; Bouchet, J.L.; Lasseur, C.; Combe, C. Nutrition and outcome on renal replacement therapy of patients with chronic renal failure treated by a supplemented very low protein diet. J. Am. Soc. Nephrol. 2000, 11, 708–716. [Google Scholar] [CrossRef]
- Gluba-Brzózka, A.; Franczyk, B.; Rysz, J. Vegetarian Diet in Chronic Kidney Disease-A Friend or Foe. Nutrients 2017, 9, 374. [Google Scholar] [CrossRef]
- Barsotti, G.; Morelli, E.; Cupisti, A.; Meola, M.; Dani, L.; Giovannetti, S. A low-nitrogen low-phosphorus Vegan diet for patients with chronic renal failure. Nephron 1996, 74, 390–394. [Google Scholar] [CrossRef]
- Di Iorio, B.; Di Micco, L.; Torraca, S.; Sirico, M.L.; Russo, L.; Pota, A.; Mirenghi, F.; Russo, D. Acute effects of very-low-protein diet on FGF23 levels: A randomized study. Clin. J. Am. Soc. Nephrol. 2012, 7, 581–587. [Google Scholar] [CrossRef]
- Fujii, H.; Iwase, M.; Ohkuma, T.; Ogata-Kaizu, S.; Ide, H.; Kikuchi, Y.; Idewaki, Y.; Joudai, T.; Hirakawa, Y.; Uchida, K.; et al. Impact of dietary fiber intake on glycemic control, cardiovascular risk factors and chronic kidney disease in Japanese patients with type 2 diabetes mellitus: The Fukuoka Diabetes Registry. Nutr. J. 2013, 12, 159. [Google Scholar] [CrossRef] [Green Version]
- Barber, T.M.; Kabisch, S.; Pfeiffer, A.F.H.; Weickert, M.O. The Health Benefits of Dietary Fibre. Nutrients 2020, 12, 3209. [Google Scholar] [CrossRef]
- Ma, Y.; Griffith, J.A.; Chasan-Taber, L.; Olendzki, B.C.; Jackson, E.; Stanek, E.J., 3rd; Li, W.; Pagoto, S.L.; Hafner, A.R.; Ockene, I.S. Association between dietary fiber and serum C-reactive protein. Am. J. Clin. Nutr. 2006, 83, 760–766. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Kopple, J.D.; Deepak, S.; Block, D.; Block, G. Food intake characteristics of hemodialysis patients as obtained by food frequency questionnaire. J. Ren. Nutr. 2002, 12, 17–31. [Google Scholar] [CrossRef] [Green Version]
- Lu, L.; Huang, Y.F.; Wang, M.Q.; Chen, D.X.; Wan, H.; Wei, L.B.; Xiao, W. Dietary fiber intake is associated with chronic kidney disease (CKD) progression and cardiovascular risk, but not protein nutritional status, in adults with CKD. Asia Pac. J. Clin. Nutr. 2017, 26, 598–605. [Google Scholar]
- Raj Krishnamurthy, V.M.; Wei, G.; Baird, B.C.; Murtaugh, M.; Chonchol, M.B.; Raphael, K.L.; Greene, T.; Beddhu, S. High dietary fiber intake is associated with decreased inflammation and all-cause mortality in patients with chronic kidney disease. Kidney Int. 2012, 81, 300–306. [Google Scholar] [CrossRef] [Green Version]
- Shen, Q.; Zhao, L.; Tuohy, K.M. High-level dietary fibre up-regulates colonic fermentation and relative abundance of saccharolytic bacteria within the human faecal microbiota in vitro. Eur. J. Nutr. 2012, 51, 693–705. [Google Scholar] [CrossRef]
- Rossi, M.; Johnson, D.W.; Xu, H.; Carrero, J.J.; Pascoe, E.; French, C.; Campbell, K.L. Dietary protein-fiber ratio associates with circulating levels of indoxyl sulfate and p-cresyl sulfate in chronic kidney disease patients. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 860–865. [Google Scholar] [CrossRef]
- Salmean, Y.A.; Segal, M.S.; Palii, S.P.; Dahl, W.J. Fiber supplementation lowers plasma p-cresol in chronic kidney disease patients. J. Ren. Nutr. 2015, 25, 316–320. [Google Scholar] [CrossRef] [Green Version]
- Camerotto, C.; Cupisti, A.; D’Alessandro, C.; Muzio, F.; Gallieni, M. Dietary Fiber and Gut Microbiota in Renal Diets. Nutrients 2019, 11, 2149. [Google Scholar] [CrossRef] [Green Version]
- Meijers, B.K.; De Preter, V.; Verbeke, K.; Vanrenterghem, Y.; Evenepoel, P. p-Cresyl sulfate serum concentrations in haemodialysis patients are reduced by the prebiotic oligofructose-enriched inulin. Nephrol. Dial. Transplant. 2010, 25, 219–224. [Google Scholar] [CrossRef] [Green Version]
- Sirich, T.L.; Plummer, N.S.; Gardner, C.D.; Hostetter, T.H.; Meyer, T.W. Effect of increasing dietary fiber on plasma levels of colon-derived solutes in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2014, 9, 1603–1610. [Google Scholar] [CrossRef] [Green Version]
- Pasman, W.J.; Saris, W.H.; Wauters, M.A.; Westerterp-Plantenga, M.S. Effect of one week of fibre supplementation on hunger and satiety ratings and energy intake. Appetite 1997, 29, 77–87. [Google Scholar] [CrossRef] [Green Version]
- Desmeules, S.; Lévesque, R.; Jaussent, I.; Leray-Moragues, H.; Chalabi, L.; Canaud, B. Creatinine index and lean body mass are excellent predictors of long-term survival in haemodiafiltration patients. Nephrol. Dial. Transplant. 2004, 19, 1182–1189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sietsema, K.E.; Amato, A.; Adler, S.G.; Brass, E.P. Exercise capacity as a predictor of survival among ambulatory patients with end-stage renal disease. Kidney Int. 2004, 65, 719–724. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thorogood, A.; Mottillo, S.; Shimony, A.; Filion, K.B.; Joseph, L.; Genest, J.; Pilote, L.; Poirier, P.; Schiffrin, E.L.; Eisenberg, M.J. Isolated aerobic exercise and weight loss: A systematic review and meta-analysis of randomized controlled trials. Am. J. Med. 2011, 124, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Wen, H.; Wang, L. Reducing effect of aerobic exercise on blood pressure of essential hypertensive patients: A meta-analysis. Medicine 2017, 96, e6150. [Google Scholar] [CrossRef] [PubMed]
- Wood, G.; Taylor, E.; Ng, V.; Murrell, A.; Patil, A.; van der Touw, T.; Sigal, R.; Wolden, M.; Smart, N. Determining the effect size of aerobic exercise training on the standard lipid profile in sedentary adults with three or more metabolic syndrome factors: A systematic review and meta-analysis of randomised controlled trials. Br. J. Sports Med. 2021. [Google Scholar] [CrossRef]
- Pischon, T.; Hankinson, S.E.; Hotamisligil, G.S.; Rifai, N.; Rimm, E.B. Leisure-time physical activity and reduced plasma levels of obesity-related inflammatory markers. Obes. Res. 2003, 11, 1055–1064. [Google Scholar] [CrossRef]
- Berggren, J.R.; Hulver, M.W.; Dohm, G.L.; Houmard, J.A. Weight loss and exercise: Implications for muscle lipid metabolism and insulin action. Med. Sci. Sports Exerc. 2004, 36, 1191–1195. [Google Scholar] [CrossRef]
- Shaw, C.S.; Clark, J.; Wagenmakers, A.J. The effect of exercise and nutrition on intramuscular fat metabolism and insulin sensitivity. Annu. Rev. Nutr. 2010, 30, 13–34. [Google Scholar] [CrossRef]
- Willey, K.A.; Singh, M.A. Battling insulin resistance in elderly obese people with type 2 diabetes: Bring on the heavy weights. Diabetes Care 2003, 26, 1580–1588. [Google Scholar] [CrossRef] [Green Version]
- Ballor, D.L.; Keesey, R.E. A meta-analysis of the factors affecting exercise-induced changes in body mass, fat mass and fat-free mass in males and females. Int. J. Obes. 1991, 15, 717–726. [Google Scholar] [PubMed]
- Willis, L.H.; Slentz, C.A.; Bateman, L.A.; Shields, A.T.; Piner, L.W.; Bales, C.W.; Houmard, J.A.; Kraus, W.E. Effects of aerobic and/or resistance training on body mass and fat mass in overweight or obese adults. J. Appl. Physiol. 2012, 113, 1831–1837. [Google Scholar] [CrossRef] [PubMed]
- Moinuddin, I.; Leehey, D.J. A comparison of aerobic exercise and resistance training in patients with and without chronic kidney disease. Adv. Chronic. Kidney Dis. 2008, 15, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.K.; Vaziri, N.D.; Barnard, R.J. Effect of diet and exercise intervention on blood pressure, insulin, oxidative stress, and nitric oxide availability. Circulation 2002, 106, 2530–2532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abramson, J.L.; Vaccarino, V. Relationship between physical activity and inflammation among apparently healthy middle-aged and older US adults. Arch. Intern. Med. 2002, 162, 1286–1292. [Google Scholar] [CrossRef] [Green Version]
- Esposito, K.; Pontillo, A.; Di Palo, C.; Giugliano, G.; Masella, M.; Marfella, R.; Giugliano, D. Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: A randomized trial. JAMA 2003, 289, 1799–1804. [Google Scholar] [CrossRef] [Green Version]
- Soukup, J.T.; Kovaleski, J.E. A review of the effects of resistance training for individuals with diabetes mellitus. Diabetes Educ. 1993, 19, 307–312. [Google Scholar] [CrossRef]
- Gacitua, T.; Karachon, L.; Romero, E.; Parra, P.; Poblete, C.; Russell, J.; Rodrigo, R. Effects of resistance training on oxidative stress-related biomarkers in metabolic diseases: A review. Sport Sci. Health 2018, 14, 1–7. [Google Scholar] [CrossRef]
- Cerqueira, É.; Marinho, D.A.; Neiva, H.P.; Lourenço, O. Inflammatory Effects of High and Moderate Intensity Exercise—A Systematic Review. Front. Physiol. 2020, 10, 1550. [Google Scholar] [CrossRef]
- Konstantinidou, E.; Koukouvou, G.; Kouidi, E.; Deligiannis, A.; Tourkantonis, A. Exercise training in patients with end-stage renal disease on hemodialysis: Comparison of three rehabilitation programs. J. Rehabil. Med. 2002, 34, 40–45. [Google Scholar] [CrossRef] [Green Version]
- Castaneda, C.; Gordon, P.L.; Uhlin, K.L.; Levey, A.S.; Kehayias, J.J.; Dwyer, J.T.; Fielding, R.A.; Roubenoff, R.; Singh, M.F. Resistance training to counteract the catabolism of a low-protein diet in patients with chronic renal insufficiency. A randomized, controlled trial. Ann. Intern. Med. 2001, 135, 965–976. [Google Scholar] [CrossRef]
- Pechter, Ü.; Ots, M.; Mesikepp, S.; Zilmer, K.; Kullissaar, T.; Vihalemm, T.; Zilmer, M.; Maaroos, J. Beneficial effects of water-based exercise in patients with chronic kidney disease. Int. J. Rehabil. Res. 2003, 26, 153–156. [Google Scholar]
- Mazurek, T.; Zhang, L.; Zalewski, A.; Mannion, J.D.; Diehl, J.T.; Arafat, H.; Sarov-Blat, L.; O’Brien, S.; Keiper, E.A.; Johnson, A.G. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 2003, 108, 2460–2466. [Google Scholar] [CrossRef] [Green Version]
- Yu, N.; Ruan, Y.; Gao, X.; Sun, J. Systematic Review and Meta-Analysis of Randomized, Controlled Trials on the Effect of Exercise on Serum Leptin and Adiponectin in Overweight and Obese Individuals. Horm. Metab. Res. 2017, 49, 164–173. [Google Scholar] [CrossRef] [Green Version]
- Vanden Wyngaert, K.; Craenenbroeck, A.; Biesen, W.; Dhondt, A.; Tanghe, A.; Ginckel, A.; Celie, B.; Calders, P. The effects of aerobic exercise on eGFR, blood pressure and VO2peak in patients with chronic kidney disease stages 3–4: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0203662. [Google Scholar] [CrossRef]
- Greenwood, S.A.; Koufaki, P.; Mercer, T.H.; MacLaughlin, H.L.; Rush, R.; Lindup, H.; O’Connor, E.; Jones, C.; Hendry, B.M.; Macdougall, I.C.; et al. Effect of exercise training on estimated GFR, vascular health, and cardiorespiratory fitness in patients with CKD: A pilot randomized controlled trial. Am. J. Kidney Dis. 2015, 65, 425–434. [Google Scholar] [CrossRef]
- Baria, F.; Kamimura, M.A.; Aoike, D.T.; Ammirati, A.; Leister Rocha, M.; de Mello, M.T.; Cuppari, L. Randomized controlled trial to evaluate the impact of aerobic exercise on visceral fat in overweight chronic kidney disease patients. Nephrol. Dial. Transplant. 2014, 29, 857–864. [Google Scholar] [CrossRef]
- Afshar, R.; Shegarfy, L.; Shavandi, N.; Sanavi, S. Effects of aerobic exercise and resistance training on lipid profiles and inflammation status in patients on maintenance hemodialysis. Indian J. Nephrol. 2010, 20, 185–189. [Google Scholar]
- Castaneda, C.; Gordon, P.L.; Parker, R.C.; Uhlin, K.L.; Roubenoff, R.; Levey, A.S. Resistance training to reduce the malnutrition-inflammation complex syndrome of chronic kidney disease. Am. J. Kidney Dis. 2004, 43, 607–616. [Google Scholar] [CrossRef]
- Koufaki, P.; Nash, P.F.; Mercer, T.H. Assessing the efficacy of exercise training in patients with chronic disease. Med. Sci. Sports Exerc. 2002, 34, 1234–1241. [Google Scholar] [CrossRef]
- Dong, J.; Sundell, M.B.; Pupim, L.B.; Wu, P.; Shintani, A.; Ikizler, T.A. The effect of resistance exercise to augment long-term benefits of intradialytic oral nutritional supplementation in chronic hemodialysis patients. J. Ren. Nutr. Off. J. Counc. Ren. Nutr. Natl. Kidney Found. 2011, 21, 149–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johansen, K.L.; Painter, P.L.; Sakkas, G.K.; Gordon, P.; Doyle, J.; Shubert, T. Effects of resistance exercise training and nandrolone decanoate on body composition and muscle function among patients who receive hemodialysis: A randomized, controlled trial. J. Am. Soc. Nephrol. 2006, 17, 2307–2314. [Google Scholar] [CrossRef] [PubMed]
- Cheema, B.; Abas, H.; Smith, B.; O’Sullivan, A.; Chan, M.; Patwardhan, A.; Kelly, J.; Gillin, A.; Pang, G.; Lloyd, B.; et al. Progressive Exercise for Anabolism in Kidney Disease (PEAK): A Randomized, Controlled Trial of Resistance Training during Hemodialysis. J. Am. Soc. Nephrol. 2007, 18, 1594–1601. [Google Scholar] [CrossRef] [Green Version]
- Song, W.J.; Sohng, K.Y. Effects of progressive resistance training on body composition, physical fitness and quality of life of patients on hemodialysis. J. Korean Acad. Nurs. 2012, 42, 947–956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.L.T.; Godfrey, S.; Ng, T.T.; Moorthi, R.; Liangos, O.; Ruthazer, R.; Jaber, B.L.; Levey, A.S.; Castaneda-Sceppa, C. Effect of intra-dialytic, low-intensity strength training on functional capacity in adult haemodialysis patients: A randomized pilot trial. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 2010, 25, 1936–1943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, P.-Y.; Huang, Y.-C.; Kao, Y.-H.; Chen, J.-Y. Effects of an Exercise Program on Blood Biochemical Values and Exercise Stage of Chronic Kidney Disease Patients. J. Nurs. Res. 2010, 18, 98–107. [Google Scholar] [CrossRef]
- Miele, E.M.; Headley, S.A.E.; Germain, M.; Joubert, J.; Herrick, S.; Milch, C.; Evans, E.; Cornelius, A.; Brewer, B.; Taylor, B.; et al. High-density lipoprotein particle pattern and overall lipid responses to a short-term moderate-intensity aerobic exercise training intervention in patients with chronic kidney disease. Clin. Kidney J. 2017, 10, 524–531. [Google Scholar] [CrossRef]
- Toyama, K.; Sugiyama, S.; Oka, H.; Sumida, H.; Ogawa, H. Exercise therapy correlates with improving renal function through modifying lipid metabolism in patients with cardiovascular disease and chronic kidney disease. J. Cardiol. 2010, 56, 142–146. [Google Scholar] [CrossRef] [Green Version]
- Headley, S.; Germain, M.; Milch, C.; Pescatello, L.; Coughlin, M.A.; Nindl, B.C.; Cornelius, A.; Sullivan, S.; Gregory, S.; Wood, R. Exercise Training Improves HR Responses and V˙O2peak in Predialysis Kidney Patients. Med. Sci. Sports Exerc. 2012, 44, 2392–2399. [Google Scholar] [CrossRef]
- Goldberg, A.P.; Geltman, E.M.; Gavin, J.R., 3rd; Carney, R.M.; Hagberg, J.M.; Delmez, J.A.; Naumovich, A.; Oldfield, M.H.; Harter, H.R. Exercise training reduces coronary risk and effectively rehabilitates hemodialysis patients. Nephron 1986, 42, 311–316. [Google Scholar] [CrossRef]
- Gordon, L.; McGrowder, D.A.; Pena, Y.T.; Cabrera, E.; Lawrence-Wright, M. Effect of exercise therapy on lipid parameters in patients with end-stage renal disease on hemodialysis. J. Lab. Physicians 2012, 4, 17–23. [Google Scholar] [CrossRef]
- Reboredo Mde, M.; Henrique, D.M.; Faria Rde, S.; Chaoubah, A.; Bastos, M.G.; de Paula, R.B. Exercise training during hemodialysis reduces blood pressure and increases physical functioning and quality of life. Artif. Organs 2010, 34, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Christensen, R.H.; Wedell-Neergaard, A.-S.; Lehrskov, L.L.; Legaard, G.E.; Dorph, E.; Larsen, M.K.; Launbo, N.; Fagerlind, S.R.; Seide, S.K.; Nymand, S.; et al. Effect of Aerobic and Resistance Exercise on Cardiac Adipose Tissues: Secondary Analyses From a Randomized Clinical Trial. JAMA Cardiol. 2019, 4, 778–787. [Google Scholar] [CrossRef] [PubMed]
- Mercer, T.H.; Koufaki, P.; Naish, P.F. Nutritional status, functional capacity and exercise rehabilitation in end-stage renal disease. Clin. Nephrol. 2004, 61 (Suppl. S1), S54–S59. [Google Scholar] [PubMed]
- Molsted, S.; Eidemak, I.; Sorensen, H.T.; Kristensen, J.H. Five months of physical exercise in hemodialysis patients: Effects on aerobic capacity, physical function and self-rated health. Nephron. Clin. Pract. 2004, 96, c76–c81. [Google Scholar] [CrossRef]
- Yurtkuran, M.; Alp, A.; Yurtkuran, M.; Dilek, K. A modified yoga-based exercise program in hemodialysis patients: A randomized controlled study. Complement. Ther. Med. 2007, 15, 164–171. [Google Scholar]
- van Vilsteren, M.C.; de Greef, M.H.; Huisman, R.M. The effects of a low-to-moderate intensity pre-conditioning exercise programme linked with exercise counselling for sedentary haemodialysis patients in The Netherlands: Results of a randomized clinical trial. Nephrol. Dial. Transpl. 2005, 20, 141–146. [Google Scholar] [CrossRef] [Green Version]
- Evelo, C.T.; Palmen, N.G.; Artur, Y.; Janssen, G.M. Changes in blood glutathione concentrations, and in erythrocyte glutathione reductase and glutathione S-transferase activity after running training and after participation in contests. Eur. J. Appl. Physiol. Occup. Physiol. 1992, 64, 354–358. [Google Scholar]
- Kopple, J.D.; Wang, H.; Casaburi, R.; Fournier, M.; Lewis, M.I.; Taylor, W.; Storer, T.W. Exercise in maintenance hemodialysis patients induces transcriptional changes in genes favoring anabolic muscle. J. Am. Soc. Nephrol. 2007, 18, 2975–2986. [Google Scholar] [CrossRef] [Green Version]
- Toussaint, N.D.; Polkinghorne, K.R.; Kerr, P.G. Impact of intradialytic exercise on arterial compliance and B-type natriuretic peptide levels in hemodialysis patients. Hemodial. Int. 2008, 12, 254–263. [Google Scholar]
- Wilund, K.R.; Tomayko, E.J.; Wu, P.T.; Ryong Chung, H.; Vallurupalli, S.; Lakshminarayanan, B.; Fernhall, B. Intradialytic exercise training reduces oxidative stress and epicardial fat: A pilot study. Nephrol. Dial. Transplant. 2010, 25, 2695–2701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gołębiowski, T.; Kusztal, M.; Weyde, W.; Dziubek, W.; Woźniewski, M.; Madziarska, K.; Krajewska, M.; Letachowicz, K.; Strempska, B.; Klinger, M. A program of physical rehabilitation during hemodialysis sessions improves the fitness of dialysis patients. Kidney Blood Press. Res. 2012, 35, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Daniilidis, M.; Kouidi, E.; Giagoudaki, F.; Fleva, A.; Nikolaides, P.; Vasilaki, A.; Deligiannis, A.; Tourkantonis, A. The immune response in hemodialysis patients following physical training. Sport Sci. Health 2004, 1, 11–16. [Google Scholar] [CrossRef]
- Załuska, A.; Załuska, W.T.; Bednarek-Skublewska, A.; Ksiazek, A. Nutrition and hydration status improve with exercise training using stationary cycling during hemodialysis (HD) in patients with end-stage renal disease (ESRD). Ann. Univ. Mariae Curie Sklodowska Med. 2002, 57, 342–346. [Google Scholar] [PubMed]
- Cheema, B.S.; Abas, H.; Smith, B.C.; O’Sullivan, A.J.; Chan, M.; Patwardhan, A.; Kelly, J.; Gillin, A.; Pang, G.; Lloyd, B.; et al. Effect of resistance training during hemodialysis on circulating cytokines: A randomized controlled trial. Eur. J. Appl. Physiol. 2011, 111, 1437–1445. [Google Scholar] [CrossRef] [PubMed]
- Viana, J.L.; Kosmadakis, G.C.; Watson, E.L.; Bevington, A.; Feehally, J.; Bishop, N.C.; Smith, A.C. Evidence for Anti-Inflammatory Effects of Exercise in CKD. J. Am. Soc. Nephrol. 2014, 25, 2121–2130. [Google Scholar] [CrossRef] [Green Version]
- Leehey, D.J.; Moinuddin, I.; Bast, J.P.; Qureshi, S.; Jelinek, C.S.; Cooper, C.; Edwards, L.C.; Smith, B.M.; Collins, E.G. Aerobic exercise in obese diabetic patients with chronic kidney disease: A randomized and controlled pilot study. Cardiovasc. Diabetol. 2009, 8, 62. [Google Scholar] [CrossRef] [Green Version]
- Aoike, D.T.; Baria, F.; Kamimura, M.A.; Ammirati, A.; de Mello, M.T.; Cuppari, L. Impact of home-based aerobic exercise on the physical capacity of overweight patients with chronic kidney disease. Int. Urol. Nephrol. 2015, 47, 359–367. [Google Scholar] [CrossRef]
- Colonetti, T.; Grande, A.J.; Amaral, M.C.; Colonetti, L.; Uggioni, M.L.; da Rosa, M.I.; Hernandez, A.V.; Tse, G.; Liu, T.; Nerlekar, N.; et al. Effect of exercise on epicardial adipose tissue in adults: A systematic review and meta-analyses. Heart Fail. Rev. 2021, 26, 1399–1411. [Google Scholar] [CrossRef]
- Jeong, J.H.; Biruete, A.; Tomayko, E.J.; Wu, P.T.; Fitschen, P.; Chung, H.R.; Ali, M.; McAuley, E.; Fernhall, B.; Phillips, S.A.; et al. Results from the randomized controlled IHOPE trial suggest no effects of oral protein supplementation and exercise training on physical function in hemodialysis patients. Kidney Int. 2019, 96, 777–786. [Google Scholar] [CrossRef]
- Chan, K.N.; Chen, Y.; Lit, Y.; Massaband, P.; Kiratli, J.; Rabkin, R.; Myers, J.N. A randomized controlled trial of exercise to prevent muscle mass and functional loss in elderly hemodialysis patients: Rationale, study design, and baseline sample. Contemp. Clin. Trials Commun. 2019, 15, 100365. [Google Scholar] [CrossRef] [PubMed]
- Kannan, U.; Vasudevan, K.; Balasubramaniam, K.; Yerrabelli, D.; Shanmugavel, K.; John, N.A. Effect of exercise intensity on lipid profile in sedentary obese adults. J. Clin. Diagn. Res. 2014, 8, BC08–BC10. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-M.; Chung, Y.-C.; Chang, J.-S.; Yeh, M.-L. Effects of Aerobic Exercise During Hemodialysis on Physical Functional Performance and Depression. Biol. Res. Nurs. 2015, 17, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Heiwe, S.; Jacobson, S.H. Exercise training for adults with chronic kidney disease. Cochrane Database Syst. Rev. 2011, Cd003236. [Google Scholar] [CrossRef] [PubMed]
- Beavers, K.M.; Brinkley, T.E.; Nicklas, B.J. Effect of exercise training on chronic inflammation. Clin. Chim. Acta Int. J. Clin. Chem. 2010, 411, 785–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiraishi, F.G.; Stringuetta Belik, F.; Oliveira, E.S.V.R.; Martin, L.C.; Hueb, J.C.; Gonçalves Rde, S.; Caramori, J.C.; Barreti, P.; Franco, R.J. Inflammation, diabetes, and chronic kidney disease: Role of aerobic capacity. Exp. Diabetes Res. 2012, 2012, 750286. [Google Scholar] [CrossRef] [Green Version]
- Mafra, D.; Deleaval, P.; Teta, D.; Cleaud, C.; Arkouche, W.; Jolivot, A.; Fouque, D. Influence of inflammation on total energy expenditure in hemodialysis patients. J. Ren. Nutr. 2011, 21, 387–393. [Google Scholar] [CrossRef]
- Anand, S.; Chertow, G.M.; Johansen, K.L.; Grimes, B.; Kurella Tamura, M.; Dalrymple, L.S.; Kaysen, G.A. Association of self-reported physical activity with laboratory markers of nutrition and inflammation: The Comprehensive Dialysis Study. J. Ren. Nutr. 2011, 21, 429–437. [Google Scholar] [CrossRef] [Green Version]
- Gomez-Cabrera, M.C.; Domenech, E.; Viña, J. Moderate exercise is an antioxidant: Upregulation of antioxidant genes by training. Free Radic. Biol. Med. 2008, 44, 126–131. [Google Scholar] [CrossRef]
- Wang, F.; Wang, X.; Liu, Y.; Zhang, Z. Effects of Exercise-Induced ROS on the Pathophysiological Functions of Skeletal Muscle. Oxid. Med. Cell. Longev. 2021, 2021, 3846122. [Google Scholar] [CrossRef]
- Bernier-Jean, A.; Beruni, N.A.; Bondonno, N.P.; Williams, G.; Teixeira-Pinto, A.; Craig, J.C.; Wong, G. Exercise training for adults undergoing maintenance dialysis. Cochrane Database Syst. Rev. 2022, 1, Cd014653. [Google Scholar] [PubMed]
- KDIGO. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Int. Soc. Nephrol. 2013, 3, 1–150. [Google Scholar]
| Aerobic Exercise | Resistance Exercise | |||
|---|---|---|---|---|
| Non-Dialysis-Dependent CKD | Dialysis-Dependent CKD | Non-Dialysis-Dependent CKD | Dialysis-Dependent CKD | |
| Body Weight | No change in body weight/composition [30,102,103,104,105] Decrease in BMI [106,107] and waist circumference [107,108] | No change in weight [109] | No change in weight [102,110] Decrease in weight and waist circumference [107] Improved muscle attenuation [102,110] | No change in weight [109,111] or LBM [112,113] Increase in weight [114,115] and LBM [116] Improved muscle attenuation [114] |
| Lipid Profile | Decrease in TGs and LDL-C [117,118,119] Increase in TGs and LDL-C [120] No change [103] | Decrease in TG [121,122] and LDL-C [122] Increase in HDL-C Increased TG and LDL-C [123] No change [123,124,125] | N/A | No change [109,126] Decrease in TGs [115,122], LDL-C [122], and TCs [115,127] Increase in HDL-C [122] |
| Markers of Inflammation | No change in CRP [102,104,105,128,129] or IL-6 [120] Decrease in IL-6 [18] | No change in CRP [130,131,132,133] or IL-6 [134] Decrease in CRP [109,135] | Decrease in CRP and IL-6 [110] | No change in CRP [130] or IL-6 [130,136] Decrease in CRP [117,123,137] |
| Markers of Oxidative Stress | Decrease in products of lipid peroxidation [103] and F2-isoprostane [18] | Decrease in TBARS [132] | N/A | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ertuglu, L.A.; Ikizler, T.A. Effects of Diet and Exercise on Metabolic Parameters and Health in Moderate to Advanced Kidney Disease. Kidney Dial. 2022, 2, 330-345. https://doi.org/10.3390/kidneydial2020030
Ertuglu LA, Ikizler TA. Effects of Diet and Exercise on Metabolic Parameters and Health in Moderate to Advanced Kidney Disease. Kidney and Dialysis. 2022; 2(2):330-345. https://doi.org/10.3390/kidneydial2020030
Chicago/Turabian StyleErtuglu, Lale A., and Talat Alp Ikizler. 2022. "Effects of Diet and Exercise on Metabolic Parameters and Health in Moderate to Advanced Kidney Disease" Kidney and Dialysis 2, no. 2: 330-345. https://doi.org/10.3390/kidneydial2020030
APA StyleErtuglu, L. A., & Ikizler, T. A. (2022). Effects of Diet and Exercise on Metabolic Parameters and Health in Moderate to Advanced Kidney Disease. Kidney and Dialysis, 2(2), 330-345. https://doi.org/10.3390/kidneydial2020030






