1. Introduction
‘What can I do to manage my kidney disease to enable me to live well?’ Every person affected by chronic kidney disease (CKD) and their family members/care givers wants the answer to this.
What does ‘living well’ mean to patients? This question was explored in an article published concurrently in many journals worldwide to raise awareness for World Kidney Day (WKD) in 2021. Kalantar-Zadeh et al. [
1] described ‘life participation’ as one key to living well. Life participation, defined by the Standardised Outcomes in Nephrology Group (SONG) [
2] is ‘the ability to do meaningful activities of life including, but not limited to, work, study, family responsibilities, travel, sport, social, and recreational activities’, and should be considered a critically important patient-reported outcome (PRO) across all treatment stages of CKD. Other critically important PROs identified by SONG include fatigue, mortality, pain, and depression. Moreover, SONG has reported in other publications [
3,
4] that patients (and caregivers) consistently gave a higher priority to these PROs than healthcare professionals.
Pharmaceutical, clinical, and surgical interventions such as dialysis and transplantation can, of course, deliver beneficial outcomes for patients. For example, fatigue caused by anaemia can be treated by iron or erythropoiesis-stimulating agents (ESA) therapies, pain by a variety of approved pharmaceutical and non-pharmaceutical treatments, depression by drugs or (cognitive behavioural therapy) CBT, and end-stage kidney disease (ESKD) by kidney replacement therapy (KRT). In addition to those listed above, a range of other ‘unpleasant symptoms’ has been reported by Kalantar-Zadeh et al. [
5]. These include ‘gastrointestinal, neurological, cardiopulmonary, sexual dysfunction, and sleep disorders’. However, patients across all CKD stages continue to report multiple symptoms that often remain challenging to treat. Many PROs are not routinely monitored or measured, owing to a lack of tools or incentives to collect the data.
Self-reported symptoms such as these are not unique to CKD. Yet CKD patients tell patient charities and foundations that the focus of their renal appointments is ‘bloods, urine, blood pressure and kidney function’ and the treatment of those complications. Little time is provided to discuss other symptoms and concerns of those with CKD and, where feasible, recommend other treatments that might help, such as lifestyle interventions.
2. Guidelines for Lifestyle Interventions in CKD Are Lacking
The lack of approved guidelines for lifestyle interventions in CKD is historic and due to a lack of evidence. The last international guideline for the ‘Evaluation and Management of Chronic Kidney Disease’ published by KDIGO in 2012 [
6] contains 14 references to ‘lifestyle’; only 1 is graded and is considered ‘low quality evidence’. Diet is mentioned more frequently and getting ‘expert dietary advice and information’ is ‘moderately’ graded but no specific dietary intervention gets any grade. There are four references to ‘psychological care’, but none are graded.
By comparison, the international ‘Clinical Practice Recommendations for Managing Type 2 Diabetes in Primary Care’ [
7] give high priority to lifestyle changes, especially diet and exercise. NICE has published comprehensive guidance [
8] for Multiple Sclerosis in Adults: Management with detailed sections on fatigue, mobility, pain, and cognition (symptoms frequently mentioned by CKD patients).
It is not surprising that patients look beyond the clinic for lifestyle interventions and complementary or alternative ways to treat their symptoms that they think will improve their quality of life. The proposed update to the KDIGO CKD 2012 guidelines will address more of these unmet patient needs. However, it is unlikely that any recommendations will be graded highly given the paucity of high-quality clinical trials in these interventions.
3. Dietary Guidance Is a Top Priority with CKD Patients
Dietary advice for managing CKD is one of the most highly searched terms on the internet. An enjoyable and nutritious diet is fundamental to living well as a human being. In the many online patient forums, diet is mentioned daily yet patient information is not consistently offered or easily accessed, and is frequently confusing, outdated, or low quality. Some information still does not account for cultural food differences or consider the social environment in which food is grown, bought, cooked, and consumed. Low health literacy is also a barrier to understanding how best to eat well for kidney health.
Early-stage CKD patients, even in high-income countries, are unfortunately rarely referred to dietitians. When patients turn to their renal multidisciplinary team (MDT) or the internet for help, they think their ‘chronic’ kidney disease is at a later stage than it may be and get confused by end-stage kidney disease diets. It is also noticeable that, despite growing evidence of the potential benefits of plant-based diets in early CKD, dietary information does not reflect this.
Patients at CKD5 or on dialysis will receive advice from dietitians but this advice tends to be about restricting or forbidding something, for example, foods with high potassium and phosphate, accompanied by stern instructions to comply. Lack of nutritional labelling on foods adds to the confusion and challenges of a major change to their habitual eating patterns. Patients can feel overwhelmed and anxious from this dietary burden (on them and their families) which has a negative impact on their quality of life. The requirement to reduce dietary phosphate is especially burdensome and is worsened by having to swallow significant numbers of phosphate binders with every meal or snack eaten. Studies have invariably shown substantial nonadherence with phosphate binders. Perversely, while clinical practice guidelines suggest that reducing high phosphate levels in the blood is essential, the effect of lowering blood phosphate levels on important patient-centred outcomes has never been tested. Meanwhile, a large percentage of the cost of dialysis treatment is the price of phosphate binders.
4. Exercise and Other Lifestyle Guidance
Another lifestyle intervention sought by CKD patients is exercise advice. Again, there is minimal quality evidence that shows a clinical benefit in CKD from a particular exercise. In 2018, the WHO published [
9] a ‘Global action plan on physical activity 2018–2030′. On its website [
10] is a list of the key facts about physical exercise. Surely, there is sufficient evidence from the WHO (and other reputable sources) to recommend a range of physical activities suitable for early-stage CKD patients at least. As the WHO says: ‘Physical activity has significant health benefits for hearts, bodies and minds’. Exercise, therefore, seems to be another fundamental aspect of living well. Of course, patients on dialysis or transplanted, or suffering from fatigue and bone disorders from CKD, will need tailored exercise advice. However, there must be transferrable and trustworthy evidence from other conditions that can be applied, such as in treating hernias (often caused by peritoneal dialysis (PD) or transplant) or osteoporosis (to help with mineral bone disease, especially in older women), or from surgical prehab/rehab programmes (for post fistula, catheter, or transplant surgery). Why is this information not provided to CKD patients?
Similarly, there must be appropriate lifestyle interventions from other conditions such as the treatment of mental health issues in cancer or intractable pain in visceral disorders (such as bowel disease) that can be adapted to CKD patients.
5. Drug Development Regulation Will Focus Attention on PROs
Hope for increased focus on lifestyle interventions may be found in the regulatory environment. The US Food and Drug Administration (FDA) is promoting publicly available standardised core sets of Clinical Outcome Assessments (COAs) to be used in drug development [
11]. A COA is a ‘measure that describes or reflects how a patient feels, functions, or survives’. All interventions must show a clinically meaningful benefit to how long a patient lives and how a patient feels or functions in daily life. Types of COAs include PROMs, Observer-reported outcome (ObsRO) measures, Clinician-reported outcome (ClinRO) measures, and Performance outcome (PerfO) measures.
The PRO can be measured from reports directly from the patient about their health status and should therefore cover the range of ‘unpleasant’ symptoms described above. The major challenge with PROs in CKD is the lack of Patient Reported Outcome Measures (PROMs) and well-defined and reliable tools to measure symptoms as diverse as pain, fatigue, and life participation. As these tools become necessary for a COA to satisfy regulators, this should encourage the kidney community to address this challenge.
Fortunately, SONG [
12] in collaboration with the international kidney community is currently undertaking a wide range of initiatives to develop tools across all its core outcomes sets, encompassing core clinical outcomes and PROs. The results of this collective endeavour should stimulate increased interest in and funding of research into delivering the positive outcomes that patients need.
6. More Innovative Research Is Needed
The gold standard RCT evidence to support lifestyle intervention guidelines may be unattainable, but different types of clinical trials, such as pragmatic, could be acceptable alternatives. Biomarkers or surrogate biomarkers may also be feasible. Traditionally in CKD research, the primary outcomes are biomarkers of kidney dysfunction such as serum creatinine, urine output, and urine albumin. However, these may not be appropriate when looking at lifestyle interventions in all kidney disorders, especially in the early stages. For example, kidney function is conserved in earlier stages of autosomal dominant polycystic kidney disease (ADPKD) whilst patients may already be experiencing many of the unpleasant symptoms of CKD and may also be undiagnosed.
New biomarkers such as neutrophil gelatinase-associated lipocalin (NGAL), cystatin C, and fibroblast growth factor-23 (FGF-23) are showing promise [
13]. In ADPKD, total kidney volume (TKV) is accepted by both the FDA [
14] and the European Medicines Agency (EMA) [
15] as a prognostic biomarker for use in clinical trial enrolment; efforts continue to qualify TKV as a more sensitive predictor of disease progression in early stages of ADPKD. Effects of exercise and lifestyle interventions on oxidative stress have been studied [
16], but the study was small and of short duration. In patients with mineral bone disorder (CKD-MBD) and osteoporosis, biomarkers such as bone-specific alkaline phosphatase (bALP) and serum intact PTH (iPTH) could be considered to assess bone turnover [
17].
7. Implementation of Guidelines into Care Pathways
Research, clinical trials, and guidelines are the first steps to ensuring that there is quality evidence to support individualised lifestyle interventions for CKD patients. The next crucial step is to implement all guidelines equitably to patients through holistic integrated multidisciplinary care pathways. Further major challenges are anticipated at this stage. Commissioning and reimbursement vary across and within countries and are often impossible for lifestyle interventions that have no supporting evidence showing the ‘hard’ clinical outcomes that commissioners and payers demand. Additionally, in the pathway development and implementation, it will be vital to include information about advice and support ‘beyond the clinic’ such as links to local/national patient and peer support groups, local community or healthcare services offering exercise/diet help, social prescribing, wellbeing, and counselling—which is often lacking in many CKD pathways. Patient and patient group involvement should be integral to pathways.
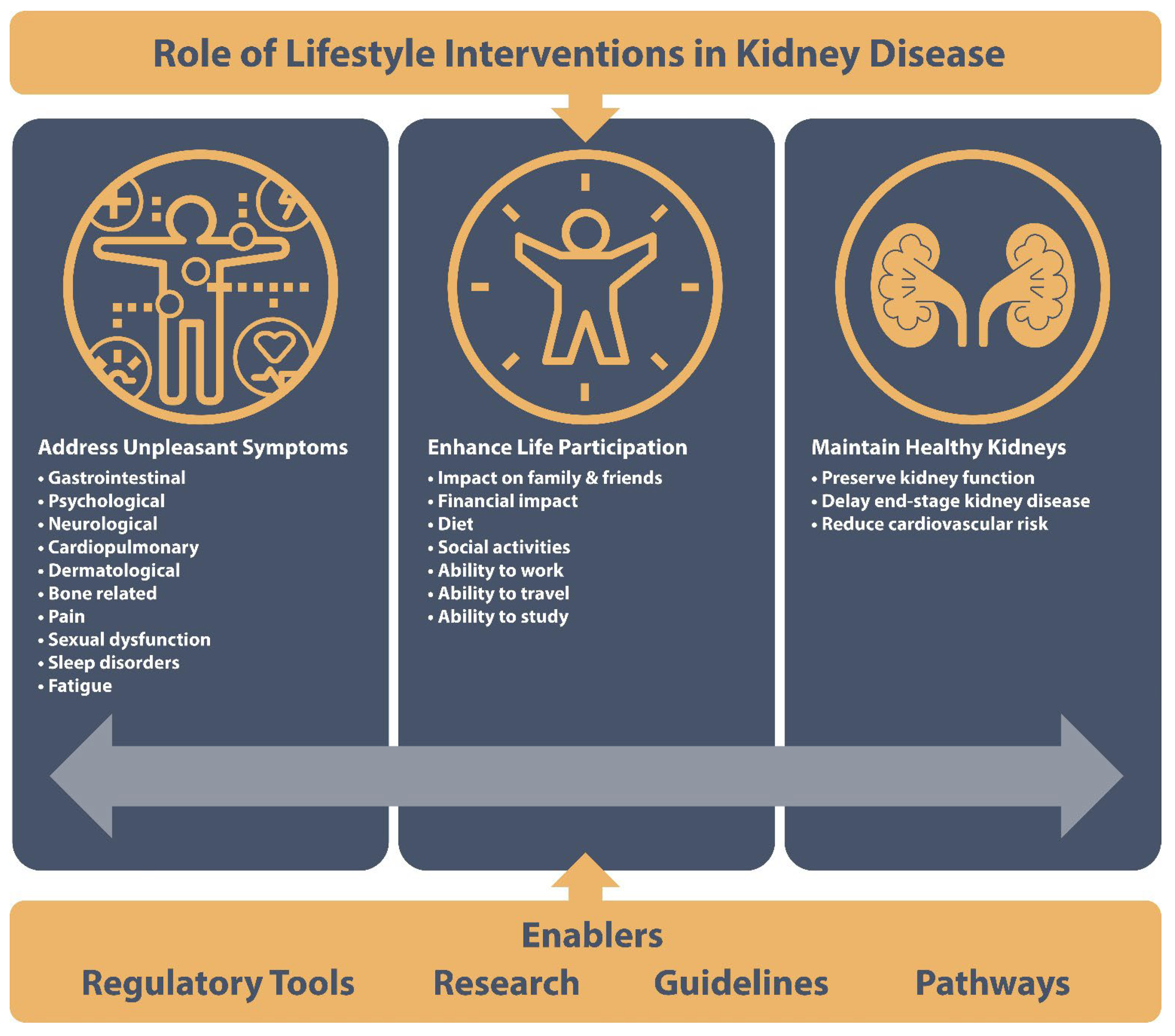
Figure 1 summarises the issues and enablers of lifestyle interventions described above.
8. Conclusions
‘Living Well with Kidney Disease’ was the 2021 global WKD theme, but it ought to be a daily mission for everyone involved in the care of chronic kidney disease (CKD) patients. For WKD 2022, many organisations called for collective action from governments to add CKD to their health agendas and create and implement a systemic approach to improving the health of all kidney patients worldwide. In addition to requests for more research and reduced inequity of access to life-saving therapies such as KRT, it is time to issue a specific international call to action or joint position statement to focus on lifestyle interventions to help minimise the lifelong consequences and health burden of living with CKD.