Hemodialysis Therapy Adherence and Contributing Factors among End-Stage Renal Disease Patients at Muhimbili National Hospital, Dar es Salaam, Tanzania
Abstract
1. Introduction
2. Materials and Methods
2.1. Recruitment and Training of Research Assistants
2.2. Ethical Issues
3. Results
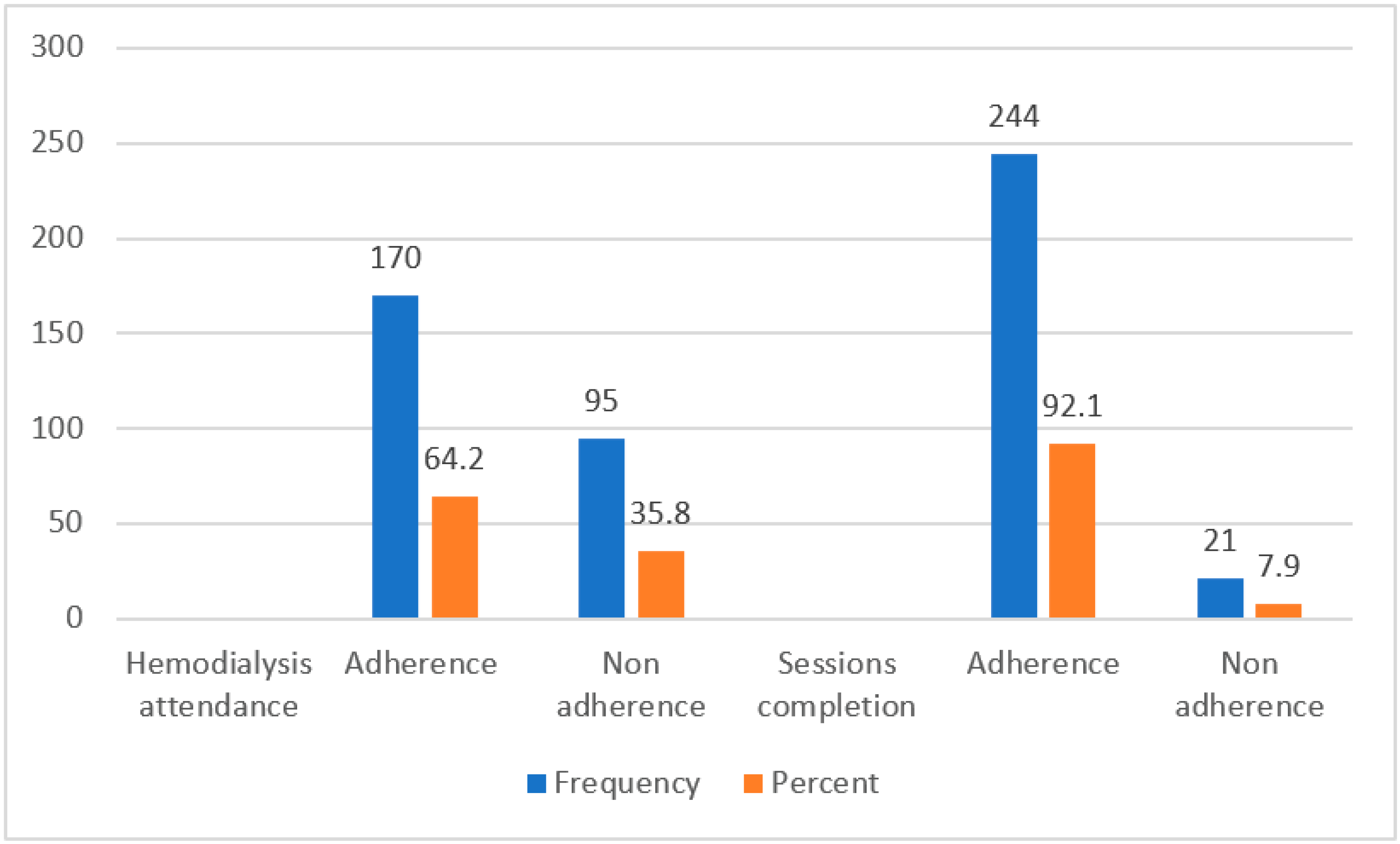
3.1. Adherence to Hemodialysis Therapy among ESRD Patients
3.2. Factors Contributing to Adherence to Hemodialysis among ESRD Patients
4. Discussion
5. Study Limitations and Strengths
6. Conclusions and Recommendation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Somji, S.S.; Ruggajo, P.; Moledina, S. Adequacy of Hemodialysis and Its Associated Factors among Patients Undergoing Chronic Hemodialysis in Dar es Salaam, Tanzania. Int. J. Nephrol. 2020, 2020, 9863065. [Google Scholar] [CrossRef] [PubMed]
- Beerappa, H.; Chandrababu, R. Adherence to dietary and fluid restrictions among patients undergoing hemodialysis: An observational study. Clin. Epidemiol. Glob. Health 2019, 7, 127–130. [Google Scholar] [CrossRef]
- Stanifer, J.W.; Muiru, A.; Jafar, T.H.; Patel, U.D. Chronic kidney disease in low- and middle-income countries. Nephrol. Dial. Transplant. 2016, 31, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Mushi, L.; Krohn, M.; Flessa, S. Cost of dialysis in Tanzania: Evidence from the providers perspective. Health Econ. Rev. 2015, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Stanifer, J.W.; Lunyera, J.; Boyd, D.; Karia, F.; Maro, V.; Omolo, J.; Patel, U.D. Traditional medicine practices among community members with chronic kidney disease in northern Tanzania: An ethnomedical survey. BMC Nephrol. 2015, 16, 170. [Google Scholar] [CrossRef]
- Meremo, A.J.; Masalu, M.; Sabi, I. Prevalence and Risk Factors Associated With Chronic Kidney Disease Among Patients Presenting at a Hemodialysis Unit in Dodoma, Tanzania. East Afr. Health Res. J. 2018, 2, 53–57. [Google Scholar] [CrossRef]
- Furia, F.F.; Shoo, J.; Ruggajo, P.J.; Kilonzo, K.; Basu, G.; Yeates, K.; Varughese, S.; Svarstad, E.; Kisanga, O. Developing nephrology services in low income countries: A case of Tanzania. BMC Nephrol. 2019, 20, 378. [Google Scholar] [CrossRef]
- Halle, M.P.; Nelson, M.; Kaze, F.F.; Pierre, N.M.J.; Denis, T.; Fouda, H.; Ashuntantang, E.G. Non-adherence to hemodialysis regimens among patients on maintenance hemodialysis in sub-Saharan Africa: An example from Cameroon. Ren. Fail. 2020, 42, 1022–1028. [Google Scholar] [CrossRef]
- Ozen, N.; Cinar, F.I.; Askin, D.; Mut, D.; Turker, T. Nonadherence in Hemodialysis Patients and Related Factors: A Multicenter Study. J. Nurs. Res. 2019, 27, e36. [Google Scholar] [CrossRef]
- The United Republic of Tanzania, Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC). National Guideline for Dialysis Services, 1st ed. 2017. Available online: https://www.globalhep.org/sites/default/files/content/resource/files/2020-02/Tanzania%20National%20Strategic%20Plan%20for%20the%20Control%20of%20Viral%20Hepatitis%202018-19-2022-23.pdf (accessed on 6 December 2021).
- Stankuvienė, A.; Žiginskienė, E.; Kuzminskis, V.; Bumblytė, I.A. Impact of hemodialysis dose and frequency on survival of patients on chronic hemodialysis in Lithuania during 1998–2005. Medicina 2010, 46, 516–521. [Google Scholar] [CrossRef]
- Naalweh, K.S.; Barakat, M.A.; Sweileh, M.W.; Al-Jabi, S.W.; Sweileh, W.M.; Zyoud, S.H. Treatment adherence and perception in patients on maintenance hemodialysis: A cross—sectional study from Palestine. BMC Nephrol. 2017, 18, 178. [Google Scholar] [CrossRef] [PubMed]
- Tayebi, A.; Einollahi, B.; Rahimi, A.; Sirati-nir, M. Kidney Diseases. The Non-adherence with Treatment in Dialysis Patients in Iran, A Systematic Review. Iran. J. Kidney Dis. 2019, 13, 347–361. [Google Scholar] [PubMed]
- Chenitz, K.B.; Fernando, M.; Shea, J.A. In-center hemodialysis attendance: Patient perceptions of risks, barriers, and recommendations. Hemodial. Int. 2014, 18, 364–373. [Google Scholar] [CrossRef] [PubMed]
- Saran, R.; Bragg-Gresham, J.L.; Rayner, H.C.; Goodkin, D.A.; Keen, M.L.; Van Dijk, P.C.; Kurokawa, K.; Piera, L.; Saito, A.; Fukuhara, S.; et al. Nonadherence in hemodialysis: Associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int. 2003, 64, 254–262. [Google Scholar] [CrossRef]
- Ibrahim, S.; Hossam, M.; Belal, D. Study of non-compliance among chronic hemodialysis patients and its impact on patients’ outcomes. Saudi J. Kidney Dis. Transplant. 2015, 26, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Qian, L.; Shi, J.; Franklin, M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med. Res. Methodol. 2018, 18, 63. [Google Scholar] [CrossRef]
- Mukakarangwa, M.C.; Chironda, G.; Bhengu, B.; Katende, G. Adherence to Hemodialysis and Associated Factors among End Stage Renal Disease Patients at Selected Nephrology Units in Rwanda: A Descriptive Cross-Sectional Study. Nurs. Res. Pract. 2018, 2018, 4372716. [Google Scholar] [CrossRef]
- Al-khattabi, G.H. Prevalence of Treatment Adherence among Attendance at Hemodialysis in Makkah. Int. J. Med. Sci. Public Health 2019, 3, 592–598. [Google Scholar]
- Duong, C.M.; Olszyna, D.P.; Nguyen, P.D.; McLaws, M.-L. Challenges of hemodialysis in Vietnam: Experience from the first standardized district dialysis unit in Ho Chi Minh City. BMC Nephrol. 2015, 16, 122. [Google Scholar] [CrossRef][Green Version]
- Leggat, J.E.; Orzol, S.M.; Hulbert-Shearon, T.E.; Golper, T.A.; Jones, C.A.; Held, P.J.; Port, F.K. Noncompliance in hemodialysis: Predictors and survival analysis. Am. J. Kidney Dis. 1998, 32, 139–145. [Google Scholar] [CrossRef]
- Dantas, L.; Cruz, C.; Rocha, M.; Moura, J.; Paschoalin, E.; De Souza, C.M. Prevalence and Predictors of Nonadherence to Hemodialysis. Nephron Exp. Nephrol. 2013, 124, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, A.M.A.; Al-Khattabi, G.H. Factors Influencing Adherence to Hemodialysis Sessions among Patients with End-Stage Renal Disease in Makkah City. Saudi J. Kidney Dis. Transplant. 2021, 32, 763. [Google Scholar] [CrossRef] [PubMed]
| Adherence Status | |||
|---|---|---|---|
| Variable | Non-Adherence | Adherence | p Value |
| Age group (in years) | |||
| 19–30 | 13 (43.3) | 17 (56.7) | |
| 31–40 | 13 (32.5) | 27 (67.5) | |
| 41–50 | 30 (52.6) | 27 (47.4) | 0.021 |
| 51–60 | 20 (30.3) | 46 (69.7) | |
| 61–99 | 19 (26.4) | 53 (73.6) | |
| Sex | |||
| Male | 70 (36.6) | 121 (63.4) | |
| Female | 25 (33.8) | 49 (66.2) | 0.663 |
| Marital status | |||
| Single | 14 (35.9) | 25 (64.1) | |
| Married/cohabiting | 68 (34.3) | 130 (65.7) | 0.459 |
| Widow/separated | 13 (46.4) | 15 (53.6) | |
| Faith | |||
| Christian | 52 (31.7) | 112 (68.3) | |
| Muslim | 43 (43.9) | 55 (56.1) | |
| Other | 0 (0) | 3 (100) | 0.059 |
| Education level | |||
| No formal school | 2 (33.3) | 4 (66.7) | |
| Primary school | 35 (42.2) | 48 (57.8) | |
| Secondary school | 31 (33.7) | 61 (66.3) | 0.543 |
| Higher education level | 27 (32.1) | 57 (67.9) | |
| Occupation | |||
| Public servant | 17 (30.4) | 39 (69.6) | |
| Self employed | 50 (45.0) | 61 (55.0) | 0.029 |
| Unemployed | 28 (28.6) | 70 (71.4) | |
| Monthly income level (TZS) | |||
| Less than 135,000 | 42 (35.6) | 76 (64.4) | |
| 135,000–270,000 | 10 (26.3) | 28 (73.7) | |
| 270,000–540,000 | 21 (36.8) | 36 (63.2) | 0.480 |
| More than 540,0000 | 22 (42.3) | 30 (57.7) | |
| Source of funding for dialysis | |||
| Self | 41 (45.1) | 50 (54.9) | |
| Insurance | 54 (31.0) | 120 (69.0) | 0.02 |
| Variable | cRR (95%) | p Value | aRR (95% CI) | p Value | p Trend |
|---|---|---|---|---|---|
| Age group (in years) | |||||
| 18–30 | 1 | 1 | |||
| 31–40 | 1.19 (0.81,1.74) | 0.367 | 1.49 (0.65, 3.36) | 0.338 | |
| 41–50 | 0.84 (0.55,1.27) | 0.399 | 1.09 (0.47, 2.55) | 0.834 | 0.049 |
| 51–60 | 1.23 (0.87,1.75) | 0.249 | 1.48 (0.67, 3.30) | 0.335 | |
| 61–99 | 1.3 (0.92,1.83) | 0.135 | 1.49 (0.66, 3.38) | 0.337 | |
| Sex | |||||
| Male | 1 | 1 | |||
| Female | 1.05 (0.86,1.27) | 0.658 | 1.09 (0.74, 1.59) | 0.665 | |
| Marital status | |||||
| Married/cohabiting | 1 | 1 | |||
| Single | 1.02 (0.79,1.32) | 0.855 | 1.22 (0.73, 2.05) | 0.636 | |
| Widow/separated | 0.83 (0.55,0.81) | 0.400 | 1.97 (1.03, 3.77) | 0.040 | |
| Faith | |||||
| Christian | 1 | 1 | |||
| Muslim | 0.82 (0.67,0.01) | 0.06 | 1.41 (0.97, 2.04) | 0.067 | |
| Education level | |||||
| No formal school | 1 | 1 | |||
| Primary school | 0.87 (0.48,1.57) | 0.639 | 0.73 (0.25, 2.15) | 0.573 | |
| Secondary school | 0.99 (0.55,1.78) | 0.985 | 0.90 (0.31, 2.65) | 0.846 | 0.224 |
| Higher education | 1.02 (0.57,1.83) | 0.953 | 0.88 (0.29, 2.72) | 0.829 | |
| Occupation | |||||
| Public servant | 1 | 1 | |||
| Self employed | 0.79 (0.62,1.00) | 0.055 | 1.59 (1.44, 1.94) | 0.048 | |
| Unemployed | 1.03 (0.59,0.83) | 0.817 | 1.09 (0.55, 2.14) | 0.896 | |
| Monthly income (TZS) | |||||
| Less than 135,000 | 1 | 1 | |||
| 135,000–270,000 | 1.14 (0.91,1.44) | 0.257 | 0.64 (0.35, 1.15) | 0.133 | 0.416 |
| 270,000–540,000 | 0.90 (0.68,1.17) | 0.422 | 1.65 (1.02, 2.69) | 0.884 | |
| More than 540,0000 | 0.98 (0.77,1.25) | 0.873 | 0.92 (0.62, 1.51) | 0.041 | |
| Source of funding | |||||
| Non-insured | 1 | 1 | |||
| Insurance | 0.69 (0.50,0.95) | 0.021 | 0.70 (0.48, 0.96) | 0.044 | |
| Duration on dialysis | |||||
| 1 month to 1 year | 1 | 1 | |||
| More than 1–2 years | 1.03 (0.34,3.07) | 0.96 | 1.13 (0.73, 1.74) | 0.594 | |
| More than 2–3 years | 0.59 (0.14, 2.56) | 0.48 | 0.83 (0.51, 1.35) | 0.447 | |
| More than 3 to 5 years | 1.14 (0.34, 3.86) | 0.83 | 0.48 (0.24, 0.97) | 0.042 | |
| More than 5 years | 0.66 (0.09, 4.81) | 0.68 | 0.38 (0.13, 1.14) | 0.087 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohamedi, S.; Mosha, I.H. Hemodialysis Therapy Adherence and Contributing Factors among End-Stage Renal Disease Patients at Muhimbili National Hospital, Dar es Salaam, Tanzania. Kidney Dial. 2022, 2, 123-130. https://doi.org/10.3390/kidneydial2010014
Mohamedi S, Mosha IH. Hemodialysis Therapy Adherence and Contributing Factors among End-Stage Renal Disease Patients at Muhimbili National Hospital, Dar es Salaam, Tanzania. Kidney and Dialysis. 2022; 2(1):123-130. https://doi.org/10.3390/kidneydial2010014
Chicago/Turabian StyleMohamedi, Salumu, and Idda Hubert Mosha. 2022. "Hemodialysis Therapy Adherence and Contributing Factors among End-Stage Renal Disease Patients at Muhimbili National Hospital, Dar es Salaam, Tanzania" Kidney and Dialysis 2, no. 1: 123-130. https://doi.org/10.3390/kidneydial2010014
APA StyleMohamedi, S., & Mosha, I. H. (2022). Hemodialysis Therapy Adherence and Contributing Factors among End-Stage Renal Disease Patients at Muhimbili National Hospital, Dar es Salaam, Tanzania. Kidney and Dialysis, 2(1), 123-130. https://doi.org/10.3390/kidneydial2010014






