Risk of SARS-CoV-2 Infection Among Hospital-Based Healthcare Workers in Thailand at Myanmar Border, 2022
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Site
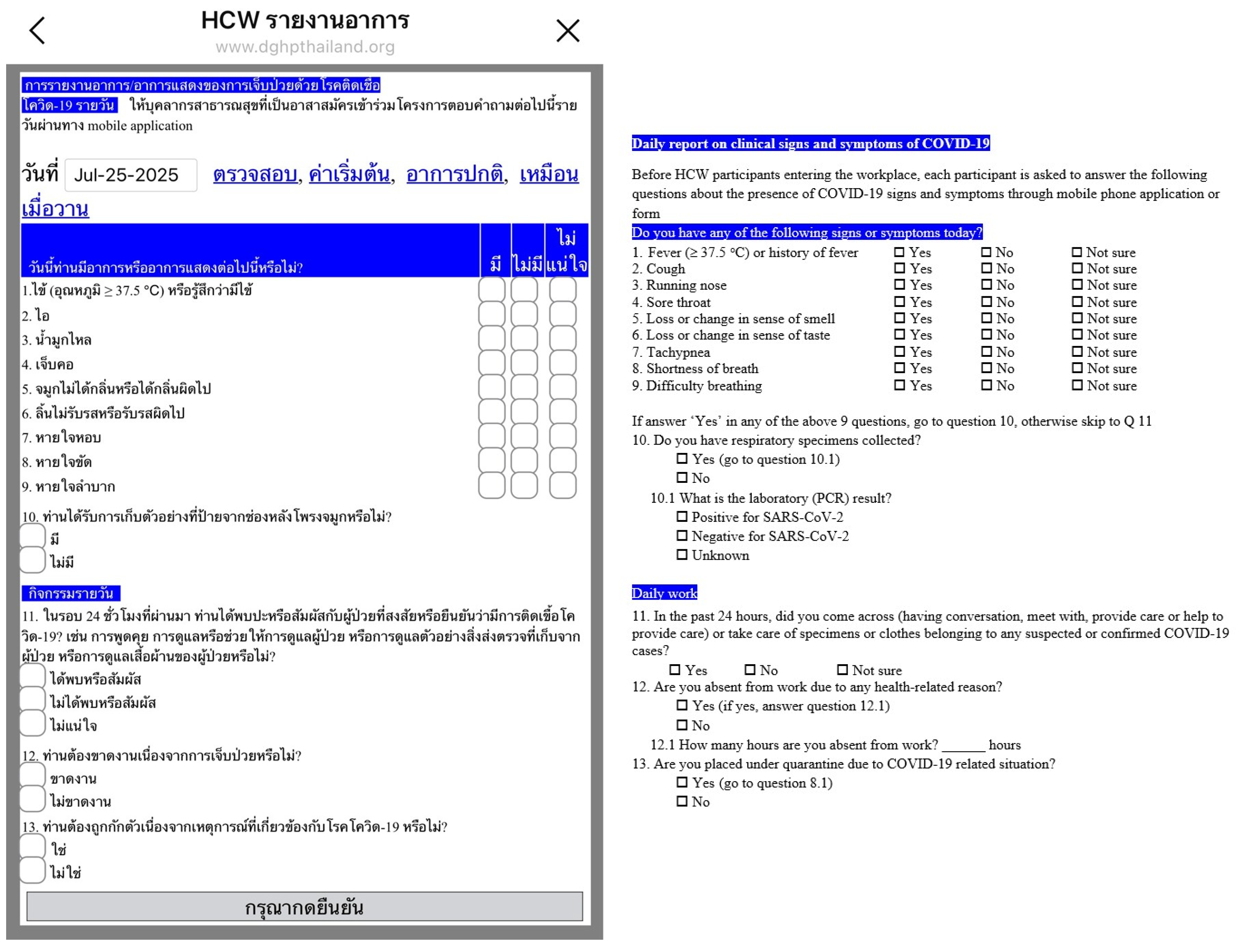
2.3. Population
2.4. Participants Enrollment
2.5. Study Procedure
2.6. Development of Electronic Mobile Application to Monitor COVID-19 Risk Management
2.7. Statistical Analysis
3. Results
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. Available online: https://data.who.int/dashboards/covid19/data dashboard (accessed on 12 July 2023).
- Bangkok Post, Thailand. Available online: https://www.bangkokpost.com/thailand/general/2004091/3-more-local-covid-transmissions-in-mae-sot (accessed on 19 October 2023).
- Department of Disease Control, Ministry of Public Health, Thailand. Guidelines on Clinical Practice, Diagnosis, Treatment, and Prevention of Healthcare-Associated Infection for COVID-19 for Medical Professionals and Public Health Personnel. Available online: https://www.ddc.moph.go.th/viralpneumonia/eng/file/guidelines/g_CPG_04Aug21.pdf (accessed on 1 April 2025).
- Department of Disease Control, Ministry of Public Health, Thailand. Guidelines for Screening, Surveillance and Investigation of COVID-19. Available online: https://www.ddc.moph.go.th/viralpneumonia/eng/file/guidelines/g_GSI_22Dec21.pdf (accessed on 1 April 2025). (In Thai)
- Whitelaw, S.; Mamas, M.A.; Topol, E.; Spall, H.G.C.V. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit. Health 2020, 8, e435–e480. [Google Scholar] [CrossRef] [PubMed]
- Chutarong, W.; Thammalikhit, R.; Kraiklang, R.; Sawangwong, A.; Saechang, O.; Guo, Y.; Zhang, W. Impact of digital device utilization on public health surveillance to enhance city resilience during the public health emergency response: A case study of SARS-CoV-2 response in Thailand (2020–2023). Digit. Health 2025, 11, 20552076241304070. [Google Scholar] [CrossRef] [PubMed]
- Intawong, K.; Olson, D.; Chariyalertsak, S. Application technology to flight the COVID-19 pandemic: Lessons learned in Thailand. Biochem. Biophys. Res. Commun. 2021, 534, 830–836. [Google Scholar] [CrossRef] [PubMed]
- Bangkok Biznews, Thailand. Available online: https://www.bangkokbiznews.com/news/986846 (accessed on 19 October 2023).
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.H.; et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Infection Prevention and Control Health-Care Facility Response for COVID-19: Interim Guidance. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/336255/WHO-2019-nCoV-HCF_assessment-IPC-2020.1-eng.pdf?sequence=1&isAllowed=y (accessed on 19 October 2023).
- Department of Disease Control, Ministry of Public Health. Guidelines for Screening, Surveillance and Investigation of COVID-19. 2020. Available online: https://ddc.moph.go.th/viralpneumonia/file/g_srrt/g_srrt_041263.pdf (accessed on 23 November 2023). (In Thai)
- Abbas, M.; Nunes, T.R.; Martischang, R.; Zingg, W.; Iten, A.; Pittet, D.; Harbarth, S. Nosocomial transmission and outbreaks of coronavirus disease 2019: The need to protect both patients and healthcare workers. Antimicrobe Resist. Infect. Control 2021, 10, 7. [Google Scholar] [CrossRef] [PubMed]
- Black, J.R.M.; Bailey, C.; Przewrocka, J.; Dijkstra, K.K.; Swanton, C. COVID-19: The case for health-care worker screening to prevent hospital transmission. Lancet 2020, 395, 1418–1420. [Google Scholar] [CrossRef] [PubMed]
- Kishk, R.M.; Nemr, N.; Aly, H.M.; Soliman, N.H.; Hagras, A.M.; Ahmed, A.A.A.; Kishk, S.M.; Mostafa, A.M.; Louis, N. Assessment of potential risk factors for coronavirus disease-19 (COVID-19) among health care workers. J. Infect. Public Health 2021, 14, 1313–1319. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Cheng, S.; Xu, K.; Yang, Y.; Zhu, Q.; Zhang, H.; Yang, D.; Cheng, S.; Xiao, H.; Wang, J.; et al. Use of personal protective equipment against coronavirus diseases 2019 by healthcare professionals in Wuhan, China: Cross sectional study. BMJ 2020, 369, m2195. [Google Scholar] [CrossRef] [PubMed]
- Erasmus, V.; Daha, T.J.; Brug, H.; Richardus, J.H.; Behrendt, M.D.; Vos, M.C.; Beeck, E.F. Systematic review of studied on compliance with hand hygiene guidelines in hospital care. Infect. Control Hosp. Epidemiol. 2010, 31, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Strain, W.D.; Jankowski, J.; Davies, A.P.; English, P.; Friedman, E.; McKeown, H.; Sethi, S.; Rao, M. Development and presentation of an objective risk stratification tool for healthcare workers when dealing with the COVID-19 pandemic in the UK: Risk modelling based on hospitalization and mortality statistics compared with epidemiological data. BMJ Open 2021, 11, e042225. [Google Scholar] [CrossRef] [PubMed]
- Song, T.; Guo, J.; Liu, B.; Yang, L.; Dai, X.; Zhang, F.; Gong, Z.; Hu, M.; Che, Q.; Shi, N. Trends in symptom prevalence and sequential onset of SARS-CoV-2 infection from 2020 to 2022 in East and Southeast Asia: A trajectory pattern exploration based on summary data. Arch. Public Health 2024, 15, 125. [Google Scholar] [CrossRef] [PubMed]
- Sha, J.; Meng, C.; Sun, J.; Sun, L.; Gu, R.; Liu, J.; Zhu, X.; Zhu, D. Clinical and upper airway characteristics of 3175 patients with the Omicron variant of SAR-CoV-2 in Changchun, China. J. Infect. Public Health 2023, 16, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Naoyuki, M.; Yasushi, N.; Makoto, O.; Naoki, F.; Akihisa, Y.; Tomoki, I. Clinical manifestations of COVID-19 Omicron variants in medical healthcare workers: Focusing on the cough. J. Infect. Chemother. 2025, 31, 102659. [Google Scholar] [CrossRef] [PubMed]
- Turer, R.W.; Jones, I.; Rosenbloom, S.T.; Slovis, C.; Ward, M.J. Electronic personal protective equipment: A strategy to protect emergency department providers in the age of COVID-19. J. Am. Med. Inform. Assoc. 2020, 27, 967–971. [Google Scholar] [CrossRef]
- Yuduang, N.; Ong, A.K.S.; Prasetyo, Y.T.; Chuenyindee, T.; Kusonwattana, P.; Limpasart, W.; Sittiwatethanasiri, T.; Gumasing, M.J.J.; German, J.D.; Nadlifatin, R. Factor influencing the perspective effectiveness of COVID-19 risk assessment mobile application “MorChana” in Thailand: UTAUT2 approach. Int. J. Environ. Res. Public Health 2022, 19, 5643. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Number (%) |
|---|---|
| Demographics | |
| Age, median (IQR) | 41 (28, 48) |
| Sex | |
| Male | 46 (15.9%) |
| Female | 243 (84.1%) |
| Vaccination doses | |
| 2 | 8(2.8%) |
| More than 2 | 281 (97.2%) |
| Job characteristics | |
| Physician | 6 (2.1%) |
| Nurse | 152 (52.6%) |
| Nurse Assistant | 23 (8.0%) |
| Laboratorian | 5 (1.7%) |
| Patient transporter | 6 (2.1%) |
| Catering staff | 7 (2.4%) |
| Cleaner/housekeeping | 10 (3.5%) |
| Admission, reception, clerk | 2 (0.7%) |
| Administrative staff | 7 (2.4%) |
| Other * | 71 (24.6%) |
| Workstation (n = 17, more than one station) | |
| Inpatient Department (IPD) | 96 (33.2%) |
| Outpatient Department (OPD) | 20 (6.9%) |
| Operating Room | 58 (20.1%) |
| COVID-19 ward | 5 (1.7%) |
| Intensive Care Unit (ICU) | 15 (5.2%) |
| Emergency Room (ER) | 21 (7.3%) |
| Acute respiratory infection (ARI) clinic | 2 (0.7%) |
| Laboratory | 5 (1.7%) |
| Cleaning section | 6 (2.1%) |
| Other | 84 (29.1%) |
| Missing | 4 (1.4%) |
| Time in position, median month (IQR) (n = 283) | 120 (41.5, 276) |
| Directly cares for patients | |
| Yes | 228 (78.9%) |
| No | 55 (19.0%) |
| Missing | 6 (2.1%) |
| Average hours taking care of patients per week (n = 228) | 40.7 |
| Median (IQR) | 40 (40, 56) |
| Smoking | |
| Yes | 12 (4.2%) |
| No | 277 (5.8%) |
| General Infection Prevention and Control (IPC) Measures | ||||||
|---|---|---|---|---|---|---|
| Characteristics (n = 289) | Yes (row %) | No (row %) | Not sure (row %) | Missing (row %) | ||
| Training on infection prevention and control (IPC) | 186 (64.4%) | 50 (17.3%) | 37 (12.8%) | 16 (5.5%) | ||
| Training on COVID-19 | 145 (50.2%) | 84 (29.1%) | 41 (14.2%) | 19 (6.6%) | ||
| Training on performing nasopharyngeal swab | 126 (43.6%) | 136 (47.1%) | 15 (5.2%) | 12 (4.2%) | ||
| Available appropriate personal protective equipment (PPE) * | 210 (72.2%) | 32 (11.1%) | 34 (11.8%) | 13 (4.5%) | ||
| Characteristics (n = 289) | Always (row %) | Most of the time (row %) | Occasionally (row %) | Rarely (row %) | Missing (row %) | |
| Follow recommended hand hygiene practices | 227 (78.5%) | 48 (16.6%) | 9 (3.1%) | 0 | 5 (1.7%) | |
| Use alcohol-based hand rub or soap and water before touching a patient | 213 (73.7%) | 53 (18.3%) | 10 (3.5%) | 2 (0.7%) | 11 (3.8%) | |
| Use alcohol-based hand rub or soap and water after touching the patient or performing any patient procedure | 236 (81.7%) | 36 (12.5%) | 5 (1.7%) | 1 (0.3%) | 11 (3.8%) | |
| Follow IPC standard precautions when in contact with any patient | 214 (74.0%) | 60 (20.8%) | 2 (0.7%) | 0 | 13 (4.5%) | |
| Wear proper PPE as required * | 219 (75.8%) | 48 (16.6%) | 5 (1.7%) | 4 (1.4%) | 13 (4.5%) | |
| Health Care Worker (HCW) Activities and Exposures to suspected or confirmed COVID-19 patients in the past 14 days | ||||||
| Characteristics (n =289) (%) | Yes (row%) | No (row%) | Not sure (row %) | Missing (row%) | ||
| Contact with anyone with an acute respiratory illness | 152 (52.6%) | 99 (34.3%) | 29 (10.0%) | 9 (3.1%) | ||
| Contact with any suspected ** or confirmed COVID-19 patients. | 175 (60.6%) | 95 (32.9%) | 13 (4.5%) | 6 (2.1%) | ||
| Physical contact with any suspected or confirmed COVID-19 patients. (n = 175) | 126 (72%) | 31 (17.7%) | 18 (10.3%) | 0 | ||
| Characteristics (n = 175) (%) | <10 (row%) | 10–49 (row %) | ≥50 (row%) | Missing (row%) | ||
| Number of suspected OR confirmed COVID-19 cases | 104 (59.4%) | 56 (32.0%) | 9 (5.1%) | 6 (3.4%) | ||
| Frequency of wearing the following PPE during activities with suspected or confirmed COVID-19 patients | ||||||
| Characteristics (n = 126) (%) | Always (row%) | Most of the time (row%) | Occasionally (row%) | Rarely (row%) | Never (row%) | Missing (row%) |
| Cloth mask | 21 (16.7%) | 0 | 0 | 2 (1.6%) | 55 (43.7%) | 48 (38.1%) |
| Surgical mask | 108 (85.7%) | 3 (2.4%) | 1 (0.8%) | 0 | 1 (0.8%) | 13 (10.3%) |
| N-95 respirator | 93 (73.8%) | 12 (9.5%) | 9 (7.1%) | 3 (2.4%) | 4 (3.2%) | 5 (4.0%) |
| Gloves | 94 (74.6%) | 12 (9.5%) | 4 (3.2%) | 3 (2.4%) | 2 (1.6%) | 11 (8.7%) |
| Disposable protective medical gown | 80 (63.5%) | 15 (11.9%) | 8 (6.3%) | 5 (4.0%) | 12 (9.5%) | 6 (4.8%) |
| Cloth gown or disposable non-medical gown | 54 (42.9%) | 19 (15.1%) | 5 (4.0%) | 5 (4.0%) | 20 (15.9%) | 23 (18.3%) |
| Goggles | 30 (23.8%) | 7 (5.6%) | 4 (4.0%) | 5 (4.0%) | 54 (42.9%) | 26 (20.6%) |
| Face shield | 82 (65.1%) | 27 (21.4%) | 4 (3.2%) | 4 (3.2%) | 3 (2.4%) | 6 (4.8%) |
| Attitudes of Health Care Workers Towards COVID-19 | ||||||
|---|---|---|---|---|---|---|
| Characteristics | Strongly agree | Agree | Indifferent | Disagree | Strongly disagree | Missing |
| Afraid of infection while caring for patient | 87 (30.1%) | 134 (46.4%) | 27 (9.3%) | 26 (9.0%) | 7 (2.4%) | 8 (2.8%) |
| Taking care of COVID-19 patient(s) causes social stigma | 32 (11.1%) | 74 (25.6%) | 55 (19.0%) | 90 (31.1%) | 30 (10.4%) | 8 (2.8%) |
| Afraid of being placed under quarantine after close contact | 36 (12.5%) | 110 (38.1%) | 34 (11.8%) | 79 (27.3%) | 21 (7.3%) | 9 (3.1%) |
| Feeling having adequate knowledge about IPC | 21 (7.3%) | 69 (23.9%) | 52 (18.0%) | 107 (37%) | 31 (10.7%) | 9 (3.1%) |
| Feeling fatigued after taking care of COVID-19 patient | 80 (27.7%) | 129 (44.6%) | 30 (10.4%) | 29 (10.9%) | 9 (3.1%) | 12 (4.2%) |
| Always wearing mask in public is a good thing to do | 235 (81.3%) | 43 (14.9%) | 1 (0.3%) | 1 (0.3%) | 1 (0.3%) | 8 (2.8%) |
| Always practicing social distancing is a good thing to do | 222 (76.8%) | 57 (19.7%) | 2 (0.7%) | 0 | 0 | 8 (2.8%) |
| Confident that collectively we can cure the disease | 184 (63.7%) | 75 (26.0%) | 19 (6.6%) | 1 (0.3%) | 0 | 10 (3.5%) |
| Patients should disclose their exposure to COVID-19 and their symptoms | 203 (70.2%) | 68 (23.5%) | 8 (2.8%) | 1 (0.3%) | 0 | 9 (3.1%) |
| Practices ofHealthCareWorkersAbout COVID-19 | ||||||
| Characteristics | Always | Most of the time | Occasionally | Rarely | Missing | |
| Maintained quarantine when appropriate | 64 (22.1%) | 56 (19.4%) | 63 (21.8%) | 98 (33.9%) | 8 (2.8%) | |
| Wears face mask in crowded places | 281 (97.2%) | 2 (0.7%) | 1 (0.3%) | 0 | 5 (1.7%) | |
| Practices hand hygiene at home | 175 (60.6%) | 80 (27.7%) | 26 (9.0%) | 2 (0.7%) | 6 (2.1%) | |
| Characteristics | SARS-CoV-2 PCR Positive n = 27 (Row %) | Bivariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| RR (95% CI) | p | Adjusted * RR (95% CI) | p | ||
| Age group | |||||
| ≥40 y | 11 (7.8%) | 0.65 (0.31, 1.35) | 0.245 | ||
| <40 y | 16 (12.0%) | Reference | |||
| Sex | |||||
| Male | 5 (11.4%) | 1.19 (0.48, 2.97) | 0.712 | ||
| Female | 22 (9.6%) | Reference | |||
| Job title | |||||
| Physician | 1 (16.7%) | 4.33 (0.53, 35.6) | 0.172 | 0.96 (0.08, 11.1) | 0.971 |
| Nurse | 15 (10.6%) | 2.75 (0.82, 9.20) | 0.101 | 1.86 (0.53, 6.53) | 0.331 |
| Nurse assistant | 5 (21.7%) | 5.65 (1.46, 21.9) | 0.012 | 3.87 (0.96, 15.6) | 0.058 |
| Patient caregiver | 3 (12.0%) | 3.12 (0.67, 14.5) | 0.146 | 2.96 (0.64, 13.6) | 0.163 |
| Other ** | 3 (3.8%) | Reference | |||
| Work Location | |||||
| Inpatient department | |||||
| Yes | 15 (17.0%) | 2.64 (1.29, 5.40) | 0.008 | 2.37 (1.09, 5.15) | 0.030 |
| No | 12 (6.5%) | Reference | |||
| Outpatient department | |||||
| Yes | 2 (11.1%) | 1.14 (0.29, 4.43) | 0.852 | ||
| No | 25 (9.8%) | Reference | |||
| Operating room | |||||
| Yes | 4 (6.8%) | 0.63 (0.23, 1.79) | 0.382 | ||
| No | 23 (10.7%) | Reference | |||
| COVID-19 ward | |||||
| Yes | 2 (40.0%) | 4.30 (1.38, 13.4) | 0.012 | 5.97 (1.32, 26.9) | 0.020 |
| No | 25 (9.3%) | Reference | |||
| Intensive care unit | |||||
| Yes | 2 (13.3%) | 1.38 (0.36, 5.29) | 0.637 | ||
| No | 25 (9.7%) | Reference | |||
| Emergency room | |||||
| Yes | 3 (13.6%) | 1.43 (0.47, 4.38) | 0.529 | ||
| No | 24 (9.5%) | Reference | |||
| Acute respiratory infection clinic | |||||
| Yes | 1 (50.0%) | 5.23 (1.25, 21.9) | 0.024 | ||
| No | 26 (9.6%) | Reference | |||
| Laboratory | |||||
| Yes | 0 (0%) | NA | - | ||
| No | 27 (10.0%) | ||||
| Cleaning section | |||||
| Yes | 0 (0%) | NA | - | ||
| No | 27 (10.1%) | ||||
| Other *** | |||||
| Yes | 6 (7.4%) | 0.68 (0.29, 1.62) | 0.386 | ||
| No | 21 (10.9%) | Reference | |||
| Work Location | |||||
| ≥2 units/departments | 3 (17.6%) | 1.89 (0.63, 5.65) | 0.255 | ||
| 1 unit/department | 24 (9.3%) | Reference | |||
| Direct care for patients (n = 269) | |||||
| Yes | 23 (10.6) | 1.35 (0.48, 3.72) | 0.568 | ||
| No | 4 (7.8%) | Reference | |||
| Direct contact with patients (n = 264) | |||||
| Yes | 21 (10.3%) | 1.26 (0.49, 3.20) | 0.625 | ||
| No | 5 (8.2%) | Reference | |||
| Existing medical conditions | |||||
| Yes | 7 (8.9%) | 0.86 (0.38, 1.96) | 0.727 | ||
| No | 20 (10.3%) | Reference | |||
| Existing Medical Conditions | |||||
| Obesity | |||||
| Yes | 3 (15.1%) | 1.59 (0.52, 4.81) | 0.415 | ||
| No | 24 (9.4%) | ||||
| Hypertension | |||||
| Yes | 3 (10.0%) | 1.02 (0.33, 3.18) | 0.977 | ||
| No | 24 (9.8%) | ||||
| Diabetes | |||||
| Yes | 1 (16.7%) | 1.72 (0.28, 10.7) | 0.561 | ||
| No | 26 (9.7%) | ||||
| Cancer | |||||
| Yes | 0 (0.0%) | NA | - | ||
| No | 27 (10.0%) | ||||
| Cardiovascular disease | |||||
| Yes | 0 (0.0%) | NA | - | ||
| No | 27 (10.0%) | ||||
| Smoking | |||||
| Yes | 0 (0.0%) | NA | - | ||
| No | 27 (10.3%) | ||||
| COVID-19 vaccination | |||||
| 2 doses | 1 (14.3%) | 1.47 (0.23, 9.34) | 0.685 | ||
| >2 doses | 26 (9.7%) | Reference | |||
| Infection, prevention, and control training (n = 260) | |||||
| Yes | 16 (8.9%) | 0.80 (0.37, 1.74) | 0.581 | ||
| No/Not sure | 9 (11.1%) | Reference | |||
| Training on COVID-19 (n = 257) | |||||
| Yes | 12 (8.6%) | 0.84 (0.39, 1.79) | 0.644 | ||
| No/Not sure | 12 (10.3%) | Reference | |||
| Characteristics | SARS-CoV-2 PCR Positive (%) |
|---|---|
| Cough | 23 (85.2) |
| Sore throat | 21 (77.8) |
| Runny nose | 20 (74.1) |
| Fever | 12 (44.4) |
| Change or loss of smell | 4 (14.8) |
| Change or loss of taste | 3 (11.1) |
| Short of breath | 2 (7.4) |
| Difficulty breathing | 2 (7.4) |
| Tachypnea | 1 (3.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sawanpanyalert, N.; Chuenchom, N.; Chen, M.-Y.; Tantilipikara, P.; Chunwimaleung, S.; Nuankum, T.; Samanmit, Y.; Petersen, B.W.; Heffelfinger, J.D.; Bloss, E.; et al. Risk of SARS-CoV-2 Infection Among Hospital-Based Healthcare Workers in Thailand at Myanmar Border, 2022. COVID 2025, 5, 115. https://doi.org/10.3390/covid5080115
Sawanpanyalert N, Chuenchom N, Chen M-Y, Tantilipikara P, Chunwimaleung S, Nuankum T, Samanmit Y, Petersen BW, Heffelfinger JD, Bloss E, et al. Risk of SARS-CoV-2 Infection Among Hospital-Based Healthcare Workers in Thailand at Myanmar Border, 2022. COVID. 2025; 5(8):115. https://doi.org/10.3390/covid5080115
Chicago/Turabian StyleSawanpanyalert, Narumol, Nuttagarn Chuenchom, Meng-Yu Chen, Peangpim Tantilipikara, Suchin Chunwimaleung, Tussanee Nuankum, Yuthana Samanmit, Brett W. Petersen, James D. Heffelfinger, Emily Bloss, and et al. 2025. "Risk of SARS-CoV-2 Infection Among Hospital-Based Healthcare Workers in Thailand at Myanmar Border, 2022" COVID 5, no. 8: 115. https://doi.org/10.3390/covid5080115
APA StyleSawanpanyalert, N., Chuenchom, N., Chen, M.-Y., Tantilipikara, P., Chunwimaleung, S., Nuankum, T., Samanmit, Y., Petersen, B. W., Heffelfinger, J. D., Bloss, E., Thamthitiwat, S., & Lurchachaiwong, W. (2025). Risk of SARS-CoV-2 Infection Among Hospital-Based Healthcare Workers in Thailand at Myanmar Border, 2022. COVID, 5(8), 115. https://doi.org/10.3390/covid5080115






