Abstract
Background: Severe and critical forms of COVID-19 have been associated with high mortality, particularly in vulnerable or underrepresented populations. The neutrophil-to-lymphocyte ratio (NLR) is an emerging inflammatory biomarker that may aid in early risk stratification. Objective: To evaluate the prognostic value of the NLR in hospitalized patients with severe or critical COVID-19 and assess its association with in-hospital mortality in the Yucatecan Maya population of southeastern Mexico. Methods: This retrospective cohort study included 172 adult patients admitted with severe or critical COVID-19 to a tertiary care center in Yucatán, Mexico. Clinical, demographic, and laboratory variables were analyzed. Univariate and multivariate logistic regression were used to identify predictors of in-hospital mortality. ROC analysis determined the optimal NLR threshold. Results: Among the 172 patients, 79 (45.9%) died during hospitalization. Non-survivors exhibited significantly higher NLR values compared to survivors (median 18.4 vs. 6.3; p < 0.001). In multivariate analysis, the NLR remained an independent predictor of mortality (OR 1.66; 95% CI: 1.26–2.17; p < 0.001). The ROC curve showed an AUC of 0. 0.83 for Intensive Care Unit and 903 for in hospital death. Conclusions: In this regional cohort of the Yucatecan Maya population, the NLR was a strong independent predictor of mortality in patients with severe or critical COVID-19. The identified cutoff of the NLR ≥ 9.76 may serve as a valuable, low-cost tool for early risk assessment in similar settings with limited resources.
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in over 761 million confirmed cases and 6.8 million deaths globally, as reported by the World Health Organization in mid-2023 [1]. In Mexico, COVID-19 has been among the leading causes of death, with more than 330,000 confirmed fatalities and over 7.6 million cases, positioning the country as one of the most severely affected worldwide [2]. The Yucatan region, particularly the city of Merida, has reported the highest concentration of cases and deaths in southeastern Mexico [3].
COVID-19 severity ranges from mild symptoms to acute respiratory distress syndrome and multi-organ failure. Severe or critical presentations are often characterized by dysregulated inflammatory responses, prompting the search for reliable, accessible, and cost-effective prognostic biomarkers [4]. Among several hematological indices, the neutrophil-to-lymphocyte ratio (NLR) has emerged as a promising marker for predicting disease progression and mortality. Elevated NLR reflects an imbalance between innate (neutrophilic) and adaptive (lymphocytic) immunity, which is particularly relevant in the hyperinflammatory state observed in severe COVID-19 [5,6,7].
Several studies across different populations have confirmed that higher NLR values are associated with increased risk of admission to Intensive Care Units (ICUs), mechanical ventilation, and death [8,9,10]. However, data specific to Latin American populations, especially those with high prevalence of cardiometabolic and respiratory comorbidities, remain scarce. Moreover, there is limited evidence from southeastern Mexico—home to the Yucatecan population, which has unique demographic, genetic, and socioeconomic characteristics that may influence COVID-19 outcomes [11,12].
In the absence of advanced laboratory testing in many resource-limited settings, the NLR, derived from routine complete blood count (CBC), offers a low-cost alternative for risk stratification. Its utility becomes even more crucial when more specific biomarkers like IL-6, ferritin, or procalcitonin are unavailable or delayed [13].
COVID-19 can trigger a stronger immune and inflammatory response than can be evidenced with laboratory tests displaying neutrophilia and lymphopenia, the latter is caused in part as a result of T-cell reduction, which is a known marker of severe viral infections. By obtaining the ratio between these two values, the increase in neutrophils in coexistence with the decrease in lymphocytes is obtained together, in a stronger indicator for severity and adverse outcomes [14,15].
Therefore, this study aims to evaluate the prognostic value of the neutrophil-to-lymphocyte ratio in hospitalized patients with severe or critical COVID-19 at a regional referral center in Yucatan, Mexico.
2. Materials and Methods
2.1. Study Design and Setting
This was a retrospective, observational study conducted at the Hospital General Agustín O’Horan, a tertiary referral center located in Merida, Yucatan, Mexico. For the present study, we analyzed electronic medical records of patients hospitalized with severe or critical COVID-19 between January 2020 and December 2022. This hospital serves as a major public health institution for the Yucatecan population, particularly during the peak of the first four pandemic waves.
2.2. Population and Inclusion Criteria
We included adult patients (≥18 years old) with a confirmed diagnosis of SARS-CoV-2 infection by real-time reverse transcription polymerase chain reaction (RT-PCR). Eligible patients met World Health Organization (WHO) clinical criteria for severe or critical COVID-19, including hypoxemia, respiratory failure, or requirement of intensive care support.
Patients were included if they:
- Were hospitalized between January 2020 and December 2022.
- Had available laboratory data, including neutrophil and lymphocyte counts upon admission.
- Had clearly documented in-hospital outcomes (discharge or death).
2.3. Exclusion Criteria
We excluded patients with:
- Mild or moderate COVID-19.
- Missing key clinical or laboratory data at admission.
- Transfer to other institutions before outcome determination.
- History of immunosuppressive or immunomodulatory therapy.
- Chronic inflammatory or hematological diseases that could confound the NLR interpretation.
2.4. Data Collection
Demographic data (age, sex), clinical variables (symptom duration, comorbidities including diabetes mellitus type 2, hypertension, asthma, chronic obstructive pulmonary disease [COPD], and dyslipidemia), and laboratory findings at admission were extracted. Laboratory parameters included leukocyte count, absolute neutrophil and lymphocyte counts, the NLR (calculated as neutrophils/lymphocytes), lactate dehydrogenase (LDH), D-dimer, ferritin, fibrinogen, creatinine, and procalcitonin.
The primary outcome was in-hospital mortality. Secondary outcomes included ICU admission and invasive mechanical ventilation (IMV) requirement.
2.5. Statistical Analysis
Continuous variables were expressed as mean ± standard deviation or median with interquartile range, depending on normality. Categorical variables were presented as frequencies and percentages. Differences between survivors and non-survivors were assessed using Student’s t-test or Mann–Whitney U test for continuous variables, and chi-square or Fisher’s exact test for categorical variables.
A logistic regression analysis was performed to identify independent predictors of mortality, including the NLR and relevant covariates. Multivariate models were adjusted for age, sex, and comorbidities. Receiver Operating Characteristic (ROC) curve analysis was conducted to determine the optimal NLR cut-off for predicting mortality, and the area under the curve (AUC) was reported. Statistical significance was set at p < 0.05. Analyses were conducted using SPSS version 26.0 (IBM Corp., Armonk, NY, USA).
2.6. Ethical Considerations
This study was approved by the Ethics and Research Committees of Hospital General Agustín O’Horan (protocol ID: FMED-00264). All data were anonymized to ensure confidentiality in accordance with the Declaration of Helsinki and national regulations on health research.
3. Results
3.1. Baseline Characteristics
A total of 172 patients with severe or critical COVID-19 were included. The median age was 61 years (range 18–92), with a mean of 56.4 years. The majority were male (59.3%). The overall in-hospital mortality rate was 45.8% (n = 79).
The most prevalent comorbidities were type 2 diabetes mellitus (46.1%), arterial hypertension (40.5%), and dyslipidemia (27.5%). Asthma was present in 22.2% of patients and was significantly associated with mortality (p < 0.001), while COPD was observed in 11.3% but did not reach statistical significance in univariate analysis. Notably, 35.9% of patients had no known comorbidities.
ICU admission was required in 61.2% of cases, and 54.8% required invasive mechanical ventilation. Among patients who were admitted to the ICU or required IMV, approximately half died during hospitalization. Table 1 summarizes the clinical and demographic characteristics stratified by survival status.

Table 1.
Sociodemographic characteristics of patients from a COVID-19 retrospective cohort.
3.2. Laboratory Findings and the NLR Differences
Patients who died had significantly higher levels of leukocytes (mean 14.1 vs. 8.5 × 103/μL), neutrophils (12.6 vs. 7.2 × 103/μL), and NLR (18.4 vs. 6.3; p < 0.001), and significantly lower lymphocyte counts (0.9 vs. 1.4 × 103/μL; p < 0.001).
Markers of organ dysfunction were also elevated among non-survivors, including serum urea (58.9 vs. 27.4 mg/dL), BUN, creatinine, and LDH (436.9 vs. 306.0 U/L). Fibrinogen levels were significantly higher in non-survivors (495.3 vs. 355.6 mg/dL), suggesting a more pronounced inflammatory and prothrombotic state. Table 2 displays the comparative laboratory values between survivors and non-survivors.

Table 2.
Comparison between laboratory values of survivors and non-survivors’ laboratory results.
3.3. Multivariate Analysis
In multivariate logistic regression, the neutrophil-to-lymphocyte ratio (NLR) remained an independent predictor of mortality (OR 1.661; 95% CI: 1.269–2.172; p < 0.001). Comorbidities significantly associated with mortality included asthma (OR 10.05; p = 0.002), COPD (OR 10.89; p = 0.018), and type 2 diabetes mellitus (OR 5.23; p = 0.025). Other inflammatory markers, such as LDH and fibrinogen, showed significance in univariate analysis but did not retain statistical significance in the adjusted model. Table 3 summarizes the combined clinical and laboratory risk factors associated with mortality.

Table 3.
Univariate and multivariate association between individual predictors of mortality.
3.4. ROC Analysis
The ROC analysis demonstrated that the NLR has a highly predictive value for Intensive Care Unit admission and mortality, with an AUC of 0.828 and 0.903, respectively. The optimal cut-off point for Intensive Care Unit was 7.7, for an area under the curve of 82, while mortality prediction was identified at the NLR ≥ 9.76, yielding a sensitivity of 85.7% and specificity of 70.3%; Figure 1 illustrates the ROC curve of the NLR for the Intensive Care Unit, mechanical ventilation and in-hospital mortality prediction.
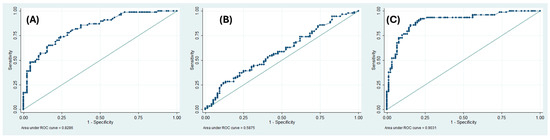
Figure 1.
Neutrophil/leukocyte ratio predicting (A) Intensive Care Unit (B) Mechanical ventilation (C) In-hospital mortality.
3.5. Secondary Outcomes
A higher NLR was also significantly associated with ICU admission (OR 0.897; 95% CI: 0.81–0.99; p = 0.046), indicating a greater risk of requiring intensive care. However, no statistically significant association was found between the NLR and the need for invasive mechanical ventilation (OR 0.953; 95% CI: 0.88–1.04; p = 0.171).
4. Discussion
The present study assessed the neutrophil-to-lymphocyte ratio (NLR) as an independent prognostic biomarker of in-hospital mortality in patients with severe or critical COVID-19 in a cohort from the Yucatan Peninsula. Even when neutrophil and lymphocyte counts are associated with adverse outcomes, the NLR, as a measure combining these two markers, predicts better. Elevated NLR values have been consistently associated with systemic inflammation and immune dysregulation—hallmarks of severe SARS-CoV-2 infection—across various global populations [1,5,8]. Our findings align with these reports; however, they offer novel insights by highlighting a notably higher optimal cutoff value of the NLR ≥ 7.7 for ICU and NLR ≥ 9.76 for mortality in this particular Mexican population.
The multivariate analysis showed that each unit increase in the NLR was associated with a 66% higher risk of death, independent of age, sex, and comorbidities. While previous studies, such as Liu et al., identified lower thresholds (e.g., NLR > 3.13) for increased mortality risk [9], the higher value observed in our cohort likely reflects a greater inflammatory burden, possibly influenced by prevalent comorbidities and delayed access to care. This underscores the importance of context-specific cutoffs when applying inflammatory biomarkers in diverse populations.
Asthma, chronic obstructive pulmonary disease (COPD), and type 2 diabetes mellitus emerged as significant clinical predictors of mortality. These associations are consistent with prior Latin American studies that have emphasized the deleterious interplay between chronic inflammatory conditions and COVID-19 outcomes [11,12,13]. Notably, asthma demonstrated an exceptionally strong association (OR > 10), which may reflect a higher prevalence of underrecognized severe phenotypes or suboptimal outpatient disease control in the region.
Interestingly, the NLR also exhibited predictive value for ICU admission, supporting its potential utility in early risk stratification and triage. However, no significant association was found between the NLR and the requirement for invasive mechanical ventilation (IMV). This may be attributed to the study’s retrospective nature and the absence of dynamic respiratory indicators—such as PaO2/FiO2 ratios or imaging severity scores—that more directly influence decisions about mechanical ventilation.
Other laboratory markers, including LDH and fibrinogen, were significantly associated with mortality in univariate analysis but lost statistical significance in multivariate models. This suggests that the NLR may more comprehensively reflect the immune/inflammatory milieu involved in COVID-19 pathogenesis than isolated biomarkers [7,16].
In summary, our study adds to the growing body of evidence supporting the NLR as an accessible, low-cost tool for prognostic assessment in severe COVID-19. Moreover, by identifying a population-specific cutoff, we provide data that may inform clinical decision-making in similar resource-constrained, ethnically distinct populations.
Limitations
Several limitations should be acknowledged. First, the retrospective and single-center design limits the generalizability of the results to broader populations. Second, while multivariate adjustment was performed, residual confounding from unmeasured factors—such as vaccination status, socioeconomic determinants, or delays in seeking care—may have influenced outcomes. Third, the study did not include repeated NLR measurements, preventing analysis of dynamic trends and temporal associations with clinical deterioration or recovery.
These limitations underscore the need for future prospective, multicenter studies with standardized biomarker monitoring to better define the prognostic utility of the NLR across diverse Latin American populations.
A key strength of this study lies in its focus on a hospitalized population from Yucatan, specifically individuals of Yucatecan Maya descent—a group historically underrepresented in COVID-19 research. Additionally, the use of readily available hematologic indices, such as the neutrophil-to-lymphocyte ratio (NLR), enhances the translational relevance of the findings in real-world, low-resource settings.
Given its simplicity, low cost, and high sensitivity, the NLR can be a valuable tool for early risk stratification in severe COVID-19. It may help guide resource allocation, particularly in settings with limited access to advanced laboratory or imaging studies. Future prospective studies should explore NLR kinetics during hospitalization and its integration into multiparametric scoring systems.
5. Conclusions
In this retrospective study of hospitalized patients with severe or critical COVID-19 in Yucatan, Mexico, the neutrophil-to-lymphocyte ratio (NLR) was identified as a strong, independent predictor of in-hospital mortality. An NLR ≥ 9.76 significantly increased the risk of death and was also associated with a higher likelihood of Intensive Care Unit admission. These findings support the use of the NLR as an accessible and cost-effective biomarker for early risk stratification in resource-limited settings.
The results also emphasize the impact of comorbidities—particularly asthma, COPD, and type 2 diabetes mellitus—on COVID-19-related mortality in the Yucatecan population. Incorporating NLR into clinical decision-making may improve patient outcomes by identifying those at higher risk who may benefit from earlier or more aggressive intervention.
Further prospective, multicenter studies are needed to validate these findings and explore the temporal dynamics of NLR during hospitalization, as well as its role in predicting long-term outcomes.
Author Contributions
Conceptualization: A.I.A.B. and N.M.-D.; Data curation: V.J.T.R. and A.I.A.B.; Formal analysis: A.I.A.B. and O.A.P.P.; Investigation: A.I.A.B. and V.J.T.R.; Methodology: N.M.-D. and A.I.A.B.; Project administration: N.M.-D.; Supervision: N.M.-D. and O.A.P.P.; Writing—original draft: A.I.A.B.; Writing—review and editing: All authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics and Research Committee of Hospital General Agustín O’Horan (protocol code FMED-00264, approved on 6 November 2024).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study and the use of anonymized data, in accordance with institutional policies and national regulations on health research.
Data Availability Statement
The data supporting the findings of this study are available upon reasonable request from the corresponding author.
Acknowledgments
The authors would like to thank the medical and administrative staff of Hospital General Agustín O’Horan for their support during the data collection phase of this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| NLR | Neutrophil leucocyte ratio |
| OR | Odds Ratio |
References
- World Health Organization. Weekly Epidemiological Update on COVID-19—29 June 2023. 2023. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---29-june-2023 (accessed on 2 June 2025).
- Alcocer Varela, J.C.; López-Gatell Ramírez, H. Informe integral de COVID-19 en México: Volumen 01-2023. Gobierno de México. 2023. Available online: https://coronavirus.gob.mx (accessed on 2 June 2025).
- Instituto Nacional de Estadística y Geografía (INEGI). Comunicado de Prensa Núm. 29/23—24 de Enero de 2023. 2023. Available online: https://www.inegi.org.mx (accessed on 2 June 2025).
- Liu, Y.; Du, X.; Chen, J.; Jin, Y.; Peng, L.; Wang, H.H.X.; Luo, M.; Chen, L.; Zhao, Y. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J. Infect. 2020, 81, e6–e12. [Google Scholar] [CrossRef] [PubMed]
- Ulloque-Badaracco, J.R.; Salas-Tello, W.I.; Al-Kassab-Córdova, A.; Alarcón-Braga, E.A.; Benites-Zapata, V.A.; Maguiña, J.L.; Hernandez, A.V. Prognostic value of neutrophil-to-lymphocyte ratio in COVID-19 patients: A systematic review and meta-analysis. Int. J. Clin. Pract. 2021, 75, e14596. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.P.; Liu, J.P.; Tao, W.Q.; Li, H.M. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int. Immunopharmacol. 2020, 84, 106504. [Google Scholar] [CrossRef] [PubMed]
- Zeng, F.; Huang, Y.; Guo, Y.; Yin, M.; Chen, X.; Xiao, L.; Deng, G. Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int. J. Infect. Dis. 2020, 96, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Liu, Y.; Xiang, P.; Pu, L.; Xiong, H.; Li, C.; Zhang, M.; Tan, J.; Xu, Y.; Song, R.; et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J. Transl. Med. 2020, 18, 206. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Wang, Q.; Zhang, D.; Ding, J.; Huang, Q.; Tang, Y.Q.; Wang, Q.; Miao, H. Lymphopenia predicts disease severity of COVID-19: A descriptive and predictive study. Signal Transduct. Target. Ther. 2020, 5, 33. [Google Scholar] [CrossRef] [PubMed]
- Altuve-Quiroz, J.; Fernández-Reynoso, C.; Mondragón-Soto, M.G.; Juárez-Ramírez, J.I. The Role of Biochemical and Respiratory Markers in the Mortality of Patients with SARS-CoV-2 Infection in a Mexican Population. Cureus 2022, 14, e26249. [Google Scholar] [CrossRef] [PubMed]
- Olivas-Martínez, A.; Cárdenas-Fragoso, J.L.; Jiménez, J.V.; Lozano-Cruz, O.A.; Ortiz-Brizuela, E.; Tovar-Méndez, V.H.; Medrano-Borromeo, C.; Martinez-Valenzuela, A.; Román-Montes, C.M.; Martinez-Guerra, B.; et al. In-hospital mortality from severe COVID-19 in a tertiary care center in Mexico City. PLoS ONE 2021, 16, e0245772. [Google Scholar] [CrossRef] [PubMed]
- Núñez, I.; Priego-Ranero, Á.A.; García-González, H.B.; Jiménez-Franco, B.; Bonilla-Hernández, R.; Domínguez-Cherit, G.; Merayo-Chalico, J.; Crispín, J.C.; Barrera-Vargas, A.; Valdés-Ferrer, S.I. Common hematological values predict unfavorable outcomes in hospitalized COVID-19 patients. Clin. Immunol. 2021, 225, 108682. [Google Scholar] [CrossRef] [PubMed]
- Lagunas-Rangel, F.A. Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): A meta-analysis. J. Med. Virol. 2020, 92, 1733–1734. [Google Scholar] [CrossRef] [PubMed]
- Messaoud-Nacer, Y.; Culerier, E.; Rose, S.; Maillet, I.; Rouxel, N.; Briault, S.; Ryffel, B.; Quesniaux, V.F.J.; Togbe, D. STING agonist diABZI induces PANoptosis and DNA mediated acute respiratory distress syndrome (ARDS). Cell Death Dis. 2022, 13, 269. [Google Scholar] [CrossRef] [PubMed]
- Sefik, E.; Qu, R.; Junqueira, C.; Kaffe, E.; Mirza, H.; Zhao, J.; Brewer, J.R.; Han, A.; Steach, H.R.; Israelow, B.; et al. Inflammasome activation in infected macrophages drives COVID-19 pathology. Nature 2022, 606, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Ye, W.; Chen, G.; Li, X.; Lan, X.; Ji, C.; Hou, M.; Zhang, D.; Zeng, G.; Wang, Y.; Xu, C.; et al. Dynamic changes of D-dimer and neutrophil-lymphocyte count ratio as prognostic biomarkers in COVID-19. Respir. Res. 2020, 21, 169. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).