Determinants of Behavioral Intention and Compliance Behavior Among Transportation Network Vehicle Service Drivers During the COVID-19 Pandemic
Abstract
1. Introduction
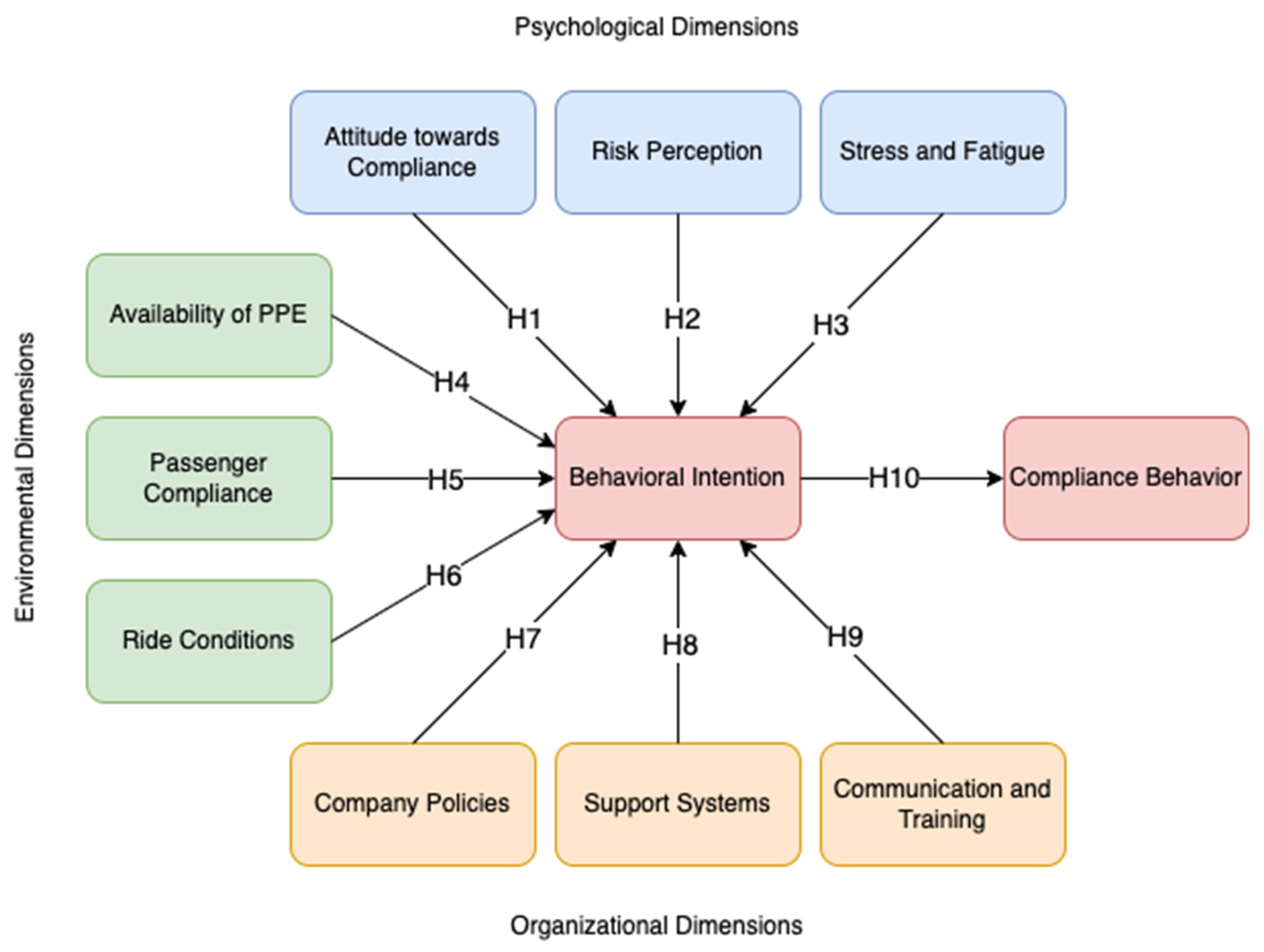
2. Conceptual Framework
Determinants of Behavioral Intention and Compliance Behavior
3. Methodology
3.1. Respondents of the Study
3.2. Instrumentation
3.3. Structural Equation Modeling
4. Results
4.1. Respondent’s Profile
4.2. Result of Initial SEM
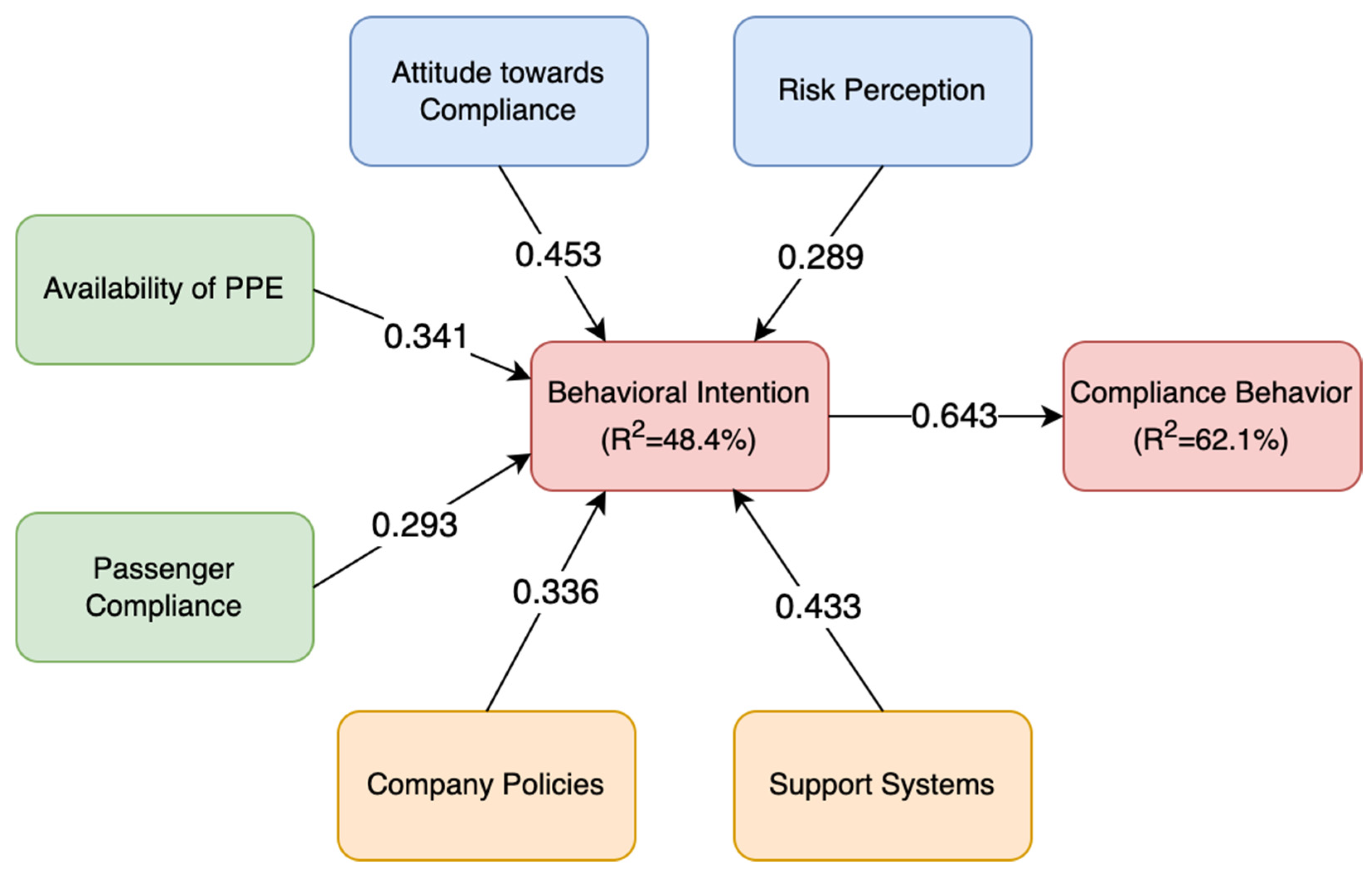
4.3. Results of Final SEM
5. Discussion
6. Conclusions
6.1. Theoretical and Practical Implications
6.2. Limitations and Future Research
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rothengatter, W.; Zhang, J.; Hayashi, Y.; Nosach, A.; Wang, K.; Oum, T.H. Pandemic waves and the time after Covid-19–Consequences for the transport sector. Transp. Policy 2021, 110, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Aranguren MA, G.; Candelaria JD, L.; De Guzman, F.L.; Sia, A.F.; Roquel, K.I.D. Structural Equation Modeling on the Impacts of COVID-19 on the Operations of Transportation Network Vehicle Services in Metro Manila. J. Comput. Innov. Eng. Appl. 2022, 6, 28–39. [Google Scholar]
- Chuenyindee, T.; Ong AK, S.; Ramos, J.P.; Prasetyo, Y.T.; Nadlifatin, R.; Kurata, Y.B.; Sittiwatethanasiri, T. Public utility vehicle service quality and customer satisfaction in the Philippines during the COVID-19 pandemic. Util. Policy 2022, 75, 101336. [Google Scholar] [CrossRef]
- Gaspay, S.M.A. Sustainable Urban Transport Index for Metro Manila and Impacts of COVID-19 on Mobility. 2021. Available online: https://repository.unescap.org/handle/20.500.12870/4156 (accessed on 21 December 2024).
- Dzisi, E.K.J.; Dei, O.A. Adherence to social distancing and wearing of masks within public transportation during the COVID 19 pandemic. Transp. Res. Interdiscip. Perspect. 2020, 7, 100191. [Google Scholar] [CrossRef]
- Bauer, M.; Dźwigoń, W.; Richter, M. Personal safety of passengers during the first phase Covid-19 pandemic in the opinion of public transport drivers in Krakow. Arch. Transp. 2021, 59, 41–55. [Google Scholar] [CrossRef]
- Natnael, T.; Alemnew, Y.; Berihun, G.; Abebe, M.; Andualem, A.; Ademe, S.; Tegegne, B.; Adane, M. Facemask wearing to prevent COVID-19 transmission and associated factors among taxi drivers in Dessie City and Kombolcha Town, Ethiopia. PLoS ONE 2021, 16, e0247954. [Google Scholar] [CrossRef]
- Roquel, K.I.D.; Aranguren, M.A.G.; Candelaria, J.D.L.; De Guzman, F.L.; Sia, A.F. Impact of the COVID-19 Pandemic on the Operations of Transportation Network Vehicle Services (TNVS) in Metro Manila. In Proceedings of the Annual National Conference of the Transportation Science Society of the Philippines, The 27th Annual Conference of Transportation Science Society of the Philippines, 19 November 2021. Webinar via Zoom. [Google Scholar]
- Lucchesi, S.T.; Tavares, V.B.; Rocha, M.K.; Larranaga, A.M. Public transport COVID-19-safe: New barriers and policies to implement effective countermeasures under user’s safety perspective. Sustainability 2022, 14, 2945. [Google Scholar] [CrossRef]
- Yin, Y.; Li, D.; Zhang, S.; Wu, L. How does railway respond to the spread of COVID-19? Countermeasure analysis and evaluation around the world. Urban Rail Transit 2021, 7, 29–57. [Google Scholar] [CrossRef]
- Shodunke, A.O. Enforcement of COVID-19 pandemic lockdown orders in Nigeria: Evidence of public (non) compliance and police illegalities. Int. J. Disaster Risk Reduct. 2022, 77, 103082. [Google Scholar] [CrossRef]
- Németh, J.; Tokodi, P. Law enforcement challenges and tasks during the COVID-19 pandemic. Cas. Polic. Teor. A Prax 2022, 2, 106–122. [Google Scholar]
- Yassin, J.; Rani, U. Ride-Hailing Versus Traditional Taxi Services: The Experiences of Taxi Drivers in Lebanon (No. 85); ILO Working Paper; ILO: Geneva, Switzerland, 2022. [Google Scholar] [CrossRef]
- Beckman, K.L.; Monsey, L.M.; Archer, M.M.; Errett, N.A.; Bostrom, A.; Baker, M.G. Health and safety risk perceptions and needs of app-based drivers during COVID-19. Am. J. Ind. Med. 2021, 64, 941–951. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Duan, H.; Zhang, B.; Wang, J.; Ji, J.S.; Wang, J.; Pan, L.; Wang, X.; Zhao, K.; Ying, B.; et al. Prevention and control of COVID-19 in public transportation: Experience from China. Environ. Pollut. 2020, 266, 115291. [Google Scholar] [CrossRef]
- Harrington, D.M.; Hadjiconstantinou, M. Changes in commuting behaviours in response to the COVID-19 pandemic in the UK. J. Transp. Health 2022, 24, 101313. [Google Scholar] [CrossRef] [PubMed]
- Sirgy, M.J.; Shultz, C.J.; Rahtz, D.R. Effective Interventions to Mitigate the Ill-Being Effects of COVID-19: Lessons Learned from Countries around the World. In Community, Economy and COVID-19: Lessons from Multi-Country Analyses of a Global Pandemic; Springer International Publishing: Cham, Switzerland, 2022; pp. 633–666. [Google Scholar]
- Agyapon-Ntra, K.; McSharry, P.E. A global analysis of the effectiveness of policy responses to COVID-19. Sci. Rep. 2023, 13, 5629. [Google Scholar] [CrossRef]
- Taylor, D.; Bury, M.; Campling, N.; Carter, S.; Garfied, S.; Newbould, J.; Rennie, T. A Review of the Use of the Health Belief Model (HBM), the Theory of Reasoned Action (TRA), the Theory of Planned Behaviour (TPB) and the Trans-Theoretical Model (TTM) to Study and Predict Health Related Behaviour Change; National Institute for Health and Clinical Excellence: London, UK, 2006; pp. 1–215. [Google Scholar]
- Alamer, A.S. Behavior Change Theories and Models Within Health Belief Model Research: A Five-Decade Holistic Bibliometric Analysis. Cureus 2024, 16, e63143. [Google Scholar] [CrossRef]
- Qiao, X.; Ji, L.; Jin, Y.; Si, H.; Bian, Y.; Wang, W.; Wang, C. Development and validation of an instrument to measure beliefs in physical activity among (pre) frail older adults: An integration of the health belief model and the theory of planned behavior. Patient Educ. Couns. 2021, 104, 2544–2551. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior: Frequently asked questions. Hum. Behav. Emerg. Technol. 2020, 2, 314–324. [Google Scholar] [CrossRef]
- Skinner, C.S.; Tiro, J.; Champion, V.L. Background on the health belief model. Health Behav. Theory Res. Pract. 2015, 75, 1–34. [Google Scholar]
- Anagaw, T.F.; Tiruneh, M.G.; Fenta, E.T. Application of behavioral change theory and models on COVID-19 preventive behaviors, worldwide: A systematic review. SAGE Open Med. 2023, 11, 20503121231159750. [Google Scholar] [CrossRef]
- Alshagrawi, S.S. Predicting COVID-19 vaccine uptake: Comparing the health belief model and theory of planned behavior. Hum. Vaccines Immunother. 2024, 20, 2361503. [Google Scholar] [CrossRef]
- McClenahan, C.; Shevlin, M.; Adamson, G.; Bennett, C.; O’Neill, B. Testicular self-examination: A test of the health belief model and the theory of planned behaviour. Health Educ. Res. 2007, 22, 272–284. [Google Scholar] [CrossRef] [PubMed]
- Gerend, M.A.; Shepherd, J.E. Predicting human papillomavirus vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Ann. Behav. Med. 2012, 44, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Mitropoulos, P.; Memarian, B. Team processes and safety of workers: Cognitive, affective, and behavioral processes of construction crews. J. Constr. Eng. Manag. 2012, 138, 1181–1191. [Google Scholar] [CrossRef]
- Watson, B.; Tunnicliff, D.; White, K.; Schonfeld, C.; Wishart, D. Psychological and Social Factors Influencing Motorcylce Rider Intentions and Behaviour. 2007. Available online: https://www.infrastructure.gov.au/department/media/publications/psychological-and-social-factors-influencing-motorcycle-rider-intentions-and-behaviour (accessed on 18 December 2024).
- Akamangwa, N. Working for the environment and against safety: How compliance affects health and safety on board ships. Saf. Sci. 2016, 87, 131–143. [Google Scholar] [CrossRef]
- Gaube, S. Understanding the Psychological Factors Influencing Hospital Patients’ and Visitors’ Hand Hygiene Behavior. Ph.D. Thesis, Universität Regensburg, Regensburg, Germany, 2021. [Google Scholar]
- Duong, H.T.; Nguyen, H.T.; McFarlane, S.J.; Nguyen, L.T.V. Risk perception and COVID-19 preventive behaviors: Application of the integrative model of behavioral prediction. Soc. Sci. J. 2024, 61, 873–886. [Google Scholar] [CrossRef]
- Ning, L.; Niu, J.; Bi, X.; Yang, C.; Liu, Z.; Wu, Q.; Ning, N.; Liang, L.; Liu, A.; Hao, Y. The impacts of knowledge, risk perception, emotion and information on citizens’ protective behaviors during the outbreak of COVID-19: A cross-sectional study in China. BMC Public Health 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Cham, B.S.; Andrei, D.M.; Griffin, M.A.; Grech, M.; Neal, A. Investigating the joint effects of overload and underload on chronic fatigue and wellbeing. Work Stress 2021, 35, 344–357. [Google Scholar] [CrossRef]
- Mtetwa, D. The Minibus Taxi Industry, Public Health, and Passengers’ Pandemic Stories in Soweto. Master’s Thesis, University of the Witwatersrand, Johannesburg, South Africa, 2022. [Google Scholar]
- Norris, E.; Myers, L. Determinants of Personal Protective Equipment (PPE) use in UK motorcyclists: Exploratory research applying an extended theory of planned behaviour. Accid. Anal. Prev. 2013, 60, 219–230. [Google Scholar] [CrossRef]
- Rezaei, R.; Seidi, M.; Karbasioun, M. Pesticide exposure reduction: Extending the theory of planned behavior to understand Iranian farmers’ intention to apply personal protective equipment. Saf. Sci. 2019, 120, 527–537. [Google Scholar] [CrossRef]
- Sigala, I.F.; Sirenko, M.; Comes, T.; Kovács, G. Mitigating personal protective equipment (PPE) supply chain disruptions in pandemics–a system dynamics approach. Int. J. Oper. Prod. Manag. 2022, 42, 128–154. [Google Scholar] [CrossRef]
- Bloomfield, S.F.; Aiello, A.E.; Cookson, B.; O’Boyle, C.; Larson, E.L. The effectiveness of hand hygiene procedures in reducing the risks of infections in home and community settings including handwashing and alcohol-based hand sanitizers. Am. J. Infect. Control 2007, 35, S27–S64. [Google Scholar] [CrossRef]
- Manh, T.H.; Anh, N.N.; Duc, N.T.; Minh, N.B.; Huong, M.T.; Hieu, N.M. Adherence to mask wearing on public transport during the COVID-19 pandemic and influential factors: The case of Hanoi. Tạp Chí Khoa Học Giao Thông Vận Tải 2021, 72, 486–497. [Google Scholar]
- Yu, P.J.; Dahai, L. Mask-Wearing Onboard Airplanes During COVID-19-Identifying Passenger Segments Using Cluster Analysis. Med. Res. Arch. 2023, 11. [Google Scholar] [CrossRef]
- Sun, C.; Zhai, Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain. Cities Soc. 2020, 62, 102390. [Google Scholar] [CrossRef] [PubMed]
- Woodside, J. Not Just Along for the Ride: Work, Justice, and Municipal Regulation of Ridehailing Platforms. 2022. Available online: https://uwspace.uwaterloo.ca/bitstreams/9e570448-8822-41d3-b0af-8f19a9b27d61/download (accessed on 19 December 2024).
- Sanguinetti, A.; DePew, A.; Hirschfelt, K. Vehicle design strategies to reduce the risk of COVID-19 transmission in shared and pooled travel: Inventory, typology, and considerations for research and implementation. Transp. Res. Rec. 2023, 2677, 641–655. [Google Scholar] [CrossRef]
- Na, C.; Lee, B.H. Improving Voluntary Compliance through Problem-Oriented Governance: A Case Study of South Korea’s Efforts to Increase the COVID-19 Vaccination Rate. J. Asian Afr. Stud. 2023, 58, 174–195. [Google Scholar] [CrossRef]
- Mpe, T. Factors Contributing to Non-Compliance with Safety Regulations Among Cleaners: A Selected Rural University in South Africa. 2018. Available online: https://univendspace.univen.ac.za/server/api/core/bitstreams/945ffd6f-e2c9-431c-8aed-719f1498b85f/content (accessed on 18 December 2024).
- Tolera, S.T.; Gobena, T.; Geremew, A.; Toseva, E.; Assefa, N. Compliance and associated factors of personal protective equipment among sanitary workers in selected public hospitals, Eastern Ethiopia: A cross-sectional study design. SAGE Open Med. 2024, 12, 20503121241308303. [Google Scholar] [CrossRef]
- NeJhaddadgar, N.; Toghroli, R.; Yoosefi Lebni, J.; AMelca, I.; Ziapour, A. Exploring the barriers in maintaining the health guidelines amid the COVID-19 pandemic: A qualitative study approach. INQUIRY: J. Health Care Organ. Provis. Financ. 2022, 59, 00469580221100348. [Google Scholar] [CrossRef]
- Haslinda, A.; Saharudin, S.; Roslan, N.H.; Mohamed, R. Safety training, company policy and communication for effective accident management. Int. J. Acad. Res. Bus. Soc. Sci. 2016, 6, 141–158. [Google Scholar]
- Jarreau, P.B.; Su, L.Y.F.; Chiang EC, L.; Bennett, S.M.; Zhang, J.S.; Ferguson, M.; Algarra, D. COVID issue: Visual narratives about COVID-19 improve message accessibility, self-efficacy, and health precautions. Front. Commun. 2021, 6, 712658. [Google Scholar] [CrossRef]
- Enria, L.; Waterlow, N.; Rogers, N.T.; Brindle, H.; Lal, S.; Eggo, R.M.; Lees, S.; Roberts, C.H. Trust and transparency in times of crisis: Results from an online survey during the first wave (April 2020) of the COVID-19 epidemic in the UK. PLoS ONE 2021, 16, e0239247. [Google Scholar] [CrossRef]
- Alagarsamy, S.; Mehrolia, S.; Pushparaj, U.; Jeevananda, S. Explaining the intention to uptake COVID-19 vaccination using the behavioral and social drivers of vaccination (BeSD) model. Vaccine X 2022, 10, 100140. [Google Scholar] [CrossRef]
- Nasir, A.; Arshah, R.A.; Ab Hamid, M.R. The significance of main constructs of theory of planned behavior in recent information security policy compliance behavior study: A comparison among top three behavioral theories. Int. J. Eng. Technol 2018, 7, 737–741. [Google Scholar] [CrossRef]
- Aschwanden, D.; Strickhouser, J.E.; Sesker, A.A.; Lee, J.H.; Luchetti, M.; Terracciano, A.; Sutin, A.R. Preventive behaviors during the COVID-19 pandemic: Associations with perceived behavioral control, attitudes, and subjective norm. Front. Public Health 2021, 9, 662835. [Google Scholar] [CrossRef] [PubMed]
- Carlucci, L.; D’ambrosio, I.; Balsamo, M. Demographic and attitudinal factors of adherence to quarantine guidelines during COVID-19: The Italian model. Front. Psychol. 2020, 11, 559288. [Google Scholar] [CrossRef]
- Nguyen-Phuoc, D.Q.; Su, D.N.; Dinh MT, T.; Newton, J.D.A.; Oviedo-Trespalacios, O. Passengers’ self-protective intentions while using ride-hailing services during the COVID-19 pandemic. Saf. Sci. 2023, 157, 105920. [Google Scholar] [CrossRef] [PubMed]
- Kyriazos, T.A. Applied psychometrics: Sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology 2018, 9, 2207. [Google Scholar] [CrossRef]
- Sasaki, N.; Imamura, K.; Kataoka, M.; Kuroda, R.; Tsuno, K.; Sawada, U.; Asaoka, H.; Iida, M.; Kawakami, N. COVID-19 measurements at the workplace in various industries and company sizes: A 2-month follow-up cohort study of full-time employees in Japan. Environ. Occup. Health Pract. 2021, 3, 2020-0017. [Google Scholar] [CrossRef]
- Juergensen, J.; Guimón, J.; Narula, R. European SMEs amidst the COVID-19 crisis: Assessing impact and policy responses. J. Ind. Bus. Econ. 2020, 47, 499–510. [Google Scholar] [CrossRef]
- Hair, J.; Alamer, A. Partial Least Squares Structural Equation Modeling (PLS-SEM) in second language and education research: Guidelines using an applied example. Res. Methods Appl. Linguist. 2022, 1, 100027. [Google Scholar] [CrossRef]
- Morales-Vives, F.; Dueñas, J.M.; Ferrando, P.J.; Vigil-Colet, A.; Varea, M.D. COmpliance with pandemic COmmands Scale (COCOS): The relationship between compliance with COVID-19 measures and sociodemographic and attitudinal variables. PLoS ONE 2022, 17, e0262698. [Google Scholar] [CrossRef]
- Kleitman, S.; Fullerton, D.J.; Zhang, L.M.; Blanchard, M.D.; Lee, J.; Stankov, L.; Thompson, V. To comply or not comply? A latent profile analysis of behaviours and attitudes during the COVID-19 pandemic. PLoS ONE 2021, 16, e0255268. [Google Scholar] [CrossRef]
- Shah, S.U.; Loo, E.X.L.; Chua, C.E.; Kew, G.S.; Demutska, A.; Quek, S.; Wong, S.; Lau, H.X.; Low, E.X.S.; Loh, T.L.; et al. Association between well-being and compliance with COVID-19 preventive measures by healthcare professionals: A cross-sectional study. PLoS ONE 2021, 16, e0252835. [Google Scholar] [CrossRef] [PubMed]
- Siegrist, M.; Luchsinger, L.; Bearth, A. The impact of trust and risk perception on the acceptance of measures to reduce COVID-19 cases. Risk Anal. 2021, 41, 787–800. [Google Scholar] [CrossRef] [PubMed]
- Capone, V.; Donizzetti, A.R.; Park, M.S.A. Validation and psychometric evaluation of the COVID-19 risk perception scale (CoRP): A new brief scale to measure individuals’ risk perception. Int. J. Ment. Health Addict. 2021, 21, 1320–1333. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, H.; Önder, A.; Becker, J.; Gröger, M.; Müller, M.M.; Zink, F.; Stein, B.; Radermacher, P.; Waller, C. Markers of oxidative stress during post-COVID-19 fatigue: A hypothesis-generating, exploratory pilot study on hospital employees. Front. Med. 2023, 10, 1305009. [Google Scholar] [CrossRef]
- Manning, K.; Zvolensky, M.J.; Garey, L.; Long, L.J.; Gallagher, M.W. The explanatory role of fatigue severity in the relation between COVID-19 perceived stress and depression, anxiety, and panic severity. Cogn. Behav. Ther. 2022, 51, 89–99. [Google Scholar] [CrossRef]
- Deressa, W.; Worku, A.; Abebe, W.; Gizaw, M.; Amogne, W. Availability and use of personal protective equipment and satisfaction of healthcare professionals during COVID-19 pandemic in Addis Ababa, Ethiopia. Arch. Public Health 2021, 79, 1–14. [Google Scholar] [CrossRef]
- Ahmed, J.; Malik, F.; Bin Arif, T.; Majid, Z.; Chaudhary, M.A.; Ahmad, J.; Malik, M.; Khan, T.M.; Khalid, M. Availability of personal protective equipment (PPE) among US and Pakistani doctors in COVID-19 pandemic. Cureus 2020, 12, e8550. [Google Scholar]
- Vichiensan, V.; Hayashi, Y.; Kamnerdsap, S. COVID-19 countermeasures and passengers’ confidence of urban rail travel in Bangkok. Sustainability 2021, 13, 9377. [Google Scholar] [CrossRef]
- Nguyen-Phuoc, D.Q.; Oviedo-Trespalacios, O.; Nguyen, M.H.; Dinh, M.T.T.; Su, D.N. Intentions to use ride-sourcing services in Vietnam: What happens after three months without COVID-19 infections? Cities 2022, 126, 103691. [Google Scholar] [CrossRef]
- Fielbaum, A.; Ruiz, F.; Boccardo, G.; Rubio, D.; Tirachini, A.; Rosales-Salas, J. The job of public transport, ride-hailing and delivery drivers: Conditions during the COVID-19 pandemic and implications for a post-pandemic future. Travel Behav. Soc. 2023, 31, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.X.; Sun, S.; Jahanshahi, A.A.; Alvarez-Risco, A.; Ibarra, V.G.; Li, J.; Patty-Tito, R.M. Developing and testing a measure of COVID-19 organizational support of healthcare workers–results from Peru, Ecuador, and Bolivia. Psychiatry Res. 2020, 291, 113174. [Google Scholar] [CrossRef]
- Lai, A.Y.K.; Cheung, G.O.C.; Choi, A.C.M.; Wang, M.-P.; Chan, P.S.L.; Lam, A.H.Y.; Lo, E.W.S.; Lin, C.-C.; Lam, T.-H. Mental health, support system, and perceived usefulness of support in university students in Hong Kong amidst COVID-19 pandemic: A mixed-method survey. Int. J. Environ. Res. Public Health 2022, 19, 12931. [Google Scholar] [CrossRef] [PubMed]
- Ecklebe, S.; Löffler, N. A question of quality: Perceptions of internal communication during the Covid-19 pandemic in Germany. J. Commun. Manag. 2021, 25, 214–232. [Google Scholar] [CrossRef]
- Schlögl, M.; Singler, K.; Martinez-Velilla, N.; Jan, S.; Bischoff-Ferrari, H.A.; Roller-Wirnsberger, R.E.; Attier-Zmudka, J.; Jones, C.A.; Miot, S.; Gordon, A.L. Communication during the COVID-19 pandemic: Evaluation study on self-perceived competences and views of health care professionals. Eur. Geriatr. Med. 2021, 12, 1181–1190. [Google Scholar] [CrossRef]
- Fischer, R.; Karl, J.A. Predicting behavioral intentions to prevent or mitigate COVID-19: A cross-cultural meta-analysis of attitudes, norms, and perceived behavioral control effects. Soc. Psychol. Personal. Sci. 2022, 13, 264–276. [Google Scholar] [CrossRef]
- Kement, U.; Çavuşoğlu, S.; Demirağ, B.; Durmaz, Y.; Bükey, A. Effect of perception of COVID-19 and nonpharmaceutical intervention on desire and behavioral intention in touristic travels in Turkey. J. Hosp. Tour. Insights 2022, 5, 230–249. [Google Scholar] [CrossRef]
- Khatoon, S.; Anwar, I.; Shamsi, M.A.; Chaudhary, A. Consumers’ behavioral intention toward online shopping in the post-COVID-19 period. Int. J. Consum. Stud. 2024, 48, e13001. [Google Scholar] [CrossRef]
- Nivette, A.; Ribeaud, D.; Murray, A.; Steinhoff, A.; Bechtiger, L.; Hepp, U.; Shanahan, L.; Eisner, M. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Soc. Sci. Med. 2021, 268, 113370. [Google Scholar] [CrossRef]
- Mueller, R.O.; Hancock, G.R. Structural equation modeling. In The Reviewer’s Guide to Quantitative Methods in the Social Sciences; Routledge: London, UK, 2018; pp. 445–456. [Google Scholar]
- Keith, T.Z. Multiple Regression and Beyond: An Introduction to Multiple Regression and Structural Equation Modeling; Routledge: London, UK, 2018. [Google Scholar]
- Chin, W.; Cheah, J.H.; Liu, Y.; Ting, H.; Lim, X.J.; Cham, T.H. Demystifying the role of causal-predictive modeling using partial least squares structural equation modeling in information systems research. Ind. Manag. Data Syst. 2020, 120, 2161–2209. [Google Scholar] [CrossRef]
- Chan, S.H.; Lay, Y.F. Examining the reliability and validity of research instruments using partial least squares structural equation modeling (PLS-SEM). J. Balt. Sci. Educ. 2018, 17, 239–251. [Google Scholar] [CrossRef]
- Haji-Othman, Y.; Yusuff, M.S.S. Assessing reliability and validity of attitude construct using partial least squares structural equation modeling. Int. J. Acad Res. Bus. Soc. Sci. 2022, 12, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef]
- Gumasing, M.J.J.; Ilo, C.K.K. The impact of job satisfaction on creating a sustainable workplace: An empirical analysis of organizational commitment and lifestyle behavior. Sustainability 2023, 15, 10283. [Google Scholar] [CrossRef]
- Plonsky, L. Statistical power, p values, descriptive statistics, and effect sizes: A “back-to-basics” approach to advancing quantitative methods in L2 research. Adv. Quant. Methods Second. Lang. Res. 2015, 23–45. [Google Scholar] [CrossRef]
- Cayaban CJ, G.; Prasetyo, Y.T.; Persada, S.F.; Borres, R.D.; Gumasing, M.J.J.; Nadlifatin, R. The influence of social media and sustainability advocacy on the purchase intention of Filipino consumers in fast fashion. Sustainability 2023, 15, 8502. [Google Scholar] [CrossRef]
- Gumasing, M.J.J.; Sobrevilla, M.D.M. Determining factors affecting the protective behavior of Filipinos in urban areas for natural calamities using an integration of protection motivation theory, theory of planned behavior, and ergonomic appraisal: A sustainable disaster preparedness approach. Sustainability 2023, 15, 6427. [Google Scholar] [CrossRef]
- Tweneboah-Koduah, E.Y.; Coffie, I.S. Social distancing, hand washing and handshaking behaviour during and beyond coronavirus pandemic: A social marketing perspective. Soc. Mark. Q. 2022, 28, 288–306. [Google Scholar] [CrossRef]
- Nudelman, G. Predicting adherence to COVID-19 behavioural guidelines: A comparison of protection motivation theory and the theory of planned behaviour. Psychol. Health 2024, 39, 1689–1705. [Google Scholar] [CrossRef]
- Foster, M.L. Exploring Health Science Students’ Perception of the Influence of Health Precaution Practices During the COVID-19 Pandemic. Ph.D. Thesis, Liberty University, Lynchburg, VA, USA, 2024. [Google Scholar]
- Green, E.C.; Murphy, E.M.; Gryboski, K. The health belief model. Wiley Encycl. Health Psychol. 2020, 211–214. [Google Scholar] [CrossRef]
- Savadori, L.; Lauriola, M. Risk perception and protective behaviors during the rise of the COVID-19 outbreak in Italy. Front. Psychol. 2021, 11, 577331. [Google Scholar] [CrossRef] [PubMed]
- Cipolletta, S.; Andreghetti GR Mioni, G. Risk perception towards COVID-19: A systematic review and qualitative synthesis. Int. J. Environ. Res. Public Health 2022, 19, 4649. [Google Scholar] [CrossRef] [PubMed]
- Cantor, D.E.; Terle, M. Applying a voluntary compliance model to a proposed transportation safety regulation. Int. J. Phys. Distrib. Logist. Manag. 2010, 40, 822–846. [Google Scholar] [CrossRef]
- Ali, R.F.; Dominic, P.D.D.; Ali, S.E.A.; Rehman, M.; Sohail, A. Information security behavior and information security policy compliance: A systematic literature review for identifying the transformation process from noncompliance to compliance. Appl. Sci. 2021, 11, 3383. [Google Scholar] [CrossRef]
- Nguyen-Phuoc, D.Q.; Mai, N.X.; Kim, I.; Oviedo-Trespalacios, O. Questioning penalties and road safety Policies: Are they enough to deter risky motorcyclist Behavior? Accid. Anal. Prev. 2024, 207, 107756. [Google Scholar] [CrossRef]
- Chun, Y.H.; Rainey, H.G. Goal ambiguity and organizational performance in US federal agencies. J. Public Adm. Res. Theory 2005, 15, 529–557. [Google Scholar] [CrossRef]
- Dawson, W.D.; Boucher, N.A.; Stone, R.; Van Houtven, C.H. COVID-19: The time for collaboration between long-term services and supports, health care systems, and public health is now. Milbank Q. 2021, 99, 565–594. [Google Scholar] [CrossRef] [PubMed]
- Payne, J.; Cluff, L.; Lang, J.; Matson-Koffman, D.; Morgan-Lopez, A. Elements of a workplace culture of health, perceived organizational support for health, and lifestyle risk. Am. J. Health Promot. 2018, 32, 1555–1567. [Google Scholar] [CrossRef]
- Hu, Q.; Dinev, T.; Hart, P.; Cooke, D. Managing employee compliance with information security policies: The critical role of top management and organizational culture. Decis. Sci. 2012, 43, 615–660. [Google Scholar] [CrossRef]
- Irfan, M.; Akhtar, N.; Ahmad, M.; Shahzad, F.; Elavarasan, R.M.; Wu, H.; Yang, C. Assessing public willingness to wear face masks during the COVID-19 pandemic: Fresh insights from the theory of planned behavior. Int. J. Environ. Res. Public Health 2021, 18, 4577. [Google Scholar] [CrossRef] [PubMed]
- Eraso, Y.; Hills, S. Intentional and unintentional non-adherence to social distancing measures during COVID-19: A mixed-methods analysis. PLoS ONE 2021, 16, e0256495. [Google Scholar] [CrossRef] [PubMed]
- Luszczynska, A.; Szczuka, Z.; Abraham, C.; Baban, A.; Brooks, S.; Cipolletta, S.; Danso, E.; Dombrowski, S.U.; Gan, Y.; Gaspar, T.; et al. The interplay between strictness of policies and individuals’ self-regulatory efforts: Associations with handwashing during the COVID-19 pandemic. Ann. Behav. Med. 2022, 56, 368–380. [Google Scholar] [CrossRef]
- Dancer, S.J. Reducing the risk of COVID-19 transmission in hospitals: Focus on additional infection control strategies. Surgery 2021, 39, 752–758. [Google Scholar] [CrossRef]
- Gander, P.; Hartley, L.; Powell, D.; Cabon, P.; Hitchcock, E.; Mills, A.; Popkin, S. Fatigue risk management: Organizational factors at the regulatory and industry/company level. Accid. Anal. Prev. 2011, 43, 573–590. [Google Scholar] [CrossRef] [PubMed]
- Jepsen, J.R.; Zhao, Z.; van Leeuwen, W.M. Seafarer fatigue: A review of risk factors, consequences for seafarers’ health and safety and options for mitigation. Int. Marit. Health 2015, 66, 106–117. [Google Scholar] [CrossRef]
- LeBlanc, V.R. The effects of acute stress on performance: Implications for health professions education. Acad. Med. 2009, 84, S25–S33. [Google Scholar] [CrossRef]
- Bandura, A. Social-learning theory of identificatory processes. Handb. Social. Theory Res. 1969, 213, 262. [Google Scholar]
- Ismail, A.; Foboy, N.A.; Nor, A.M. Effect of managers’ communication on training application with motivation to learn as an intervening variable. South East Asian J. Manag. 2018, 12, 2. [Google Scholar] [CrossRef]
- Awais Bhatti, M.; Ali, S.; Mohd Isa, M.F.; Mohamed Battour, M. Training transfer and transfer motivation: The influence of individual, environmental, situational, training design, and affective reaction factors. Perform. Improv. Q. 2014, 27, 51–82. [Google Scholar] [CrossRef]

| Construct | Item | Measure | Supporting References |
|---|---|---|---|
| Attitude Towards Compliance | AC1 | I believe following COVID-19 safety protocols (e.g., wearing masks) protects me and my passengers. | [59,60,61] |
| AC2 | Sanitizing my vehicle regularly is worth the time and effort. | ||
| AC3 | Adhering to COVID-19 safety measures ensures safer working conditions. | ||
| AC4 | I feel a sense of responsibility to follow health guidelines for the safety of others. | ||
| Risk Perception | RP1 | I am at high risk of contracting COVID-19 due to frequent interactions with passengers. | [62,63] |
| RP2 | Driving during the pandemic exposes me to significant health risks. | ||
| RP3 | COVID-19 poses a serious threat to my overall well-being. | ||
| RP4 | I feel vulnerable to COVID-19 because of my job as a TNVS driver. | ||
| Stress and Fatigue | SF1 | I feel stressed about the possibility of getting infected while working. | [64,65] |
| SF2 | Long working hours reduce my ability to follow safety protocols effectively. | ||
| SF3 | I experience mental exhaustion from balancing passenger interactions and safety measures. | ||
| SF4 | Thinking about the risks of COVID-19 adds to my daily stress levels. | ||
| Availability of PPE | AV1 | I have easy access to personal protective equipment (PPE) like masks and sanitizers. | [66,67] |
| AV2 | My ride-hailing platform provides adequate resources to maintain hygiene. | ||
| AV3 | I never run out of necessary PPE while working. | ||
| AV4 | I can afford to replenish my PPE supplies regularly. | ||
| Passenger Compliance | PC1 | Most of my passengers comply with wearing masks during rides. | [68,69] |
| PC2 | I rarely encounter passengers who refuse to follow COVID-19 protocols. | ||
| PC3 | Passengers respect social distancing guidelines inside my vehicle. | ||
| PC4 | My passengers willingly follow hygiene protocols, such as sanitizing their hands. | ||
| Ride Conditions | RC1 | My vehicle is well-ventilated, minimizing the risk of COVID-19 transmission. | [56,70] |
| RC2 | I frequently clean and sanitize my vehicle to maintain hygiene. | ||
| RC3 | The physical layout of my vehicle supports safe interactions with passengers. | ||
| RC4 | I use dividers or barriers to separate myself from passengers. | ||
| Company Policies | CP1 | My ride-hailing platform enforces strict COVID-19 safety guidelines. | [71,72] |
| CP2 | The company monitors drivers’ compliance with health protocols. | ||
| CP3 | I am aware of the company’s policies regarding COVID-19 safety measures. | ||
| CP4 | The company takes passenger non-compliance seriously and provides support to drivers. | ||
| Support Systems | SS1 | My ride-hailing platform provides free or subsidized PPE for drivers. | [73,74] |
| SS2 | The company offers regular COVID-19 testing for its drivers. | ||
| SS3 | I receive financial support or incentives for following safety protocols. | ||
| SS4 | The company provides resources to address drivers’ health concerns. | ||
| Communication and Training | CT1 | My ride-hailing platform regularly communicates updates about COVID-19 protocols. | [75,76] |
| CT2 | I have received training on how to implement safety measures effectively. | ||
| CT3 | I am informed about the latest COVID-19 guidelines from the company. | ||
| CT4 | The company provides clear instructions on managing non-compliant passengers. | ||
| Behavioral Intention | BI1 | I intend to sanitize my vehicle after every ride. | [77,78,79] |
| BI2 | I plan to ensure passengers follow COVID-19 protocols during rides. | ||
| BI3 | I am committed to wearing a mask while driving. | ||
| BI4 | I will take all necessary precautions to minimize the risk of COVID-19 transmission. | ||
| Compliance Behavior | CB1 | I sanitize my vehicle after every ride. | [61,62,80] |
| CB2 | I always wear a mask while working. | ||
| CB3 | I ensure passengers comply with health protocols, such as wearing masks. | ||
| CB4 | I use dividers or barriers to maintain social distancing in my vehicle. |
| Construct | Item | Mean | S.D. | F.L. (≥0.7) | α (≥0.7) | C.R. (≥0.7) | A.V.E. (≥0.5) |
|---|---|---|---|---|---|---|---|
| Attitude Towards Compliance | AC1 | 3.51 | 1.02 | 0.78 | 0.876 | 0.853 | 0.672 |
| AC2 | 3.40 | 1.09 | 0.71 | ||||
| AC3 | 3.29 | 1.06 | 0.83 | ||||
| AC4 | 3.62 | 0.98 | 0.72 | ||||
| Risk Perception | RP1 | 3.54 | 1.02 | 0.79 | 0.892 | 0.881 | 0.658 |
| RP2 | 3.45 | 1.01 | 0.88 | ||||
| RP3 | 3.47 | 0.96 | 0.73 | ||||
| RP4 | 3.62 | 1.02 | 0.73 | ||||
| Stress and Fatigue | SF1 | 3.54 | 1.07 | 0.74 | 0.923 | 0.890 | 0.781 |
| SF2 | 3.53 | 1.12 | 0.77 | ||||
| SF3 | 3.84 | 1.11 | 0.78 | ||||
| SF4 | 3.58 | 1.03 | 0.77 | ||||
| Availability of PPE | AV1 | 3.49 | 1.01 | 0.80 | 0.821 | 0.804 | 0.762 |
| AV2 | 3.39 | 0.94 | 0.88 | ||||
| AV3 | 3.46 | 0.96 | 0.78 | ||||
| AV4 | 3.42 | 1.08 | 0.82 | ||||
| Passenger Compliance | PC1 | 3.56 | 1.03 | 0.88 | 0.890 | 0.870 | 0.769 |
| PC2 | 4.01 | 1.22 | 0.78 | ||||
| PC3 | 3.60 | 1.03 | 0.76 | ||||
| PC4 | 3.63 | 1.04 | 0.70 | ||||
| Ride Conditions | RC1 | 3.62 | 1.09 | 0.71 | 0.925 | 0.891 | 0.792 |
| RC2 | 3.65 | 1.05 | 0.78 | ||||
| RC3 | 3.57 | 1.06 | 0.70 | ||||
| RC4 | 3.51 | 1.03 | 0.70 | ||||
| Company Policies | CP1 | 3.43 | 1.07 | 0.90 | 0.890 | 0.850 | 0.791 |
| CP2 | 3.21 | 1.07 | 0.71 | ||||
| CP3 | 3.60 | 0.99 | 0.76 | ||||
| CP4 | 3.56 | 1.03 | 0.78 | ||||
| Support Systems | SS1 | 3.45 | 1.02 | 0.81 | 0.924 | 0.911 | 0.781 |
| SS2 | 3.48 | 0.98 | 0.80 | ||||
| SS3 | 3.68 | 1.04 | 0.76 | ||||
| SS4 | 3.54 | 1.09 | 0.72 | ||||
| Communication and Training | CT1 | 3.56 | 1.11 | 0.73 | 0.858 | 0.842 | 0.722 |
| CT2 | 3.85 | 1.11 | 0.77 | ||||
| CT3 | 3.57 | 1.02 | 0.83 | ||||
| CT4 | 3.47 | 1.00 | 0.85 | ||||
| Behavioral Intention | BI1 | 3.51 | 1.03 | 0.73 | 0.871 | 0.859 | 0.676 |
| BI2 | 3.41 | 1.07 | 0.77 | ||||
| BI3 | 3.24 | 1.07 | 0.73 | ||||
| BI4 | 3.69 | 0.99 | 0.84 | ||||
| Compliance Behavior | CB1 | 3.51 | 1.03 | 0.91 | 0.892 | 0.889 | 0.652 |
| CB2 | 3.40 | 1.02 | 0.88 | ||||
| CB3 | 3.49 | 0.98 | 0.89 | ||||
| CB4 | 3.66 | 1.04 | 0.90 |
| AC | AV | B1 | CB | CP | CT | PC | RC | RP | SF | SS | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| AC | 0.897 | ||||||||||
| AV | 0.587 | 0.768 | |||||||||
| BI | 0.600 | 0.710 | 0.751 | ||||||||
| CB | 0.663 | 0.623 | 0.654 | 0.825 | |||||||
| CP | 0.437 | 0.531 | 0.565 | 0.653 | 0.708 | ||||||
| CT | 0.667 | 0.656 | 0.640 | 0.673 | 0.497 | 0.727 | |||||
| PC | 0.448 | 0.611 | 0.527 | 0.446 | 0.329 | 0.585 | 0.752 | ||||
| RC | 0.716 | 0.720 | 0.608 | 0.698 | 0.526 | 0.676 | 0.575 | 0.853 | |||
| RP | 0.487 | 0.690 | 0.681 | 0.675 | 0.600 | 0.657 | 0.473 | 0.600 | 0.817 | ||
| SF | 0.350 | 0.761 | 0.561 | 0.671 | 0.450 | 0.711 | 0.651 | 0.661 | 0.771 | 0.881 | |
| SS | 0.671 | 0.451 | 0.661 | 0.541 | 0.659 | 0.606 | 0.671 | 0.561 | 0.712 | 0.701 | 0.761 |
| AC | AV | B1 | CB | CP | CT | PC | RC | RP | SF | SS | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| AC | |||||||||||
| AV | 0.623 | ||||||||||
| BI | 0.648 | 0.771 | |||||||||
| CB | 0.723 | 0.679 | 0.726 | ||||||||
| CP | 0.496 | 0.591 | 0.652 | 0.762 | |||||||
| CT | 0.733 | 0.723 | 0.720 | 0.759 | 0.579 | ||||||
| PC | 0.426 | 0.752 | 0.558 | 0.446 | 0.347 | 0.663 | |||||
| RC | 0.770 | 0.769 | 0.661 | 0.758 | 0.595 | 0.747 | 0.588 | ||||
| RP | 0.551 | 0.792 | 0.791 | 0.789 | 0.738 | 0.676 | 0.533 | 0.690 | |||
| SF | 0.231 | 0.342 | 0.459 | 0.698 | 0.761 | 0.651 | 0.761 | 0.661 | 0.541 | ||
| SS | 0.623 | 0.561 | 0.716 | 0.459 | 0.566 | 0.551 | 0.671 | 0.653 | 0.551 | 0.655 |
| No | Relationship | Beta Coefficient | p-Value | Result | Significance | Hypothesis | Effect Size (f2) |
|---|---|---|---|---|---|---|---|
| 1 | AC→BI | 0.453 | <0.001 | Positive | Significant | Do not reject | 0.268 |
| 2 | RP→BI | 0.289 | 0.001 | Positive | Significant | Do not reject | 0.153 |
| 3 | SF→BI | 0.131 | 0.211 | Positive | Not Significant | Reject | 0.012 |
| 4 | AV→BI | 0.341 | <0.001 | Positive | Significant | Do not reject | 0.204 |
| 5 | PC→BI | 0.293 | 0.002 | Positive | Significant | Do not reject | 0.167 |
| 6 | RC→BI | 0.198 | 0.241 | Positive | Not Significant | Reject | 0.031 |
| 7 | CP→BI | 0.336 | 0.001 | Positive | Significant | Do not reject | 0.178 |
| 8 | SS→BI | 0.433 | <0.001 | Positive | Significant | Do not reject | 0.242 |
| 9 | CT→BI | 0.211 | 0.058 | Positive | Not Significant | Reject | 0.045 |
| 10 | BI→CB | 0.643 | <0.001 | Positive | Significant | Do not reject | 0.413 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gumasing, M.J.J. Determinants of Behavioral Intention and Compliance Behavior Among Transportation Network Vehicle Service Drivers During the COVID-19 Pandemic. COVID 2025, 5, 38. https://doi.org/10.3390/covid5030038
Gumasing MJJ. Determinants of Behavioral Intention and Compliance Behavior Among Transportation Network Vehicle Service Drivers During the COVID-19 Pandemic. COVID. 2025; 5(3):38. https://doi.org/10.3390/covid5030038
Chicago/Turabian StyleGumasing, Ma. Janice J. 2025. "Determinants of Behavioral Intention and Compliance Behavior Among Transportation Network Vehicle Service Drivers During the COVID-19 Pandemic" COVID 5, no. 3: 38. https://doi.org/10.3390/covid5030038
APA StyleGumasing, M. J. J. (2025). Determinants of Behavioral Intention and Compliance Behavior Among Transportation Network Vehicle Service Drivers During the COVID-19 Pandemic. COVID, 5(3), 38. https://doi.org/10.3390/covid5030038






