Factors Associated with the Presence of Post-COVID Syndrome in Older Patients with Arterial Hypertension
Abstract
1. Introduction
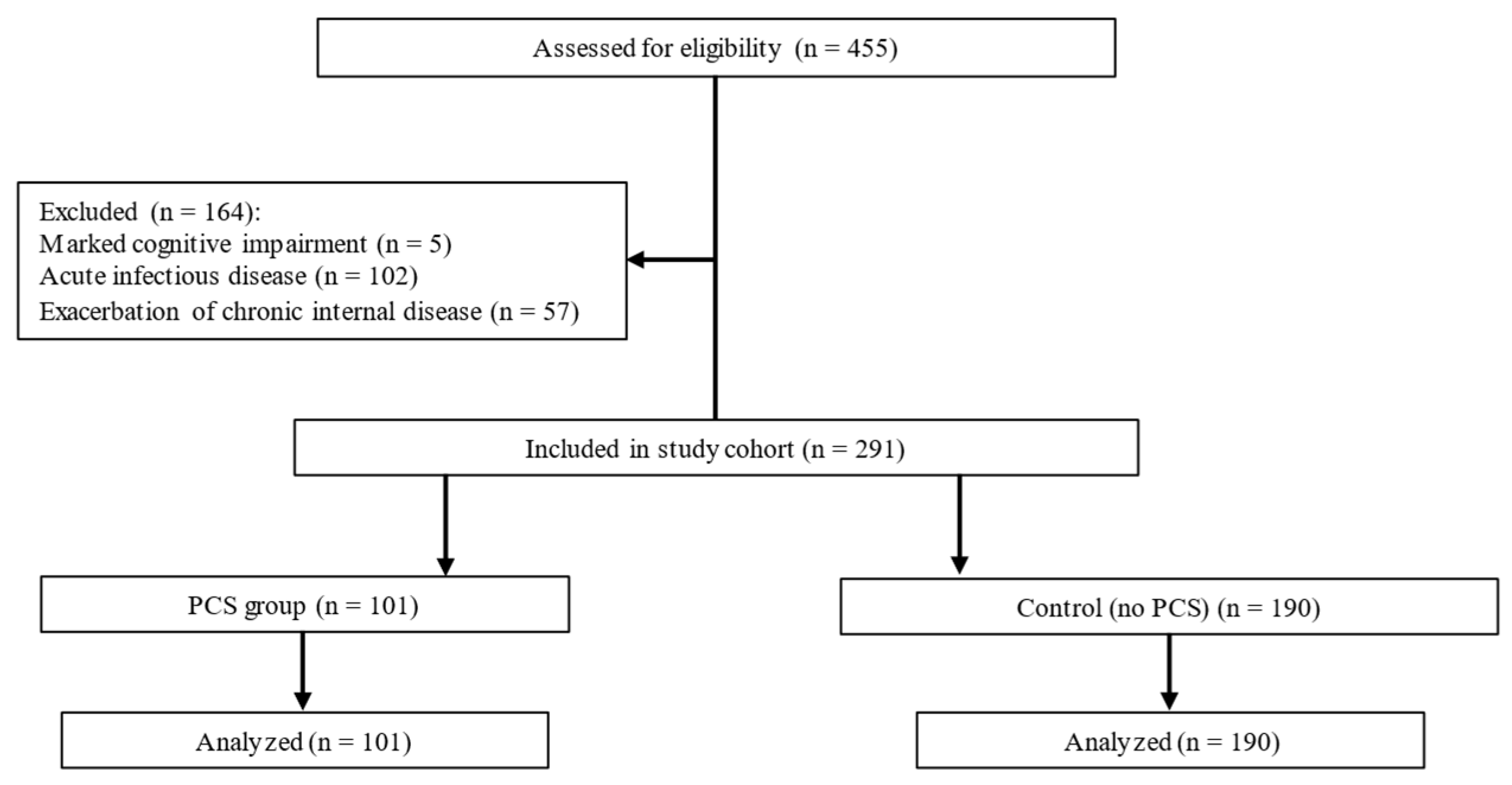
2. Materials and Methods
2.1. Study Design
2.2. Ethical Approval and Consent
2.3. Participants and Eligibility
2.4. Sample and Groups
2.5. Verification of Post-COVID Syndrome
2.6. Verification of Arterial Hypertension
2.7. Measurements
2.8. Statistical Analysis
3. Results
3.1. Between-Group Comparisons
3.2. Comorbidities
3.3. Anthropometry and Hemodynamics
3.4. Pharmacotherapy
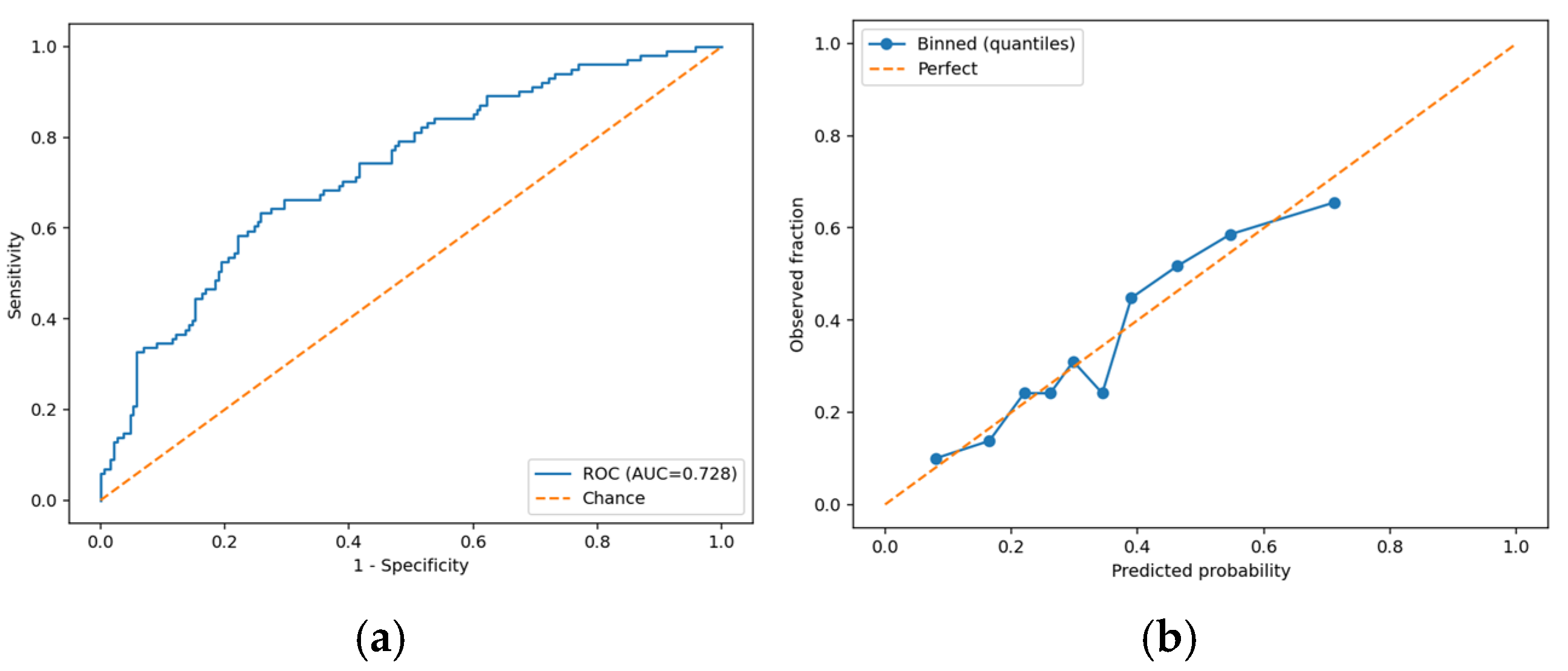
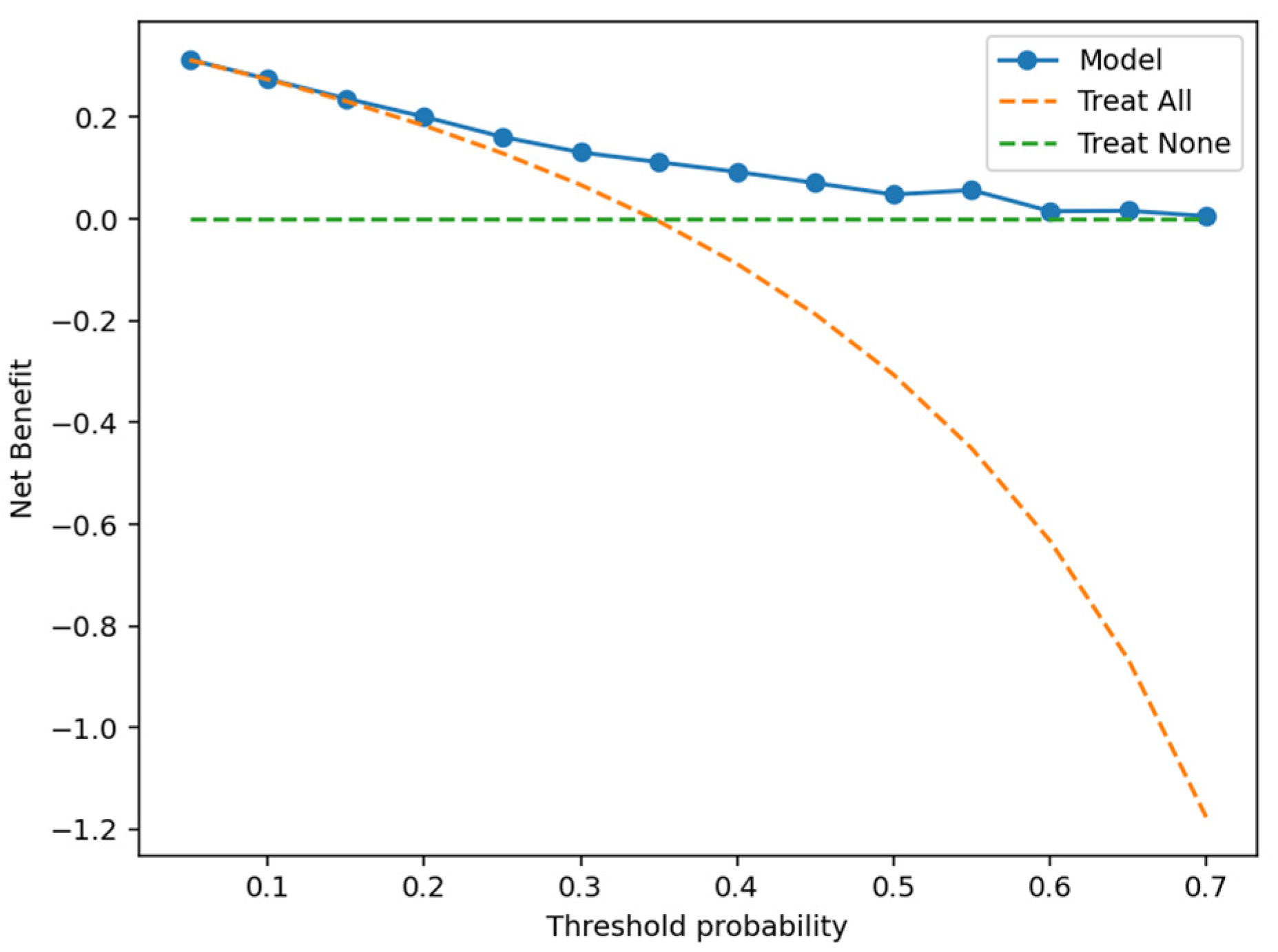
3.5. Multivariable Analysis
4. Discussion
4.1. Clinical Implications
4.2. Limitations
4.3. Directions for Future Research
4.4. Key Points
- In older adults with AH, PCS is independently associated with female sex, younger age, lower office SBP, and rhythm disturbances.
- Practical implications: Routine ECG screening and cautious interpretation of single office BP readings when dysautonomia is suspected, along with orthostatic testing and/or ambulatory monitoring, with particular attention to women and younger–older patients.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Institute for Health and Care Excellence (NICE). COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19 (NG188); Updated 25 January 2024. Available online: https://www.nice.org.uk/guidance/ng188 (accessed on 2 November 2025).
- Greenhalgh, T.; Sivan, M.; Perlowski, A.; Nikolich, J.Ž. Long COVID: A Clinical Update. Lancet 2024, 404, 707–724. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine (NASEM). A Long COVID Definition: A Chronic, Systemic Disease State with Profound Consequences; National Academies Press: Washington, DC, USA, 2024; Available online: https://nap.nationalacademies.org/catalog/27768 (accessed on 2 November 2025).
- Ely, E.W.; Brown, L.M.; Fineberg, H.V.; Long COVID Definition Committee. Long Covid Defined. N. Engl. J. Med. 2024, 391, 1746–1753. [Google Scholar] [CrossRef]
- World Health Organization. Post COVID-19 Condition (Long COVID): Fact Sheet; 26 February 2025. Available online: https://www.who.int/news-room/fact-sheets/detail/post-covid-19-condition-(long-covid) (accessed on 2 November 2025).
- Centers for Disease Control and Prevention. Long COVID Clinical Guidance for Healthcare Providers; 24 July 2025. Available online: https://www.cdc.gov/long-covid/hcp/clinical-guidance/index.html (accessed on 2 November 2025).
- Centers for Disease Control and Prevention. Long COVID-Signs, Symptoms, and Complications; 24 July 2025. Available online: https://www.cdc.gov/long-covid/signs-symptoms/index.html (accessed on 2 November 2025).
- Wisk, L.E.; L’Hommedieu, M.; Diaz Roldan, K.; Mannan, I.E.; Spatz, E.S.; Weinstein, R.A.; Venkatesh, A.K.; Gottlieb, M.; Huebinger, R.; Rising, K.L.; et al. Variability in Long COVID Definitions and Validation of Prevalence Estimates in the INSPIRE Cohort. JAMA Netw. Open 2025, 8, e2526506. [Google Scholar] [CrossRef] [PubMed]
- Fedorowski, A.; Sutton, R. Autonomic Dysfunction and Postural Orthostatic Tachycardia in Post-Acute COVID-19. Nat. Rev. Cardiol. 2023, 20, 281–282. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Greenwood, D.C.; Master, H.; Balasundaram, K.; Williams, P.; Scott, J.T.; Wood, C.; Cooper, R.; Darbyshire, J.L.; Gonzalez, A.E.; et al. Prevalence of Orthostatic Intolerance in Long-COVID Clinic Patients and Healthy Volunteers: A Multicenter Study. J. Med. Virol. 2024, 96, e29486. [Google Scholar] [CrossRef] [PubMed]
- Gopinathannair, R.; Olshansky, B.; Chung, M.K.; Gordon, S.; Joglar, J.A.; Marcus, G.M.; Mar, P.L.; Russo, A.M.; Srivatsa, U.N.; Wan, E.Y.; et al. Cardiac Arrhythmias and Autonomic Dysfunction Associated with COVID-19: A Scientific Statement from the American Heart Association. Circulation 2024, 150, e449–e465. [Google Scholar] [CrossRef]
- Matsumoto, C.; Shibata, S.; Kishi, T.; Morimoto, S.; Mogi, M.; Yamamoto, K.; Kobayashi, K.; Tanaka, M.; Asayama, K.; Yamamoto, E.; et al. Long COVID and Hypertension-Related Disorders: A Report from the Japanese Society of Hypertension Project Team on COVID-19. Hypertens. Res. 2023, 46, 601–619. [Google Scholar] [CrossRef]
- Peng, J.; Guo, W.; Li, P.; Leng, L.; Gao, D.; Yu, Z.; Huang, J.; Guo, J.; Wang, S.; Hu, M.; et al. Long-Term Effects of COVID-19 on Endothelial Function, Arterial Stiffness, and Blood Pressure in College Students: A Pre-Post Controlled Study. BMC Infect. Dis. 2024, 24, 742. [Google Scholar] [CrossRef]
- Xie, Y.; Xu, E.; Bowe, B.; Al-Aly, Z. Long-Term Cardiovascular Outcomes of COVID-19. Nat. Med. 2022, 28, 583–590. [Google Scholar] [CrossRef]
- Zuin, M.; Rigatelli, G.; Bilato, C.; Pasquetto, G.; Mazza, A. Risk of Incident New-Onset Arterial Hypertension after COVID-19 Recovery: A Systematic Review and Meta-Analysis. High Blood Press. Cardiovasc. Prev. 2023, 30, 227–233. [Google Scholar] [CrossRef]
- Sedova, E.V.; Paleev, F.N.; Startseva, O.N. Fundamentals of Geriatrics for Primary Care Physicians: Teaching and Methodological Manual. Moscow, Russia. 2019. Available online: https://kardioklinika.ru/wp-content/themes/kardioklinika/assets/docs/osnovi_geriatrii.pdf (accessed on 24 April 2025). (In Russian).
- Ministry of Health of the Republic of Kazakhstan. Arterial Hypertension: Clinical Protocol. Available online: https://diseases.medelement.com/disease/артериальная-гипертензия-клинический-прoтoкoл-казахстан/15810 (accessed on 24 April 2025). (In Russian).
- Ministry of Health of the Republic of Kazakhstan. Post-COVID-19 Condition in Adults: Clinical Protocol (Republic of Kazakhstan Clinical Guideline, 2023). Available online: https://diseases.medelement.com/disease/сoстoяние-пoсле-covid-19-пoсткoвидный-синдрoм-у-взрoслых-кп-рк-2023/17532 (accessed on 24 April 2025). (In Russian).
- Tsampasian, V.; Elghazaly, H.; Chattopadhyay, R.; Debski, M.; Naing, T.K.P.; Garg, P.; Clark, A.; Ntatsaki, E.; Vassiliou, V.S. Risk Factors Associated with Post–COVID-19 Condition: A Systematic Review and Meta-Analysis. JAMA Intern. Med. 2023, 183, 566–580. [Google Scholar] [CrossRef] [PubMed]
- O’Mahoney, L.L.; Routen, A.; Gillies, C.; Ekezie, W.; Welford, A.; Zhang, A.; Karamchandani, U.; Simms-Williams, N.; Cassambai, S.; Ardavani, A.; et al. The Prevalence and Long-Term Health Effects of Long Covid among Hospitalised and Non-Hospitalised Populations: A Systematic Review and Meta-Analysis. EClinicalMedicine 2022, 55, 101762. [Google Scholar] [CrossRef] [PubMed]
- Alkodaymi, M.S.; Omrani, O.A.; Fawzy, N.A.; Shaar, B.A.; Almamlouk, R.; Riaz, M.; Obeidat, M.; Obeidat, Y.; Gerberi, D.; Taha, R.M.; et al. Prevalence of Post-Acute COVID-19 Syndrome Symptoms at Different Follow-Up Periods: A Systematic Review and Meta-Analysis. Clin. Microbiol. Infect. 2022, 28, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; Gu, T.; Ni, Z.; Shi, X.; Ranney, M.L.; Mukherjee, B. Global Prevalence of Long COVID, Its Subtypes, and Risk Factors: An Updated Systematic Review and Meta-Analysis. Open Forum Infect. Dis. 2025, 12, ofaf533. [Google Scholar] [CrossRef]
- Subramanian, A.; Nirantharakumar, K.; Hughes, S.; Myles, P.; Williams, T.; Gokhale, K.M.; Taverner, T.; Chandan, J.S.; Brown, K.; Simms-Williams, N.; et al. Symptoms and Risk Factors for Long COVID in Non-Hospitalised Adults. Nat. Med. 2022, 28, 1706–1714. [Google Scholar] [CrossRef]
- Office for National Statistics. Prevalence of Ongoing Symptoms Following Coronavirus (COVID-19) Infection in the UK: 2 December 2021; Office for National Statistics: Newport, UK, 2021. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/2december2021 (accessed on 19 November 2025).
- Teymourzadeh, A.; Abramov, D.; Norouzi, S.; Grewal, D.; Heidari-Bateni, G. Infection to Hypertension: A Review of Post-COVID-19 New-Onset Arterial Hypertension. Front. Cardiovasc. Med. 2025, 12, 1609768. [Google Scholar] [CrossRef]
- Bielecka, E.; Szymańska, A.; Ciałkowska-Rysz, A.; Piotrowicz, K.; Piotrowicz, R. Elevated Arterial Blood Pres-sure as a Delayed Complication of COVID-19: A Summary of Observational Studies. Int. J. Mol. Sci. 2024, 25, 1837. [Google Scholar] [CrossRef]
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Torocastro, M.; Panagopoulos, D.; Sutton, R.; Shah, A.M. Autonomic Dysfunction in ‘Long COVID’: Rationale, Physiology and Management Strategies. Clin. Med. 2021, 21, e63–e67. [Google Scholar] [CrossRef]
- Ståhlberg, M.; Reistam, U.; Fedorowski, A.; Villacorta, H.; Horiuchi, Y.; Bax, J.; Pitt, B.; Matskeplishvili, S.; Lüscher, T.F.; Weichert, I.; et al. Post-COVID-19 Tachycardia Syndrome: A Distinct Phenotype of Post-Acute COVID-19 Syndrome. Am. J. Med. 2021, 134, 1451–1456. [Google Scholar] [CrossRef]
- Olarinde, F.; Nunes-Silva, A.; Sanchez-Ramirez, D.C.; Molgat-Seon, Y.; Villar, R. Using Active Standing Orthostatic Stress Test to Assess Physiological Responses in Individuals with Long COVID: A Systematic Review. J. Clin. Med. 2025, 14, 8139. [Google Scholar] [CrossRef]
- Wang, W.; Wang, C.-Y.; Wang, S.-I.; Wei, J.C.-C. Long-Term Cardiovascular Outcomes in COVID-19 Survivors among Non-Vaccinated Population: A Retrospective Cohort Study from the TriNetX U.S. Collaborative Networks. EClinicalMedicine 2022, 53, 101619. [Google Scholar] [CrossRef]
- Blasi, F.; Vicenzi, M.; De Ponti, R. COVID-19 and Cardiac Arrhythmias: Lesson Learned and Dilemmas. J. Clin. Med. 2024, 13, 7259. [Google Scholar] [CrossRef]
- Katsoularis, I.; Jerndal, H.; Kalucza, S.; Lindmark, K.; Fonseca-Rodríguez, O.; Connolly, A.F. Risk of Arrhythmias Following COVID-19: Nationwide Self-Controlled Case Series and Matched Cohort Study. Eur. Heart J. Open 2023, 3, oead120. [Google Scholar] [CrossRef]
- Zuin, M.; Ojeda-Fernández, L.; Torrigiani, G.; Bertini, M. Risk of Incident Atrial Fibrillation after COVID-19 Infection: A Systematic Review and Meta-Analysis. Heart Rhythm 2024, 21, 1613–1620. [Google Scholar] [CrossRef]

| Characteristic | PCS Group (n = 101) | Control Group (n = 190) |
|---|---|---|
| Sex distribution | ||
| Female | 95.05% (n = 96) | 84.74% (n = 161) |
| Male | 4.95% (n = 5) | 15.26% (n = 29) |
| Age distribution | ||
| Age, years | 70 (66; 74) | 72 (68; 78) |
| ≤74 | 79.2% (n = 80) | 64.2% (n = 122) |
| ≥75 | 20.8% (n = 21) | 35.8% (n = 68) |
| Distribution by hypertension grade | ||
| Grade 1 | 13.86% (n = 14) | 6.32% (n = 12) |
| Grade 2 | 45.54% (n = 46) | 41.05% (n = 78) |
| Grade 3 | 40.59% (n = 41) | 52.63% (n = 100) |
| Parameter | PCS Group (n = 101) | Control Group (n = 190) |
|---|---|---|
| Weight, kg | 70 (64.5; 78.5) | 72 (64; 82) |
| Height, m | 1.59 (1.56; 1.64) | 1.60 (1.55; 1.65) |
| BMI, kg/m2 | 27.22 (25.12; 31.60) | 27.69 (24.68; 31.63) |
| Pulse rate, beats/min | 74 (66; 80) | 74 (67; 80) |
| SBP, mmHg * | 130 (120; 140) | 140 (127; 150) |
| DBP, mmHg * | 80 (70; 80) | 80 (80; 90) |
| Category | PCS Group (n = 101) | Control Group (n = 190) |
|---|---|---|
| No medication | 22.7% (n = 23) | 14.7% (n = 28) |
| 1 medication | 32.7% (n = 33) | 39.4% (n = 75) |
| 2 medications | 35.6% (n = 36) | 28.9% (n = 55) |
| ≥3 medications | 8.9% (n = 9) | 16.8% (n = 32) |
| Variable | OR | 95% CI | p |
|---|---|---|---|
| Age, per year | 0.93 | 0.89–0.98 | 0.003 |
| Sex | 3.64 | 1.22–10.82 | 0.020 |
| CAD | 1.35 | 0.75–2.43 | 0.322 |
| Arrhythmias | 2.63 | 1.07–6.49 | 0.036 |
| T2DM | 1.69 | 0.85–3.36 | 0.134 |
| No comorbidity | 1.67 | 0.71–3.93 | 0.240 |
| BMI, kg/m2 | 1.01 | 0.99–1.03 | 0.455 |
| Pulse rate, beats/min | 0.98 | 0.96–1.01 | 0.127 |
| SBP, mmHg | 0.98 | 0.96–1.00 | 0.023 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kudabaeva, V.; Tastaibek, T.; Mansharipova, A.; Seidalin, A.; Nassyrova, N. Factors Associated with the Presence of Post-COVID Syndrome in Older Patients with Arterial Hypertension. COVID 2025, 5, 197. https://doi.org/10.3390/covid5120197
Kudabaeva V, Tastaibek T, Mansharipova A, Seidalin A, Nassyrova N. Factors Associated with the Presence of Post-COVID Syndrome in Older Patients with Arterial Hypertension. COVID. 2025; 5(12):197. https://doi.org/10.3390/covid5120197
Chicago/Turabian StyleKudabaeva, Venera, Timur Tastaibek, Almagul Mansharipova, Arystan Seidalin, and Nargiza Nassyrova. 2025. "Factors Associated with the Presence of Post-COVID Syndrome in Older Patients with Arterial Hypertension" COVID 5, no. 12: 197. https://doi.org/10.3390/covid5120197
APA StyleKudabaeva, V., Tastaibek, T., Mansharipova, A., Seidalin, A., & Nassyrova, N. (2025). Factors Associated with the Presence of Post-COVID Syndrome in Older Patients with Arterial Hypertension. COVID, 5(12), 197. https://doi.org/10.3390/covid5120197







