1. Introduction
During the protracted evolution of the COVID-19 pandemic, a range of ophthalmic manifestations has been reported in the literature, including conjunctivitis and, less commonly, posterior segment manifestations including uveitis and retinal disease [
1,
2]. Retinal microvascular disease—retinal hemorrhage, cotton wool spots, and retinal artery and vein occlusions—may be due to a constellation of inflammatory, vascular, and coagulation abnormalities [
3]. Herein, we report two patients who presented with ocular ischemic events with severe vision loss in the setting of acute hypoxic respiratory failure (AHRF) and critical illness due to COVID-19.
2. Case Reports
2.1. Case 1
A 44-year-old woman with a history of poorly controlled type 2 diabetes mellitus and non-proliferative diabetic retinopathy presented with progressively worsening cough, dyspnea, and chest pain of 3 days duration. She was febrile with a temperature of 102.8 °F and tachycardic. The patient was admitted for AHRF and sepsis in the setting of multifocal pneumonia and tested positive for COVID-19 by reverse transcription polymerase chain reaction (RT-PCR) on a nasopharyngeal swab.
Given the patient’s respiratory status, mechanical ventilation was initiated, but she failed extubation after 16 days on the ventilator, which prompted tracheostomy placement. After decannulation of the tracheostomy and weaning off sedation, the patient complained of a visual deficit in her left eye (OS) and an ophthalmology consult was requested.
The patient’s pertinent labs during her ICU admission (peak values) included C-reactive protein 27.34 mg/dL (normal < 1.00 mg/dL), D-dimer 13.3 ug/mL (normal 0.22–0.49 ug/mL), platelet count 520 × 103 cells/L (normal 150–450 × 103 cells/L), and white blood cell (WBC) count 19.4 × 103 cells/L (normal 4.5–11 × 103 cells/L). The patient’s nadir hematocrit was 20.5% (normal 15–45%). The patient’s HgBA1c one month prior to admission was 6.9%.
The patient’s uncorrected visual acuity was an ability to count fingers at two feet in the right eye (OD) and light perception (LP) in the left (OS). Pupillary exam showed sluggish reactivity to light in both eyes with an afferent pupillary defect OS. Intraocular pressures were 14 mmHg OD and 12 mmHg OS. The anterior segment was normal on slit lamp examination OU and fundus examination OD showed exudates in the temporal macula and few, scattered intraretinal hemorrhages. Dilated funduscopic exam OS showed optic disc pallor, mild macular exudates, and sclerosis of the proximal vessels. There were dot blot hemorrhages involving the macula and throughout the retinal periphery (
Figure 1).
A fluorescein angiograph (FA) obtained after the patient was discharged showed punctate microaneurysms throughout the periphery with late leakage OD. FA OS showed mild–late leakage of vessels in the periphery with late leakage at the optic nerve and punctate hyperfluorescence from microaneurysms throughout the periphery.
Optical coherence tomography (OCT) in the right eye showed hyper-reflective deposits consistent with exudate temporal to the fovea with retinal thinning of the inner retina temporal to the fovea. OCT OS showed a thin inner retina with outer segment attenuation with no macular edema.
An MRI of the brain without contrast, obtained to evaluate for cortical etiologies of vision loss, and MR angiography were unremarkable (
Figure 1).
The patient’s presentation was suggestive of bilateral ocular ischemic event, likely secondary to ophthalmic artery occlusion during the patient’s acute hospitalization for COVID-19. She was observed to monitor for retinal neovascularization, but her visual acuity and examination remained unchanged at final 6-month follow-up and a low vision evaluation was subsequently recommended.
2.2. Case 2
This patient was a 69-year-old woman with a history of hypertension, type 2 diabetes, and breast cancer status post-resection who was admitted for AHRF secondary to COVID-19-induced pneumonia. While in the ICU, the patient required prolonged intubation and mechanical ventilation, as well as proning. A tracheostomy was also performed on her and subsequently decannulated after 32 days. The patient also experienced delirium during her treatment in the ICU. Upon weaning off sedation and improvement in her mental status, the patient reported bilateral deceased vision. However, because of her history of ICU delirium, the precise time course of the onset of visual changes are unknown.
While in the ICU, the patient’s pertinent labs (peak value) included C-reactive protein 229.5 mg/L (normal ≤ 10 mg/L), fibrinogen 965 mg/L (normal 200 to 393 mg/dL), interleukin-6 level of 5.3 pg/mL (normal ≤ 2 pg/mL), WBC 21.1 × 103 cells/L (normal 4.0–10.0 × 103 cells/L), and platelets 438 × 103 cells/L (normal 150–450 × 103 cells/L). The patient’s nadir hematocrit level was 20.7% (normal 33.3–41.4%).
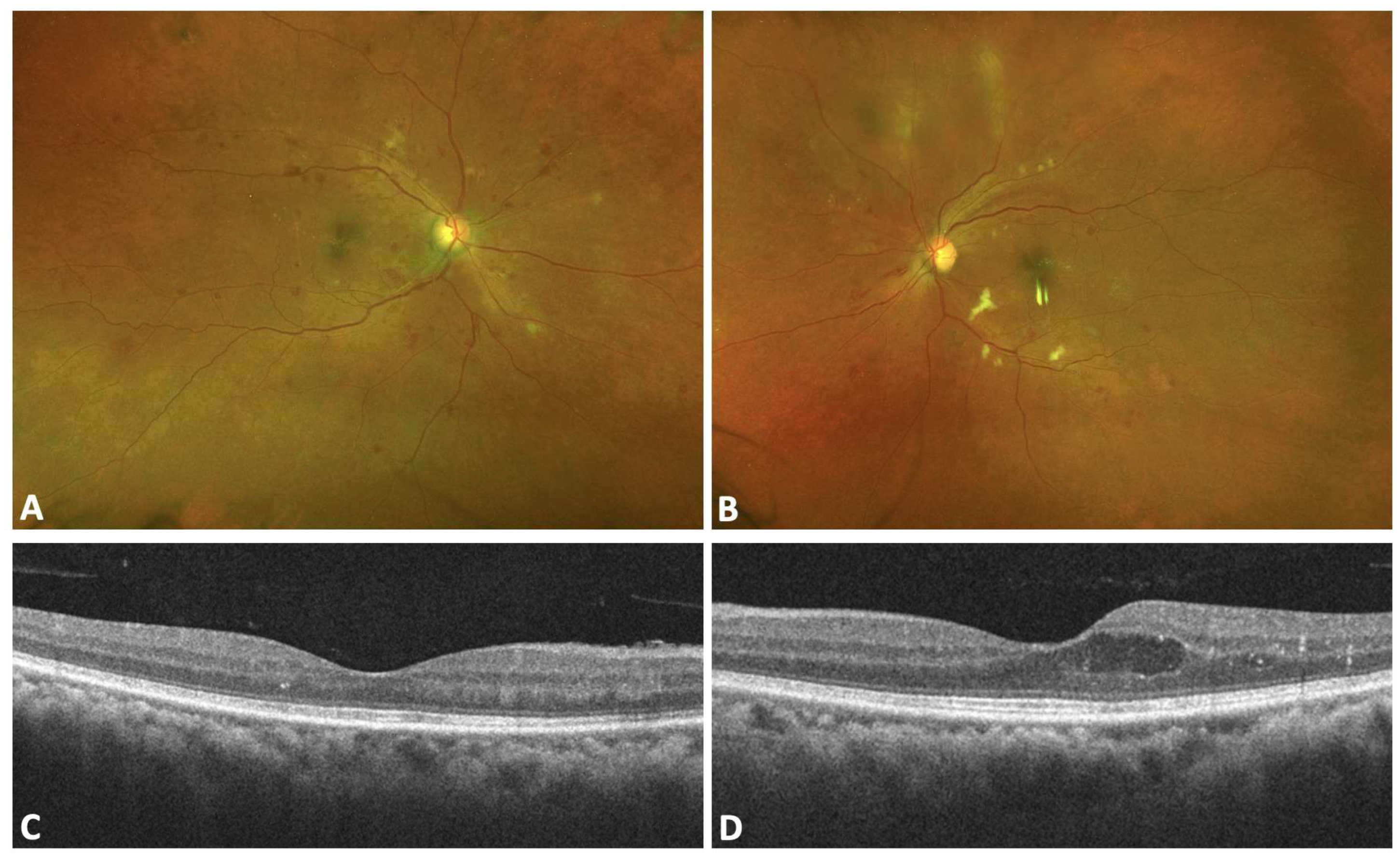
Ophthalmic examination showed a corrected visual acuity of 20/300 OD and 20/200 OS. Dilated fundoscopy showed bilateral retinal hemorrhage, cotton wool spots predominantly in the peripapillary distribution, bilateral macular edema OS greater than OD, and retinal vascular tortuosity in both eyes (
Figure 2).
A fluorescein angiogram was attempted but unsuccessful due to poor venous access. The patient was diagnosed with bilateral central retinal vein occlusion and macular edema of the left eye. Expectant management was recommended at the time with consideration of anti-VEGF injections if the macular edema failed to resolve.
Follow-up evaluation 2 weeks after initial presentation showed visual acuity still decreased at 20/80 OD and 20/300 OS. Dilated fundoscopy and OCT findings also remained unchanged. On final follow-up evaluation 8 weeks after initial presentation without intravitreal anti-VEGF, visual acuity was improved at 20/20 OD and 20/20-2 OS. Dilated fundoscopy showed signs of improved hemorrhages and few cotton-wool spots, and OCT showed mild persistent macular edema OS (
Figure 3).
3. Discussion
Several prior case reports and series have described central retinal venous occlusion and arterial occlusion temporally associated with COVID-19. We report two cases of severe vision loss secondary to acute vascular occlusion during AHRF due to COVID-19. The first patient presented with profound vision loss suggestive of bilateral ocular ischemia while the second patient showed CRVO, which improved with observation. Interestingly, in the second patient, her visual acuity improved without anti-vascular endothelial growth factor injection, which was discussed at her initial visit.
Both patients required hospitalization, invasive mechanical ventilation, and intensive care unit interventions. Their courses of treatment were complicated by prolonged ventilation, with one of the patients requiring proning. Additionally, blood work indices showed severe abnormal coagulation and inflammatory parameters including extreme elevation in D-dimers. In patient 1, the visual acuity remained poor at ensuing follow-up while in patient 2, a nearly complete recovery was experienced. While the precise SARS-CoV-2 variant leading to COVID-19 in the two patients is unknown, episodic increases in COVID-19 due to newer variants, some of which may demonstrate a higher prevalence of ocular findings, warrants further understanding and characterization of both the acute and post-acute SARS-CoV-2 findings.
The mechanisms of microvascular occlusion associated with COVID-19 likely involve a combination of inflammatory, thrombotic, and vascular endothelial dysfunction. Coagulopathy has been reported in 50% of patients infected with the severe form of COVID-19 infection, with D-dimer noted to increase significantly among these patients [
4]. Whether coagulopathies played a role in mediating the events in our patients is unknown and patient 2 also showed highly elevated fibrinogen, indicative of coagulation diathesis. Additionally, since hypertension can be associated with ocular vascular occlusive events, it is noteworthy that the patient in Case 1 presented with a lower blood pressure of 109/58 when consulted by ophthalmology for changes in vision. Her blood pressure further decreased to 88/50 as she became septic in the following days. Despite her previous blood pressures during hospitalization ranging from the 130s to the mid-140s, the timing of the vascular event during a period of low blood pressure makes hypertension a less likely cause. Moreover, we acknowledge that COVID-19 cannot be definitively confirmed as the cause of vascular occlusion, given the broad differential that exists for such an oscular ischemic event. However, we believe it was a significant contributing factor given the patient’s vasculopathic factors including diabetes and hypertension, in addition to the higher risk of an occlusive event in the setting of the inflammation and coagulopathy of severe COVID-19.
The onset of retinal vascular complications related to COVID-19 appears to vary in timing and presentation, as indicated by various case-control studies and individual case reports [
5,
6]. While some studies reported no retinal vascular changes upon fundus examination, others have highlighted significant findings such as retinal hemorrhages, cotton wool spots (CWS), dilated veins, and reduced vessel density (VD) on optical coherence tomography angiography (OCTA) in COVID-19 patients compared to controls [
3,
7]. In one study of retinal and optic nerve complications in young individuals, the mean time between infection and diagnosis of a retinal vascular or optic nerve condition was 3.5 ± 1.2 months and presented most commonly as central retinal vein occlusion with central retinal artery occlusion as the second most common event, in the absence of any other hypercoagulable or genetic disorder [
6].
Prior reports have described an increased prevalence of retinopathy in association with severe COVID-19, particularly in the setting of abnormal coagulation and inflammatory parameters [
7]. The retinal findings associated with COVID-19 that has been reported however mainly include subtle cotton wool spots and microhemorrhages [
3]. While retinal artery and venous occlusive events appear rare [
3,
7,
8,
9], understanding of these events that may result in severe visual dysfunction is needed for timely diagnosis and treatment when indicated. Whether microvascular disease observed in the retina may reflect microvascular disease involving other organ systems (i.e., pulmonary, renal) also requires further investigation.