Home Isolation and Online Support Strategies during Mild COVID-19 Pandemic Waves in Thailand: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population and Selection
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Effective Management and Vaccine Status
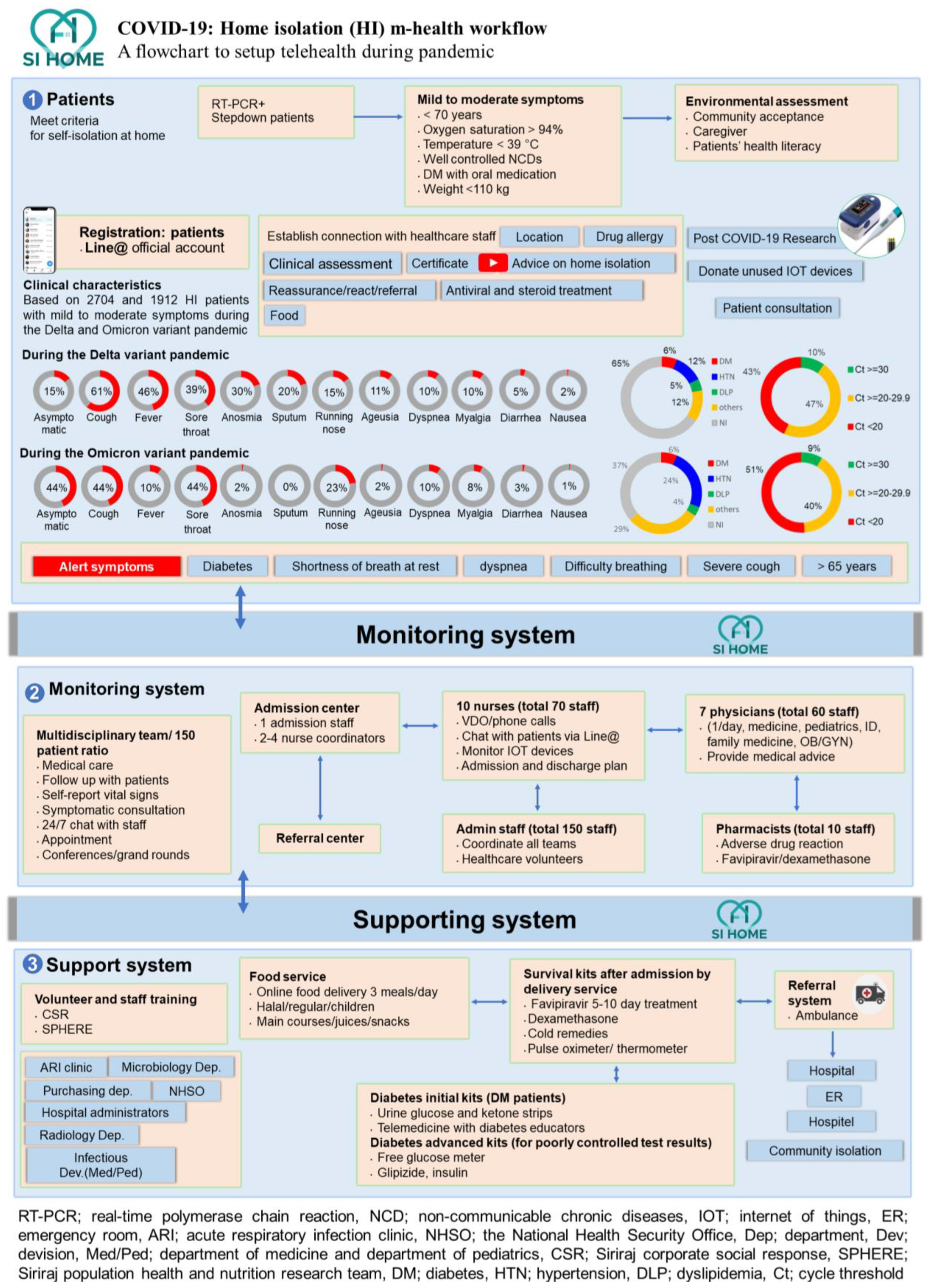
3.2. Establishing Home Isolation Using the Find-Test-Trace-Isolate-Support System
3.3. Adherence to Home Isolation and System Support
4. Discussion
4.1. Digital Tools to Secure Isolation
- Enrollment: To accept and confirm the enrollment of patients assigned to HI. Their data were collected and confirmed using an application programming interface.
- Monitoring: To record, analyze, and summarize the data that patients input into the management system.
4.2. Team Preparedness
4.3. Supporting System
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Triukose, S.; Nitinawarat, S.; Satian, P.; Somboonsavatdee, A.; Chotikarn, P.; Thammasanya, T.; Wanlapakorn, N.; Sudhinaraset, N.; Boonyamalik, P.; Kakhong, B.; et al. Effects of public health interventions on the epidemiological spread during the first wave of the COVID-19 outbreak in Thailand. PLoS ONE 2021, 16, e0246274. [Google Scholar] [CrossRef] [PubMed]
- Thailand WHO. COVID-19-WHO Thailand Situation Reports Bangkok: World Health Organization. 2022. Available online: https://www.who.int/thailand/emergencies/novel-coronavirus-2019/situation-reports (accessed on 4 May 2023).
- Mayurasakorn, K.; Pinsawas, B.; Mongkolsucharitkul, P.; Sranacharoenpong, K.; Damapong, S.-N. School closure, COVID-19 and lunch programme: Unprecedented undernutrition crisis in low-middle income countries. J. Paediatr. Child Health 2020, 56, 1013–1017. [Google Scholar] [CrossRef] [PubMed]
- Kunno, J.; Supawattanabodee, B.; Sumanasrethakul, C.; Wiriyasivaj, B.; Kuratong, S.; Kaewchandee, C. Comparison of Different Waves during the COVID-19 Pandemic: Retrospective Descriptive Study in Thailand. Adv. Prev. Med. 2021, 2021, 5807056. [Google Scholar] [CrossRef] [PubMed]
- Mlcochova, P.; Kemp, S.A.; Dhar, M.S.; Papa, G.; Meng, B.; Ferreira, I.; Datir, R.; Collier, D.A.; Albecka, A.; Singh, S.; et al. SARS-CoV-2 B.1.617.2 Delta variant replication and immune evasion. Nature 2021, 599, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, I.; Kemp, S.A.; Datir, R.; Saito, A.; Meng, B.; Rakshit, P.; Takaori-Kondo, A.; Kosugi, Y.; Uriu, K.; Kimura, I.; et al. SARS-CoV-2 B.1.617 Mutations L452R and E484Q Are Not Synergistic for Antibody Evasion. J. Infect. Dis. 2021, 224, 989–994. [Google Scholar] [CrossRef]
- World Health Organization. Classification of Omicron (B.1.1.529): SARS-CoV-2 Cariant of Concern: World Health Organization. 2021. Available online: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern (accessed on 4 May 2023).
- Markov, P.V.; Ghafari, M.; Beer, M.; Lythgoe, K.; Simmonds, P.; Stilianakis, N.I.; Katzourakis, A. The evolution of SARS-CoV-2. Nat. Rev. Microbiol. 2023, 21, 361–379. [Google Scholar] [CrossRef]
- Cheng, V.C.C.; Ip, J.D.; Chu, A.W.H.; Tam, A.R.; Chan, W.M.; Abdullah, S.M.U.; Chan, B.P.C.; Wong, S.C.; Kwan, M.Y.W.; Chua, G.T.; et al. Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Omicron Subvariant BA.2 in a Single-Source Community Outbreak. Clin. Infect. Dis. 2022, 75, e44–e49. [Google Scholar] [CrossRef]
- Carabelli, A.M.; Peacock, T.P.; Thorne, L.G.; Harvey, W.T.; Hughes, J.; de Silva, T.I.; Peacock, S.J.; Barclay, W.S.; Towers, G.J.; Robertson, D.L.; et al. SARS-CoV-2 variant biology: Immune escape, transmission and fitness. Nat. Rev. Microbiol. 2023, 21, 162–177. [Google Scholar] [CrossRef]
- World Health Organization. Weekly Epidemiological Update on COVID-19-20 April 2023. 2023. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---20-april-2023 (accessed on 4 May 2023).
- World Health Organization. XBB.1.5 Updated Risk Assessment, 24 February 2023. 2023. Available online: https://www.who.int/docs/default-source/coronaviruse/22022024xbb.1.5ra.pdf?sfvrsn=7a92619e_ (accessed on 4 May 2023).
- Yue, C.; Song, W.; Wang, L.; Jian, F.; Chen, X.; Gao, F.; Shen, Z.; Wang, Y.; Wang, X.; Cao, Y. Enhanced transmissibility of XBB.1.5 is contributed by both strong ACE2 binding and antibody evasion. bioRxiv 2023, 2023.01.03.522427. [Google Scholar] [CrossRef]
- Suphanchaimat, R.; Teekasap, P.; Nittayasoot, N.; Phaiyarom, M.; Cetthakrikul, N. Forecasted Trends of the New COVID-19 Epidemic Due to the Omicron Variant in Thailand, 2022. Vaccines 2022, 10, 1024. [Google Scholar] [CrossRef]
- Zhang, Y.; Luo, M.-T.; Wu, Q.; Wang, Y.-X.; Ma, X.; Yan, G.; Zhang, S.-H.; Chen, Y.; Wan, N.; Zhang, L.; et al. Long-term and effective neutralization against omicron sublineages elicited by four platform COVID-19 vaccines as a booster dose. Cell Discov. 2023, 9, 17. [Google Scholar] [CrossRef]
- Lau, J.J.; Cheng, S.M.S.; Leung, K.; Lee, C.K.; Hachim, A.; Tsang, L.C.H.; Yam, K.W.H.; Chaothai, S.; Kwan, K.K.H.; Chai, Z.Y.H.; et al. Real-world COVID-19 vaccine effectiveness against the Omicron BA.2 variant in a SARS-CoV-2 infection-naive population. Nat. Med. 2023, 29, 348–357. [Google Scholar] [CrossRef]
- Dejnirattisai, W.; Huo, J.; Zhou, D.; Zahradník, J.; Supasa, P.; Liu, C.; Duyvesteyn, H.M.E.; Ginn, H.M.; Mentzer, A.J.; Tuekprakhon, A.; et al. SARS-CoV-2 Omicron-B.1.1.529 leads to widespread escape from neutralizing antibody responses. Cell 2022, 185, 467–484.e15. [Google Scholar] [CrossRef] [PubMed]
- Shuai, H.; Chan, J.F.-W.; Hu, B.; Chai, Y.; Yuen, T.T.-T.; Yin, F.; Huang, X.; Yoon, C.; Hu, J.-C.; Liu, H.; et al. Attenuated replication and pathogenicity of SARS-CoV-2 B.1.1.529 Omicron. Nature 2022, 603, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Rickeard, T.; Gallagher, E.; Gower, C.; Kall, M.; Groves, N.; O’Connell, A.-M.; et al. COVID-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N. Engl. J. Med. 2022, 386, 1532–1546. [Google Scholar] [CrossRef] [PubMed]
- Mongkolsucharitkul, P.; Surawit, A.; Pumeiam, S.; Sookrung, N.; Tungtrongchitr, A.; Phisalprapa, P.; Sayabovorn, N.; Srivanichakorn, W.; Washirasaksiri, C.; Auesomwang, C.; et al. SARS-CoV-2 Antibody Response against Mild-to-Moderate Breakthrough COVID-19 in Home Isolation Setting in Thailand. Vaccines 2022, 10, 1131. [Google Scholar] [CrossRef]
- Tan, S.T.; Kwan, A.T.; Rodríguez-Barraquer, I.; Singer, B.J.; Park, H.J.; Lewnard, J.A.; Sears, D.; Lo, N.C. Infectiousness of SARS-CoV-2 breakthrough infections and reinfections during the Omicron wave. Nat. Med. 2023, 29, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Link-Gelles, R.; Ciesla, A.; Roper, L.; Scobie, H.; Ali, A.; Miller, J.D.; Wiegand, R.E.; Accorsi, E.K.; Verani, J.R.; Shang, N.; et al. Early estimates of bivalent mRNA booster dose vaccine effectiveness in preventing symptomatic SARS-CoV-2 infection attributable to Omicron BA.5– and XBB/XBB.1.5–related sublineages among immunocompetent adults—Increasing community access to testing program, United States, December 2022–January 2023. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 119–124. [Google Scholar]
- Chevaisrakul, P.; Lumjiaktase, P.; Kietdumrongwong, P.; Chuatrisorn, I.; Chatsangjaroen, P.; Phanuphak, N. Hybrid and herd immunity 6 months after SARS-CoV-2 exposure among individuals from a community treatment program. Sci. Rep. 2023, 13, 763. [Google Scholar] [CrossRef]
- Johnson, A.G.; Linde, L.; Ali, A.R.; DeSantis, A.; Shi, M.; Adam, C.; Armstrong, B.; Armstrong, B.; Asbell, M.; Auche, S.; et al. COVID-19 incidence and mortality among unvaccinated and vaccinated persons aged ≥12 years by receipt of bivalent booster doses and time since vaccination—24 U.S. jurisdictions, October 3, 2021–December 24, 2022. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 145–152. [Google Scholar] [CrossRef]
- Department of Disease Control, Ministry of Public Health. Thai MOPH Emphasized People to Comply with the Disease Prevention Measures Even COVID-19 Vaccinated: Department of Disease Control, Ministry of Public Health; 2021 [Updated 28 February 2021]. Available online: https://ddc.moph.go.th/oic/news.php?news=17337&deptcode= (accessed on 20 February 2023).
- Kanokudom, S.; Assawakosri, S.; Suntronwong, N.; Auphimai, C.; Nilyanimit, P.; Vichaiwattana, P.; Thongmee, T.; Yorsaeng, R.; Srimuan, D.; Thatsanatorn, T.; et al. Safety and immunogenicity of the third booster dose with inactivated, viral vector, and mRNA COVID-19 vaccines in fully immunized healthy adults with inactivated vaccine. Vaccines 2022, 10, 86. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.-C.; Marlow, S.; Tobias, N.; Alogna, A.; Alogna, I.; You, S.-L.; Khunti, K.; McKee, M.; Michie, S.; Pillay, D. Lessons from countries implementing find, test, trace, isolation and support policies in the rapid response of the COVID-19 pandemic: A systematic review. BMJ Open 2021, 11, e047832. [Google Scholar] [CrossRef] [PubMed]
- National Health Security Office. Thai Government Ensures COVID-19 Essential Health Services 2021. Available online: https://eng.nhso.go.th/view/1/DescriptionNews/Thai-government-ensures-COVID-19-essential-health-services/309/EN-US (accessed on 20 February 2023).
- Aranha, C.; Pate, V.; Bhor, V.; Gogoi, D. Cycle threshold values in RT-PCR to determine dynamics of SARS-CoV-2 viral load An approach to reduce the isolation period for COVID-19 patients. J. Med. Virol. 2021, 93, 6794–6797. [Google Scholar] [CrossRef]
- Sirijatuphat, R.; Manosuthi, W.; Niyomnaitham, S.; Owen, A.; Copeland, K.K.; Charoenpong, L.; Rattanasompattikul, M.; Mahasirimongkol, S.; Wichukchinda, N.; Chokephaibulkit, K. Early treatment of Favipiravir in COVID-19 patients without pneumonia: A multicentre, open-labelled, randomized control study. Emerg. Microbes Infect. 2022, 11, 2197–2206. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, N.R.; Molina, K.C.; Beaty, L.E.; Bennett, T.D.; Carlson, N.E.; Mayer, D.A.; Peers, J.L.; Russell, S.; Wynia, M.K.; Ginde, A.A. Real-world use of nirmatrelvir-ritonavir in outpatients with COVID-19 during the era of omicron variants including BA.4 and BA.5 in Colorado, USA: A retrospective cohort study. Lancet Infect. Dis. 2023, 23, 696–705. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Nussbaumer-Streit, B.; Mayr, V.; Dobrescu, A.I.; Chapman, A.; Persad, E.; Klerings, I.; Wagner, G.; Siebert, U.; Ledinger, D.; Zachariah, C.; et al. Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database Syst. Rev. 2020, 4, Cd013574. [Google Scholar]
- Auranen, K.; Shubin, M.; Erra, E.; Isosomppi, S.; Kontto, J.; Leino, T.; Lukkarinen, T. Efficacy and effectiveness of case isolation and quarantine during a growing phase of the COVID-19 epidemic in Finland. Sci. Rep. 2023, 13, 298. [Google Scholar] [CrossRef]
- Uansri, S.; Tuangratananon, T.; Phaiyarom, M.; Rajatanavin, N.; Suphanchaimat, R.; Jaruwanno, W. Predicted Impact of the Lockdown Measure in Response to Coronavirus Disease 2019 (COVID-19) in Greater Bangkok, Thailand, 2021. Int. J. Environ. Res. Public Health 2021, 18, 12816. [Google Scholar] [CrossRef]
- World Health Organization. Considerations for quarantine of contacts of COVID-19 cases: Interim guidance, 19 August 2020. Geneva, Switzerland: World Health Organization; 2020. Available online: https://apps.who.int/iris/handle/10665/333901 (accessed on 7 May 2023).
- Sungsana, W.; Nakaranurack, C.; Weeraphon, B.; Charoenwaiyachet, W.; Chanprasert, S.; Torvorapanit, P.; Santimaleeworagun, W.; Putcharoen, O. Telepharmacy during home isolation: Drug-related problems and pharmaceutical care in COVID-19 patients receiving antiviral therapy in Thailand. J. Pharm. Policy Pract. 2023, 16, 29. [Google Scholar] [CrossRef]
- National Center for Immunization and Respiratory Diseases DoVD. Isolation and Precautions for People with COVID-19: Center for Disease Control and Prevention 2023. Available online: https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html (accessed on 7 May 2023).
- Brown, K.; Yahyouche, A.; Haroon, S.; Camaradou, J.; Turner, G. Long COVID and self-management. Lancet 2022, 399, 355. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Soave, P.M.; Antonelli, M. Treating Anti-Vax Patients, a New Occupational Stressor—Data from the 4th Wave of the Prospective Study of Intensivists and COVID-19 (PSIC). Int. J. Environ. Res. Public Health 2022, 19, 5889. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.; Chen, W.; Liu, J.; Yang, A.; Shu, K.; Zhou, Y.; Wang, M.; Huang, M.; Liao, M.; Liu, J.; et al. Effects of centralized isolation vs. home isolation on psychological distress in patients with COVID-19. J. Psychosom. Res. 2021, 143, 110365. [Google Scholar] [CrossRef] [PubMed]
- Hassanipour, S.; Arab-Zozani, M.; Amani, B.; Heidarzad, F.; Fathalipour, M.; Martinez-de-Hoyo, R. The efficacy and safety of Favipiravir in treatment of COVID-19: A systematic review and meta-analysis of clinical trials. Sci. Rep. 2021, 11, 11022. [Google Scholar] [CrossRef]
- Sayabovorn, N.; Phisalprapa, P.; Srivanichakorn, W.; Washirasaksiri, C.; Auesomwang, C.; Sitasuwan, T.; Tinmanee, R.; Chayakulkeeree, M.; Phoompoung, P.; Mayurasakorn, K.; et al. Early diagnosis by antigen test kit and early treatment by antiviral therapy: An ambulatory management strategy during COVID-19 crisis in Thailand. Med. Baltim. 2022, 101, e29888. [Google Scholar] [CrossRef]
- Foroozanfar, Z.; Zamanian, M.; Moradzadeh, R.; Hajiabadi, F.; Ahmadzadeh, J.; Hosseinkhani, Z. Isolation Compliance and Associated Factors Among COVID-19 Patients in North-West Iran: A Cross-Sectional Study. Int. J. Gen. Med. 2020, 13, 1697–1703. [Google Scholar] [CrossRef]
- Almathami, H.K.Y.; Win, K.T.; Vlahu-Gjorgievska, E. Barriers and Facilitators That Influence Telemedicine-Based, Real-Time, Online Consultation at Patients’ Homes: Systematic Literature Review. J. Med. Internet Res. 2020, 22, e16407. [Google Scholar] [CrossRef] [PubMed]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinsawas, B.; Ophakas, S.; Bedavanija, A.; Kochasawas, W.; Jitpun, P.; Leemongkol, S.; Phisalprapa, P.; Srivanichakorn, W.; Chaisathaphol, T.; Washirasaksiri, C.; et al. Home Isolation and Online Support Strategies during Mild COVID-19 Pandemic Waves in Thailand: A Scoping Review. COVID 2023, 3, 987-998. https://doi.org/10.3390/covid3070071
Pinsawas B, Ophakas S, Bedavanija A, Kochasawas W, Jitpun P, Leemongkol S, Phisalprapa P, Srivanichakorn W, Chaisathaphol T, Washirasaksiri C, et al. Home Isolation and Online Support Strategies during Mild COVID-19 Pandemic Waves in Thailand: A Scoping Review. COVID. 2023; 3(7):987-998. https://doi.org/10.3390/covid3070071
Chicago/Turabian StylePinsawas, Bonggochpass, Suphawan Ophakas, Anan Bedavanija, Wanwalee Kochasawas, Phakamas Jitpun, Suree Leemongkol, Pochamana Phisalprapa, Weerachai Srivanichakorn, Thanet Chaisathaphol, Chaiwat Washirasaksiri, and et al. 2023. "Home Isolation and Online Support Strategies during Mild COVID-19 Pandemic Waves in Thailand: A Scoping Review" COVID 3, no. 7: 987-998. https://doi.org/10.3390/covid3070071
APA StylePinsawas, B., Ophakas, S., Bedavanija, A., Kochasawas, W., Jitpun, P., Leemongkol, S., Phisalprapa, P., Srivanichakorn, W., Chaisathaphol, T., Washirasaksiri, C., Auesomwang, C., Sitasuwan, T., Tinmanee, R., Sayabovorn, N., Nopmaneejumruslers, C., Chayakulkeeree, M., Phoompoung, P., Sanpawitayakul, G., Wanitphakdeedecha, R., ... on behalf of the SPHERE Group. (2023). Home Isolation and Online Support Strategies during Mild COVID-19 Pandemic Waves in Thailand: A Scoping Review. COVID, 3(7), 987-998. https://doi.org/10.3390/covid3070071






