Abstract
Coronavirus disease 2019 is a highly contagious infectious disease. Research on heart rhythm disorders in children affected by COVID-19 infection is quite lacking. An infant and a congenital heart disease (CHD) teenager with a pacemaker presented fascicular tachycardia and atrial flutter, respectively, during COVID-19 pauci-symptomatic infection. The hemodynamic condition was always stable. The self-resolving trend of the atrial flutter and progressive resolution of the ventricular tachycardia occurred in conjunction with the negativization of the swab. These particular tachyarrhythmias have been reported as a form of potential arrhythmic complication during active pauci-symptomatic COVID-19 infection for the first time ever.
1. Introduction
Coronavirus disease 2019 (COVID-19) is a highly contagious infectious disease that is widespread worldwide. COVID-19 has multiorgan consequences with subsequent outcomes of varying severity.
Our worldwide knowledge about this new virus is mostly based on studies in adults, which demonstrate aftermaths of the virus on the respiratory system, but there are many hemodynamic complications and electrophysiologic abnormalities as well. Some reports and one review describe life-threatening arrhythmias as a potential severe complication in COVID-19 adult patients, especially patients who suffer from pre-existing heart disease (such as inherited arrhythmias syndrome) and other comorbidities, such as renal failure, hypertension, diabetes, acute respiratory distress syndrome (ARDS), or cancer [1,2,3]. Hypoxia, electrolyte imbalances, and the hyper-inflammatory response (IL-6, TNF-α, IL-1) are risk factors for the ion K+ and Ca+ channel dysfunction, which can lead to the onset of arrhythmias, especially ventricular arrhythmias from simple premature ventricular contractions (PVCs) up to Torsades de Pointes or ventricular fibrillation. Up to now, literature regarding the heart rhythm disorders in pediatric patients affected by COVID-19 infection has been quite lacking. Mostly, pediatric studies report the most frequent arrhythmic involvement during multisystem inflammatory syndrome in children; in particular, 7–60% of patients have cardiac rhythm disorders, which include aspecific repolarization abnormalities, QTc prolongation, first- and second atrio-ventricular block, premature ventricular contractions and premature atrial contractions, supraventricular tachyarrhythmias (especially atrial fibrillation), and non-sustained ventricular tachyarrhythmias [4]. On the contrary, acute pediatric COVID-19 infections are usually asymptomatic and mild and healthy children generally do not develop severe cardiac manifestations [5]. As a matter of fact, they tend to have less life-threatening arrhythmias, such as premature ventricular contractions, premature atrial contractions, incomplete right bundle branch block, first degree atrio-ventricular block, or supraventricular tachycardias [6]. One study reports a very low percent of mild electrophysiological involvement (12% of repolarization abnormalities and mild PR prolongation) in non-hospitalized children with asymptomatic mild COVID-19 infection [7]. These mild heart rhythm disorders then spontaneously resolved over time. Another worldwide study reports 15% of arrhythmic complications in a huge hospitalized pediatric population without further details about the type or severity of arrhythmias [8].
A past medical history of congenital heart disease (CHD), bronchopulmonary disease, immune system deficiency, and hemoglobinopathies are considered to be predisposing factors for the development of severe cardiac manifestations, both hemodynamic (acute heart failure, myo-pericarditis) and arrhythmic cases [9]. Rare case reports describe the association and the outcome between CHD and arrhythmias or between healthy children and severe arrhythmias.
In this study, we report two unusual COVID-19-related arrhythmic cases that were collected from March 2020 to October 2021 by our tertiary referral center.
2. Case Presentation
2.1. Case 1
A 10-month-old baby presented to the pediatric emergency department with irritability and inconsolable crying for 24 h without other symptoms, including fever or either respiratory or gastrointestinal involvement. Upon his arrival, the infant had stable hemodynamic condition with normal blood pressure for age, but the heart rhythm was tachycardic. No heart murmurs or pericardial rubs were found. Additionally, no respiratory pathological noises or gastrointestinal pathological signs were detected. On the electrocardiogram, sustained ventricular tachycardia was found at 220 beats per minute (bpm) (Figure 1). An echocardiogram was performed, which showed no congenital heart disease, ventricular dysfunction, or coronary dilatation. The baby had no family history of sudden death or rhythm disorders.
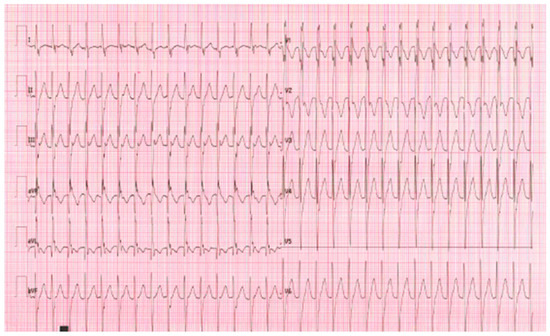
Figure 1.
Posterior left fascicular tachycardia (left axis deviation with RBBB).
The pre-admission nasopharyngeal swab was positive for COVID-19 with all the other blood exams negative, especially inflammatory tests (C-reactive protein) and troponin. The serology for SARS-CoV-2 demonstrated high antibody titer for IgM (6797 kU/L). Continuous intravenous therapy with amiodarone was started, which was effective even if there were still some paroxysms of tachycardia in the following four days. The intravenous antiarrhythmic therapy was gradually matched with oral somministration up to the total oral administration of amiodarone.
The arrhythmia was overall well controlled without recurrence of ventricular tachyarrhythmia. Another echocardiography was performed after 5 days, showing normal systolic and diastolic biventricular function with normal size of coronary arteries. The patient was discharged in good condition with stable sinus rhythm after 21 days of recovery on oral antiarrhythmic therapy with amiodarone (7 mg/kg/die three times per day).
2.2. Case 2
A 16-year-old teenager with surgically corrected congenital heart disease (atrio-ventricular septal defect (AVSD) and a dual chamber pacemaker for post-surgical complete AV block reported palpitations in the two days preceding access to the pediatric emergency department. Remote control of the device at the beginning of symptoms showed the onset of atrial flutter from 2 days before; this supraventricular tachyarrhythmia has been never detected at the previous periodic PM controls in telemedicine.
Upon arrival at the emergency department, the patient presented stable hemodynamic condition and was completely asymptomatic; the EKG confirmed an atrial flutter 2:1 at the heart rate of 120 bpm (Figure 2).
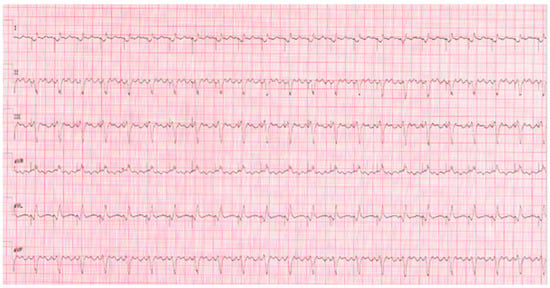
Figure 2.
Atrial flutter 2:1.
The pre-admission nasopharyngeal swab was positive for COVID-19, with all the other blood exams negative. C-reactive protein, the other inflammation tests, and troponin were negative. An echocardiogram was performed without signs of enlargement of both atria or valve insufficiency, ventricular dysfunction, or coronary dilatation.
Anticoagulant therapy with subcutaneous heparin was started without considering an antiarrhythmic therapy, but the pacemaker was reprogrammed (DDIR 75–160 bpm) by obtaining a median heart rate of 80 bpm with persistent heart rhythm disorder.
After 15 days of quarantine, the nasopharyngeal swab was negative. Remote control of the device showed the spontaneous restoration of the sinus rhythm in correspondence with the negativization of the swab (Figure 3). No further supraventricular arrhythmias were detected in the next short-term and medium-term follow-up.
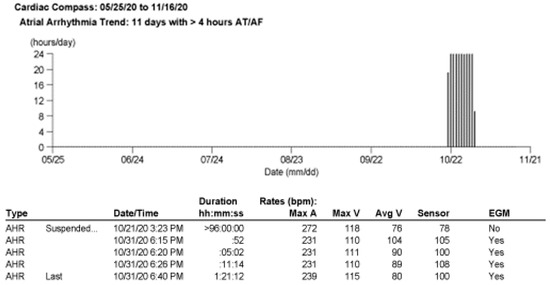
Figure 3.
Remote control of PM about FLA.
3. Discussion
Some previous studies and reviews have reported a correlation between electrophysiologic abnormalities and COVID-19 in children. Sharmeen et al. described a pediatric population affected by COVID-19 infection with low prevalence of significant arrhythmias (NSVT or AT) in normal heart [10]. One interesting and a rare case was described by US colleagues [11]. During the acute phase of symptomatic COVID-19 infection, a 9-day-old girl presented with aberrant supraventricular tachycardia, which was correctly diagnosed and then effectively treated by overdrive through a transesophageal pacing.
Up to now, no literature has described an atrial flutter in congenital heart disease during a COVID-19 infection, especially in regard to pediatric population.
The only case report talks about an adult patient with a previously healthy heart who had been affected by severe SARS-CoV-2 infection that was complicated by cardiovascular involvement, especially an arrhythmic one [12]. This patient presented an atrial flutter with high ventricular response rate that further compromised the cardiac pump function and the critical respiratory situation. The antiarrhythmic therapy failed, and catheter ablation had to be performed, despite the patient’s critically ill condition. The procedure was effective in terms of the stable restoration of sinus rhythm and respiratory conditions. Unlike this case, we did not have to perform any medical therapy or invasive procedure during the acute phase because the girl was completely asymptomatic both for cardiac hemodynamic involvement and respiratory involvement, despite the cardiac heart disease. As a matter of fact, the hypothesis of concomitant myocarditis was ruled out by analyzing the primary data collected from cardiac objectivity, the negative blood test, and the normal biventricular function in both of the patients. The myocardial involvement during the acute phase of SARS-CoV-2 infection is well known [13], but these two patients basically had arrhythmic complications of the acute COVID-19 infection, which were then followed by stable restoration of sinus rhythm.
For the first time, we recorded this type of supraventricular tachycardia as it occurred spontaneously in a CHD pediatric patient with stable hemodynamic condition. This type of tachyarrhythmia is typically related as a potential arrhythmic consequence during post-surgical follow-up of this CHD; nevertheless, the hemodynamic instability has not been previously reported in this case or from any other potential causes as well. The temporal correlation between the duration of this supraventricular tachycardia and the microbiological positivization might suggest the role of this virus as trigger factor of cardiac arrhythmia.
The broad spectrum of ventricular tachyarrhythmias (VTs) has been already reported as arrhythmic involvement which is related to hemodynamic deterioration in critical COVID-19 disease, but no fascicular tachycardia has been documented either in adult or in pediatric populations.
Considering the quite rare manifestation of this VT during the first decade of life of a healthy child, it is undoubtedly even rarer to record a fascicular tachycardia in a 10- month-old baby with normal heart and stable hemodynamic condition.
This is the first time ever that this idiopathic ventricular tachycardia has been registered in a healthy infant who also had a documented SARS-CoV-2 infection. Could the SARS-CoV-2 infection really be a co-factor of fascicular tachycardia in this case?
We thought this might be a possibility, which is supported by the good control of the heart rhythm on antiarrhythmic therapy after the negativization of the swab.
4. Conclusions
The worldwide literature about the correlation between pediatric cardiac arrhythmias and COVID-19 is growing.
These particular tachyarrhythmias have been reported as potential arrhythmic complications during active pauci-symptomatic COVID-19 infection for the first time ever. The self-resolving trend of the AFL and the progressive resolution of the fascicular tachycardia occurred in conjunction with the negativization of the swab. Might it be only SARS-CoV-2 infection correlated? This could be a good hypothesis, but the long-term follow-up needs to be studied.
5. Learning Objectives
5.1. Case 1: An Infant with Posterior Left Fascicular Tachycardia
- To define the etiology of the fascicular tachycardia
- To understand the role of COVID-19 as a trigger factor of the ventricular tachycardia
5.2. Case 2: A CHD Patient with PMK and Atrial Flutter
- To define the trigger mechanism of the supraventricular tachycardia
- To understand the time correlation between the arrhythmias and COVID-19 infection
Author Contributions
Conceptualization: J.F.; methodology: J.F.; software: J.S. and J.F.; validation: R.B., E.R., G.D.S. and L.L.; formal analysis: J.F. and J.S.; investigation: J.F.; resources: L.L. and J.F.; data curation: J.F.; writing—original draft preparation: J.F.; writing—review and editing: J.S. and L.L.; visualization: J.F.; supervision: J.S. and L.L.; project administration: J.F.; funding acquisition: G.D.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study did not require ethical approval.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data was derived from the management system of patients at Children’s Hospital, Pediatric Cardiology Unit, of Padua and the telemedicine monitoring system of implanted devices.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dherange, P.; Lang, J.; Qian, P.; Oberfeld, B.; Sauer, W.H.; Koplan, B.; Tedrow, U. Arrhythmias and COVID-19: A Review. JACC Clin. Electrophysiol. 2020, 6, 1193–1204. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, A.; Mayer, M.M.; Adusumalli, S.; Hyman, M.C.; Oh, E.; Tierney, A.; Moss, J.; Chahal, A.A.; Anesi, G.; Denduluri, S.; et al. COVID-19 and cardiac arrhythmias. Heart Rhythm 2020, 17, 1439–1444. [Google Scholar] [CrossRef] [PubMed]
- Manolis, A.S.; Manolis, A.A.; Manolis, T.A.; Apostolopoulos, E.J.; Papatheou, D.; Melita, H. COVID-19 infection and cardiac arrhythmias. Trends Cardiovasc. Med. 2020, 30, 451–460. [Google Scholar] [CrossRef] [PubMed]
- Sperotto, F.; Friedman, K.G.; Son, M.B.F.; VanderPluym, C.J.; Newburger, J.W.; Dionne, A. Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: A comprehensive review and proposed clinical approach. Eur. J. Pediatr. 2021, 180, 307–322. [Google Scholar] [CrossRef] [PubMed]
- de Souza, T.H.; Nadal, J.A.; Nogueira, R.J.N.; Pereira, R.M.; Brandão, M.B. Clinical Manifestations of Children with COVID-19: A Systematic Review. Pediatr. Pulmonol. 2020, 55, 1892–1899. [Google Scholar] [CrossRef] [PubMed]
- Xia, W.; Shao, J.; Guo, Y.; Peng, X.; Li, Z.; Hu, D. Clinical and CT features in pediatric patients with COVID-19 infection: Different points from adults. Pediatr. Pulmonol. 2020, 55, 1169–1174. [Google Scholar] [CrossRef] [PubMed]
- Heching, H.J.; Goyal, A.; Harvey, B.; Malloy-Walton, L.; Follansbee, C.; Mcintosh, A.; Forsha, D. Electrocardiographic changes in non-hospitalised children with COVID-19. Cardiol. Young 2022, 32, 1910–1916. [Google Scholar] [CrossRef] [PubMed]
- Bourgeois, F.T.; Gutiérrez-Sacristán, A.; Keller, M.S.; Liu, M.; Hong, C.; Bonzel, C.L.; Tan, A.L.M.; Aronow, B.J.; Boeker, M.; Booth, J.; et al. International Analysis of Electronic Health Records of Children and Youth Hospitalized with COVID-19 Infection in 6 Countries. JAMA Netw. Open 2021, 4, e2112596. [Google Scholar] [CrossRef] [PubMed]
- Sanna, G.; Serrau, G.; Bassareo, P.P.; Neroni, P.; Fanos, V.; Marcialis, M.A. Children’s heart and COVID-19: Up-to-date evidence in the form of a systematic review. Eur. J. Pediatr. 2020, 179, 1079–1087. [Google Scholar] [CrossRef] [PubMed]
- Samuel, S.; Friedman, R.A.; Sharma, C.; Ganigara, M.; Mitchell, E.; Schleien, C.; Blaufox, A.D. Incidence of arrhythmias and electrocardiographic abnormalities in symptomatic pediatric patients with PCR-positive SARS-CoV-2 infection, including drug-induced changes in the corrected QT interval. Heart Rhythm 2020, 17, 1960–1966. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, K.A.; Webster, G. Aberrated supraventricular tachycardia associated with neonatal fever and COVID-19 infection. BMJ Case Rep. 2021, 14, e241846. [Google Scholar] [CrossRef] [PubMed]
- Bertini, M.; Vitali, F.; Malagù, M.; Rapezzi, C. Atrial Flutter in Patient with Critical COVID-19: Beneficial Effects of Rhythm Control on Respiratory Distress. JACC Case Rep. 2021, 3, 162–164. [Google Scholar] [CrossRef]
- Castiello, T.; Georgiopoulos, G.; Finocchiaro, G.; Claudia, M.; Gianatti, A.; Delialis, D.; Aimo, A.; Prasad, S. COVID-19 and myocarditis: A systematic review and overview of current challenges. Heart Fail. Rev. 2022, 27, 251–261. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).