Abstract
The COVID-19 pandemic has affected the outcomes of ST-elevation myocardial infarction (STEMI) patients in most countries. We aimed to retrospectively assess the admissions, treatments, complications, and mortality of STEMI patients in the northeast of Slovenia during the first (March–May 2020) and second waves (October–December 2020) of the COVID-19 pandemic and to compare them with data from 2019 (March–October). Comparing 2019 and both waves of the COVID-19 pandemic, we observed nonsignificant differences in the number of STEMI admissions, baseline characteristics, use of primary percutaneous coronary intervention (PCI) within the first 3 (40.5%* vs. 38.7% vs. 25%*, *p = 0.074) or 6 h, TIMI III flow after primary PCI, and hospital complications, as well as significant increases in hospital heart failure (23.3% vs. 42%, p = 0.015) and mitral regurgitation in the second wave (10% vs. 26.9%, p = 0.008) of the pandemic and a nonsignificant increase in hospital mortality (8.9% vs. 9.4% vs. 13.6%) during both waves of the pandemic. We conclude that, due to the increased severity of the COVID-19 pandemic in the second wave, there were longer delays to primary PCI in STEMI patients, resulting in significantly increased hospital heart failure and non-significantly increased hospital mortality.
1. Introduction
In early March 2020, the WHO classified COVID-19 as a pandemic due to the rapid, worldwide spread of the highly contagious SARS-CoV-2 virus [1]. To date, more than 500 million people have been infected and more than 6 million people have died of the novel coronavirus disease (COVID-19) [1,2,3]. In more than 80% of cases, COVID-19 is an asymptomatic or a mild–moderate respiratory disorder. In approximately 14% of patients, COVID-19 presents as a more severe respiratory disease with dyspnea and a need for ICU admission, and 5% develop a critical illness with ARDS and multiorgan failure syndrome, which is responsible for the increased mortality of COVID-19 patients [4,5]. To limit the spread of COVID-19, the majority of countries, including Slovenia, implemented strict social containment measures, including lockdowns [6]. At the peak of the pandemic, hospitals, and intensive care units in particular, were overcrowded in every country, and at the same time, there was excess mortality from respiratory failure in critically ill COVID-19 patients [6]. To accommodate the increased workload in intensive care units, hospitals, and emergency rooms (ER), healthcare facilities were reorganized [6,7]. There was a rapid mobilization of substantial healthcare resources worldwide geared exclusively toward COVID-19, and levels of care for other noncommunicable disorders were reduced. The consequence was reduced patient visits to ERs, family physicians, outpatient clinics, and hospitals for medical conditions other than COVID-19 [6,7]. Elective surgery, diagnostics, and therapeutic procedures were canceled; only emergency and urgent procedures and treatments were performed. At the same time, patients were anxious and avoided medical facilities to prevent infection.
In most countries, cardiologists reported a significant decrease in admissions of ST-segment elevation myocardial infarction (STEMI) patients, a decrease in the number of primary percutaneous coronary interventions (PCI), and substantial delays in the start of treatment [7,8,9,10,11,12]. The most important causes were fear, prolonged transport to the ER due to the use of personal protective equipment by medical staff, testing for COVID-19, waiting for the results with prolonged triage in the ER, prolonged transport to the catheterization laboratory, and prolonged time of coronary intervention [13,14,15]. Studies have predominantly reported worse outcomes in STEMI patients, with hospital mortality exceeding 10%, particularly in COVID-19 epicenters in Italy and China [9,12,15,16].
In the three first months (March to May 2020) of the pandemic in Slovenia, only 1398 COVID-19 cases were registered among its 2,000,000 inhabitants, but the number of COVID-19 cases increased to 117,853 from October to December 2020, with a parallel increase in patient mortality [17]. To overcome the pandemic, social restrictions continued, along with the mobilization of healthcare resources to cater to COVID-19 patients. The reduction in care for patients with other noncommunicable disorders escalated even further in autumn 2020 [6,17].
Our aim was to assess STEMI admissions, delays in treatment, in-hospital complications, and mortality during the first and second waves of the COVID-19 pandemic and to compare the data to pre-pandemic data from 2019.
2. Materials and Methods
This was a retrospective monocenter observational study of STEMI patients during the first and second waves of the COVID-19 pandemic in 2020 that involved comparing the 2020 data to pre-pandemic data from 2019. The study was conducted at University Clinical Centre Maribor, a tertiary clinical institution in the northeast of Slovenia. It is the referral 24/7 regional center for primary PCI in STEMI patients and covers an area with a population of 850,000.
2.1. Data Collection
In this study, we retrospectively included all consecutive patients referred with a diagnosis of STEMI from March to May 2020 (during the first wave of the COVID-19 pandemic), from October to December 2020 (during the second wave of the COVID-19 pandemic), and from March to May 2019 (pre-pandemic). We extracted standard patient data from electronic medical records according to the ICD-10 code, and a supervising physician carefully reviewed them. Well-known criteria established the diagnosis of STEMI [13]. We registered the demographic, clinical, and mortality data of STEMI patients.
2.2. Methods
Primary PCI was the main reperfusion strategy. The treatment of STEMI patients in 2019 was in accordance with set guidelines. In 2020, treatment procedures were adapted to the COVID-19 pandemic, which involved prior, time-consuming testing for SARS-CoV-2 infection before obtaining the results, as well as using protective equipment [18,19].
We gathered data on gender, age, prior myocardial infarction, diabetes, arterial hypertension, resuscitation before admission, and time to primary PCI. From the laboratory data, we noted measurements of cardiac troponin I and serum creatinine on admission, as well as peak levels during in-hospital stay. From the treatment data, we noted the use of primary PCI, TIMI (thrombolysis in myocardial infarction) flows before and after primary PCI, and radial or femoral access.
After primary PCI, we monitored the patients in the medical ICU or coronary care unit for approximately 24 h or longer in case of complications until we transferred them to the cardiology ward or local hospitals in stable condition [18,19].
During hospital stay, we registered acute complications, such as in-hospital acute heart failure, arrhythmias, acute bleeding, acute kidney dysfunction, in-stent thrombosis, hospital infection, COVID-19, and mortality. Acute heart failure was classified as either pulmonary congestion (Killip class II), pulmonary edema (Killip class III), or cardiogenic shock or any hypotension necessitating a vasopressor infusion (Killip class IV) [18,19,20]. We registered arrhythmias as ventricular and/or atrial. We registered acute kidney dysfunction as an increase in serum creatinine by at least 50% from the baseline within the first 72 h [18].
Hospital infection was defined as the presence of microorganisms in the otherwise sterile milieu of the body (blood, cerebrospinal liquor, lung tissue, urinary tract, etc.) with or without clinical symptoms (fever, increased CRP, leukocytosis, or leukocytopenia) or as antibiotic administration due to strong clinical suspicion of infection [21].
We also registered COVID-19 infection via positive PCR tests for SARS-CoV-2.
We registered all standard pharmacological treatments (the use of acetylsalicylic acid (ASA) with clopidogrel, ticagrelor, or prasugrel; heparins; noradrenalin; dobutamin; levosimendan; loop diuretic; and glycoprotein receptor antagonist IIb/IIIa) and treatments used for complications (insertion of intra-aortic balloon pump (IABP) and mechanical ventilation). Patients’ left ventricular systolic function was assessed using transthoracic echocardiography during in-hospital stay [18,19].
2.3. Data Analysis and Endpoints
We compared the baseline, treatment, complication, and mortality data between STEMI patients in 2019 and STEMI patients during the first and the second waves of the COVID-19 pandemic with an emphasis on the following:
- The number of STEMI admissions during both waves of the COVID-19 pandemic;
- The time delay to primary PCI during both waves of the pandemic;
- The prevalence of complications in STEMI patients during both waves of the pandemic;
- The mortality data of STEMI patients during both waves of the pandemic.
2.4. Ethical Approval
The Institutional Medical Ethics Committee (University Clinical Center Maribor Medical Ethics Committee (KME)) approved the retrospective observational study (approval UKC-MB KME-62/19). The informed consent of the included patients was waived due to the retrospective nature of the study. The study was conducted in accordance with the 1964 Declaration of Helsinki and its subsequent amendments. We protected the personal data of the patients according to the Law on Personal Data Protection.
2.5. Statistical Analysis
Statistical analysis was performed using the SPPS Statistical package version 19 (IBM Corp., Armonk, NY, USA) for Windows. We present the data as means ± standard deviations or percentages. We used the two-sided Student’s t-test to test the differences between the groups for means ± standard deviations and Fisher’s exact test for percentages. A p value < 0.05 was considered statistically significant. Kaplan–Meier survival curves were employed to show the 30-day and 6-month survival of STEMI patients in 2019 and during the first and second waves of the pandemic. A p value < 0.05 was considered statistically significant.
3. Results
3.1. Baseline Characteristics
We present the baseline characteristics of all included patients in Table 1. There were nonsignificant differences in the number of STEMI admissions (90 patients vs. 96 patients vs. 81 patients), gender, mean age, age over 65 years, comorbidities, resuscitation before admission, anterior STEMI location, and admission troponin I levels between STEMI patients in 2019 and STEMI patients during both waves of the COVID-19 pandemic.

Table 1.
Comparison of baseline characteristics between STEMI patients in March–May 2019, March–May 2020 (first wave of the COVID-19 pandemic), and October–December 2020 (second wave of the COVID-19 pandemic).
We observed a nonsignificant increase in admissions for acute heart failure (30% vs. 34.4% vs. 40.5%; pre-pandemic, first wave, second wave, respectively) and an increase in prior resuscitation in the second wave of the pandemic (10% vs. 10.4% vs. 16.5%, respectively). We also observed a nonsignificant decline in primary PCI within the first 6 h and within the first 3 h during the pandemic (40.5% vs. 38.7% vs. 25%, respectively; p = 0.075).
3.2. Treatment Data
We present the hospital treatment data in Table 2. We observed similar rates of primary PCI (94.4% vs. 94.8% vs. 91.4%), TIMI III flow after primary PCI, and radial access in all three time periods. The use of mechanical ventilation was similar in 2019 and during the first wave of the COVID-19 pandemic, but it was non-significantly increased during the second wave (Table 2).

Table 2.
Comparison of treatments in STEMI patients in March–May 2019, March–May 2020 (first wave of the COVID-19 pandemic), and October–December 2020 (second wave of the COVID-19 pandemic).
There were nonsignificant differences in the use of various pharmacological therapies between 2019 and the first and second waves of the COVID-19 pandemic (Table 2). Meanwhile, beta blockers were used significantly less frequently during the second wave of the pandemic due to the increased prevalence of heart failure in this period.
In Table 3, we present target coronary vessels and TIMI flows before and after primary PCI. Nonsignificant differences were observed between the STEMI groups.

Table 3.
Comparison of target vessels and TIMI flows before and after primary PCI of STEMI patients in March–May 2019, March–May 2020 (first wave of the COVID-19 pandemic), and October–December 2020 (second wave of the COVID-19 pandemic).
3.3. Hospital Complications and Mortality Data
Hospital complication and mortality data are presented in Table 4. We observed similar increases in peak troponin I levels ≥ 50 µg/L, similar decreases in EF levels < 45%, and similar in-stent thrombosis and reinfarction prevalence in all three time periods. Between STEMI patients in 2019 and STEMI patients in the first wave of the COVID-19 pandemic, we observed similar acute kidney injury (6.6% vs. 5.2% vs. 10.7%; pre-pandemic, first wave, second wave, respectively) and arrhythmias prevalence, but nonsignificant increases were observed during the second wave of the pandemic. In comparison to 2019, we observed a nonsignificant increase in hospital infections (17.8% vs. 18.8% vs. 26.9%) and bleeding (8.9% vs. 12.5% vs. 11.1%) during both waves of the COVID-19 pandemic. Concomitant COVID-19 was observed in 5.2% of patients during the first wave and 4.9% of patients during the second wave of the pandemic.

Table 4.
Comparison of hospital complications in STEMI patients in March–May 2019, March–May 2020 (first wave of the COVID-19 pandemic), and October–December 2020 (second wave of the COVID-19 pandemic).
Compared with 2019, we observed a nonsignificant increase in hospital heart failure (23.3%* vs. 27.1% vs. 42%*; p = 0.015) and mitral regurgitation (10%* vs. 18.8% vs. 26.9%*; p = 0.008) in the first wave and a significant increase in both complications in the second wave. We observed increased hospital mortality in STEMI patients in both waves of the COVID-19 pandemic, particularly the second one, but the difference was not statistically significant (8.9% vs. 9.4% vs. 13.6%).
Kaplan–Meier 30-day and 6-month survival curves for STEMI patients in 2019 and during the first and second waves of the COVID-19 pandemic are presented in Figure 1 and Figure 2, respectively.
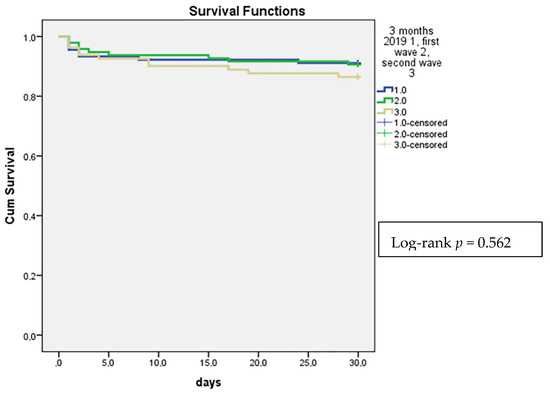
Figure 1.
Comparison of Kaplan–Meier 30-day survival curves in STEMI patients in March–May 2019, March–May 2020 (first wave of the COVID-19 pandemic), and October–December 2020 (second wave of the COVID-19 pandemic).
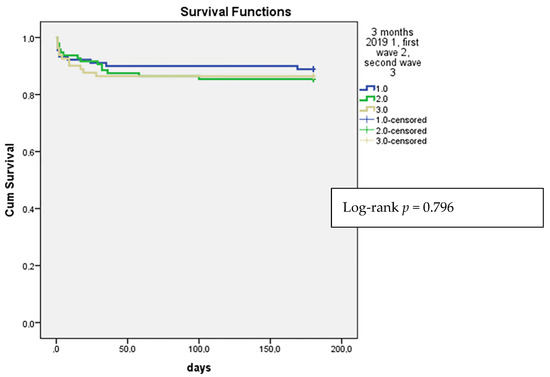
Figure 2.
Comparison of Kaplan–Meier 6-month survival curves in STEMI patients in March–May 2019, March–May 2020 (first wave of the COVID-19 pandemic), and October–December 2020 (second wave of the COVID-19 pandemic).
The 30-day survival of STEMI patients in 2019 was 91.1%, compared to 90.6% during the first wave and 86.4% during the second wave of the COVID-19 pandemic (Figure 1).
The 6-month survival of STEMI patients in 2019 was 88.9%, compared to 85.4% during the first wave and 86.4% during the second wave of the COVID-19 pandemic (Figure 2).
4. Discussion
Our results show that, during the first and second waves of the COVID-19 pandemic in 2020, the number of STEMI patients and primary PCI procedures did not change significantly in comparison to 2019. In comparison to 2019, there was a nonsignificant decrease in the number of primary PCI procedures within the first 3 and 6 h of chest pain during the first and particularly the second waves of the pandemic. There was a nonsignificant increase in hospital heart failure and mitral regurgitation during the first wave of the pandemic, but there was a significant increase in both complications during the second wave. There was also a nonsignificant difference in other hospital complications and mortality between 2019 and both waves of the pandemic.
Similar numbers of STEMI patients were admitted in all three time periods, in contrast to the results of some other studies, which reported significant decreases in the number of STEMI patient admissions during the pandemic in comparison to the pre-pandemic period [7,8,9,10,11,12]. Epidemiological studies have also pointed out that European regions were not equally hit by the COVID-19 pandemic. Great differences existed between areas with limited COVID-19 cases and epicenters of COVID-19 [22,23,24,25,26,27,28,29]. The regional and local impact of COVID-19 had significant consequences for crisis management and policy responses, including STEMI management [22,23,24,25,26,27,28,29,30,31,32,33].
The gender and age of our STEMI patients during both waves of the COVID-19 pandemic were similar to those of patients in the pre-pandemic period. This observation accords with the findings of other studies [34,35]. However, some studies reported increased admissions of younger STEMI patients.
We observed nonsignificant differences in comorbidities among STEMI patients in all studied periods, which is similar to the findings of other studies. However, regarding the nonsignificant increase in arterial hypertension and prior myocardial infarction in the second wave of the pandemic in our patients, we can speculate that patients with comorbidities were more aware of the importance of chest pain during the pandemic than patients without any prior comorbidities.
In parallel to reduced admission numbers of STEMI patients in the epicenters of COVID-19, studies have also reported a significant decline in primary PCI procedures. However, in areas with better healthcare resources and a limited number of COVID-19 patients, the same levels of primary PCI procedure use were reported during the pandemic compared with the pre-pandemic period [12,14,15,34,35,36]. In our STEMI patients, primary PCI remained the leading reperfusion strategy during the pandemic and was performed in more than 90% of patients with a similar TIMI III flow after primary PCI, even reaching 80% in the second wave of COVID-19 pandemic.
In spite of more than 90% of primary PCI procedures taking place in our STEMI patients during the pandemic, only 25% of primary PCIs were performed within the first 3 h during the second wave of the pandemic in comparison to 40% in 2019 and 38% during the first wave. However, this difference was nonsignificant. Several factors were associated with a more pronounced time delay for primary PCI during the second wave. In the first place, there was an increased number of COVID-19 cases in the ER. On the other hand, several STEMI patients avoided hospitals due to the fear of becoming infected, as well as being generally recommended to stay at home. There was time-consuming use of personal protection equipment by the medical staff during transport, in the ER, and in the catheterization laboratory, as well as time-consuming nasopharyngeal swab sampling and waiting for the results before entering the catheterization laboratory [6,37]. Other studies report similar reasons for time delays for primary PCI [13,14,15].
In our patients, we observed an increased incidence of hospital heart failure as assessed by Killip classification, particularly in the second wave the pandemic. The prevalence of cardiogenic shock in the second wave of the pandemic was 27%, but the difference in comparison to 2019 was not significant. Longer delays to primary PCI and to appropriate pharmacological treatment represented the most important contributors to heart failure, which in turn was the most important cause of death after STEMI.
Despite a significant difference in heart failure being assessed at the bedside by Killip classification between 2019 and the second wave of the pandemic (23.3% vs. 42%; p = 0.014), we observed only a nonsignificant difference in decreased EF < 45% (21.1% vs. 23.5%; p = 0.66), reflecting the predominant congestive nature of heart failure. This observation was similar to the findings of a multicenter registry study on STEMI patients by Fardman et al., demonstrating that longer total ischemia time in STEMI patients in the COVID-19 pandemic resulted in an increase in congestive heart failure [38].
The hospital mortality of our STEMI patients in 2019 was 8.9%. It increased to 9.4% during the first wave and to 13.5% during the second wave of the pandemic. However, the differences were nonsignificant. One meta-analysis reported a significant increase in the mortality of STEMI patients during the pandemic in comparison to the pre-pandemic period. However, another meta-analysis demonstrated a significant increase in hospital mortality only in COVID-19 epicenters in Italy and China, whereas globally, only nonsignificant changes in STEMI mortality were observed during the pandemic [9,12,15,16]. The rapid optimization of pre-hospital and in-hospital procedures by the medical community and cardiology professionals are the most likely reasons for better outcomes in STEMI patients in some centers during the COVID-19 pandemic [12,37,39,40].
The limitations of our study are numerous. The study is retrospective and observational and was performed in a single tertiary medical center in Northeastern Slovenia. Therefore, a limited number of patients were included within a limited time interval. However, the data give important insights into STEMI admissions, the percentage of early treatment by primary PCI, and the hospital outcomes of STEMI patients. Our data suggest that in the future, more effort should be put into educating the population to be aware of oppressive chest pain and to call emergency services for help as soon as possible despite the pandemic. We also learned that faster and more accurate microbiological testing, better organization of medical facilities, and vaccinating the population could improve prognoses in non-communicable diseases, such as acute STEMI, in future pandemics.
5. Conclusions
In parallel with the increased severity and number of COVID-19 patients in the second wave of the COVID-19 pandemic in 2020, we observed more delays to primary PCI in STEMI patients, which led to a significant increase in hospital heart failure and a nonsignificant increase in hospital mortality during October–December 2020 in comparison to the pre-pandemic period.
Author Contributions
Conceptualization, A.S., M.M., M.K. and D.Š.; methodology, A.S. and M.K.; writing—original draft preparation, A.S.; writing—review and editing, A.S.; visualization, A.S.; supervision, A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of the University Clinical Center Maribor (approval UKC-MB kmE-62/19) for studies involving humans.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.
Acknowledgments
We would like to thank the staff at the Medical Statistics Center for help with the electronic data and Alojz Tapajner for help with the statistics.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 22 March 2022).
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef]
- Wang, M.-Y.; Zhao, R.; Gao, L.-J.; Gao, X.-F.; Wang, D.-P.; Cao, J.-M. SARS-CoV-2: Structure, Biology, and Structure-Based Therapeutics Development. Front. Cell. Infect. Microbiol. 2020, 10, 587269. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- WHO Europe. A Timeline of WHO’s Response to COVID-19 in the WHO European Region A Living Document (Version 2.0 from 31 December 2019 to 31 December 2020). Available online: WHO-EURO-2021-1772-41523-56652-eng.pdf (accessed on 22 March 2022).
- Pessoa-Amorim, G.; Camm, C.F.; Gajendragadkar, P.; De Maria, G.L.; Arsac, C.; Laroche, C.; Zamorano, J.L.; Weidinger, F.; Achenbach, S.; Maggioni, A.; et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: A survey by the European Society of Cardiology. Eur. Heart J. Qual. Care. Clin. Outcomes 2020, 6, 210–216. [Google Scholar] [CrossRef]
- Gluckman, T.J.; Wilson, M.A.; Chiu, S.-T.; Penny, B.W.; Chepuri, V.B.; Waggoner, J.W.; Spinelli, K.J. Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic. JAMA Cardiol. 2020, 5, 1419–1424. [Google Scholar] [CrossRef]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Perrone Filardi, P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef]
- Fabris, E.; Bessi, R.; De Bellis, A.; Gregorio, C.; Peratoner, A.; Lardieri, G.; Cominotto, F.; Vitrella, G.; Rakar, S.; Perkan, A.; et al. COVID-19 impact on ST-elevation myocardial infarction incidence rate in a Italian STEMI network: A U-shaped curve phenomenon. J. Cardiovasc. Med. 2021, 22, 344–349. [Google Scholar] [CrossRef]
- Jaina, V.; Gupta, K.; Bhatiac, K.; Bansal, A.; Arora, S.; Khandelwal, A.K.; Rosenberg, J.R.; Levisay, J.P.; Tommaso, C.L.; Ricciardi, M.J.; et al. Management of STEMI during the COVID-19 pandemic: Lessons learned in 2020 to prepare for 2021. Trends Cardiovasc. Med. 2021, 31, 135–140. [Google Scholar] [CrossRef]
- Rattka, M.; Dreyhaupt, J.; Winsauer, C.; Stuhler, L.; Baumhardt, M.; Thiessen, K.; Rottbauer, W.; Imhof, A. Effect of the COVID-19 pandemic on mortality of patients with STEMI: A systematic review and metaanalysis. Heart 2021, 107, 482–487. [Google Scholar] [CrossRef]
- Soylu, K.; Coksevim, M.; Yanık, A.; Bugra Cerik, I.; Aksan, G. Effect of COVID-19 pandemic process on STEMI patients timeline. Int. J. Clin. Pract. 2021, 75, 14005. [Google Scholar] [CrossRef] [PubMed]
- De Luca, G.; Verdoia, M.; Cercek, M.; Okkels Jensen, L.; Vavlukis, M.; Calmac, L.; Johnson, T.; Rourai Ferrer, G.; Ganyukov, V.; Wojakowski, W.; et al. Impact of COVID-19 Pandemic on Mechanical Reperfusion for Patients With STEMI. J. Am. Coll. Cardiol. 2020, 76, 2321–2330. [Google Scholar] [CrossRef] [PubMed]
- Chew, N.W.S.; Ow, W.Z.G.; Teo, V.X.Y.; Heng, R.R.Y.; Ng, C.H.; Lee, C.-H.; Low, A.F.; Chan, M.Y.-Y.; Yeo, T.-C.; Tan, H.-C.; et al. The Global Effect of the COVID-19 Pandemic on STEMI Care: A Systematic Review and Meta-analysis. Can. J. Cardiol. 2021, 37, 1450–1459. [Google Scholar] [CrossRef] [PubMed]
- Xiang, D.; Xiang, X.; Zhang, W.; Yi, S.; Zhang, J.; Gu, X.; Xu, Y.; Huang, K.; Su, X.; Yu, B.; et al. Management and Outcomes of Patients With STEMI During the COVID-19 Pandemic in China. J. Am. Coll. Cardiol. 2020, 76, 1318–1324. [Google Scholar] [CrossRef]
- COVID-19 Sledilnik. Available online: https://covid-19.sledilnik.org/sl/stats (accessed on 22 March 2022).
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Huber, K.; Goldstein, P. COVID-19: Implications for prehospital, emergency and hospital care in patients with acute coronary syndromes. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. The Task Force for the diag.nosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef]
- Calandra, T.; Cohen, J. The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit. Care Med. 2005, 33, 1538–1548. [Google Scholar] [CrossRef]
- Bourdin, S.; Amdaoud, M.; Arcuri, G.; Costanzo, G.D.; Eva, M.; Iatu, C.; Ibanescu, B.; Jeanne, L.; Levratto, N.; Nadou, F.; et al. ESPON STUDY. Geography of COVID-19 Outbreak and First Policy Answers in European Regions and Cities. Policy Brief. December 2020. Available online: https://www.espon.eu/sites/default/files/attachments/GEOCOV%20final%20report.pdf (accessed on 5 April 2022).
- Scalise, M.; Bossone, E.; Mannelli, M.P.; Ranieri, B.; Franzese, M.; Castaldo, R.; Fidecicchi, A.; Esposito, M.; Cocchia, R.; Lodato, S.; et al. STEMI-PCI incidence rates and outcomes during COVID-19 pandemic: Insights from Cardarelli Hospital, Naples, Southern Italy. Eur. J. Prev. Cardiol. 2022, 29, e216–e219. [Google Scholar] [CrossRef]
- Garcia, S.; Stanberry, L.; Schmidt, C.; Sharkey, S.; Megaly, M.; Albaghdadi, M.S.; Meraj, P.M.; Garberich, R.; Jaffer, F.A.; Stefanescu Schmidt, A.C.; et al. Impact of COVID-19 pandemic on STEMI care: An expanded analysis from the United States. Catheter. Cardiovasc. Interv. 2021, 98, 217–222. [Google Scholar] [CrossRef]
- Little, C.D.; Kotecha, T.; Candilio, L.; Jabbour, R.J.; Collins, G.B.; Ahmed, A.; Connolly, M.; Kanyal, R.; Demir, O.M.; Lawson, L.O.; et al. COVID-19 pandemic and STEMI: Pathway activation and outcomes from the pan-London heart attack group. Open Heart 2020, 7, e001432. [Google Scholar] [CrossRef] [PubMed]
- Hodas, R.; Benedek, I.; Rat, N.; Kovacs, I.; Chitu, M.; Benedek, T. Impact of COVID-19 Pandemic on STEMI Networks in Central Romania. Life 2021, 11, 1004. [Google Scholar] [CrossRef]
- Velicu, M.A.; Furlanetti, L.; Jung, J.; Askhan, K. Epidemiological trends in COVID-19 pandemic: Prospective critical appraisal of observations from six countries in Europe and the USA. BMJ Open 2021, 11, e045782. [Google Scholar] [CrossRef] [PubMed]
- Rattka, M.; Stuhler, L.; Winsauer, C.; Dreyhaupt, J.; Thiessen, K.; Baumhardt, M.; Markovic, S.; Rottbauer, W.; Imhof, A. Outcomes of Patients With ST-Segment Elevation Myocardial Infarction Admitted During COVID-19 Pandemic Lockdown in Germany—Results of a Single Center Prospective Cohort Study. Front. Cardiovasc. Med. 2021, 8, 638954. [Google Scholar] [CrossRef] [PubMed]
- Scholz, K.H.; Lengenfelder, B.; Thilo, C.; Jeron, A.; Stefanow, S.; Janssens, U.; Bauersachs, J.; Schulze, P.C.; Winter, K.D.; Schröder, J.; et al. Impact of COVID-19 outbreak on regional STEMI care in Germany. Clin. Res. Cardiol. 2020, 109, 1511–1521. [Google Scholar] [CrossRef]
- Cameli, M.; Pastore, M.C.; Mandoli, G.E.; D’Ascenzi, F.; Focardi, M.; Biagioni, G.; Cameli, P.; Patti, G.; Franchi, F.; Mondillo, S.; et al. COVID-19 and Acute Coronary Syndromes: Current Data and Future Implications. Front. Cardiovasc. Med. 2021, 7, 593496. [Google Scholar] [CrossRef] [PubMed]
- Henry, T.D.; Kereiakes, D.J. The direct and indirect effects of the COVID-19 pandemic on cardiovascular disease throughout the world. Eur. Heart J. 2022, 43, 1154–1156. [Google Scholar] [CrossRef]
- Cannata, A.; Bromage, D.I.; McDonagh, T.A. The collateral cardiovascular damage of COVID-19: Only history will reveal the depth of the iceberg. Eur. Heart J. 2021, 42, 1524–1527. [Google Scholar] [CrossRef]
- De Lange, M.; Carvalho, A.S.; Brito Fernandes, Ó.; Lingsma, H.; Klazinga, N.; Kringos, D. The Impact of the COVID-19 Pandemic on Hospital Services for Patients with Cardiac Diseases: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 3172. [Google Scholar] [CrossRef]
- Gramegna, M.; Baldetti, L.; Beneduce, A.; Pannone, L.; Falasconi, G.; Calvo, F.; Pazzanese, V.; Sacchi, S.; Pagnesi, M.; Moroni, F.; et al. ST-Segment–Elevation Myocardial Infarction During COVID-19 Pandemic. Insights From a Regional Public Service Healthcare Hub. Circ. Cardiovasc. Interv. 2020, 13, 009413. [Google Scholar] [CrossRef]
- Baumhardt, M.; Rattka, M.; Dreyhaupt, J.; Thiessen, K.; Markovic, S.; Buckert, D.; Mörike, J.; Schneider, L.M.; Gonska, B.; Scharnbeck, D.; et al. Clinical Characteristics and In-Hospital Outcomes of STEMI Patients Admitted during the SARS-CoV-2 Pandemic—An Observational Comparative Study. Cardiol. Cardiovasc. Med. 2021, 5, 224–235. [Google Scholar] [CrossRef]
- Kiris, T.; Avci, E.; Ekin, T.; Akgün, D.E.; Tiryaki, M.; Yidirim, A.; Hazir, K.; Murat, B.; Yeni, M. Impact of COVID-19 outbreak on patients with ST-segment elevation myocardial ınfarction (STEMI) in Turkey: Results from TURSER study (TURKISH St-segment elevation myocardial ınfarction registry). J. Thromb. Thrombolysis 2021, 53, 321–334. [Google Scholar] [CrossRef] [PubMed]
- Huh, S. How to train the health personnel for protecting themselves from novel coronavirus (COVID-19) infection during their patient or suspected case care. J. Educ. Eval. Healt. Prof. 2020, 17, 10. [Google Scholar] [CrossRef]
- Fardman, A.; Zahger, D.; Orvin, K.; Oren, D.; Kofman, N.; Mohsen, J.; Tsafrir, O.; Asher, E.; Rubinshtein, R.; Jamal, J.; et al. Acute myocardial infarction in the Covid-19 era: Incidence, clinical characteristics and in-hospital outcomes—A multicenter registry. PLoS ONE 2021, 16, 0253524. [Google Scholar] [CrossRef] [PubMed]
- Mesnier, J.; Cottin, Y.; Coste, P.; Ferrari, E.; Schiele, F.; Lemesle, G.; Thuaire, C.; Angoulvant, D.; Cayla, G.; Bouleti, C.; et al. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: A registry study. Lancet Public Health 2020, 5, 536–542. [Google Scholar] [CrossRef]
- Burger, A.L.; Kaufmann, C.C.; Jäger, B.; Pogran, E.; Ahmed, A.; Wojta, J.; Farhan, S.; Huber, K. Direct cardiovascular complications and indirect collateral damage during the COVID-19 pandemic. A review. Wien. Klin. Wochenschr. 2021, 133, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).